Abstract
Appropriate selection and correct use of inhalation devices is an integral component in the management of asthma and chronic obstructive pulmonary disease (COPD). It is well known that there are many challenges with the use of inhalers, and no one device suits all patients. Challenges can range from difficulties related to lung disease severity and pulmonary function to physical considerations, including manual dexterity and comorbidities such as arthritis. In terms of device selection and adherence, patient engagement and satisfaction are also important factors to consider. Furthermore, problems with inhaler use can be most evident in children and older patients. Here, we discuss aspects for consideration with commonly used devices, including nebulizers, pressurized metered-dose inhalers, dry powder inhalers, and the soft mist inhaler. As each inhaler offers varying technical properties, a tailored and personalized approach to the selection of the most appropriate device for the patient is highly recommended in order to increase the likelihood of achieving improved disease outcomes and enhance persistence with device adherence. Importantly, education and support is crucial, not only to enable patients to recognize the need for optimal disease management, but also to help them develop good inhaler technique. In addition, health care professionals should also aim to increase their knowledge of the devices they prescribe, and develop systems to ensure that they offer comprehensive support to patients in clinical practice. Considering these aspects, this review discusses potential strategies to help address the challenges of inhaler use in asthma and COPD.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are common chronic conditions that comprise approximately 78% of direct health care costs associated with respiratory diseases in the European Union.Citation1 In the UK alone, 5.4 million patients are currently receiving treatment for asthma; of these, 1.1 million are children.Citation2 Over three million people die of COPD worldwide each year, an estimated 6% of all deaths worldwide.Citation3 The delivery of drugs by inhalation is an integral component in the treatment and management of patients with both diseases. Over the past 30 years, there has been unprecedented growth in the market for inhaled therapy, with annual sales having increased from $7 billion in 1987 to $36 billion in 2014 and with over 90 billion inhaled doses prescribed to patients in a single year.Citation4 Unlike systemic treatments, inhaled medicines are rapidly directed to the airways, allowing for rapid onset. Targeting a drug directly to the lungs allows for lower doses to be administered, limiting potential side effects. There is a large choice of inhalers; in 2011, more than 230 different device-drug combinations were available to prescribers in Europe,Citation5 with 48 different inhaler products in the UK alone,Citation6 each with its own specific design characteristics.Citation7,Citation8 The most common device types sold in Europe in 2011 were pressurized metered-dose inhalers (pMDIs; 47.5%), followed by dry powder inhalers (DPIs; 39.5%) and nebulizers (13%), although distribution between inhalers differed considerably between countries.Citation5 Therefore, choosing the most appropriate device to meet individual patient needs is an important consideration in clinical practice.
The correct use of inhalation devices and adherence to prescribed therapy are key aspects in achieving better clinical control and improved quality of life.Citation9–Citation11 Lack of adherence is an important health challenge, yet both asthma and COPD have lower adherence rates compared with other chronic conditions.Citation12 The detrimental impact of lack of adherence to COPD medication has been well documented by the TOwards a Revolution in COPD Health (TORCH) study, which found it to be significantly associated with increased risk of death and admission to hospital due to exacerbations.Citation13 In patients with COPD discharged from hospital, adherence to medication has been found to be low, with impairment in cognitive function and degree of airways obstruction being key negative influences.Citation14 It is recognized that a wide range of factors are known to present challenges to patients with respect to inhaler use, including inhalation technique and pulmonary function. In patients with asthma or COPD, incorrect inhaler technique is associated with a 50% increased risk of hospitalization, increased emergency department visits, and increased use of oral corticosteroids.Citation15 User errors are common, regardless of the device used. A study of 3,393 devices used for continuous treatment of COPD in 2,935 patients has found critical errors in inhalation tests, including with Breezhaler® (Novartis AG, Basel, Switzerland), Diskus® (GlaxoSmithKline, London, UK), Handihaler® (Boehringer Ingelheim Pharma, Ingelheim am Rhein, Germany), pMDIs, Respimat® (Boehringer Ingelheim Pharma), and Turbuhaler® (AstraZeneca, Cambridge, UK) in 15.4%, 21.2%, 29.3%, 43.8%, 46.9%, and 32.1% of patients.Citation16 A recent systematic review, however, found 299 descriptions for “critical error”, highlighting the need to achieve a consensus on the definition of an inhaler critical error.Citation17 It is also recommended that patient preferences for devices should be considered when prescribing an inhaler,Citation10 but physicians must be cognizant that patients often overestimate their ability to handle a device correctly.Citation18 Factors that influence patient preference include simplicity and convenience (eg, size and durability) and user experience (eg, taste and side effects).Citation19 Inhaler technique is not necessarily improved due to higher satisfaction with a device, a health care professional’s personal perspective that the patient is engaged in the choice of device, or a patient feeling comfortable using a device in public.Citation20 Given the substantial cost of managing asthma and COPD worldwide, it is important to optimize the use of inhalation devices and technique.Citation21 Strategies to achieve this include the provision of high-quality education, both for patients and the multidisciplinary team (MDT) involved in asthma care, utilization of device technology, and implementation of techniques designed specifically to support adherence.
Scope
This review discusses the factors for consideration when choosing an inhaler device in adults and children with asthma or COPD. It presents evidence to support the selection of the most appropriate device to meet individual patient’s needs, with the aim of optimizing adherence and hence patient outcomes. This is not a systematic literature review, rather an overview of current thoughts, and draws upon clinical experience as well as current literature.
