Abstract
Introduction
An epidermoid cyst in an intrapancreatic accessory spleen (ECIPAS) is a rare non-neoplastic cyst, typically occurring in the pancreatic tail. It is difficult to preoperatively differentiate ECIPAS from other types of pancreatic neoplastic cysts.
Case presentation
We herein report a case of a 32-year-old man with a cystic tumor in the tail of the pancreas. The patient underwent a laparoscopic spleen-preserving distal pancreatectomy, and histological examination revealed the presence of ECIPAS. In addition, we also performed a literature review of 42 case reports of ECIPAS.
Conclusion
Although the preoperative diagnosis of ECIPAS is relatively difficult, familiarity with the imaging features, the clinical presentation and the location of the cyst could lead to a correct preoperative diagnosis of ECIPAS, which might thereby reduce the number of unnecessary resections.
Keywords:
Introduction
An epidermoid cyst in an intrapancreatic accessory spleen (ECIPAS) is extremely rare, with the prevalence of 1.7% in general population.Citation1 The differential diagnosis of pancreatic cystic lesions is often challenging because of their similar findings on imaging. It is difficult to preoperatively differentiate ECIPAS from the “other” cystic neoplasms, such as a pancreatic pseudocyst, serous cystic neoplasm, mucinous cystic neoplasm, intraductal papillary mucinous neoplasm and lymphoepithelial cyst, or a solid pancreatic tumor, such as a pancreatic neuroendocrine tumor and solid pseudopapillary tumor, by using conventional imaging. Of the 51 cases of ECIPAS that have been reported in the English literature, only 5 cases were correctly diagnosed based on preoperative imaging.Citation2–Citation43 As ECIPAS is a non-neoplastic pancreatic cyst and has no malignant potential, a correct preoperative diagnosis could thereby reduce the number of unnecessary surgical resections of the pancreas. Herein, we report a case of a 32-year-old male with an ECIPAS and make a comprehensive review of the literature.
Case presentation
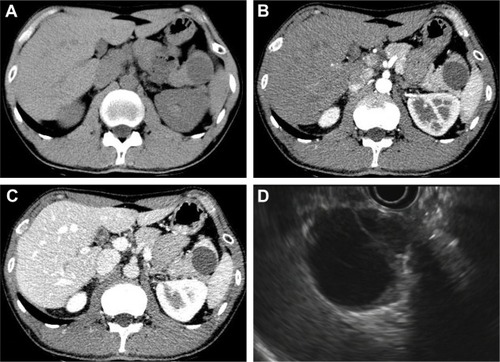
A 32-year-old male was admitted to The First Affiliated Hospital with a mass lesion on the pancreatic tail that was detected by abdominal ultrasound during an annual health checkup. No history of trauma or pancreatitis was recorded. He had normal vital signs and abdominal examination. Initial laboratory data also showed no abnormalities, including those for tumor markers such as carcinoembryonic antigen (CEA) or carbohydrate antigen 19-9 (CA19-9). Abdominal computed tomography (CT) revealed a well-defined cystic neoplasm, which was located in the tail of pancreas and approaching to splenic hilum (), without enhancement in the arterial phase () and the portal phase (). Additionally, endoscopic ultrasonography (EUS) showed a 3.5 cm multilocular cystic lesion in the pancreatic tail with an internal nodule (). The cystic tumor did not communicate with the main pancreatic duct.
Figure 1 The abdominal computed tomography (CT) scan confirmed a well-defined cystic neoplasm in the pancreatic tail (A), without enhancement in the arterial phase (B) and the portal phase (C). Endoscopic ultrasonography (EUS) showed a 3.5 cm multilocular cystic lesion in the pancreatic tail with an internal nodule (D).
