Abstract
Cerebral infarction due to acute embolism in the large artery during pregnancy is a rare but severe condition threatening both the mother’s and child’s life. Physicians lack diagnostic and therapeutic guidance to manage this particular situation due to the paucity of published cases. Furthermore, the pathogeny is poorly known, rendering preventive strategies difficult. We describe the case of a young woman presenting cryptogenic acute cerebral infarction during the first trimester of pregnancy who was successfully treated with combined reperfusion therapy. We reviewed the literature to collect data about pathogeny and management. A 28-year-old pregnant woman was diagnosed with acute cerebral infarction due to left middle cerebral artery occlusion at 9 weeks of gestation. Endovascular thrombectomy combined with intravenous thrombolysis allowed cerebral reperfusion leading to a decrease in the National Institute of Health Stroke Score from 13 to 1 at 24 hours. Comprehensive etiological investigation was negative. Anticoagulation therapy with low-molecular-weight heparin was administered as preventive treatment during the pregnancy and postpartum. Neither the mother nor the child experienced any complications: the baby was born by normal vaginal delivery and the outcome was good at 1 year. We identified 21 other cases of patients treated with reperfusion therapies, four of which consisted of endovascular thrombectomy, and only one a combined strategy. Pregnant women with acute cerebral infarction due to arterial occlusion can benefit from combined reperfusion therapy. More cases should be collected to assess treatment in these patients, to understand pathogeny, and propose the best preventive strategy.
Stroke during pregnancy affects 30 women per 100,000 representing a 3-fold higher risk than in young adults overall. Cerebrovascular events in pregnancy are usually related to eclampsia and cerebral venous thrombosis.Citation1,Citation2 Cerebral infarction due to acute embolism in a large intracranial artery is rare and has hardly ever been described. Consequently, physicians lack information to diagnose and treat this severe life-threatening condition for both mother and child. There is a high risk of obstetric and pediatric complications associated with reperfusion therapies. Furthermore, the pathogeny of ischemic stroke during pregnancy remains poorly understood, rendering it difficult to recommend preventive strategies. We report the case of a patient who presented severe cryptogenic cerebral infarction due to occlusion of the left middle cerebral artery (MCA) and who was successfully treated with recombinant tissue plasminogen therapy (rt-PA) and endovascular thrombectomy. Based on our experience and a literature review, we describe diagnostic methods, the use of reperfusion therapies, etiological investigations and preventive strategies in this particular context.
Case report
The patient provided written informed consent for the case details to be published. All data have been anonymized.
History
A 28-year-old woman with a medical history of miscarriage was admitted in the Verdun Hospital (Lorraine, France) during the first trimester of pregnancy (9 weeks of gestation) because of right motor and sensitive deficit with dysarthria experienced on waking.
Examination
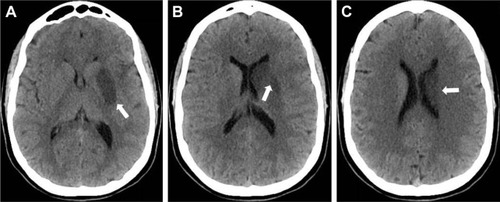
Neurological examination was performed by the stroke unit of the University Hospital of Nancy 180 minutes later through telemedicine. The patient was found to have a National Institute of Health Stroke Score (NIHSS) of 13; her blood pressure was 93/60 kPa and heart rate 76 bpm. A computed tomography (CT) scan of the brain showed early signs of acute cerebral infarction in the left MCA territory (). The Alberta Stroke Program Early CT Score (ASPECTS) was 8. Proximal thromboembolic occlusion of the left MCA was confirmed by cerebral CT angiography ().
Figure 1 Cerebral CT scan showing spontaneous hyperdensity in the left middle cerebral artery proximal segment M1 (A), lentiform nucleus obscuration (B, arrow 1), loss of gray-white matter discrimination (B, arrow 2), and proximal occlusion of the left middle cerebral artery on CT angiography (C).
