Abstract
Purpose
Diabetes is a chronic lifelong condition, and adherence to medications and self-monitoring of blood glucose are challenging for diabetic patients. The dramatic increase in the prevalence of diabetes is largely due to the incidence of type 2 diabetes in low- and middle-income countries (LMIc) besides high-income countries (HIc). We aimed to evaluate whether pharmacist care (PC) service model in LMIc and HIc could improve clinical outcomes in diabetic patients by performing a meta-analysis.
Methods
PubMed, Embase, and ProQuest Dissertations Unlimited Published Literature database were searched to find publications pertaining to pharmacist-led intervention in patients with diabetes. The inclusion criteria were as follows: 1) randomized controlled trials, 2) confirmed diabetic patients (type 1 or type 2), 3) pharmaceutical care intervention by clinical pharmacist or/and multidisciplinary team, and 4) reporting HbA1c at baseline and end of study or the mean change in these values.
Results
A total of 37 articles were included in the meta-analysis. The overall result was significant and in favor of PC intervention on HbA1c change (standard difference in mean values [SDM]: 0.379, 95% CI: 0.208–0.550, P<0.001). The stratified meta-analysis showed that PC was significant in both HIc (n=20; SDM: 0.351, 95% CI: 0.207–0.495) and LMIc (n=15; SDM: 0.426, 95% CI: 0.071–0.780). More than 6 months is needed to obtain adequate effects on clinical diabetes parameters.
Conclusion
Our study presented that an adequate duration of pharmacist-led pharmaceutical care was effective in improving HbA1c in patients with diabetes in both LMIc and HIc.
Introduction
Diabetes is a serious and chronic disease that can lead to various complications and premature death. According to the “Global Report on Diabetes (2016)” by World Health Organization (WHO), the number of diabetic adults has quadrupled to 422 million since 1980. This recent dramatic rise is largely due to the incidence of type 2 diabetes in low- and middle-income countries (LMIc). In all, 43% of deaths in a total or 3.7 million deaths related to diabetes in 2012 is attributable to higher than optimal blood glucose, and this occurs before the age of 70,Citation1 which is much shorter than the life expectancy of 81.3 mean years among the Organisation for Economic Co-operation and Development (OECD) countries in 2015.Citation2 Since diabetes is a chronic lifelong condition, adherence to medications and self-monitoring of blood glucose are quite challenging to the patients. Blood glucose concentration is a sensitive marker affected by numerous outer environments such as food intake, exercise, stress and medication.Citation3 On the contrary, HbA1c concentration in the blood reflects the average blood glucose over the previous 8–12 weeks. The HbA1c level can predict the clinical outcome of microvascularCitation4,Citation5 and macrovascular complicationsCitation6 as well, and the American Diabetes Association (ADA) recommend that HbA1c should be measured at regular intervals in all patients with diabetes.Citation7 Thus, many researches on diabetes management are using HbA1c as a surrogate marker for clinical outcomes. There have been numerous efforts to implement pharmaceutical care in diabetic patients to improve disease outcomes. Improved management with the consistent support of multidisciplinary pharmaceutical care services can lead to better control of diabetes and fewer complications.Citation8 For example, in Medication Therapy Management (MTM), a range of services including education, counseling, and assessing each medication and medication-related problems are provided to patients by clinical pharmacists to optimize and improve therapeutic outcomes in the USA.Citation9 Together with hospital-based clinician-monitored programs, pharmacist-led community/hospital-based pharmaceutical care programs can be designed in an effort to achieve better glycemic, metabolic outcome and blood pressure control in this patient group.Citation10
A recent meta-analysisCitation11 and a systematic reviewCitation12 of pharmacist for blood pressure and cardiovascular diseases showed that the implementation of a pharmacist care (PC) model provided improvement in outcomes. The systematic analysis and meta-analysis of PC for diabetic patients showed positive impact on HbA1c outcomes.Citation13–Citation15 However, recent studies reported no significantly different clinical parameters between the PC group and usual care (UC) group,Citation16–Citation18 rendering the need to reevaluate PC. Moreover, they did not present the effectiveness of PC in LMIc apart from high-income countries (HIc). Since the 2016 report of WHO revealed a considerable increase in the number of diabetic patients in LMIc, thus we aimed to evaluate whether the PC service model in HIc and LMIc could improve the clinical outcomes of diabetic patients by performing a meta-analysis including the up-to-date studies.
