Abstract
Introduction
Renal cell carcinoma (RCC) is one of the most lethal urological malignancies, and surgeries remain the mainstay for localized RCC. This study aimed to compare the selection of open surgery and minimally invasive kidney surgery for RCCs for the aspects of complication, medical costs, and patient preference.
Materials and methods
We conducted a population-based case–control study by using the National Health Insurance Research Database of Taiwan, which included data from 23 million Taiwanese residents. Patients newly diagnosed with RCC during 2006–2012 were included. We compared the general characteristics, underlying disease, complications, hospital stay, postoperative analgesic dosage, and medical costs between open group and minimally invasive group.
Results
A total of 3,172 patients who received radical nephrectomy (RN) or partial nephrectomy (PN) for RCC were included. The mean age was 61.1 years, with a male to female ratio of 1.88. In the minimally invasive groups, the mean hospital stay was significantly shorter than in open groups (12.4 days in open RN versus 10.3 days in minimally invasive RN, and 9.7 days in open PN versus 8.2 days in minimally invasive PN). There was no significant difference between the medical costs and the incidence of major bleeding complication between the open group and the minimally invasive group. Female patients and patients with higher monthly income were more likely to receive minimally invasive surgery.
Conclusion
During past decades, open RN has gradually been replaced by minimally invasive surgeries and PN. Compared to open surgeries, minimally invasive surgeries could lead to less postoperative pain and faster recovery. Economic status of the patients potentially hinders them from receiving minimally invasive surgeries, which may cost more.
Introduction
Renal cell carcinoma (RCC) is one of the most lethal urological malignancies. The 5-year relative survival rate of RCC patients was about 71%, compared to 78% for bladder urothelial cell carcinoma (excluding carcinoma in situ) and 99% for prostate cancer.Citation1
The incidence of RCC is about 12 per 100,000 population per year, with a male to female ratio 1.5.Citation1 RCC is a disease of aging people, with higher prevalence among those aged between 50 and 70 years.Citation1–Citation3 The incidence has increased in recent decades by an average of 3%–4% per year, and this trend was largely related to the increased prevalence of imaging survey techniques, such as ultrasonography or computed tomography scan, for the evaluation of all cause of abdominal problems.Citation4,Citation5
With the wide use of cross-sectional imaging, RCC is more often diagnosed at early stage as localized disease.Citation6–Citation8 The management of localized RCC includes radical nephrectomy (RN), partial nephrectomy (PN), thermal ablation, and active surveillance.Citation9–Citation14 Among the variety of treatment modalities, surgery remains the mainstay for curative treatment of this disease.
The goal of surgery for RCC is to excise all tumors with adequate preservation of surgical margin. RN is the preferred option for many patients with localized RCC, such as those with very large tumors (most clinical T2 tumors) or the relatively limited subgroup of patients with clinical T1 tumors whose tumor are not amenable to nephron-sparing approaches.Citation15 Compared to RN, PN is the preferred choice for renal function preservation in selected feasible patients, especially for those with chronic kidney disease.Citation10,Citation15–Citation17
Although effective, traditional open surgeries to the kidney are associated with significant postoperative discomfort and longer recovery period. Compared with open renal surgery, minimally invasive surgery which is laparoscopic-assisted resulted in less change in muscle volume and a lower rate of flank bulge, paresthesias, and numbness postoperatively.Citation18
In this study, we used a nationwide health insurance database to compare the open surgery and minimally invasive kidney surgery for RCCs for the aspects of complication, medical costs, and patient preference.
Materials and methods
Data sources
We conducted a population-based case–control study by using the National Health Insurance (NHI) Research Database (NHIRD) of Taiwan. The database contained data from the state-run NHI program, which was established in 1995 and provides universal health care for 23 million Taiwanese residents.Citation19 The current health care system in Taiwan, known as NHI, was instituted in 1995. NHI is a single-payer compulsory social insurance plan which centralizes the disbursement of health care funds. The system promises equal access to health care for all citizens, and the population coverage had reached 99% by the end of 2004. NHI is mainly financed through premiums, which are based on the payroll tax, and is supplemented with out-of-pocket payments and direct government funding. This study was approved by the Institutional Review Board of Chang-Gung Memorial Hospital (IRB), approval number 104-7905B. All patient data from NHIRD are anonymized; therefore the board did not require informed consent from the patients for this study.