Inhalation devices in asthma and COPD
A variety of different drug and inhaler combinations are available for the management of asthma and COPD, thereby increasing the likelihood of finding an appropriate option for each individual patient. Inhaler devices vary in several ways, including how the inhaler dispenses the medication, whether the treatment is passively or actively generated (eg, using propellant, mechanical, or compressed air), aspects of the drug formulation (eg, solution, dry powder, or mist), whether the inhaler contains medication in a single- or multi-dose, and whether the device is disposable or refillable.Citation21 Each inhaler device also has unique design characteristics, meaning that there is the option to tailor choice to meet the patient’s specific needs.Citation22
However, it can be appreciated that these factors also present the challenge of ensuring that the patient knows how to use their own device, and that they have sufficient education and support to continue to use it properly. This is compounded by the fact that patients are often given multiple devices that work in very different ways. The use of multiple respiratory inhalers requiring different inhalation techniques has been shown to have an adverse effect on clinical outcomes in patients with COPDCitation23 and asthma.Citation24 Patients who believe using their inhaler is an important part of their asthma management demonstrate higher levels of correct inhaler use.Citation21 However, it is recognized that in addition to understanding the need to use an inhaler for disease control, patients must be educated on the necessity of using it properly.Citation25 Thus, from the patient perspective, it is likely that the choice of an inhalation device is often as important as the choice of treatment.Citation21 The most commonly used devices include nebulizers, pMDIs, DPIs, and the soft mist inhaler (SMI). The advantages and limitations of the main inhaler devices are overviewed in . Visual images of the different inhaler types in this article can be found on http://inhalers4u.org/ and https://www.rightbreathe.com/.
Table 1 Advantages and limitations of commonly used inhalation devices
Nebulizers
Nebulizers are one of the oldest types of device. In general, they are only used in the emergency setting for the acute treatment of patients, or in chronic disease management for children or elderly patients who are unable to use an inhaler with a spacer or who have coordination problems.Citation10,Citation26–Citation28 Once operational, nebulizers are easy to use and offer a convenient way of delivering a higher dose of treatment to the airways if required.Citation26 As nebulizers omit the need for patient coordination between inhalation and actuation, these devices are particularly useful in those with cognitive, neuromuscular, or ventilation impairments.Citation26–Citation28 Over 50% of patients using nebulizers instead of other devices do so because of physical or cognitive disabilities.Citation26,Citation27,Citation29 However, most nebulizer devices are generally bulky and inconvenient, require regular maintenance, prolong drug delivery from seconds to 10–15 minutes, and require regular thorough cleaning to sterilize the device.Citation27 It has been shown that in the acute management of disease, nebulizers produced outcomes that were not significantly different than pMDIs with a spacer;Citation30 but compared with DPIs, nebulizers may be beneficial in COPD patients with a suboptimal inspiratory flow.Citation31 A new portable nebulizer (Lonhala™ Magnair™, Sunovion Pharmaceuticals Inc., Marlborough, MA, USA), designed to administer glycopyrrolate within 2–3 minutes whilst allowing patients to breathe normally, has recently been approved by the US Food and Drug Administration (FDA).Citation32
Pressurized metered-dose inhalers
The pMDI is a commonly used device, driven by the wide range of medication that can be delivered via this type of inhaler and the relatively low costs. Recent years have seen the transition from chlorofluorocarbon (CFC) pMDIs, which are almost obsolete, to mainly hydrofluoroalkane (HFA) pMDIs. Available HFA solutions include the long-acting β2-agonist formoterol; the corticosteroids ciclesonide (CIC), beclomethasone dipropionate (BDP), and flunisolide; and a drug combination of BDP/formoterol in a single inhaler.Citation33 BDP and CIC formulations contain extra-fine particles (,2 μm mass median aerodynamic diameter), which are associated with lower oropharyngeal deposition and enhanced deposition in the lung.Citation33 Preparations with extra-fine inhaled corticosteroids (ICS) have significantly higher odds of achieving asthma control, with lower exacerbation rates at significantly lower doses than fine-particle ICSs.Citation34 Patients stepping up to extra-fine particle ICS preparations experienced lower risk of pneumonia, acute COPD exacerbations, and respiratory events.Citation35 Common user errors with pMDIs include inhaling too fast (and thus not slowly and deeply), failure to tilt head to the correct position, failure to empty lungs prior to inhalation, and failure to hold breath following inhalation.Citation11,Citation21 Patients are also not always able to reliably determine the remaining number of doses, as there are still pMDI devices on the market that do not have a dose counter despite FDA guidance in 2003. In a study assessing patient satisfaction with their pMDI, 52% reported that they were “extremely unsure” and 10% “somewhat unsure” of how much medication remained.Citation8 While this has been solved by the addition of dose counters in many devices, the patient must be aware of the need to keep track of remaining medication.Citation36
Dry powder inhalers