Abbreviation: CT, computed tomography.
Operation
The patient subsequently underwent intravenous thrombolysis with 70 mg (0.9 mg/kg) of rt-PA before being transferred to the stroke unit. On arrival (5.5 hours after reporting initial signs) the NIHSS was unchanged. We decided to perform an endovascular thrombectomy.
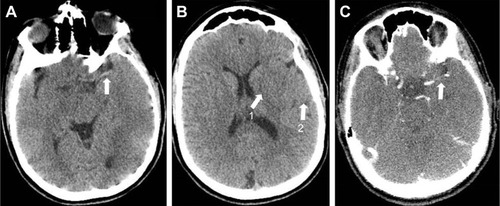
Conventional angiography was performed on a biplane image-guided system (Innova system GE) with a low dose protocol (686 cGy/cm2) after protecting the patient’s abdomen by a lead apron. A Neuron Max 088 catheter (Penumbra Inc., Alameda, CA, USA) was placed in the left internal carotid artery via the femoral artery. Angiography showed persistent occlusion of the proximal segment (M1) of the left MCA (). The thrombus was penetrated by a microcatheter RapidTransit® (Codman, Johnson & Johnson, New Brunswick, NJ, USA) and a microguide wire Terumo 16. A Trevo ProVue (Stryker Neurovascular, Fremont, CA, USA) retriever stent was then delivered through the micro-catheter and deployed inside the thrombus for 3 minutes. A Sofia® 6F (MicroVention, Aliso Viejo, CA, USA) aspiration catheter was advanced to the level of the occlusion. Continuous aspiration was performed for 30 seconds using a Penumbra aspiration pump and the system was then slowly removed under aspiration. A 6-mm red clot was taken out from between the stent retriever and the aspiration catheter (). Angiography showed successful recanalization of more than half of the left MCA territory (Thrombolysis in Cerebral Infarction [TICI] scale grade IIb). A slight spasm was observed on the proximal segment (M1) (). The NIHSS score immediately decreased to 3 and then to 1 by the 24-hour assessment with limited infarction of the corpus striatum on the control CT scan ().
Figure 2 Initial left internal carotid angiogram (lateral [A], and anteroposterior [B] views) showing proximal occlusion of the left middle cerebral artery (white arrow), lack of perfusion in the respective territory, and collateral flow from the left anterior cerebral artery through leptomeningeal anastomoses (black arrows).
![Figure 2 Initial left internal carotid angiogram (lateral [A], and anteroposterior [B] views) showing proximal occlusion of the left middle cerebral artery (white arrow), lack of perfusion in the respective territory, and collateral flow from the left anterior cerebral artery through leptomeningeal anastomoses (black arrows).](/cms/asset/a9b37337-1751-4265-bbe3-76e5a5f7ccab/dtcr_a_166289_f0002_b.jpg)
Figure 3 The 6 mm red clot removed from left middle cerebral artery following endovascular thrombectomy.

Pathological findings
Comprehensive etiological investigations did not reveal any cause of the cerebral infarction. It was thus classified as cryptogenic. A detailed medical interview revealed no history of cardiovascular disease (personal or familial), drug consumption, or recent headache. Cervical and transcranial Doppler ultrasonography were normal. Cervical arteries were also examined during conventional angiography with no sign of dissection. Electrocardiogram and 72-hour cardiac monitoring did not detect arrhythmia and blood pressure levels were normal. Transoesophageal echocardiography failed to find any thrombus or patent foramen ovale. Blood tests did not reveal any prothrombotic anomalies: the hemoglobin level was 12.6 g/dL, the platelet count was 312 G/L, C-reactive protein level was <5 mg/L, the low-density lipoprotein-cholesterol level was 1.89 mmol/L, the pre-prandial blood glucose level was 4.83 mmol/L, and the homocysteine level was normal at 12.6 μmol/L. All the coagulation tests including prothrombin time, activated partial thromboplastin time, lupus anticoagulant and anticardiolipin antibody were normal. Anticoagulation factor activities were normal for protein S, protein C and antithrombin (respectively at 78, 99, and 91%). No activated protein C resistance or mutation of the prothrombin gene were found.
