Abstract
Purpose
Conservative management is successful in unperforated (Hinchey Ia) acute diverticulitis (AD) and also generally in local perforation or small abscesses (Hinchey Ib). A higher degree of radiological severity (Hinchey >Ib), ie, a larger abscess (>3–4 cm) or peritonitis, commonly requires percutaneous drainage or surgery. Retrospective studies show that high levels of C-reactive protein (CRP) distinguish Hinchey Ia from all cases of minor and major perforations (Hinchey >Ia). The current study aims to evaluate the usefulness of CRP in distinguishing AD with a higher degree of severity (Hinchey >Ib) from cases that can be treated noninvasively (Hinchey Ia/Ib).
Methods
Data from consecutive patients with AD were collected prospectively. All underwent computed tomography (CT). Index parameters obtained at the initial evaluation at the emergency unit were analyzed to assess the association with the outcome. The exclusion criteria comprised concomitant conditions that affected CRP baseline levels.
Results
Ninety-nine patients were analyzed. Eighty-eight had mild radiological grading (Hinchey Ia/Ib), and 11 had severe radiological grading (Hinchey >Ib) (median index CRP 80 mg/L vs 236 mg/L [P<0.001]). White blood cells, neutrophils/lymphocytes, serum creatinine, serum glucose, generalized peritonitis, generalized abdominal tenderness, urinary symptoms, and index CRP were related to severe disease. Index CRP was the only independent predictor for Hinchey >Ib (P=0.038). The optimal cutoff value calculated by receiver operating characteristic curve analysis was found to be 173 mg/L (sensitivity 90.9%, specificity 90.9%, P<0.001). All patients who underwent radiological drainage or surgery had an index CRP >173 mg/L and Hinchey >Ib.
Conclusion
CRP levels >173 mg/L obtained at the initial evaluation at the emergency unit predict major acute complications in AD. These patients commonly require urgent percutaneous drainage or surgical management.
Introduction
Acute diverticulitis (AD) of the colon is an increasingly prevalent condition in Western societies.Citation1,Citation2 In the US, a 50% rise in incidence was documented for the 2000–2007 period compared to the 1990s.Citation1 Similarly, a 2.8-fold increase in the hospital admission rate has been reported in northern Europe over a period of 25 years, contributing to a substantial economic burden.Citation2
Patients with AD experience a varying degree of disease severity. Approximately 80%–85% of patients have a clinically mild disease and are treated conservatively,Citation1–Citation3 even as outpatients.Citation4 Nonoperative treatment is successful in cases of the phlegmonous disease;Citation4 however, recent data have shown that this is also the rule for those with radiological signs of local perforation or a small abscess.Citation4–Citation9 On the contrary, patients with a larger abscess (>4 cm) commonly necessitate percutaneous drainage or operative management, whereas frank peritonitis – either purulent or fecal – mandates an emergency operation.Citation10 Currently, there is a trend toward less operative and interventionist radiological treatment in selected patients with an absence of sepsis or significant comorbidities, regardless of the imaging findings.Citation4–Citation6,Citation8,Citation10,Citation11 Computed tomography (CT) is the preferred imaging method for grading the severity of AD.Citation10 However, it should be emphasized that judgment for the actual necessity of invasive treatment should be based on both clinical and radiological grounds, as CT severity alone does not necessarily mandate the need for drainage or an operation.Citation5,Citation6,Citation8,Citation11
C-reactive protein (CRP) has been found to be a useful marker in the prediction of the inflammation grade and severity of AD.Citation10 According to retrospective data that assessed imaging severity, CRP may discriminate the mere phlegmonous disease from the remainder of cases with either minor or major perforation (local or diffuse free intraperitoneal air, a small or large abscess, peritonitis).Citation3,Citation12–Citation14 However, the value of CRP in predicting the severity of AD should be further evaluated according to specific clinical problems, since patients with a contained perforation or small abscess are as a rule treated conservatively during the acute episode.Citation4–Citation9
The present observational study uses prospectively collected data to evaluate the role of index CRP in predicting the increased severity of AD, defined as the presence of a larger abscess (>3 cm) or peritonitis.