Methods
Search strategy
A systematic review protocol conforming to the Effective Practice and Organization of Care (EPOC) guideline was developed and prepared following the PRISMA recommendations.Citation19 Electronic databases of PubMed, Embase, and ProQuest Dissertations Unlimited Published Literature database were searched by using the following keywords: “diabetes”, “diabetes mellitus”, “type one diabetes”, “type two diabetes”, “diabetes type 1”, “diabetes type 2”, “community pharmacy”, “community pharmacies”, “community pharmacist”, “community pharmacists”, “pharmacy”, “pharmacist”, “hospital pharmacy”, “hospital pharmacist”, “hospital pharmacists”, “pharmacy services”, “pharmacist intervention”, “pharmaceutical care”, “pharmac*”. A manual review was performed to search for unindexed articles in the Journal of Research in Medical Sciences, Journal of American Pharmacists Association and reference lists of related articles.
Inclusion and exclusion criteria
The literature search was performed to include studies published up to July 27, 2017, by two independent reviewers. Any disagreement was resolved by discussion among the two reviewers and a third researcher. The inclusion criteria for full-text review were as follows: 1) randomized controlled trial (RCT); 2) confirmed adult diabetic patients (type 1 or type 2); 3) pharmaceutical care intervention by clinical pharmacist or/and multidisciplinary team (PC includes working in cooperation with the patient and other health care providers to assess, monitor, initiate, and modify medication use and to provide education service to health care professionals as well as to the patients); and 4) each article should have reported HbA1c or fasting blood glucose (FBG) level at baseline and end of study or the mean change in these values.
The exclusion criteria were as follows: non-English language, editorials, commentaries, narrative reviews, clinical practice guidelines, conference abstracts, and literature not in peer-reviewed journals. The same reviewers independently evaluated the full text of all identified studies in the first stage of screening and resolved any disagreements.
Outcome assessment
HbA1c concentration in the blood reflects the average blood glucose over the previous 8–12 weeks. The HbA1c level can predict the clinical outcome of microvascularCitation4,Citation5 and macrovascular complicationsCitation6 as well, and ADA recommend HbA1c to be measured at regular intervals in all patients with diabetes.Citation7 Thus, HbA1c has been utilized as an additional stable criterion for assessing glucose control. In this aspect, we chose the difference of HbA1c change and the proportion of patients achieving target HbA1c level (<7%) between two groups as the main outcome measure.
Data extraction
The following information was extracted from the full text of included studies by two independent researchers: first author, year of publication, study type, country of study site, disease type of patients, age, service providers, intervention type, and laboratory data pertaining to HbA1c and the number of patients achieving HbA1c goal. The income levels were searched to pool outcomes by income level using the data from the World Bank Group.Citation20 The duration of intervention was stratified and designated as 1 (<6 months), 2 (≥6 and <12 months), and 3 (≥12 months).
Quality score assessment
The quality of individual study was assessed by two independent reviewers using the EPOC risk of bias tool. This risk of bias tool is used when the clinical trials involve patient care, educational intervention, patient performance measure, health care quality measure.Citation21 The standard risk of bias tool includes assessment of domains such as allocation concealment, baseline outcome, baseline characteristics, blinding, and selective reporting.
A domain with a low risk of bias is indicated by “low” and that with a high risk of bias is indicated by “high”. If a particular domain has ambiguity or uncertainty due to lack of information, then it is indicated as “unclear”.
Statistical analyses
The association between HbA1c levels after PC intervention and clinical outcomes was evaluated quantitatively by meta-analysis. The pooled OR were calculated for the included articles stratified by income status of the countries and duration of follow-up (3–5 months, 6–11 months, and ≥12 months). The primary outcome of this study was to evaluate the association between PC and HbA1c change.