Postoperative course
Obstetric examination and fetal ultrasound showed that neither the mother nor the fetus had experienced any complications. Anticoagulation therapy was initiated as a preventive strategy with low-molecular-weight heparin (tinzaparin 175 anti-Xa IU/kg/day) and administered up to 35 weeks of gestation, when a daily dose of enoxaparin (4,000 anti-Xa IU) was started. The patient gave birth at a gestational age of 39 weeks and 2 days to a healthy infant of 3.8 kg by normal vaginal delivery with no complications. The Apgar score at 5 minutes was 7/10 and the umbilical cord arterial blood pH was 7.35. Enoxaparin was discontinued after postpartum and replaced by a daily dose of 160 mg of aspirin. Both the mother and child had a normal medical examination at 1 year.
Discussion
We describe the diagnosis and management of an acute cryptogenic cerebral infarction due to left MCA occlusion in a woman during the first trimester of pregnancy. The patient was successfully treated by combined reperfusion therapy.
The first issue that arises for a woman with stroke symptoms during the first trimester of pregnancy is the use of diagnostic cerebral imaging. We used a cerebral CT scan with iodine injection for intracranial angiography. According to the French public expert authority in nuclear and radiological risks (IRSN), the uterus is exposed to less than 0.1 mGy during this examination, which is under the teratogenic dose range.Citation3,Citation4 However, most centers in France prefer cerebral MRI to diagnose acute stroke and determine reperfusion therapies. This would have allowed a better estimation of the time of the stroke onset.Citation5 Ray et al compared the outcome in 1,737 women who underwent MRI during the first trimester of pregnancy with an unexposed cohort of more of 1,400,000 patients. They found no significant increased risk of fetal or early infant death, congenital anomalies, neoplasms, vision or hearing loss in the children by the age of 4 years.Citation6 MRI has also been shown to be safe in women in the second and third trimesters of pregnancy.Citation7 Nevertheless, gadolinium injection should be avoided throughout pregnancy because of a significant risk of perinatal mortality and a broad set of rheumatological and infiltrative skin diseases related to nephrogenic systemic fibrosis.Citation6 The intracranial arteries can be explored through three-dimensional time-of-flight sequence and cerebral perfusion through arterial spin labeling sequence without contrast agent injection. Unlike a cerebral CT-scan, MRI does not require additional irradiation or injections of iodine inherent to conventional angiography for endovascular thrombectomy. A low dose protocol with tight collimation on angiogram should be used allowing a 50% reduction in irradiation compared to usual procedures and provides satisfactory, through reduced image resolution.Citation8 The infant should be examined for neonatal hypothyroidism at 3 days due to the iodine injection even if this would appear to be a rare complication.Citation9
Physicians are reluctant to use rt-PA to treat acute cerebral infarction in pregnant women due to the risk of obstetric hemorrhage and the unknown effect on fetal development, especially during the first trimester. However, literature argues in favor of rt-PA safety during pregnancy. Data from animal models suggest that rt-PA does not pass the placental barrier due to its large molecular size, and no teratogenic effects have been observed.Citation10 Gartman reviewed 231 cases of thrombolytic agent use in patients to treat systemic arterial or venous thrombosis during pregnancy and found no significant increased risk of complication compared to a non-pregnant population.Citation11 Tversky et al and Reining-Festa et al identified 17 cases of patients with acute cerebral infarction during pregnancy treated with rt-PA (intravenous