Methods
Demographic, clinical, laboratory, and imaging data were collected prospectively from all patients treated for AD at the Department of Surgery, Konstantopouleion Hospital, Athens, Greece, between 2011 and 2014. The study was approved by the ethics committee of the hospital (local authorization number 19183, research registry identification number 2575). All patients provided written informed consent to participate in the study. The management policy of AD was based on the recommendation available during the period of the study (subsequently updated).Citation15 All patients had a CT scan, which was performed during the initial evaluation at the emergency unit. Intravenous contrast was used for the CT scans unless contraindicated. The modified Hinchey classification by Wasvary et alCitation28 was used to grade radiological severity ().Citation10 Antibiotics were routinely administered. Patients with peritonitis and severe sepsis underwent an emergency operation. Percutaneous drainage was performed on all patients with an abscess >5 cm. Patients with a smaller abscess and those with a local perforation (local extracolonic air) or the simple phlegmonous disease were treated conservatively. The patients’ clinical status was assessed frequently, as deterioration is an indicator of the failure of conservative therapy. Blood cultures were obtained in the case of clinical signs of sepsis. A follow-up colonoscopy was performed for all patients.
Table 1 Depiction of treatment and radiological severity according to the modified Hinchey classification by Wasvary et alCitation28
We analyzed the laboratory and clinical parameters obtained at the initial evaluation of the patient at the emergency unit (index parameters). They were correlated with the level of imaging severity expressed by the CT findings. Patients with the phlegmonous disease (Hinchey Ia) or with a contained perforation or small local abscess (Hinchey Ib) were classified as having mild radiological disease. Patients with a distant or larger abscess (>4–5 cm) or frank peritonitis were classified as having severe radiological disease (Hinchey >Ib).
Dedicated inclusion criteria were employed, as CRP baseline levels may be affected by various factors.Citation16 Liver failure and therapies or diseases affecting the acute-phase stimulus are common causes for the muted or reduced reaction of CRP to infection ().Citation16 Index CRP levels during AD may be reduced in such patients with the same degree of radiological severity. On the other hand, concomitant infections, tissue necrosis or trauma, neoplasia, and other inflammatory disorders may increase CRP baseline levels.Citation16 The exclusion of all these factors increases the homogeneity of the sample, which is essential for the avoidance of bias in any research correlating CRP levels with CT grading.
Table 2 Exclusion criteria (conditions potentially affecting CRP basal levels)
In view of the above, diseases or conditions that could potentially affect baseline CRP levels formed the exclusion criteria of this study (). They comprised the presence or history of extracolonic cancer, autoimmune diseases, inflammatory bowel disease, glucocorticoid therapy,Citation14 or any other immunosuppressive state (either due to disease, transplantation, or medication). Accordingly, patients with a concomitant infection of another organ, prehospital antibiotics (either for diverticulitis or another cause), recent failed discharge, symptoms >5 days, recent surgery (within 1 month), and liver disease were excluded for the same reason. Furthermore, patients with colorectal cancer documented before the study period, during the hospitalization, or at a follow-up colonoscopy were also not considered for analysis. Lastly, patients with chronic sequelae of AD, such as a colonic fistula or unremitting/recurrent symptoms after a previous episodeCitation17 and perforation of a diverticulum without underlying inflammation (eg, during colonoscopy), were considered as distinct entities and excluded.
Statistics
Continuous variables were compared using the Mann–Whitney U test. The association between categorical data was assessed using Fisher’s exact test and the chi-squared test. Statistical significance was set at a P-value of <0.05. Only two-tailed, statistically significant results were considered for multivariate analysis. Logistic regression analysis was used for the assessment of independent predictor factors (multivariate analysis). Receiver operating characteristic (ROC) analysis was used to detect the best prognostic cutoff value of the continuous variables, which were found to be independent risk factors for the outcome. The statistical software package used for the analysis was SPSS 21.0.
Results
Ninety-nine patients with AD were analyzed. Their characteristics and clinical information are given in . The excluded cases are depicted in . In all, 88 cases with a mild disease (Hinchey Ia and Ib) had a median CRP of 80.35 mg/L (range 1.78–299.58 mg/L) and were treated conservatively. Eleven patients with severe CT findings (Hinchey >Ib) had a median CRP of 236 mg/L (range 166–297 mg/L), and nine of them underwent an invasive procedure (). The median CRP level for Hinchey II was 196.0 mg/L (166–286.85 mg/L), and the median CRP level for Hinchey III/IV was 258.5 mg/L (201–297 mg/L). An 89-year-old woman with Hinchey II developed bacteremia and died of multi-organ failure (index CRP 259 mg/L).