Between-study heterogeneity was assessed by Q-statistic (heterogeneity was considered statistically significant if P<0.1)Citation22 and quantified by I2 value. Both fixed- and random-effects models were used to combine the aggregate data determined by the I2 value. When I2 was >50%, the random-effects model was used for analysis. Potential publication bias was assessed using the Egger’s linear regression test.Citation23
Statistical analyses were performed using Comprehensive Meta-Analysis (ver 3; Biostat, Inc., Engelwood, NJ, USA) and IBM SPSS (ver 21; IBM Corporation, Armonk, NY, USA). All tests were two sided, and P<0.05 was considered as significant unless otherwise specified.
Results
PRISMA flow for study selection
As shown in , of the 3,794 publications identified, 35 publications were found eligible for meta-analysis.
Figure 1 PRISMA flow diagram of selected publications in systematic review and meta-analysis.
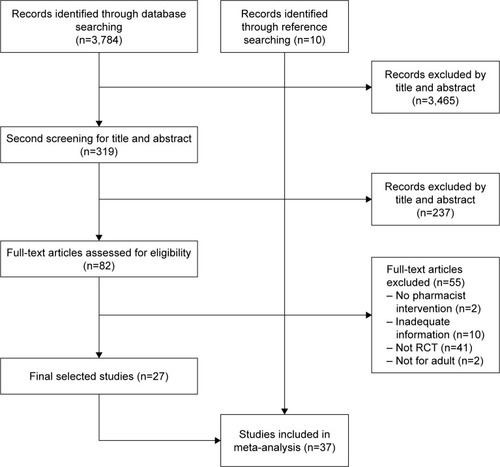
Among the identified publications, 3,465 articles were excluded as inappropriate by title and abstract review. In all, 82 articles were eligible for full-text review. After excluding studies with no pharmacist intervention (n=2), inadequate information (n=10), non-RCT studies (n=41), and non-adult studies (n=2), 27 articles were finally selected. Upon searching for the reference review, 10 additional articles were found to be eligible for meta-analysis; therefore finally, 37 studies were included in the meta-analysis.
Overall review
In all, 14 articles were published in the North American region (USA [n=13] and Canada [n=1]), three in the European region (UK, Spain, and Belgium), eight in Asia (Thailand [n=3], Hong Kong, Taiwan, Malaysia, Pakistan, and India), six in the Middle East (Jordan [n=2], Iraq, Iran [n=2], and UAE), three in Brazil, and three in Australia. Brazil, Iran, Iraq, Malaysia, Pakistan, Thailand, Jordan, UAE, and India were classified as LMIc.Citation20 The intervention period was stratified as follows: intervention period <6 months (n=7), between 6 and 12 months (n=10), and ≥12 months (n=12). All the trials were conducted in ambulatory settings, including private clinic, hospital-based clinic, community pharmacies, and nationwide health care system or regional health care system ().
Table 1 Characteristics of randomized controlled studies included in the final analysis
All 37 studies included 2,961 PC and 2,899 UC patients. The overall period of pharmacist intervention was mean 9.07 months (SD 5.73) ranging from 3 to 32 months. In 27 studies, >100 diabetic patients were enrolled, and in 15 studies, the follow-up period was ≥12 months. The interventions were given from 2-week to 3-month interval, and several studies did not report the interval. The PC was conducted by pharmacists in 24 studies and MTC in 13 studies. The PC program consisted of information on disease and medications, adherence education, survival skills regarding hypo- and hyperglycemia incidence, and insulin injection skills. The delivery type of education or intervention was face-to-face intervention, telephone counseling, or group appointments, meeting, or education sessions. Adjunctive tools such as booklets, disease or medication information sheets, pillbox, and stickers were provided in many studies ().