or intra-arterial) in their systematic literature review.Citation12,Citation13 We found another case where rt-PA was used for combined reperfusion therapy.Citation14 In all, two medical terminations of pregnancy have been reported, including one due to a lethal chromosomal anomaly.Citation15 One patient presented an intrauterine hematoma, which was successfully drained.Citation15 Three patients experienced cerebral hemorrhagic complications after rt-PA: two presented asymptomatic deep hematoma,Citation16,Citation17 and another died but in the context of arterial dissection related to angioplasty.Citation15 Finally, international guidelines incite physicians to consider intravenous thrombolysis during pregnancy “when the anticipated benefits of treating moderate to severe stroke outweigh the anticipated increased risks of uterine bleeding.”Citation18
Endovascular thrombectomy now forms an integral part of reperfusion therapies to treat proximal occlusion of cerebral arteries.Citation19 Four cases during pregnancy have recently been reported in the literature. Aaron et al described two cases of MCA occlusion treated with endovascular thrombectomy only through aspiration by the Penumbra system.Citation20 Bhogal et al reported a case of MCA occlusion treated by stent retriever thrombectomy and a basilar artery occlusion treated by combined reperfusion therapy.Citation14 The outcome was good for both the mothers and children in these four cases, emphasizing the benefit of this treatment approach in this specific population. Endovascular thrombectomy alone could be an interesting strategy in acute ischemic stroke management during pregnancy as it prevents the mother and fetus from being exposed to rt-PA and the inherent risks. More broadly, some studies have shown that endovascular therapy provides a higher rate of recanalization, thus improving outcome in young patients and supporting aggressive interventional strategies in this population.Citation21 Nevertheless, to date, the effectiveness of endovascular thrombectomy during the first hours after stroke onset has only been demonstrated in combination with intravenous thrombolysis.Citation22 In our case we were able to initiate intravenous thrombolysis early in a local hospital through telestroke as the patient was approximately 2 hours from an endovascular thrombectomy capable center.
After managing the acute phase, it is crucial to undertake etiological investigations to understand the stroke mechanism so as to initiate a prevention strategy. Most etiologies described in literature pertain to a young population with stroke: cardiac valve diseases (especially rheumatologic valve disease), coagulopathy, and patent foramen ovale.Citation2,Citation13,Citation23,Citation24 The most frequent etiology of cerebral infarction in this population is cervical artery dissection. The risk of cervical artery dissection is accrued during pregnancy and postpartum by modifications of media due to hormonal changes.Citation23,Citation25 Pregnant women presenting with stroke should thus undergo the same etiological investigation as the general young population with stroke, paying particular attention to exploration of cervical and intracranial arteries, transoesophageal echocardiography, and detection of biological prothrombotic agents (platelet count, lupus anticoagulant and anticardiolipin antibody). Most cerebrovascular events occurring during pregnancy are related to eclampsia and cerebral venous thrombosis, both of which cause cerebral infarction and hematomas.Citation2 Several other etiologies have been reported such as amniotic fluid embolism, postpartum angiopathy and ovarian stimulation.Citation18,Citation26 Comprehensive etiological investigation failed to find any of these causes in our patient (including absence of patent foramen ovale), which led us to classify this cerebral infarction as cryptogenic.