Study population
In this study, patients newly diagnosed with malignant neoplasm of the kidney, except that in the pelvis (renal cancer; International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] 189.0), during the period from 2006 to 2012 were identified from the Registry for Catastrophic Illness Patient database. The insurance coverage for catastrophic illnesses is an extension of the NHI program of Taiwan for protecting people with serious diseases from the financial burden. Renal cancer is an NHI-defined catastrophic illness, and the NHI program covers the costs incurred during treatment of the disease. Patients who underwent radical or PN for pathologically confirmed RCC were included. Types of surgeries were as open or minimally invasive surgeries. Minimally invasive surgeries included hand-assisted/pure laparoscopic or retroperitoneoscopic surgeries.
Statistical analyses
We compared demographic characteristics, namely, gender, age, monthly income, underlying disease, and geographical location and urbanization level of the area of residence; and bleeding-related complications, hospital stay, postoperative analgesic dosage, and medical costs between the open surgery group and minimally invasive group.
Monthly income was identified according to insured amount of NHI, categorized as NTD$20,000 (694 USD) and NTD$40,000 NT (1,388 USD) (NTD$ represents New Taiwan dollar). Bleeding relate complications were defined by perioperative or postoperative blood transfusion or receiving angiography with embolization during admission or 1 month after discharge from the hospital. Postoperative analgesic dosage was assessed with total postoperative dosage of opioid analgesic consumption.
The patients were then divided into 4 groups: open RN, minimally invasive RN (including laparoscopic and retroperitoneoscopic), open PN, and minimally invasive PN (including laparoscopic and retroperitoneoscopic). Comparison of open surgery and minimally invasive surgery was performed in RN and PN groups.
The associations between nominal variables were examined using the χ2 test and that between the continuous variables using independent t-test.
Results
A total of 3,172 patients were included, and all of them were diagnosed as having RCC and underwent either radical or PN for tumor excision. The mean age was 61.1 years old, with a male to female ratio of 1.88. The mean stay in the hospital for renal surgery was 11.3 days, and medical costs was 102,186 NTD (3,546.9 USD). All the other detailed general characteristics are listed in .
Table 1 General characteristics of all patients
The results of comparison between different surgery groups are shown in .
Table 2 Subgroup analysis between 4 groups divided by type of surgery
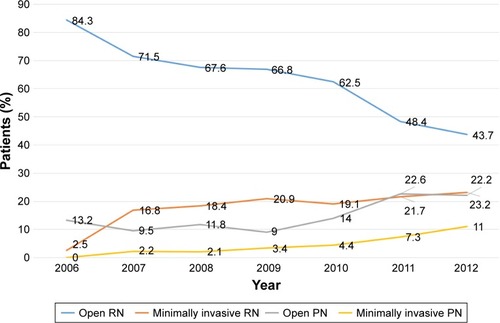
The percentage of open RN, minimally invasive RN, open PN, and minimally invasive PN are shown from 2006 to 2012 (). The number of open RN performed decreased gradually, with minimally invasive RN, open PN, and minimally invasive PN counts increasing year by year.
Figure 1 The change in the trend of surgery type for RCC in Taiwan from 2006 to 2012.
The average age of patients between open RN/minimally invasive RN, and open PN/minimally invasive PN was 58.9, 60.3, 57.4, and 56.9 years old, respectively. The male to female ratio was around 1.5–2.2 in all 4 groups. If RN or PN was required, the percentage of patients who received minimally invasive surgeries among male and female groups were 23.94% and 28.13%, respectively, with a significantly higher proportion of females choosing for this option (p=0.0104). In patients with monthly income more than $NT 40,000 (1,388 USD), surgery was more likely minimally invasive when compared to patients of lower economic status.