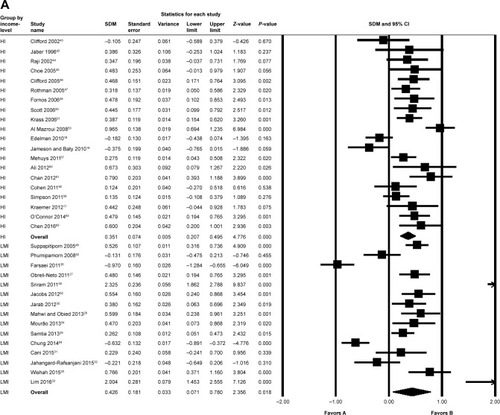
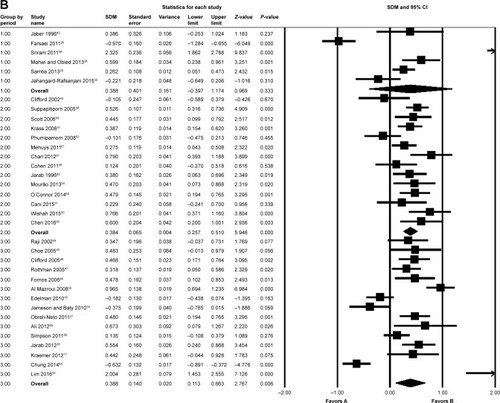
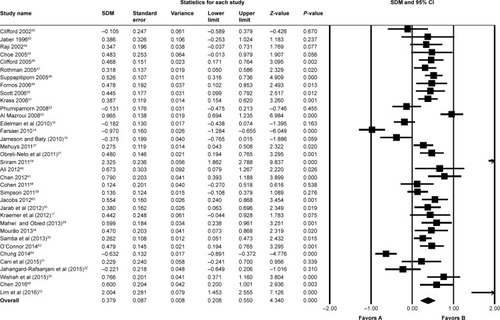
The overall pooled analysis for HbA1c change included 35 articles out of total 37 studies (Table S1). Owing to the high I2 value (89.380), the random-effects model was used. The result was significant and in favor of pharmacist-led intervention on HbA1c change (standard difference in mean values [SDM]: 0.379, 95% CI: 0.208–0.550, P=0.001), indicating the positive effect of pharmacist intervention in the improvement of clinical parameters in diabetes patients. The HbA1c level was 37.9% more reduced in the PC group than in the UC group ().
Figure 2 The overall comparison of PC and UC on the improvement of HbA1C level changes.
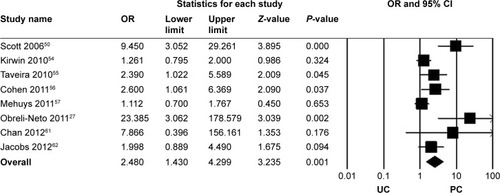
The proportion of patients achieving HbA1c goals was evaluated using eight articles that reported targeted outcomes out of total 37 included studies (Table S2). All the seven studies set the HbA1c target <7%, and the pooled result for the articles was significant and in favor of pharmacist intervention (OR: 2.48, 95% CI: 1.430–4.299, P=0.001). Approximately three times more patients achieved their HbA1c goal in the PC group compared to that in the UC group ().
Group analysis for income status and intervention period
The stratified meta-analysis showed that PC was significant in both 20 HIc (SDM: 0.351, 95% CI: 0.207–0.495) and 15 LMIc (SDM: 0.426, 95% CI: 0.071–0.780; ). The analysis for intervention period showed that interventions <6 months did not affect the clinical parameters of the patient (P=0.333). In the second group, 6–12 months of pharmacist intervention showed an improved effect, and the patients exhibited 36.4% more mean HbA1c level changes than the UC group (P<0.001). The longest intervention period of ≥12 months exhibited better effect on HbA1c reduction, with 38.8% more change in levels of HbA1c than the UC group (P=0.006; ).
Risk of bias score assessment by EPOC
The quality score of each study was graded by EPOC risk of bias tool by two independent researchers. As the selected primary literature had a low risk of bias in the domain of baseline outcome measure and characteristics, the baseline characteristics between two groups were similar. The reporting of results section had little risk either. However, the risks on blinding, allocation concealment, and contamination were high due to the nature of educational intervention studies (Table S3).