Table 3 Patient characteristics, clinical information, and outcome
Index CRP (P<0.001), white blood cells (WBCs; P<0.001), neutrophil/lymphocyte (N/L) ratio (P<0.001), serum creatinine (P=0.004), serum glucose (P=0.031), generalized peritonitis (P=0.011), abdominal tenderness in more than two quadrants (P=0.009), and urinary symptoms (P=0.026) were related to increased radiological severity according to the univariate analysis. Of these factors, only index CRP was an independent predictor for radiological severity in the multivariate logistic regression analysis (P=0.038). ROC curve analysis showed that the best CRP cutoff value for the prediction of Hinchey >Ib is 173 mg/L (sensitivity 90.9%, specificity 90.9%, area under the curve [AUC] 95.8, P<0.001). The negative predictive value (NPV) was 98.7%, and the positive predictive value (PPV) was 55.5%. The relation between the index CRP values of this series and radiological severity is depicted in .
Figure 1 Scatter plot showing the distribution of CRP values for cases with Hinchey Ia and Ib (small circles) and for cases with Hinchey >Ib (larger circles).
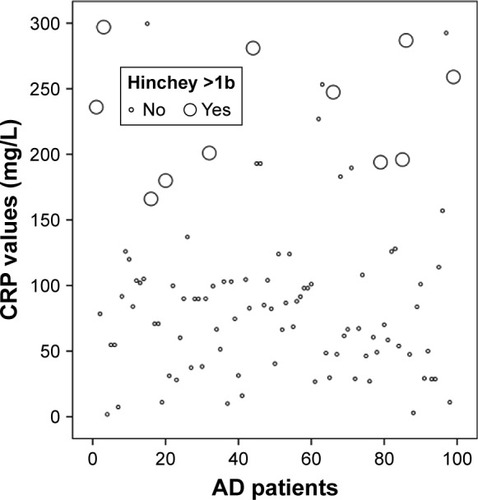
There were 61 (61.6%) patients with CRP levels <100 mg/L. All of them had a Hinchey radiological grade of I (sensitivity 100%, specificity 68.2%), and none necessitated any intervention during the acute attack. In all, 25 (25.3%) patients had CRP levels <50 mg/L (sensitivity 100%, specificity 28.4%). All patients who underwent CT drainage or operation had CRP levels >173 mg/L.
The Hinchey stage of the excluded cases ranged between Ia and III, with index CRP values varying between 1 and 115 mg/L. Of these cases, two patients received the Hartmann procedure: one had Hinchey Ia and an index CRP of 115 mg/L and the other had Hinchey III with an index CRP of 106 mg/L. A patient with Hinchey II and an index CRP of 64 mg/L received percutaneous drainage.
Discussion
This study showed that a high index CRP value is independently related to the increased severity of AD. A CRP level >173 mg/L at presentation accurately identifies patients with major acute complications that correspond to Hinchey stages >Ib. Patients with the mere phlegmonous disease (Hinchey Ia) or a minor perforation or small abscess (Hinchey Ib) presented with lower index CRP values and were all treated medically in our series. The abovementioned results apply to patients without comorbidities or concomitant conditions that affect CRP and patients without chronic sequelae from previous diverticulitis. Univariate analysis showed the association between various further parameters (obtained during the initial evaluation of the patients) and severe AD. These included clinical signs of widespread infection within the abdomen, an increased N/L ratio and WBCs, and laboratory measurements that may be deranged during acute infection (serum creatinine and glucose). However, these factors were not identified as independent predictive factors for severe disease.