DPIs were introduced into clinical practice as user-friendly alternatives to CFC- and HFA-driven pMDIs.Citation37 Breath-actuated DPIs are aimed to overcome the difficulties with coordination of inhaler actuation and inspiration.Citation15,Citation38 There are three main systems: capsule-based pre-metered single-dose devices; multi-unit dose inhalers (preloaded by the manufacturer with a blister foil); and multiple-dose inhalers that employ an in-built mechanism that meters out a single dose with each actuation from a reservoir of powder.Citation38,Citation39 Effective use of a DPI requires that each dose is primed and loaded in the correct manner.Citation40 DPIs derive the energy for emptying the drug system from the user’s inspiratory flow, and the failure to achieve a forceful inspiratory flow through a device is the most common critical mishandling error with DPIs, occurring in 26%–38% of cases.Citation11,Citation15 Common errors for DPIs include not keeping the device in the correct position while loading the dose, failure to tilt head in the correct position, insufficient inspiratory effort, and not emptying lungs before inhalation.Citation11,Citation21 It is increasingly recognized that many patients with asthma and COPD find difficulty in generating the necessary optimal inspiratory flow rates for DPIs in order to achieve effective drug delivery and consequent clinical benefit.Citation41 DPIs are also susceptible to heat and moisture, and special precaution must be taken to avoid humidity. This means that their use in hot and humid climate zones is limited, and care must be taken to store the device in appropriate conditions.Citation42,Citation43
Soft mist inhalers
The SMI provides an alternative option to pMDIs and DPIs, aiming to improve the effective delivery of drug to the lungs in order to benefit the patient and enhance adherence. The Respimat® Soft Mist™ inhaler (Boehringer Ingelheim Pharma), so far the only commercially available SMI for asthma and COPD, was developed with the aim of providing optimal drug delivery to the lungs while avoiding propellants, as well as to reduce the need for patient coordination and inspiratory effort.Citation28,Citation37,Citation44 The Respimat® device does not require propellants as it is powered by the energy of a compressed spring inside the inhaler, and individual doses are delivered via a specifically engineered nozzle system as a slow-moving aerosol cloud.Citation28 In addition, as the aerosol is generated from a solution rather than a powder, the Respimat® is resilient to moisture, making it suitable for humid climates.Citation28 While the required inhalation technique is like that used with a pMDI, the aerosol is released very slowly from the device compared with an HFA-driven pMDI.Citation45 Dal Negro et alCitation46 compared the instant velocity and the consistency of the emitted cloud from five different pMDIs and the Respimat® at different distances from the nozzle and at different levels of canister filling. Findings suggest that the dynamic characteristics of the SMI result in higher stability of the cloud emitted and hence may contribute to more convenient use to the patient. This is mainly attributed to the slower jet emission and to the more homogeneous composition of the droplet cloud generated. Findings showed that the higher stability of cloud emission from the Respimat® was likely to contribute to easier and more convenient use for patients.Citation47 Additionally, the relatively long duration over which the dose is expelled from the Respimat® (about 1.2 s compared with 0.1 s from traditional pMDIs) is thought to largely reduce the impact of poor coordination between actuation and inspiration (a regular patient error still seen with the Respimat® deviceCitation16), thus improving the potential for greater lung deposition.Citation8 Thus, while coordination between actuation and inhaling is required, the velocity of the Respimat® reduces the potential for drug impaction in the throat. Scintigraphic studies with the Respimat® device have reported that, compared with an HFA-based pMDI, lung deposition is higher (up to 50%) and oropharyngeal deposition is lower.Citation48 These findings are attributed to the small particle size emitted by the Respimat®. Overall, the Respimat® Soft Mist™ inhaler offers an alternative option in clinical practice, overcoming some of the limitations of other devices ().
Inhaler selection in clinical practice
Choice of inhaler depends on a combination of factors,Citation49,Citation50 including pulmonary function (ie, inspiratory flow and breathing techniqueCitation22,Citation51), device handling,Citation8,Citation52–Citation55 use of a spacer, required inhaler technique,Citation7,Citation11,Citation56,Citation57 and patient preference.Citation19,Citation58,Citation59 Correct inhaler technique is important for optimal delivery of the drug to the lungs and peripheral airways, resulting in greater potential for the achievement of disease control.Citation36,Citation57,Citation60,Citation61 As treatment efficacy is linked to adherence, addressing patient preferences are essential,Citation62 and tailored device selection can help enhance patient satisfaction, treatment adherence, and long-term outcomes.Citation22,Citation62
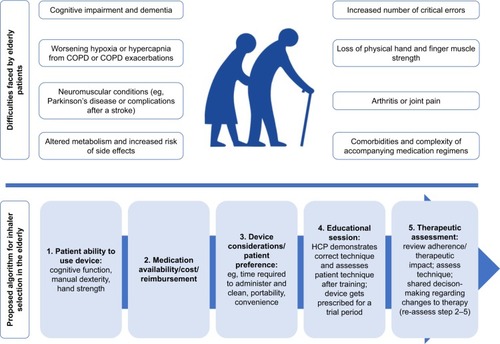
Physical barriers that affect device handling are well documented.Citation8,Citation52–Citation55 Children, the elderly, and those with conditions that may impact on handgrip and manual dexterity require special consideration to ensure selection of the most appropriate inhaler. In older patients, common physical challenges include difficulty manipulating the device due to problems with dexterity, including osteoarthritis, joint pain, stroke, and muscle weakness.Citation26,Citation27,Citation60 Difficulty connecting a pMDI to a spacer and an inability to achieve a firm seal around the mouthpiece when using inhalers alone or with a spacer have also been suggested, particularly for patients with cognitive impairment, facial weakness, or who are missing teeth. In children, the choice of inhaler more specifically depends on the child’s age and capability, and challenges with correct handling may be experienced due to manual dexterity and finger size. Successful inhaler use in young children depends on coordination, the technical properties of the inhalation device, and the ability of the child to perform a correct inhalation maneuver with the device.Citation55 Spacers are commonly used in children to reduce the need for actuation and breathing coordination.Citation52–Citation54 A summary showing the challenges related to the use of inhalation therapy in children and a guide on age-appropriate devices and interfaces are shown in . Specific issues related to the use of inhalation therapy in elderly patients and an algorithm for inhaler selection in this patient group are shown in .
Figure 1 Challenges of inhalation therapy in pediatric patients, and age-appropriate inhaler devices and interfaces.
Abbreviations: DPI, dry powder inhaler; pMDI, pressurized metered-dose inhaler; SMI, soft mist inhaler; VHC, valved holding chamber.