Publication bias
As widely accepted tools for publication bias, funnel plot visualization and Egger’s regression method were used to detect publication bias. Overall, the funnel plot and Egger’s regression (P=0.183) methods did not detect publication bias (Figure S1).
Discussion
In this study, we found a significant association between pharmacist-led pharmaceutical care and clinical diabetes management. This finding is corroborated by previous meta-analysis and systematic analysis for cardiovascular disease patients.Citation11,Citation12 Well-trained clinical pharmacists and a medical system utilizing active pharmacist-driven patient care can improve the quality, outcomes, and efficiency of patient management. Because this analysis included 20 studies from HIc and 15 from LMIc, the group analysis by income level showed that PC intervention was helpful in improving clinical outcomes in patients with diabetes in both HIc and LMIc. The positive outcomes observed in LMIc are particularly important considering the recent increase in the number of patients with diabetes and metabolic diseases in LMIc. The rapid spread of Western diet and lifestyle, as well as the improvement of socioeconomic status in LMIc, accelerates the incidence of obesity and chronic metabolic diseases in these countries. However, the introduction of clinical PC, such as MTM or multidisciplinary team care, is relatively rare in LMIc compared to that in HIc. A recent review reported that only 12% of clinical PC service is available for drug monitoring activities in Saudi Arabia.Citation24 Controlling the glucose levels at a recommended level is a difficult task, and therefore, <57% of these patients achieved control of blood glucose as measured by HbA1c concentrations.Citation25
A meta-analysis by Li et alCitation14 included 14 RCTs and reported higher mean change in HbA1c (0.68) than that in our study (0.370), and another meta-analysis by Poolsup et alCitation15 included 22 RCTs and reported the same mean change of 0.68 between PC and UC groups. We tried not to include heterogeneous population and excluded the research on adolescents and gestational diabetes patients. We excluded some studies that reported inadequate information to incorporate into meta-analysis that were included in the previous meta-analyses, which might be the reason of the different result. Furthermore, we included additionally 10 recently published studies conducted in LMIc,Citation26–Citation35 and this factor impacted the different results as well.
Generally, the care itself and the social/individual treatment costs of passive medical service administration are challenging. Therefore, more active and interactive multisec-tor collaboration work is essential to manage complicated diseases such as diabetes. In addition, the length of the intervention period is important in achieving adequate effects on clinical parameter improvement.
Another important finding of this study is that the longer intervention period of >6 months showed significant impact on the clinical parameters, while the intervention period of <6 months did not. These factors suggest the need for expanded training in primary care, with at least 6 months of education and intervention, to improve the comprehensiveness and quality of care provided to the growing number of patients with diabetes.
From the aspect of intervention tools, most interventions comprise a face-to-face method between pharmacists and patients, supplemented with leaflets and telephone outreach. The growing information age has enabled the availability of high-technology information and education tool kits. To educate diabetic patients, high-technology investments should be accelerated by country-level funding as suggested by a few studiesCitation36–Citation38 in which the participants showed a considerable decrease in the HbA1c level and several technological suggestions were provided. The technologies for health care providers include electronic database identifying and tracking patients and computer software designed for clinical decision support to the providers and telemedicine and telecare services, which currently equipped in HIc widely. Specific tool for patients focuses on the self-management skill improvement by the internet-, telephone- and mobile-based tools. If PC service