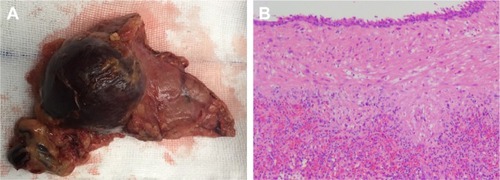
Upon diagnosis of mucinous cystic neoplasms, the patient underwent a laparoscopic spleen-preserving distal pancreatectomy. Macroscopic analysis revealed that the mass in the tail of the pancreas was 4 cm at its greatest diameter and consisted of parenchymal and cystic components (). The gross pathology showed a well-demarcated, multilocular mass, containing colorless serous fluid. Microscopic analysis revealed a multilocular cyst surrounded by accessory splenic tissue in the pancreas parenchyma, and the cyst wall showed a thin multilayered squamous epithelium (). The final pathological diagnosis was epidermoid cyst originating from an intrapancreatic accessory spleen. His postoperative course was uneventful and he was discharged 8 days after the surgery.
Figure 2 (A) Gross appearance of the epidermoid cyst in an intrapancreatic accessory spleen (ECIPAS), with 4 cm at its greatest diameter. (B) Microscopic analysis revealed a multilocular cyst surrounded by accessory splenic tissue in the pancreas parenchyma, and the cyst wall showed a thin multilayered squamous epithelium (H&E staining, ×50).
Ethical approval
The study was approved by the ethics committee of The First Affiliated Hospital of Zhejiang University School of Medicine. Written informed consent was obtained from the patient to have the case details and any accompanying images published.
Discussion
Accessory spleens occur in ~10% of the population and can be found in various anatomic locations other than the splenic hilum. Approximately 20% of accessory spleens occur in or around the tail of the pancreas.Citation1 Epidermoid cysts of the spleen are rare entities, comprising <10% of true non-parasitic splenic cysts.Citation44 An ECIPAS is extremely rare, with only a few reports describing their clinical characteristics. Currently, with the advancement of imaging techniques, such as CT, magnetic resonance imaging (MRI) and EUS, an increasing number of ECIPASs have been detected.
Since Davidson et alCitation2 reported the first case of ECIPAS in 1980, 41 articles and 50 patients have been reported in the English literature (). Including the present case, 20 cases were men and 32 cases were women. The mean age of the patients was 45.4 years (range 12–70 years), and 32 cases (61.5%) were younger than 50 years. Additionally, >50% of the cases were incidentally detectedCitation6,Citation7,Citation10,Citation12,Citation13,Citation16,Citation17,Citation19–Citation22,Citation24–Citation26,Citation29–Citation31,Citation33,Citation35,Citation39,Citation41–Citation43 while the other symptoms included nausea, vomiting, abdominal pain and discomfort, back pain, epigastric pain and fever. In all cases, the tumors were located on the pancreatic tail. The cyst appeared to be multilocular in 31 cases and unilocular in 14 cases (no information for 7 cases). The average cyst size was 4.3 cm (range 1.4–15 cm). As ECIPAS occurs at a relatively young age and it is located in the pancreatic tail, it is always necessary to differentiate ECIPAS when identifying a pancreatic tail cystic mass in young patients.
Table 1 Reported studies of an ECIPAS in the English language literature
An elevation of serum CA19-9 level was observed in 21 cases,Citation8,Citation9,Citation13,Citation16–Citation19,Citation22,Citation26,Citation27,Citation29,Citation30,Citation36,Citation37,Citation41,Citation42 and hence, it was difficult to preoperatively differentiate between an ECIPAS and pancreatic malignancy during clinical analysis. Higaki et alCitation8 reported that the serum CA19-9 levels markedly decreased to normal levels after surgery in patients diagnosed with an ECIPAS, a result suggesting that the serum CA19-9 might be secreted from the ECIPAS.
Most cases of ECIPAS are diagnosed after surgical resection based on the pathological characteristics. A preoperative imaging diagnosis of an ECIPAS is extremely difficult. Only 5 cases (9.8%) among the 51 reported cases were diagnosed preoperatively, while 1 out of 5 cases correctly diagnosed preoperatively was followed up without resection. Notably, in the present case, abdominal CT and EUS also revealed pancreatic mucinous neoplasm. As there are no characteristic features to define the lesion on radiology, it is difficult to entirely differentiate the cystic pancreatic malignancy prior to surgery and histopathological examination.