Our findings highlight the importance of obtaining a CT scan in patients with suspected AD and an index CRP >173 mg/L. Routine measurement of index CRP is essential, especially when the diagnosis has been reached clinically or with ultrasound.Citation21 Diagnosis with clinical-only means has been reported in part of the patients of series from dedicated centers,Citation2,Citation18,Citation20,Citation24 and its accuracy ranges from 43% to 68%.Citation21 Index CRP is particularly important in rural or remote areas with limited access to diagnostic imaging.Citation25,Citation26
Two previous investigations assessed the role of initial CRP in the prediction of the clinical outcome during index hospitalization. A small prospective observational study reported that patients who underwent emergency surgery for AD had higher index CRP levels (281 vs 58 mg/L).Citation22 Similarly, a retrospective study showed that a CRP value of >170 mg/L (sensitivity 87.5%, specificity 91.1%) is associated with the need for percutaneous drainage and/or surgery in a cohort with the same exclusion criteria as the present study.Citation19
So far, only retrospective reports have correlated CRP with radiological grading.Citation3,Citation12–Citation14 Attention should be paid to the fact that these investigations classified minor perforations and small abscesses (Hinchey Ib) as “severe disease” alongside larger abscesses and generalized peritonitis (Hinchey >Ib). This is also a useful distinction, but it is not entirely consistent with the current clinical perspective, according to which perforated cases with minor radiological complications (Hinchey Ib) are treated medically during the acute phase. In addition, labeling patients who are as a rule managed conservatively (Hinchey Ib)Citation4–Citation9 as having severe disease may contribute to lower sensitivity rates for CRP’s predictive value.Citation3,Citation12–Citation14
The earliest of these reports found that local perforation was unlikely for a CRP value of <50 mg/L, whereas a value of >200 mg/L was a strong indicator of either minor or major complications in imaging (Hinchey >Ia).Citation12 However, it should be noted that CRP values were measured during a 48-hour period before CT.Citation12 This may have created a degree of bias, as CRP levels are highly time dependent and display significant changes in sub-24-hour intervals.Citation23 Another study noted that index CRP levels were significantly lower in patients using corticosteroids for the same radiological degree of severity in AD and provided a rather low CRP cutoff level (CRP >90 mg/L, 88% sensitivity and 75% specificity) for the prediction of Hinchey >Ia in the entire cohort.Citation14 The authors stated that ~20% of CT scans could have been avoided with the use of a CRP threshold of <50 mg/L.Citation14 Two further investigations provided CRP cutoff values of 150 mg/L (sensitivity 65%, specificity 85%)Citation3 and 175 mg/L (sensitivity 61%, specificity 82%)Citation13 for the prediction of Hinchey >Ia. The studies mentioned earlier evaluated unselected cases, as prehospital antibiotics, corticosteroids, immunosuppression, or comorbidities and conditions that affect CRP basal levels were not excluded.Citation3,Citation12–Citation14 This may further explain the calculation of lower sensitivity rates for the CRP cutoff level.Citation3,Citation12,Citation13
We used prospectively collected data, which increased the strength of our investigation. Nevertheless, a future study with a larger cohort is necessary to provide definitive conclusions through the evaluation of a larger subgroup with radiologically severe disease. The present study supported a more clinically oriented definition of severity in patients with AD: local perforation or small abscess (Hinchey Ib) was considered as an uncomplicated disease resulting in the improved NPV of the CRP cutoff level, whereas major perforation only (Hinchey >Ib) constituted the complicated disease. Indeed, patients with the perforated disease who commonly necessitate a higher level of care and interventional or operative management are those with Hinchey >Ib.Citation15 Treatment with antibiotics (and in a few cases, even observation without antibiotics) is generally successful for the resolution of the acute event in Hinchey Ib patients.Citation4–Citation9 Sensitivity and specificity rates were strengthened by the use of dedicated exclusion criteria, which were specifically tailored to the physiology of CRP. The inclusion of patients with factors affecting baseline index CRP levels in the analysis would have decreased the accuracy of the CRP cutoff value, as may have happened in previous studies. Indeed, excluded patients who received interventions in our series had index CRP levels between 64 and 115 mg/L. As a result, index CRP should be used as a predictor of the severity of AD in properly selected patients.
As our patients had undergone a CT scan, this investigation is not designed to support the argument that the amount of staging CT should be reduced in patients with AD and low index CRP values. Since the great majority of patients with an acute episode of the disease experience an uneventful clinical course,Citation1–Citation3 dedicated future research should aim to identify how to avoid unnecessary CT scans. The role of index CRP warrants further evaluation in this context, taking into consideration that clinicalCitation2,Citation18,Citation20,Citation24 and/or ultrasoundCitation21,Citation27 diagnosis is gaining increasing popularity. It is nonetheless judicious that patients with adverse characteristics such as older age,Citation3 bowel obstruction, significant comorbidity or immunosuppressive medication,Citation20 organ dysfunction,Citation24 systemic sepsis, and hypotension at presentation should undergo a CT scan even if they have a low index CRP value. Lastly, it should be mentioned that the maximum abscess diameter in Hinchey Ib cases in our series was 3 cm. Therefore, conclusions cannot be drawn for Hinchey Ib patients with a local pericolic or mesocolic abscess >3 cm.
Conclusion
A high index CRP in patients with AD predicts severe complications, defined as an abscess ≥3 cm or findings of peritonitis in the CT scan. CRP should not be used as a predictor of severity if there are concomitant conditions that may affect its baseline levels. Our investigation calls for the use of meticulous methodological criteria in future research, including patient selection and a clinically oriented definition of disease severity.
Disclosure
The authors report no conflicts of interest in this work.