model incorporates these high technologies into the PC, the care can produce much better clinical outcomes. Since most of the HIc have already adopted or are adopting pharmacist-led pharmaceutical care, the results of this study can encourage the utilization of pharmaceutical care in LMIc. A trend was observed in the following LMIc studies conducted in recent years: Obreli-Neto et al,Citation27 2011 (Brazil); Mahwi et al,Citation28 2013 (Iraq); Samtia et al,Citation29 2013 (Pakistan); Cani et al,Citation31 2015 (Brazil); Jahangard-Rafsanjani et al,Citation32 2015 (Iran); Wishah et al,Citation30 2015 (Jordan); and Lim et al,Citation33 2016 (Malaysia), except for Jahangard-Rafsanjani et al,Citation32 2015 (Iran) and Wishah et al,Citation30 2015 (Jordan), in that all the studies showed promising outcomes for pharmacist-led pharmaceutical care strategy in diabetes care in LMIc. A study evaluating the clinical outcome of blood pressure control reported that after stopping the PC, patient behavior returned to pre-intervention level, meaning consistent PC care is needed to better contribute to patients’ clinical outcome.Citation39
There are some limitations to our study. The risk of bias evaluated by EPOC guideline showed that some of the included publications lack methodical robust in blinding, allocation concealment, and reporting of contaminations. These factors can be considered in future clinical studies to make the results more reliable. The big heterogeneity of included studies is another limitation of this study. This heterogeneity is not from the clinical factor but is derived from statistical or unexplainable factors, so we adopted the random-effects model into the meta-analysis by using a statistic that indicates the percentage of variance in a meta-analysis that is attributable to study heterogeneity (I2). This model sets an assumption that the effects being estimated in the different studies are not identical but follow some distribution. Even though the random-effects model confronts some criticism but simulations have proven that this method is relatively robust even under wide range of distributional assumptions, both in estimating heterogeneityCitation40 and calculating an overall effect size.Citation41 Thus, by using random-effects model in our analysis, the heterogeneity of included studies has been overcome in our research.
Conclusion
Clinical pharmacists can make a comparative evaluation of medications based on sound knowledge of medications. The multitasking of clinical pharmacists, which includes healthy communication with health care workers and active interaction with patients, can lead to adherence to clinical therapeutic guidelines and medications. Pharmacist-led pharmaceutical care is a robust health care strategy maximizing therapeutic efficacy and improving lifelong care in diabetes patients in both HIc and LMIc.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We thank our colleagues of Drug Therapy Evaluation and Management (DrugTEAM™) group including Jung Mi Oh and Jeong-Hyun Yoon for their priceless support. This study was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI13C0731).
Supplementary materials
Figure S1 Publication bias visualized by funnel plot.
Abbreviation: SDM, standard difference in mean values.
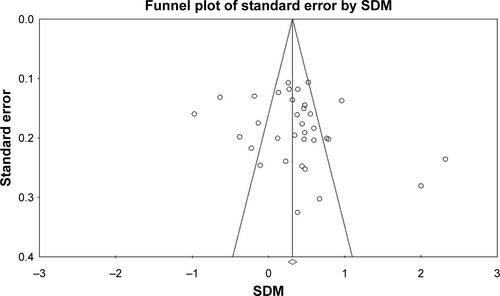
Table S1 The changes in HbA1C between PC group and UC group
Table S2 Proportion of patients achieving HbA1c goal between PC group and UC group
Table S3 Quality check for included studies (randomized controlled studies) by EPOC risk of bias
References
- EdelmanDFredricksonSKMelnykSDMedical clinics versus usual care for patients with both diabetes and hypertension: a random-ized trialAnn Intern Med20101521168969620513826
- JamesonJPBatyPJPharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trialAm J Manag Care201016425025520394460
- Obreli-NetoPRGuidoniCMde Oliveira BaldoniAEffect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patientsInt J Clin Pharm201133464264921544559
- JarabASAlqudahSGMukattashTLShattatGAl-QirimTRandom-ized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in JordanJ Manag Care Pharm201218751652622971205
- KraemerDFKradjanWABiancoTMLowJAA randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER studyJ Pharm Pract201225216917921987530