Although cryptogenic strokes can occur in the general young population, our case raises the question of the role of pregnancy in the pathogeny of cerebral infarction. Besides the hemodynamic changes brought about by elevated blood volume and cardiac flow during pregnancy,Citation27 some reports seem to incriminate a prothrombotic state but without convincing evidence. Partly because of hormonal modifications,Citation28 pregnancy is associated with major changes in hemostasis due to an increase in most thrombotic agents (factors VIII, X, XII, von Willebrand, and ristocetin cofactors) combined with a decrease in the quality of natural anticoagulants such as protein S. Fibrinolytic activity is decreased due to the production of plasminogen activator inhibitor by the placenta.Citation29 However, these abnormalities are more likely to cause venous thromboembolism, and have been described during advanced stages of pregnancy or during the postpartum.Citation23,Citation29
In view of the unknown origin of the stroke in our patient and the possible implication of a prothrombotic state as suggested by literature, we decided to administer anticoagulation therapy to prevent recurrence during pregnancy and postpartum even though this approach remains debatable.Citation30 Several studies are currently underway to determine whether anticoagulation or antiplatelet therapy is the best preventive strategy in cases such as ours.Citation31 While use of heparin and low-dose aspirin use is allowed during pregnancy, oral anticoagulants are not recommended during the first and third trimesters due to a risk of malformation.Citation32 Currently, there are no data reporting the use of direct oral anticoagulants and clopidogrel. A cesarean section is preferable in patients with obstetric complication or recent cervical artery dissection only, to prevent worsening during labor from pushing.Citation33 Finally, a French multicenter study has shown that stroke recurrence during subsequent pregnancies is rare.Citation34
Conclusion
Management of acute cerebral infarction in pregnant women should not differ from that in the general population. Adjustments are possible to minimize irradiation during the diagnostic phase. Combined reperfusion therapy remains the best strategy to restore intracranial reperfusion, without compromising safety, and consequently to ensure good outcome for both mother and child. Nevertheless, it is necessary to collect more cases to assess these practices and especially to understand the pathogeny of stroke during pregnancy.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- JamesAHBushnellCDJamisonMGMyersERIncidence and risk factors for stroke in pregnancy and the puerperiumObstet Gynecol2005106350951616135580
- SwartzRHCayleyMLFoleyNThe incidence of pregnancy-related stroke: A systematic review and meta-analysisInt J Stroke201712768769728884652
- French public expert authority in nuclear and radiological risks (IRSN)[Delivered doses to patients in Computed Tomography and conventional radiology] Doses délivrées aux patients en scanographie et en radiologie conventionnelle Rapport DRPH/SER n°2010-12 Available from: http://www.irsn.fr/FR/expertise/rapports_expertise/Documents/radioprotection/IRSN-Rapport-dosimetrie-patient-2010-12.pdfAccessed August 23, 2018 French
- de SantisMdi GianantonioEStrafaceGIonizing radiations in pregnancy and teratogenesis: a review of literatureReprod Toxicol200520332332915925481
- ThomallaGChengBEbingerMDWI-FLAIR mismatch for the identification of patients with acute ischaemic stroke within 4:5 h of symptom onset (PRE-FLAIR): a multicentre observational studyLancet Neurol2011101197898621978972
- RayJGVermeulenMJBharathaAMontaneraWJParkALAssociation between MRI exposure during pregnancy and fetal and childhood outcomesJAMA2016316995296127599330
- StrizekBJaniJCMucyoESafety of MR imaging at 1.5 T in fetuses: a retrospective case-control study of birth weights and the effects of acoustic noiseRadiology2015275253053725575119
- YiHJSungJHLeeDHKimSWLeeSWAnalysis of radiation doses and dose reduction strategies during cerebral digital subtraction angiographyWorld Neurosurg201710021622328089806