In patients who received RN, open group patients had significant longer hospital stay compared to those who underwent minimally invasive surgery (12.4±8.8 days versus 10.3±6.7 days, p-value <0.0001). A similar result was also seen in PN patients, with hospital stay duration of 9.7±5.7 days in open group versus 8.2±5.3 days in minimally invasive group (p-value =0.0031).
There was no significant difference between the medical costs when comparing open group and minimally invasive group, and neither was there a difference when comparing RN and PN groups.
In , we demonstrated the occurrence of bleeding-related complications and opioid analgesic demand, comparing the values between the open and minimally invasive groups.
Table 3 Bleeding-related complications and opioid analgesics consumption in all 4 groups
Bleeding-related complications were defined by peri-operative or postoperative blood transfusion or receiving angiography with embolization during admission or 1 month after discharge from the hospital. The incidence of blood transfusion and angiography with embolization were separately listed.
In the RN group, the patients receiving open surgery had significantly higher bleeding-related complication than those in the minimally invasive group. However, there was no significant difference between patients who received open and minimally invasive PN.
The postoperative opioid analgesics demand was calculated by total dosage (mg/mL). In the RN group, patients receiving open surgeries significantly required more opioid analgesics than patients receiving minimally invasive surgery (87.6±120 mg/mL versus 55.3±89 mg/mL, p-value <0.0001). However, in patients receiving PN, open group and minimally invasive group had similar opioid analgesics demand (49.9±65 mg/mL versus 48±65 mg/mL, p-value =0.8334).
Discussion
For localized RCC, the efficacy and durability of operative extirpation had been demonstrated to be central to cure. However, studies also have shown that many patients can have permanent unfavorable body shape alterations with flank incisions resulting in significantly larger postoperative surface area and volume changes on the operated flank compared with the uninvolved flank. The dissatisfaction with regard to the body changes occurred in up to 60% of flank incisions, with a patient preference toward minimally invasive techniques.Citation20–Citation22
In addition to less body image change, minimally invasive surgery also results in minimal postoperative discomfort, a brief hospital stay, and a rapid recovery. Besides cosmetic and recovery advantage compared to open surgery, minimally invasive surgeries have been demonstrated to have equivalent functional and oncological outcomes.Citation23–Citation26 With experience, all manner of laparoscopic renal surgeries are now routinely accomplished without compromise on surgical outcomes.
In our study, we used a nationwide, single-payer health insurance system, which covered 99% of about 23 million Taiwanese residents, to analyze the difference between open and minimally invasive surgeries for RCCs.
The average length of hospital stay of patients receiving minimally invasive surgeries was significantly shorter than those in the open surgery groups, with a difference of 2.1 days and 1.5 days in RN and PN group, respectively. The postoperative opioid analgesics demand was also significantly lower in open RN group than in minimally invasive RN group. This confirmed the result of previous studies regarding the faster recovery and better postoperative discomfort.Citation23,Citation27,Citation28
Even with shorter hospital stay in minimally invasive group patients, the medical costs were similar in minimally invasive group and open group. However, the medical costs gathered from the Taiwan NHIRD are probably not the real total medical costs. The NHI covers most of the medical costs, except some expanse which was considered unnecessary for the treatment. Referring to laparoscopic RN or PN, medical instruments such as the GelPort Laparoscopic System manufactured by the Applied Medical Resources Corporation (Rancho Santa Margarita, CA, USA) or the Harmonic scalpel manufactured by Ethicon Endo-Surgery (Somerville, NJ, USA), etc, were considered unnecessary, although surgeons would consider those instruments helpful while performing minimally invasive renal surgeries in selected cases.
In this circumstance, a significant amount of the medical costs could be unrevealed in the study. Instead, the unrevealed medical costs were covered by the private medical insurance companies or the patients themselves. Overall, the medical expenditure paid by the patients is higher with minimally invasive surgery than with open surgery for RCC. This could also explain the trend why people with higher economic status would prefer to receive minimally invasive surgeries for RCC.