- MahwiTOObiedKARole of the pharmaceutical care in the management of patients with type 2 diabetes mellitusIJPSR20134413631369
- SamtiaAMRasoolMFRanjhaNMUsmanFJavedIA multifactorial intervention to enhance adherence to medications and disease-related knowledge in type 2 diabetic patients in Southern Punjab, PakistanTrop J Pharm Res2013125851856
- CaniCGLopesLSQueirozMNeryMImprovement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospitalClinics201570210210625789518
- Jahangard-RafsanjaniZSarayaniANosratiMEffect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trialDiabetes Educ201541112713525420946
- WishahRAAl-KhawaldehOAAlbsoulAMImpact of pharmaceutical care interventions on glycemic control and other health-related clinical outcomes in patients with type 2 diabetes: randomized controlled trialDiabetes Metab Syndr20159427127625301007
- LimPCLimKEmbeeZCHassaliMAThiagarajanAKhanTMStudy investigating the impact of pharmacist involvement on the outcomes of diabetes medication therapy adherence program Malaysia PakJ Pharm Sci2016292595601
- JaberLAHalapyHFernetMTunmalapalliSDiwakaranAEvaluation of a pharmaceutical care model on diabetes managementThe Annals of Pharmacotherapy1996302382438833557
- CliffordRMBattyKTDavisTMEDavisWSteinGStewartGA randomised controlled trial of a pharmaceutical care programme in high-risk diabetic patients in an outpatient clinicInt J Pharm Pract2002108589
- RajiAGomesHBeardJOMacDonaldPConlinPRA randomized trial comparing intensive and passive education in patients with Diabetes MellitusArch Intern Med20021621301130412038949
- ChoeHMMitrovichSDubayDHaywardRAKreinSLVijanSProactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trialAm J Manag Care20051125326015839185
- CliffordRMDavisWABattyKTDavisTMEEffect of a Pharmaceutical Care Program on Vascular Risk Factors in Type 2 Diabetes: The Fremantle Diabetes StudyDiabetes Care20052877177615793171
- RothmanRMaloneRBryantBShintaniAKCriglerBDewaltDAA randomized trial of a primary care–based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetesThe American Journal of Medicine200511827628415745726
- SuppapitipornSChindavijakBOnsanitSEffects of Diabetes Drug Counseling by Pharmacist, Diabetic Disease Booklet and Special Medication Containers on Glycemic Control of Type 2 Diabetes MellitusJ Med Assoc of Thai200588Suppl 4S134S141
- FornosJA´sNFA´sJCAGuerraMMEgeaBA pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in SpainPharm World Sci200628657216791717
- ScottDMT BoydSStephanMAugustineSCReardonTPOutcomes of pharmacist-managed diabetes care services in a community health centerAm J Health-Syst Pharm2006632116212217057049
- KrassIArmourCLMitchellBBrillantMDienaarRHughesJThe Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in AustraliaDiabetic Medicine200624677683
- PhumipamornSPongwecharakJSoorapanSPattharachayakulSEffects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetesPrim Care Diabetes200821313718684418
- MazrouiNRAKamalMMGhabashNMYacoutTAKolePLMcElnayJCInfluence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitusBr J Clin Pharmacol2008675547557
- FarsaeiSSabzghabaeeAMZargarzadehAHAminiMEffect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trialJ Res Med Sci2011161434921448382
- JamesonJPBatyPJPharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trialAm J Manag Care201016425025520394460
- CohenLBTaveiraTHKhatanaSAMDooleyAGPirragliaPAWuW-CPharmacist-Led Shared Medical Appointments for Multiple Cardiovascular Risk Reduction in Patients With Type 2 DiabetesThe Diabetes Educator201137800809
- MehuysEBortelLVBolleLDTongelenIVTongelenLAAnnemansLEffectiveness of a community pharmacist intervention in diabetes care: a randomized controlled trialJournal of Clinical Pharmacy and Therapeutics20113660261321143256
- SimpsonSLewanczukRMajumdarSSpoonerRTsuyukiRJohnsonJEffect of Adding Pharmacists to Primary Care Teams on Blood Pressure Control in Patients With Type 2 Diabetes: A random-ized controlled trialDiabetes Care201134202620929988
- SriramSChackLERamasamyRGhasemiARaviTKSabzghabaeeAMImpact of pharmaceutical care on quality of life in patients with type 2 diabetes mellitusJRMS201116412418
- AliMFSRobinsonPPhillipsGDohertyLMelnickPLamingLSinclairADhillonSImpact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled studyDiabetic Medicine2012c326c33.61.