References
- BharuchaAEParthasarathyGDitahITemporal Trends in the Incidence and Natural History of Diverticulitis: A Population-Based StudyAm J Gastroenterol2015110111589159626416187
- Jamal TalabaniALydersenSEndresethBHEdnaTHMajor increase in admission- and incidence rates of acute colonic diverticulitisInt J Colorectal Dis201429893794524802814
- MäkeläJTKlintrupKTakalaHRautioTThe role of C-reactive protein in prediction of the severity of acute diverticulitis in an emergency unitScand J Gastroenterol201550553654125665622
- MaliJPMentulaPJLeppäniemiAKSallinenVJSymptomatic Treatment for Uncomplicated Acute Diverticulitis: A Prospective Cohort StudyDis Colon Rectum201659652953427145310
- DharmarajanSHuntSRBirnbaumEHFleshmanJWMutchMGThe efficacy of nonoperative management of acute complicated diverticulitisDis Colon Rectum201154666367121552049
- GregersenRMortensenLQBurcharthJPommergaardHCRosenbergJTreatment of patients with acute colonic diverticulitis complicated by abscess formation: A systematic reviewInt J Surg20163520120827741423
- ThorissonASmedhKTorkzadMRPåhlmanLChabokACT imaging for prediction of complications and recurrence in acute uncomplicated diverticulitisInt J Colorectal Dis201631245145726490053
- SallinenVJMentulaPJLeppäniemiAKNonoperative management of perforated diverticulitis with extraluminal air is safe and effective in selected patientsDis Colon Rectum201457787588124901689
- DanielsLÜnlüÇde KorteNRandomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitisBr J Surg20171041526127686365
- SartelliMCatenaFAnsaloniLWSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency settingWorld J Emerg Surg2016113727478494
- CostiRCauchyFLe BianAChallenging a classic myth: pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery in hemodynamically stable patients. A 10-year experience with a nonoperative treatmentSurg Endosc20122672061207122274929
- KäserSAFankhauserGGlauserPMToiaDMaurerCADiagnostic value of inflammation markers in predicting perforation in acute sigmoid diverticulitisWorld J Surg201034112717272220645093
- van de WallBJDraaismaWAvan der KaaijRTThe value of inflammation markers and body temperature in acute diverticulitisColorectal Dis201315562162623088216
- NizriESpringSBen-YehudaAC-reactive protein as a marker of complicated diverticulitis in patients on anti-inflammatory medicationsTech Coloproctol201418214514923807310
- FeingoldDSteeleSRLeeSPractice parameters for the treatment of sigmoid diverticulitisDis Colon Rectum201457328429424509449
- MontecuccoFMachFNew evidences for C-reactive protein (CRP) deposits in the arterial intima as a cardiovascular risk factorClin Interv Aging20083234134918686755
- AmbrosettiPGervazPManagement of sigmoid diverticulitis: an updateUpdates Surg2016681253527086288
- RidgwayPFLatifAShabbirJRandomized controlled trial of oral vs intravenous therapy for the clinically diagnosed acute uncomplicated diverticulitisColorectal Dis200911994194619016815
- KechagiasARautioTKechagiasGMäkeläJThe role of C-reactive protein in the prediction of the clinical severity of acute diverticulitisAm Surg201480439139524887672
- LorimerJWDoumitGComorbidity is a major determinant of severity in acute diverticulitisAm J Surg2007193668168517512276
- AndewegCSMulderIMFelt-BersmaRJFGuidelines of Diagnostics and Treatment of Acute Left-Sided Colonic DiverticulitisDig Surg2013304–627829223969324
- JohnSKTeoNBForsterALA prospective study of acute admissions in a surgical unit due to diverticular diseaseDig Surg200724318619017522465
- KechagiasARautioTMäkeläJThe early C-reactive protein trend does not have a role in monitoring acute diverticulitis progressionChir20161114347
- SallinenVJLeppäniemiAKMentulaPJStaging of acute diverticulitis based on clinical, radiologic, and physiologic parametersJ Trauma Acute Care Surg201578354355125710425
- NixonGSamaranayakaAde GraafBGeographic disparities in the utilisation of computed tomography scanning services in southern New ZealandHealth Policy2014118222222824973925
- LysdahlKBBørretzenIGeographical variation in radiological services: a nationwide surveyBMC Health Serv Res200772117302970
- de KorteNKuyvenhovenJPvan der PeetDLMild colonic diverticulitis can be treated without antibiotics. A case-control studyColorectal Dis201214332533021689302
- WasvaryHTurfahFKadroOBeauregardWSame hospitalization resection for acute diverticulitisAm Surg199965763263510399971