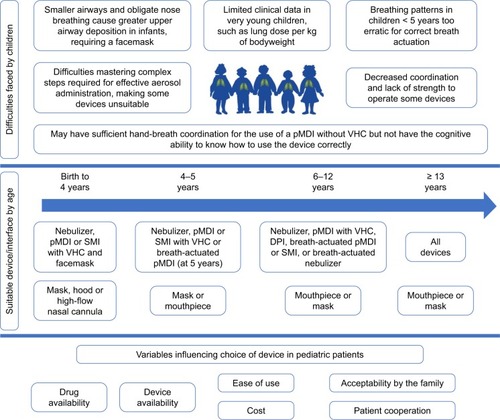
Figure 2 Challenges with the use of inhalation therapy in elderly patients, and an algorithm for appropriate inhaler device selection.Citation26,Citation92,Citation93
Inhaled drug deposition in the airways is impacted by the patient’s inspiratory flow, the aerosol velocity, and the inhaled drug particle size.Citation63–Citation65 These challenges can be particularly evident in young children and older individuals, and, in addition to the difficulties these groups can have with coordination of device actuation with inspiration,Citation37 may lead to a significant reduction in drug deposition in the lungs. The CRITical Inhaler mistaKes and Asthma controL study (CRITIKAL)Citation11 is one of the largest studies to investigate inhaler technique. Conducted in a real-life, multinational study population, this study investigated the association between specific inhaler errors and asthma outcomes, and included data from 3,660 patients. Insufficient inspiratory effort was common (made by 32%–38% of DPI users), and was associated with uncontrolled asthma (adjusted odds ratios: 1.30 and 1.56 in those using Turbuhaler and Diskus devices, respectively) and increased exacerbation rate. In pMDI users, actuation before inhalation (24.9% of patients) was also associated with uncontrolled asthma.
Patient factors including preferences and satisfaction can play a significant role in inhaler choice and use.Citation19 In addition to ease of use, this can be influenced by the portability and compact design of the device, as well as noise, taste, treatment time, and convenience.Citation44 Engaging patients in selection of the inhaler that suits them best may help optimize device adherence. In a real-world observational study, Small et alCitation66 reported that the higher the level of satisfaction patients had with their device, the more likely they were to be compliant and to experience better outcomes (eg, quality of life and fewer health care challenges), including fewer exacerbations, fewer hospital visits, fewer health care visits, and fewer sleep disturbances. In one study in which patients were interviewed to determine their inhaler preferences, it was confirmed that smaller-sized inhalers are desirable due to their portability, and interviewees stated that this characteristic is linked to adherence.Citation67 In addition, most participants believed that a dose counter should be an integral part of an inhaler, while the need for proper training with a health care professional was also emphasized.Citation67 Patient preference for different inhaler types has been investigated in many studies. Given the wide selection of inhalers available, patient preference for one particular inhaler type has not been demonstrated, and the choice depends on a number of factors, as already discussed.Citation20,Citation47,Citation68–Citation72
Training and education to support the use of inhalers
Inhaler misuse is one of the most commonly reported barriers to adherence. Melani et alCitation15 observed the strongest and most significant associations between inhaler misuse with older age, lower schooling, and lack of instruction regarding inhaler technique. It must be acknowledged that even the most user-friendly devices still require education and a demonstration, which has been shown to be lacking in several studies.
Education is the one factor that is modifiable, and health care professionals should seek to tailor advice according to individual patient needs in addition to ensuring that their own education is up to date.Citation7 On the introduction of a device into clinical practice, the suggestion that it is user-friendly gives the impression that education and training may not be required. However, a patient will require training and upskilling on any device,Citation15,Citation52 and user technique should always be reviewed in patients with poor asthma control, even if they are using a device that is considered easy to use.Citation56 However, while training can enhance the ability to use inhalers, it has been reported that many patients revert to an incorrect technique after a short time.Citation73,Citation74 The Global Initiative for Asthma (GINA) recommends strategies for helping to ensure effective device use, including a physical demonstration of inhaler technique and patient retraining at follow-up appointments.Citation10 A Cochrane review evaluated a range of interventions and determined that although many studies demonstrated a post-intervention improvement in the number of individuals with correct inhaler technique, it could not be confirmed whether this translated into clinical benefits.Citation51 The authors recommended that health care professionals continue to ask their patients to regularly demonstrate their technique and correct this as required, and to refer patients for training as necessary where available.
Patient-related education
The most effective patient training technique has been established as verbal instruction combined with a physical demonstration.Citation75–Citation77 Repeating information over time increases the proportion of patients who maintain the correct technique at follow-up visits.Citation77 If poor technique persists, it is essential to elucidate from the patient the challenges they are experiencing, and address any potential lack of understanding around the need for medication and adherence.Citation7 Furthermore, treatment decisions should always be taken in collaboration with the patient and/or their carer in the case of young patients and often elderly individuals.Citation7 A selection of educational aids has been developed and are reviewed elsewhere.Citation74 In an attempt to improve patient recall of the optimal technique required for use, some device tools provide real-time, interactive sensory feedback of the patient’s performance in various aspects of inhalation.Citation74 A number of online tools, including videos, also offer patient support, and the Aerosol Drug Management Improvement Team (ADMIT)Citation74 provide an online platform offering patients and health care professional educational resources to support the decision-making process regarding which inhaler might be most appropriate and the correct inhaler technique.
Health care professional-related education
The role of the health care professional, whether physician, pharmacist, or other member of the MDT, in inhaler use is central.Citation7,Citation52 The wide range of drug and inhaler combinations increases the complexity of inhaler choice for physicians, and may also reduce their experience with each device, hence affecting patient tuition. It has been suggested that up to 67% of clinicians cannot describe the steps involved or demonstrate correct inhaler use.Citation51 It is recommended that each health care professional should look to expand their knowledge on inhalation devices and strategies to support their patients, enabling them to offer tailored care that aims to maximize disease control and patient experience while minimizing clinic visits.Citation7,Citation77
When considering pediatric patients specifically, a UK-based study evaluated whether health care professionals were able to counsel this group on use of inhalers, including MDIs and Turbuhaler. Findings were similar to those observed with adults, and concluded that less than 10% of health care professionals were competent with the MDI device. Overall, just 13% of participants provided counseling on all the essential criteria for an MDI inhaler. Pharmacy teams within the hospital and community saw the highest competency levels, with 31% and 30% of staff able to discuss the essential steps, respectively. The physicians or nurses included were not able to identify all the necessary steps. Furthermore, only 10% of participants counseled patients on all essential steps for an MDI with a spacer device, with no nurse or doctor achieving all steps.Citation78 Commonly omitted steps included shaking the inhaler and leaving sufficient time between doses.