- ChauvetPTerralDColombierM[Iodinated contrast in pregnant women and neonatal thyroid function] Injection de produit de contraste iodé en cours de grossesse et fonction thyroïdienne néonataleGynecol Obstet Fertil20164412685689 French27839713
- TanakaMStudy in rats treated intravenously with GMK-527 (II) teratogenicity study in rats with GMK-527Yakuri Chiryo19881693106
- GartmanEJThe use of thrombolytic therapy in pregnancyObstet Med20136310511127708701
- TverskySLibmanRBReppucciMLTufanoAMKatzJMThrombolysis for ischemic stroke during pregnancy: a case report and review of the literatureJ Stroke Cerebrovasc Dis20162510e167e17027523596
- Reining-FestaAFöldyDCoulibaly-WimmerMEischerLHegerMFertlEIntravenous thrombolysis of stroke in early pregnancy: a case report and review of the literatureJ Neurol2017264239740028028624
- BhogalPAguilarMAlmatterMKarckUBäznerHHenkesHMechanical thrombectomy in pregnancy: report of 2 cases and review of the literatureInterv Neurol201761–2495628611834
- MurugappanACoplinWMAl-SadatANThrombolytic therapy of acute ischemic stroke during pregnancyNeurology200666576877016534124
- DapprichMBoesseneckerWFibrinolysis with alteplase in a pregnant woman with strokeCerebrovasc Dis200213429012011557
- ElfordKLeaderAWeeRStysPKStroke in ovarian hyperstimulation syndrome in early pregnancy treated with intra-arterial rt-PANeurology20025981270127212391365
- DemaerschalkBMKleindorferDOAdeoyeOMScientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke AssociationStroke201647258164126696642
- NogueiraRGJadhavAPHaussenDCThrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarctN Engl J Med20183781112129129157
- AaronSShyamkumarNKAlexanderSMechanical thrombectomy for acute ischemic stroke in pregnancy using the penumbra systemAnn Indian Acad Neurol201619226126327293343
- ChalouhiNTjoumakarisSStarkeRMEndovascular stroke intervention in young patients with large vessel occlusionsNeurosurg Focus2014361E6
- BracardSDucrocqXMasJLMechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trialLancet Neurol201615111138114727567239
- UlrichNJohnsonAJodryDDolaCMartin-SchildSEl KhouryRResolution of internal carotid dissection with middle cerebral artery occlusion in pregnancyCase Rep Neurol Med2015201515
- SkidmoreFMWilliamsLSFradkinKDAlonsoRJBillerJPresentation, etiology, and outcome of stroke in pregnancy and puerperiumJ Stroke Cerebrovasc Dis200110111017903792
- BarrettJMvan HooydonkJEBoehmFHPregnancy-related rupture of arterial aneurysmsObstet Gynecol Surv19823795575666752786
- FronteraJAAhmedWNeurocritical care complications of pregnancy and puerperumJ Crit Care20142961069108125123793
- LundCJDonovanJCBlood volume during pregnancy. Significance of plasma and red cell volumesAm J Obstet Gynecol19679833944035621454
- SattarNGreerIARumleyAA longitudinal study of the relationships between haemostatic, lipid, and oestradiol changes during normal human pregnancyThromb Haemost199981171759974378
- ThorntonPDouglasJCoagulation in pregnancyBest Pract Res Clin Obstet Gynaecol201024333935220097136
- HelmsAKDroganOKittnerSJFirst trimester stroke prophylaxis in pregnant women with a history of strokeStroke20094041158116119211492
- HartRGCataneseLPereraKSNtaiosGConnollySJEmbolic stroke of undetermined source: a systematic review and clinical updateStroke201748486787228265016
- BatesSMGreerIAMiddeldorpSVeenstraDLPrabulosA-MVandvikPOVTE, thrombophilia, antithrombotic therapy, and pregnancyChest20121412e691Se736S22315276
- ReinhardMMunzMvon KannenALGriesser-LeuteHJDittrichREngelterSTRisk of recurrent cervical artery dissection during pregnancy, childbirth and puerperiumEur J Neurol201522473673925444227
- LamyCHamonJBCosteJMasJLIschemic stroke in young women: risk of recurrence during subsequent pregnancies. French Study Group on Stroke in PregnancyNeurology200055226927410908903

![Figure 4 Left internal carotid artery angiogram (lateral [A], and anteroposterior [B] views) showing recanalization (Thrombolysis in Cerebral Infarction [TICI] scale grade IIb), and slight vasospasm (white arrow) of the left middle cerebral artery following mechanical thrombectomy.](/cms/asset/a8890df4-11a6-4f30-adbb-6a9880980bda/dtcr_a_166289_f0004_b.jpg)