Until now, few studies have reported the imaging characteristics of ECIPAS. Hu et alCitation45 noted that an accessory spleen surrounding the cyst was a key component for correct diagnosis, and therefore the relationship of enhancement between the splenic parenchyma and the parenchymal component of the lesion for the differential diagnosis of a cystic mass in the pancreatic tail was important. Itano et alCitation21 described that 8 of 13 cases showed a solid tumor component upon CT or MRI, and several reports mentioned retrospectively that the images of the solid component were similar to those of the spleen. In our review, a diagnosis of a mucinous cyst-adenoma, cystadenocarcinoma, pseudocyst, neuroendocrine tumor or a potential malignant tumor was suspected in most cases.Citation21 Interestingly, 3 out of 52 cases were diagnosed as ECIPAS preoperatively based on the similar density in the solid component and spleen on CT or MRI.Citation21,Citation37,Citation43 Furthermore, Motosugi et alCitation46 suggested that superparamagnetic iron oxide-based (SPIO) MRI was the most reliable tool for identifying an ECIPAS, because reticuloendothelial tissues including spleen took up SPIO and the signal intensity of the tissues changes (drops). Unfortunately, our patient did not receive MRI examination preoperatively. All the findings suggest that, in the presence of a relatively large amount of splenic tissues, a correct diagnosis would be possible based on a careful examination of images prior to surgery. However, relatively small amounts of splenic tissues may not be useful in the diagnosis. Therefore, ECIPAS should be considered in the differential diagnosis of pancreatic cystic lesions.
Until now, the treatment of ECIPAS consists of follow-up and surgical removal, including open or laparoscopic surgery with or without splenic preservation. No death has been reported during operation or in the short-term postoperative period. Fujii et alCitation41 suggested that laparoscopic distal pancreatectomy could be a useful, minimally invasive surgical approach for treating pancreatic cysts as well as for the treatment of benign or low-grade malignant tumors located in the pancreatic body or tail. As ECIPAS was reported not to have malignant potential, a correct preoperative diagnosis could thereby avoid unnecessary surgery.
Conclusion
An ECIPAS is an extremely rare disease entity. Enhancing the cystic wall of ECIPAS similar to the spleen was a helpful feature. To prevent any unnecessary surgical intervention, it is important to recognize the ECIPAS as the differential diagnosis of pancreatic cyst. Familiarity with the imaging features, the clinical presentation and the location of the cyst will help radiologists make a more confident diagnosis. Thus, making a definite preoperative diagnosis in most cases is possible.
Acknowledgments
This work was supported by grants from the General Research Projects of the Department of Education of Zhejiang Province (No Y201737812), Zhejiang Province Department of Laboratory Animal Science and Technology Plan Projects (No 2018C37115), and Key Research and Development Project of Science and Technology Department of Zhejiang Province (No 2015C03053).
Disclosure
The authors report no conflicts of interest in this work.