An improvement in inhaler knowledge and skills has been reported following educational workshops and a small-group lecture format with web-based inhaler tutorials.Citation21 Leung et alCitation79 tested the usefulness of a physician education implemented as a two-session education program. Attendees were armed with slide decks and access to placebo inhalers so that they could not only teach patients proper inhaler technique, but also raise awareness among other members of the MDT. Before the program, 49% of participants reported providing some form of inhaler teaching in their practices, yet only 10% felt fully competent to teach their patients the inhaler technique. After the program, 98% rated their inhaler teaching as good to excellent, and 83% reported providing inhaler teaching in their practices, either by themselves or by a member of the MDT that they had personally trained. In another study,Citation80 health care professionals watched tablet-based multimedia educational videos that demonstrated correct inhaler technique by a clinical pharmacist with teach-back from a patient, before being re-evaluated. Correct inhaler technique was significantly increased among all health care professionals after the training, with the largest increase observed for the Respimat® device; 32% versus 93% demonstrated the correct steps for usage before and after training.
Research has shown that it is necessary to repeat instructions several times to achieve effective inhalation skills in both asthma and COPD patients. A study by Takaku et alCitation81 designed to evaluate the number of instructions that are necessary to minimize errors in using pMDI, DPI, and Respimat® concluded that, for every device, at least three instructions were required to achieve less than 10% of errors. As a support strategy to providing verbal instructions, Basheti et alCitation82 investigated the effect of the use of inhaler technique reminder labels. Findings demonstrated significantly better inhaler technique after 3 months among those using labels compared with those using initial training alone. The personalized labels highlighted original errors, serving as a reminder of the correct technique; 67% of patients maintained correct technique at follow-up, compared with only 12% of those who received education alone. It was concluded that this is a simple intervention that has the potential to support continued good inhaler technique among patients. Furthermore, the labeling might also help health care professionals with providing instruction during a consultation. The authors also suggested that future research could investigate the potential for inhalers to talk the patient through the steps needed for good medication delivery.
There are many guidelines (eg, GINA and Global Initiative for Chronic Obstructive Lung Disease) to support health care professionals. The UK Inhaler Group have published the “Inhaler Standards and Competency Document”, which provides guidance and recommends that health care professionals are able to demonstrate device use effectively. Furthermore, it has been recommended that health care professionals limit the range of devices they use by balancing the patient’s needs and preferences with prescribing devices that they feel confident explaining.Citation83 Finally, health care professionals should consider the most effective educational tool according to the patient’s needs; for example, younger patients may benefit more from multimedia teaching methods, whereas elderly patients respond well to one-to-one tuition.Citation73
An update on new inhalational therapeutics
Over the past 5–10 years, a number of technological innovations have been introduced that improve the performance of all device types; in addition, new delivery systems have been developed that improve delivery efficacy. Amongst these are “intelligent inhalers”, which carry features to monitor patients’ inhalation and adherence to treatment. Using new technology, pulmonary disposition fractions have been increased up to 40%–50% of the nominal dose compared with 10%–15% of levels achieved in the past, meaning that less drug is required for similar efficacy.Citation8 Other innovations (reviewed in more detail by Lavorini et alCitation8) include the insertion of microprocessors into pMDIs, novel ways of initiating breath actuation (including the analysis of inspiratory flow profiles), electronic dose counters, heating elements to reduce aerosol droplet size, and mechanisms that give visual and acoustic feedback to reassure patients that their medication has been taken correctly.
Future developments in inhaler management
Many inhalation products have reached or are approaching patent expiration, leading to a worldwide trend of switching from branded to generic inhalation medicine and the development of new generic inhalers. In the light of this, the European Medicines Agency issued stringent guidelines in 2009 recommending a stepwise approach to demonstrate therapeutic equivalence between two inhaled products. The guidelines stipulate that the generic and reference products must have an identical dosage form containing the same active substance(s). Devices containing generic and reference substances should be equivalent in terms of handling and resistance to airflow, and the delivered dose and particle size should be similar (within 15%) between products. If these in vitro criteria are satisfied, the product may be approved without further pharmacokinetic or pharmacodynamic studies to demonstrate equivalence. The FDA has taken a different approach, and has issued separate draft guidance for each specific inhalation product (pMDIs of albuterol sulfate, ipratropium bromide, lev-albuterol tartrate, budesonide/formoterol fumarate, and DPI of fluticasone propionate/salmeterol). To get FDA approval for a generic product, in vitro tests and in vivo equivalence studies are required, making it much harder to get approval.Citation84
Digital health is a growing phenomenon, and offers the potential to help optimize patient care in several aspects of asthma management.Citation85 A selection of the digital and electronic options either available or under investigation are reviewed in detail elsewhere.Citation86,Citation87 Briefly, one digital platform that has FDA approval (Propeller Health) aims to provide geospatial information on asthma attacks to help health care professionals identify exacerbation triggers. In addition, weekly email reports are considered to help increase disease awareness, as well as to enhance understanding of treatment and preventative measures.Citation86 The approach, based on the global positioning system functionality of smartphones and available for the three main device types – pMDI, DPI, and Respimat® – features sensor technology, software, and services; remotely monitors use of inhaled asthma and COPD treatment; analyses patient trends; and provides regular feedback. As technology in this area progresses, it is likely that many additional options to support inhaler use in asthma and COPD will become available. There is also a lot of work in the innovation of inhaler formulations,Citation88 their engineered design,Citation8 and also the aerosol formCitation89 in order to make inhalers more efficient in their ability to deliver drug to the lungs.