In RN group, patients receiving open surgery required more perioperative or postoperative blood transfusion than patients receiving minimally invasive surgery. However, the incidence of angiography with embolization after operation was similar in these 2 groups. The result could be explained that the overall major bleeding complications requiring angiography with embolization is similar in open surgery and minimally invasive surgeries. The benefit of cosmetic appearance and faster recovery from minimally invasive surgeries did not result in increase in major bleeding complication. However, in more advanced-stage disease, such as those with huge tumor volume, adjacent organ adhesion, or inferior vena cava thrombus, etc, open surgery was preferred to minimally invasive surgery by the surgeons, since the open surgery could possibly provide a clearer operation field and more immediate response for hemostasis if unexpected bleeding was encountered. This bias resulted in the higher chance of blood transfusion rate in open surgery group.
Despite the possible bias, this result still suggested that after proper selection of the patients, minimally invasive surgeries could provide adequate safety for hemostasis and no more bleeding complication than open surgeries.
Although many studies have demonstrated advantage of minimally invasive surgery for kidney cancers, as mentioned earlier, the minimally invasive surgeries including laparoscopic and retroperitoneoscopic surgeries have been underutilized.Citation29–Citation31
It is thought that after controlling all the variables including demographics, tumor size, and comorbidities, the consideration and preference of surgeons were the most significant predictors for the type of surgery performed. Besides the preference of surgeons, in this study we also addressed the possible impact of patients’ economic status on the choice of medical treatment modalities, as some require extra expenditure. Also, female patients were more likely to choose minimally invasive surgeries if RN or PN is required. Cosmetic preference might be one of the reasons for this.
There has been a noticeable trend toward increased application of PN, both open and laparoscopic, and a trend toward minimally invasive renal surgeries such as laparoscopic and robotic-assisted laparoscopic over time.Citation32 Our results also revealed a trend of decreased open RN, and instead increased minimally invasive RN and both open and minimally invasive PN during 2006–2012.
Although the open surgery still played an important role in managing certain complicated cases, the rapid and wide adoption of minimally invasive techniques for kidney surgeries in selected and suitable candidates is occurring. In addition, the incorporation of robotic assistance in minimally invasive renal surgery may also facilitate broader implementation of minimally invasive renal surgery.Citation33
Conclusion
During past decades, fewer and fewer open radical nephrectomies were performed in patients with RCC requiring surgery in Taiwan. Instead, the number of cases of minimally invasive surgeries and PN increased. Compared to open surgeries, minimally invasive surgeries could lead to less postoperative pain and faster recovery. The economic status of the patients potentially hinders them from receiving minimally invasive surgeries which may cause more medical costs.
Acknowledgments
The authors acknowledge institutional grants from the Research Services Center for Health Information, Chang Gung University, Taoyuan, Taiwan (CMRP-MK 103 number: CIRPD1D0031/CMRP-MK 104 number: CIRPD1D0032).
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRNaishadhamDJemalACancer statistics, 2013CA Cancer J Clin2013631113023335087
- PantuckAJZismanABelldegrunASThe changing natural history of renal cell carcinomaJ Urol200116651611162311586189
- WallenEMPruthiRSJoyceGFWiseMUrologic Diseases in America ProjectKidney cancerJ Urol2007177620062018 discussion 2018–201917509280
- DecastroGJMcKiernanJMEpidemiology, clinical staging, and presentation of renal cell carcinomaUrol Clin North Am2008354581592vi18992612