References
- HalpertBAldenZAAccessory spleens in or at the tail of the pancreas. a survey of 2,700 additional necropsiesArch Pathol19647765265414130052
- DavidsonEDCampbellWGHershTEpidermoid splenic cyst occurring in an intrapancreatic accessory spleenDig Dis Sci198025129649677449592
- HanadaMKimuraMKitadaMNakajimaTYamadaKYoshiiMEpidermoid cyst of accessory spleenActa Pathol Jpn19813158638727304174
- MorohoshiTHamamotoTKunimuraTEpidermoid cyst derived from an accessory spleen in the pancreas. A case report with literature surveyActa Pathol Jpn199141129169211785350
- NakaeYHayakawaTKondoTEpidermoid cyst occurring in a pancreatic accessory spleenJ Clin Gastroenterol19911333623642066557
- TangXTanakaYTsutsumiYEpithelial inclusion cysts in an intra-pancreatic accessory spleenPathol Int19944486526547952152
- FurukawaHKosugeTKanaiYMukaiKEpidermoid cyst in an intrapancreatic accessory spleen: CT and pathologic findingsAJR Am J Roentgenol19981711271
- HigakiKJimiAWatanabeJKusabaAKojiroMEpidermoid cyst of the spleen with CA19-9 or carcinoembryonic antigen productions: report of three casesAm J Surg Pathol19982267047089630177
- TateyamaHTadaTMuraseTFujitakeSEimotoTLymphoepithelial cyst and epidermoid cyst of the accessory spleen in the pancreasMod Pathol19981112117111779872647
- SasouSNakamuraSInomataMEpithelial splenic cysts in an intrapancreatic accessory spleen and spleenPathol Int199949121078108310632928
- ChoiSKAhnSIHongKCA case of epidermoid cyst of the intra-pancreatic accessory spleenJ Korean Med Sci200015558959211068999
- TsutsumiSKojimaTFukaiYEpidermoid cyst of an intra-pancreatic accessory spleen – a case reportHepatogastroenterology200047351462146411100377
- HoribeYMurakamiMYamaoKImaedaYTashiroKKasaharaMEpithelial inclusion cyst (epidermoid cyst) formation with epithelioid cell granuloma in an intrapancreatic accessory spleenPathol Int2001511505411148465
- SonomuraTKataokaSChikugoTEpidermoid cyst originating from an intrapancreatic accessory spleenAbdom Imaging200227556056212172998
- FinkAMKulkarniSCrowleyPCrameriJAEpidermoid cyst in a pancreatic accessory spleen mimicking an infected abdominal cyst in a childAJR Am J Roentgenol2002179120620812076937
- YokomizoHHifumiMYamaneTEpidermoid cyst of an accessory spleen at the pancreatic tail: diagnostic value of MRIAbdom Imaging200227555755912172997
- KanazawaHKamiyaJNaginoMEpidermoid cyst in an intra-pancreatic accessory spleen: a case reportJ Hepatobiliary Pancreat Surg2004111616315754048
- WatanabeHYamaguchiYOhtsuboKEpidermoid cyst of the intrapancreatic accessory spleen producing CA 19-9Dig Endosc2004163244248
- WonJKLeeYJKangGHEpithelial cysts in the intrapancreatic accessory spleen that clinically mimic pancreatic cystic tumorKorean J Pathol200539437441
- RuKKalraAUcciAEpidermoid cyst of intrapancreatic accessory spleenDig Dis Sci20075251229123217385039
- ItanoOShiragaNKoutaEEpidermoid cyst originating from an intrapancreatic accessory spleenJ Hepatobiliary Pancreat Surg200815443643918670847
- ServaisELSarkariaISSolomonGJGumpeniPLiebermanMDGiant epidermoid cyst within an intrapancreatic accessory spleen mimicking a cystic neoplasm of the pancreas: case report and review of the literaturePancreas20083619810018192891
- GleesonFCKendrickMLChariSTZhangLLevyMJEpidermoid accessory splenic cyst masquerading as a pancreatic mucinous cystic neoplasmEndoscopy200840suppl 2E141E14218633876
- ZhangZWangJCAn epithelial splenic cyst in an intrapancreatic accessory spleen. A case reportJOP200910666466619890189
- ReissGSickelJZSee-ThoKRamrakhianiSIntrapancreatic splenic cyst mimicking pancreatic cystic neoplasm diagnosed by EUS-FNAGastrointest Endosc200970355755819608182
- KadotaKKushidaYMiyaiYEpidermoid cyst in an intrapancreatic accessory spleen: three case reports and review of the literaturesPathol Oncol Res201016343544219949910