In conclusion, there are a broad range of inhaler devices available for the management of asthma and COPD. Each has varying technical features, and so it is important that the choice of device is tailored to meet individual patient’s needs, preferences, and satisfaction, while offering the requisite level of disease control. While there may be no one ideal device for all patients, the range of options available means that there should be a device to suit every patient. Education, both for patients and physicians, is also a key component of optimizing device choice and use.
Acknowledgments
The author would like to thank Kjeld Hansen, a member of the Patient Ambassador Group for the European Lung Foundation, for his input to the video summary for this manuscript. Louise Brady, PhD, from MediTech Media has provided medical writing assistance, funded by Boehringer Ingelheim.
Disclosure
OSU has received industry–academic funding from Boehringer Ingelheim, Chiesi, Edmond Pharma, GlaxoSmithKline, and Mundipharma International, and has received consultancy or speaker fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Edmond Pharma, GlaxoSmithKline, Mundipharma International, Napp, Novartis, Pearl Therapeutics, Roche, Sandoz, Takeda, UCB, Vectura, and Zentiva. The author reports no other conflicts of interest in this work.
References
- LewisATorvinenSDekhuijzenPNThe economic burden of asthma and chronic obstructive pulmonary disease and the impact of poor inhalation technique with commonly prescribed dry powder inhalers in three European countriesBMC Health Serv Res20161625127406133
- Asthma UKAsthma facts and statistics Available from: https://www.asthma.org.uk/about/media/facts-and-statistics/Accessed February 12, 2018
- World Health OrganizationChronic respiratory diseases Available from: http://www.who.int/respiratory/en/Accessed October 26, 2017
- SteinSWThielCGThe history of therapeutic aerosols: a chronological reviewJ Aerosol Med Pulm Drug Deliv2017301204127748638
- LavoriniFCorriganCJBarnesPJAerosol Drug Management Improvement TeamRetail sales of inhalation devices in European countries: so much for a global policyRespir Med201110571099110321489771
- RoguedaPTrainiDThe future of inhalers: how can we improve drug delivery in asthma and COPD?Expert Rev Respir Med201610101041104427545190
- BraidoFChrystynHBaiardiniIRespiratory Effectiveness Group“Trying, but failing” – the role of inhaler technique and mode of delivery in respiratory medication adherenceJ Allergy Clin Immunol Pract20164582383227587316
- LavoriniFFontanaGAUsmaniOSNew inhaler devices – the good, the bad and the uglyRespiration201488131524902629
- Dudvarski IlicAZugicVZvezdinBInfluence of inhaler technique on asthma and COPD control: a multicenter experienceInt J Chron Obstruct Pulmon Dis2016112509251727785007
- Global Initiative for AsthmaGINA Report: Global Strategy for Asthma Management and Prevention Available from: http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention/Accessed August 1, 2017
- PriceDBRomán-RodríguezMMcQueenRBInhaler errors in the CRITIKAL study: type, frequency, and association with asthma outcomesJ Allergy Clin Immunol Pract2017541071108128286157
- BrandstetterSFingerTFischerWDifferences in medication adherence are associated with beliefs about medicines in asthma and COPDClin Transl Allergy201773929152167
- VestboJAndersonJACalverleyPMAdherence to inhaled therapy, mortality and hospital admission in COPDThorax2009641193994319703830
- SulaimanICushenBGreeneGObjective assessment of adherence to inhalers by patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2017195101333134327409253
- MelaniASBonaviaMCilentiVGruppo Educazionale Associ-azione Italiana Pneumologi OspedalieriInhaler mishandling remains common in real life and is associated with reduced disease controlRespir Med2011105693093821367593
- MolimardMRaherisonCLignotSChronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patientsEur Respir J2017492160179428182569
- UsmaniOSLavoriniFMarshallJCritical inhaler errors in asthma and COPD: a systematic review of impact on health outcomesRespir Res20181911029338792
- PressVGAroraVMShahLMTeaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trialJ Gen Intern Med201227101317132522592354
- DekhuijzenPNLavoriniFUsmaniOSPatients’ perspectives and preferences in the choice of inhalers: the case for Respimat(®) or HandiHaler(®)Patient Prefer Adherence2016101561157227574405
- ChorãoPPereiraAMFonsecaJAInhaler devices in asthma and COPD – an assessment of inhaler technique and patient preferencesRespir Med2014108796897524873873
- Inhaler Error Steering CommitteePriceDBosnic-AnticevichSInhaler competence in asthma: common errors, barriers to use and recommended solutionsRespir Med20131071374623098685
- BoniniMUsmaniOSThe importance of inhaler devices in the treatment of COPDCOPD Res Pract2015119
- Bosnic-AnticevichSChrystynHCostelloRWThe use of multiple respiratory inhalers requiring different inhalation techniques has an adverse effect on COPD outcomesInt J Chron Obstruct Pulmon Dis201612597128053517
- PriceDBColiceGIsraelEAdd-on LABA in a separate inhaler as asthma step-up therapy versus increased dose of ICS or ICS/LABA combination inhalerERJ Open Res2016220010627730200
- LavoriniFUsmaniOSCorrect inhalation technique is critical in achieving good asthma controlPrim Care Respir J201322438538624270367
- TaffetGEDonohueJFAltmanPRConsiderations for managing chronic obstructive pulmonary disease in the elderlyClin Interv Aging20149233024376347