- KummerlinIPten KateFJWijkstraHde la RosetteJJLagunaMPChanges in the stage and surgical management of renal tumours during 1995–2005: an analysis of the Dutch national histopathology registryBJU Int2008102894695118564136
- LipworthLTaroneREMcLaughlinJKThe epidemiology of renal cell carcinomaJ Urol20061766 Pt 12353235817085101
- JemalABrayFCenterMMFerlayJWardEFormanDGlobal cancer statisticsCA Cancer J Clin2011612699021296855
- MillerDCRuterbuschJColtJSContemporary clinical epidemiology of renal cell carcinoma: insight from a population based case-control studyJ Urol201018462254225820952033
- KunkleDAEglestonBLUzzoRGExcise, ablate or observe: the small renal mass dilemma – a meta-analysis and reviewJ Urol2008179412271233 discussion 1233–122418280512
- CampbellSCNovickACBelldegrunAGuideline for management of the clinical T1 renal massJ Urol200918241271127919683266
- AronMKamoiKRemerEBergerADesaiMGillILaparoscopic renal cryoablation: 8-year, single surgeon outcomesJ Urol2010183388989520089263
- Van PoppelHBeckerFCadedduJATreatment of localised renal cell carcinomaEur Urol201160466267221726933
- VolpeACadedduJACestariAContemporary management of small renal massesEur Urol201160350151521664040
- KimSPThompsonRHApproach to the small renal mass: to treat or not to treatUrol Clin North Am201239217117922487760
- NguyenCTCampbellSCNovickACChoice of operation for clinically localized renal tumorUrol Clin North Am2008354645655vii18992618
- NakadaSYSurgical removal of small renal tumors – going, going, gone?J Urol20051741915947565
- RussoPHuangWThe medical and oncological rationale for partial nephrectomy for the treatment of T1 renal cortical tumorsUrol Clin North Am2008354635643vii18992617
- CrouzetSChopraSTsaiSFlank muscle volume changes after open and laparoscopic partial nephrectomyJ Endourol201428101202120724894128
- LuJFHsiaoWCDoes universal health insurance make health care unaffordable? Lessons from TaiwanHealth Aff (Millwood)20032237788
- ChatterjeeSNamRFleshnerNKlotzLPermanent flank bulge is a consequence of flank incision for radical nephrectomy in one half of patientsUrol Oncol2004221363914969802
- KobayashiTTeraiAYoshimuraKNishizawaKMitsumoriKOguraKAssessment of body image alteration after renal surgery using a novel three-dimensional laser scannerUrology200464226426815302475
- ParkSKOlwenyEOBestSLTracyCRMirSACadedduJAPatient-reported body image and cosmesis outcomes following kidney surgery: comparison of laparoendoscopic single-site, laparoscopic, and open surgeryEur Urol20116051097110421856076
- KerblKClaymanRVMcDougallEMKavoussiLRLaparoscopic nephrectomy: the Washington University experienceBr J Urol19947332312368162498
- DunnMDPortisAJShalhavALLaparoscopic versus open radical nephrectomy: a 9-year experienceJ Urol200016441153115910992356
- GillISKavoussiLRLaneBRComparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumorsJ Urol20071781414617574056
- TanHJWolfJSJrYeZWeiJTMillerDCPopulation-level comparative effectiveness of laparoscopic versus open radical nephrectomy for patients with kidney cancerCancer2011117184184419321365632
- GolombosDMChughtaiBTrinhQDMinimally invasive vs open nephrectomy in the modern era: does approach matter?World J Urol201735101557156828477204
- BayrakOSeckinerIErturhanSCilGErbagciAYagciFComparison of the complications and the cost of open and laparoscopic radical nephrectomy in renal tumors larger than 7 centimetersUrol J20141111222122724595928
- PermpongkosolSBaggaHSRomeroFRSolomonSBKavoussiLRTrends in the operative management of renal tumors over a 14-year periodBJU Int200698475175516796695
- MillerDCSaigalCSBanerjeeMHanleyJLitwinMSUrologic Diseases in America ProjectDiffusion of surgical innovation among patients with kidney cancerCancer200811281708171718330868
- LiuJJLeppertJTMaxwellBGPanousisPChungBITrends and perioperative outcomes for laparoscopic and robotic nephrectomy using the National Surgical Quality Improvement Program (NSQIP) databaseUrol Oncol201432447347924332644
- PoonSASilbersteinJLChenLYEhdaieBKimPHRussoPTrends in partial and radical nephrectomy: an analysis of case logs from certifying urologistsJ Urol2013190246446923454156
- PatelHDMullinsJKPierorazioPMTrends in renal surgery: robotic technology is associated with increased use of partial nephrectomyJ Urol201318941229123523085300