- ItanoOChibaNWadaTLaparoscopic resection of an epidermoid cyst originating from an intrapancreatic accessory spleen: report of a caseSurg Today2010401727520037845
- HornAJLeleSMEpidermoid cyst occurring within an intrapancreatic accessory spleen. A case report and review of the literatureJOP201112327928221546709
- IwasakiYTagayaNNakagawaALaparoscopic resection of epidermoid cyst arising from an intrapancreatic accessory spleen: a case report with a review of the literatureSurg Laparosc Endosc Percutan Tech2011215e275e27922002295
- YamanishiHKumagiTYokotaTEpithelial cyst arising in an intrapancreatic accessory spleen: a diagnostic dilemmaIntern Med201150181947195221921374
- UrakamiAYoshidaKHirabayashiYLaparoscopic-assisted spleen preserving pancreatic resection for epidermoid cyst in an intra-pancreatic accessory spleenAsian J End Surg201144185188
- KhashabMACantoMISinghVKHrubanRHMakaryMAGidaySEndosonographic and elastographic features of a rare epidermoid cyst of an intrapancreatic accessory spleenEndoscopy201143suppl 2 UCTNE193E19421590599
- HarrisACChaudryMAMenziesDConnPCLaparoscopic resection of an epidermoid cyst within an intrapancreatic accessory spleen: a case report and review articleSurg Laparosc Endosc Percutan Tech2012224e246e24922874714
- HongRChoiNSunKLimSHanYEpidermoid cyst arising from an intrapancreatic accessory spleen: a case report and review of the literatureOncol Lett20135246947223420784
- Hamidian JahromiAFallahzadehMKDela CruzNChuQEpidermoid cyst arising from an intrapancreatic accessory spleen: a case report and a review of the literatureJ La State Med Soc2013165315315624015430
- ZavrasNMachairasNFoukasPLazarisAPatapisPMachairasAEpidermoid cyst of an intrapancreatic accessory spleen: a case report and literature reviewWorld J Surg Oncol2014129224721745
- KumamotoYKaizuTTajimaHKuboHNishiyamaRWatanabeMA rapidly growing epidermoid cyst in an intrapancreatic accessory spleen treated by laparoscopic spleen-preserving distal pancreatectomy: report of a caseInt Surg Epub201562
- KwakMKLeeNKKimSA case of epidermoid cyst in an intrapancreatic accessory spleen mimicking pancreas neoplasms: MRI with DWIClin Imaging201640116416626422768
- KatoSMoriHZakimiMEpidermoid cyst in an intrapancreatic accessory spleen: case report and literature review of the preoperative imaging findingsIntern Med201655233445345227904107
- ModiRMKambojAKSwansonBConwellDLKrishnaSGEpidermoid cyst within an intrapancreatic accessory spleen: endosonography and confocal endomicroscopy of an unusual pancreatic cystic lesionEndoscopy201648S 01E332E33327741530
- FujiiMYoshiokaMShiodeJTwo cases of an epidermoid cyst developing in an intrapancreatic accessory spleen identified during laparoscopic distal pancreatectomyIntern Med201655213137314127803407
- HirabayashiKYamadaMKonoHEpidermoid cysts are a characteristic feature of intrapancreatic but not of extrapancreatic accessory spleensVirchows Arch20174711919828540449
- MatsumotoKKatoHOkadaHEpidermoid cyst in an intrapancreatic accessory spleen diagnosed by typical radiographic images and endoscopic ultrasound fine-needle aspiration findings with contrast agentClin Gastroenterol Hepatol201816e13e1428300686
- RobbinsFGYellinAELinguaRWCraigJRTurrillFLMikkelsenWPSplenic epidermoid cystsAnn Surg19781873231235637577
- HuSZhuLSongQChenKEpidermoid cyst in intrapancreatic accessory spleen: computed tomography findings and clinical manifestationAbdom Imaging201237582883322327420
- MotosugiUYamaguchiHIchikawaTEpidermoid cyst in intrapancreatic accessory spleen: radiological findings including superparamagnetic iron oxide-enhanced magnetic resonance imagingJ Comput Assist Tomogr201034221722220351508