- YawnBPColiceGLHodderRPractical aspects of inhaler use in the management of chronic obstructive pulmonary disease in the primary care settingInt J Chron Obstruct Pulmon Dis2012749550222888221
- WachtelHKattenbeckSDunneSThe Respimat(®) development story: patient-centered innovationPulm Ther2017319
- BowlesSKSketrisIKephartGDrug Evaluation Alliance of Nova ScotiaUse of wet nebulized inhaled respiratory medications under criteria-based reimbursement guidelines in a publicly funded Seniors’ Pharmacare Program in Nova Scotia, CanadaAm J Geriatr Pharmacother20075212012817719514
- CatesCJWelshEJRoweBHHolding chambers (spacers) versus nebulisers for beta-agonist treatment of acute asthmaCochrane Database Syst Rev20139CD000052
- LohCHPetersSPLovingsTMOharJASuboptimal inspiratory flow rates are associated with chronic obstructive pulmonary disease and all cause readmissionsAnn Am Thorac Soc20171481305131128406710
- BusinessWireSunovion Receives FDA Approval for Lonhala™ Magnair™ Inhalation Solution to Treat COPD Available from: https://www.businesswire.com/news/home/20171205006502/en/Sunovion-Receives-FDA-Approval-Lonhala%E2%84%A2-Magnair%E2%84%A2-InhalationAccessed February, 2018
- UsmaniOSTreating the small airwaysRespiration201284644145323154684
- SonnappaSMcQueenBPostmaDSExtrafine versus fine inhaled corticosteroids in relation to asthma control: a systematic review and meta-analysis of observational real-life studiesJ Allergy Clin Immunol Pract Epub2017920
- SonnappaSMartinRIsraelERespiratory Effectiveness Group, Small Airways Study GroupRisk of pneumonia in obstructive lung disease: a real-life study comparing extra-fine and fine-particle inhaled corticosteroidsPLoS One2017126e017811228617814
- LevyMLDekhuijzenPNBarnesPJInhaler technique: facts and fantasies. A view from the Aerosol Drug Management Improvement Team (ADMIT)NPJ Prim Care Respir Med2016261601727098045
- DalbyRNEicherJZierenbergBDevelopment of Respimat(®) Soft Mist™ inhaler and its clinical utility in respiratory disordersMed Devices (Auckl)2011414515522915941
- LavoriniFPistolesiMUsmaniOSRecent advances in capsule-based dry powder inhaler technologyMultidiscip Respir Med2017121128536654
- MuralidharanPHayesDJrMansourHMDry powder inhalers in COPD, lung inflammation and pulmonary infectionsExpert Opin Drug Deliv201512694796225388926
- RauJLPractical problems with aerosol therapy in COPDRespir Care200651215817216441960
- Al-ShowairRATarsinWYAssiKHPearsonSBChrystynHCan all patients with COPD use the correct inhalation flow with all inhalers and does training help?Respir Med2007101112395240117629471
- BorgströmLAskingLLipniunasPAn in vivo and in vitro comparison of two powder inhalers following storage at hot/humid conditionsJ Aerosol Med200518330431016181005
- GandertonDTargeted delivery of inhaled drugs: current challenges and future goalsJ Aerosol Med199912Suppl 1S3S810623339
- Moroni-ZentgrafPImpact of patient needs on design and usage of an inhalation device in respiratory medicineRespir Drug Deliv20131141
- AndersonPUse of Respimat Soft Mist inhaler in COPD patientsInt J Chron Obstruct Pulmon Dis20061325125918046862
- Dal NegroRWLongoPZianiOVBonadimanLTurcoPInstant velocity and consistency of emitted cloud change by the different levels of canister filling with Metered Dose Inhalers (MDIs), but not with Soft Mist Inhalers (SMIs): a bench studyMultidiscip Respir Med2017121328560037
- Dal NegroRWPoveroMAcceptability and preference of three inhalation devices assessed by the Handling Questionnaire in asthma and COPD patientsMultidiscip Respir Med201611726865979
- BrandPHedererBAustenGDewberryHMeyerTHigher lung deposition with Respimat Soft Mist inhaler than HFA-MDI in COPD patients with poor techniqueInt J Chron Obstruct Pulmon Dis20083476377019281091
- PedersenSDubusJCCromptonGKADMIT Working GroupThe ADMIT series – issues in inhalation therapy. 5) Inhaler selection in children with asthmaPrim Care Respir J201019320921620640390
- VinckenWDekhuijzenPRBarnesPADMIT GroupThe ADMIT series – issues in inhalation therapy. 4) How to choose inhaler devices for the treatment of COPDPrim Care Respir J2010191102019890594
- NormansellRKewKMMathioudakisAGInterventions to improve inhaler technique for people with asthmaCochrane Database Syst Rev20173CD01228628288272
- FinkJBRubinBKProblems with inhaler use: a call for improved clinician and patient educationRespir Care2005501013741375
- AriAFinkJBGuidelines for aerosol devices in infants, children and adults: which to choose, why and how to achieve effective aerosol therapyExpert Rev Respir Med20115456157221859275
- MelaniASBracciLSRossiMReduced peak inspiratory effort through the Diskus(®) and the Turbuhaler(®) due to mishandling is common in clinical practiceClin Drug Investig2005258543549
- KaminWFrankMKattenbeckSMoroni-ZentgrafPWachtelHZielenSA handling study to assess use of the Respimat(®) Soft Mist™ inhaler in children under 5 years oldJ Aerosol Med Pulm Drug Deliv201528537238125844687
- WesterikJACarterVChrystynHCharacteristics of patients making serious inhaler errors with a dry powder inhaler and association with asthma-related events in a primary care settingJ Asthma201653332132926810934
- LevyMLHardwellAMcKnightEHolmesJAsthma patients’ inability to use a pressurised metered-dose inhaler (pMDI) correctly correlates with poor asthma control as defined by the global initiative for asthma (GINA) strategy: a retrospective analysisPrim Care Respir J201322440641124042172
- HodderRPriceDPatient preferences for inhaler devices in chronic obstructive pulmonary disease: experience with Respimat Soft Mist inhalerInt J Chron Obstruct Pulmon Dis2009438139019888356
- PerrielloEASobierajDMThe Respimat Soft Mist inhaler, a novel inhaled drug delivery deviceConn Med201680635936427509644
- DarbàJRamírezGSicrasAFrancoliPTorvinenSSánchez-de la RosaRThe importance of inhaler devices: the choice of inhaler device may lead to suboptimal adherence in COPD patientsInt J Chron Obstruct Pulmon Dis2015102335234526604733
- UsmaniOSSmall-airway disease in asthma: pharmacological considerationsCurr Opin Pulm Med2015211556725415404
- ScichiloneNAsthma control: the right inhaler for the right patientAdv Ther201532428529225845769
- VerbanckSGhorbaniaslGBiddiscombeMFInhaled aerosol distribution in human airways: a scintigraphy-guided study in a 3D printed modelJ Aerosol Med Pulm Drug Deliv201629652553327337643
- VerbanckSKalsiHSBiddiscombeMFInspiratory and expiratory aerosol deposition in the upper airwayInhal Toxicol201123210411121309663
- UsmaniOSBiddiscombeMFBarnesPJRegional lung deposition and bronchodilator response as a function of beta2-agonist particle sizeAm J Respir Crit Care Med2005172121497150416192448
- SmallMAndersonPVickersAKaySFermerSImportance of inhaler-device satisfaction in asthma treatment: real-world observations of physician-observed compliance and clinical/patient-reported outcomesAdv Ther201128320221221331556
- JahediLDownieSRSainiBChanHKBosnic-AnticevichSInhaler technique in asthma: how does it relate to patients’ preferences and attitudes toward their inhalers?J Aerosol Med Pulm Drug Deliv2017301425227676193
- MiravitllesMMontero-CaballeroJRichardFA cross-sectional study to assess inhalation device handling and patient satisfaction in COPDInt J Chron Obstruct Pulmon Dis20161140741527013871
- SchürmannWSchmidtmannSMoroniPMasseyDQidanMRespimat Soft Mist inhaler versus hydrofluoroalkane metered dose inhaler: patient preference and satisfactionTreat Respir Med200541536115725050
- HodderRReesePRSlatonTAsthma patients prefer Respimat Soft Mist Inhaler to TurbuhalerInt J Chron Obstruct Pulmon Dis2009422523219554196
- LenneyJInnesJACromptonGKInappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. EDICIRespir Med200094549650010868714
- MolimardMColthorpePInhaler devices for chronic obstructive pulmonary disease: insights from patients and healthcare practitionersJ Aerosol Med Pulm Drug Deliv201528321922825265316
- CromptonGKBarnesPJBroedersMAerosol Drug Management Improvement TeamThe need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement TeamRespir Med200610091479149416495040
- LavoriniFLevyMLCorriganCCromptonGADMIT Working GroupThe ADMIT series – issues in inhalation therapy. 6) Training tools for inhalation devicesPrim Care Respir J201019433534121049263
- MelaniASZanchettaDBarbatoNAssociazione Italiana Pneumologi Ospedalieri Educational GroupInhalation technique and variables associated with misuse of conventional metered-dose inhalers and newer dry powder inhalers in experienced adultsAnn Allergy Asthma Immunol200493543944615562882
- BashetiIAReddelHKArmourCLBosnic-AnticevichSZCounseling about turbuhaler technique: needs assessment and effective strategies for community pharmacistsRespir Care200550561762315871755
- Bosnic-AnticevichSZSinhaHSoSReddelHKMetered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over timeJ Asthma201047325125620394511
- GoodwinRChanderTShahNTomlinSInhaler counselling, the real deal or just fresh air?Arch Dis Child20161019e2
- LeungJBhutaniMLeighRPelletierDGoodCSinDDEmpowering family physicians to impart proper inhaler teaching to patients with chronic obstructive pulmonary disease and asthmaCan Respir J201522526627026436910
- MulhallAMZafarMARecordSChannellHPanosRJA tablet-based multimedia education tool improves provider and subject knowledge of inhaler use techniquesRespir Care201762216317128108685
- TakakuYKurashimaKOhtaCHow many instructions are required to correct inhalation errors in patients with asthma and chronic obstructive pulmonary disease?Respir Med201712311011528137486
- BashetiIAObeidatNMReddelHKEffect of novel inhaler technique reminder labels on the retention of inhaler technique skills in asthma: a single-blind randomized controlled trialNPJ Prim Care Respir Med2017271928184045
- GoodwinRHeraghtyJDo healthcare professionals understand asthma devices?Arch Dis Child Educ Pract Ed2015100630230526407731
- HouSWuJLiXShuHPractical, regulatory and clinical considerations for development of inhalation drug productsAsian J Pharm Sci201510490500
- SimpsonAJHonkoopPJKenningtonEPerspectives of patients and healthcare professionals on mHealth for asthma self-managementEur Respir J2017495160196628461291
- KikidisDKonstantinosVTzovarasDUsmaniOSThe digital asthma patient: the history and future of inhaler based health monitoring devicesJ Aerosol Med Pulm Drug Deliv201629321923226919553
- CarpenterDMRobertsCASageAJGeorgeJHorneRA review of electronic devices to assess inhaler techniqueCurr Allergy Asthma Rep20171731728290015
- UsmaniOSNew developments in inhaled drugs: within and beyond the lungsRespiration20148811224801444
- BiddiscombeMFUsmaniOSBarnesPJA system for the production and delivery of monodisperse salbutamol aerosols to the lungsInt J Pharm2003254224325312623200
- BerlinskiAPediatric aerosol therapyRespir Care201762666267728546371
- HamelmannESzeflerSJEfficacy and safety of tiotropium in children and adolescentsDrugs201878332733829368127
- BarronsRWheelerJWoodsJAOpportunities for inhaler device selection in elderly patients with asthma or COPDPatient Intelligence201575365
- ScichiloneNBraidoFLavoriniFLevyMLUsmaniOSRoutine use of budesonide/formoterol fixed dose combination in elderly asthmatic patients: practical considerationsDrugs Aging201734532133028258535