- ChanC-WSiuS-CWongCKWLeeVWYA Pharmacist Care Program: Positive Impact on Cardiac Risk in Patients With Type 2 DiabetesJournal of Cardiovascular Pharmacology and Therapeutics2012171576421335480
- JacobsMSherryPTaylorLAmatoMTataronisGCushingGPharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) studyJ Am Pharm Assoc2012525613622
- MourãoAOFerreiraWRMartinsMAPharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trialInt J Clin Pharm2013351798623161124
- O’ConnorPSchmittdielJPathakRHarrisRNewtonKOhnsorgKRandomized trial of telephone outreach to improve medication adherence and metabolic control in adults with diabetesDiabete Care2014371233173324
- ChenJOuHLinTLaiEKaoYPharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: a randomized controlled trialInt J Clin Pharm2016381889526499503
- KirwinJLCunninghamRJSequistTDPharmacist Recommendations to Improve the Quality of Diabetes Care: A Randomized Controlled TrialJ Manag Care Pharm201016210411320178395
- TaveiraTHFriedmannPDCohenLBDooleyAGKhatanaSAMPirragliaPAPharmacist-Led Group Medical Appointment Model in Type 2 DiabetesThe Diabetes Educator20103610911719966072
- JacobsMSherryPTaylorLAmatoMTataronisGCushingGPharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) studyJ Am Pharm Assoc2012525613621
- ChungWWChuaSSLaiPSMChanSPEffects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetesPatient Preference and Adherence201481185119425214772
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization [webpage on the Internet]Diabetes: Global Report on DiabetesWorld Health Organization2016 Available from: http://www.who.int/diabetes/global-report/en/Accessed July 26, 2017
- OECD [webpage on the Internet] OECD. Stat2015 Available from: http://stats.oecd.org/index.aspx?DataSetCode=HEALTH_STATAccessed July 26, 2017
- SacksDBA1C versus glucose testing: a comparisonDiabetes Care201134251852321270207
- NathanDMGenuthSDiabetes Control and Complications Trial Research GroupThe effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitusN Engl J Med1993329149779868366922
- UK Prospective Diabetes Study (UKPDS) GroupIntensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33)Lancet19983528378539742976
- NathanDClearyPBacklundJDiabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research GroupIntensive diabetes treatment and cardiovascular disease in patients with type 1 diabetesN Engl J Med20053532643265316371630
- American Diabetes AssociationStandards of medical care in diabetes – 2012Diabetes Care201235suppl 1S11S6322187469
- World Health OrganizationGlobal Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020GenevaWorld Health Organization2013
- American Pharmacists Association, The National Association of Chain Drug Stores FoundationMedication therapy management in pharmacy practice. Core elements of an MTM service model version 2.0J Am Pharm Assoc (2003)200848334135318595820
- WermeilleJBennieMBrownIMcknightJPharmaceutical care model for patients with type 2 diabetes: integration of the community pharmacist into the diabetes team – a pilot studyPharm World Sci2004261182515018255
- SantschiVChioleroAColosimoALImproving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trialsJ Am Heart Assoc201432e00071824721801
- KoshmanSLCharroisTLSimpsonSHMcalisterFATsuyukiRTPharmacist care of patients with heart failure: a systematic review of randomized trialsArch Intern Med2008168768769418413550
- MachadoMBajcarJGuzzoGCEinarsonTRSensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes managementAnn Pharmacother200741101569158217712043
- LiXMaoMPingQEffect of pharmaceutical care programs on glycemic control in patients with diabetes mellitus: a meta-analysis of randomized controlled trialsJ Pharm Technol2010265255263
- PoolsupNSuksomboonNIntaratesMEffect of pharmacist’s interventions on glycemic control in diabetic patients: a systematic review and meta-analysis of randomized controlled trialsMahidol Univ J Pharm Sci20134041730
- EdelmanDFredricksonSKMelnykSDMedical clinics versus usual care for patients with both diabetes and hypertension: a random-ized trialAnn Intern Med20101521168969620513826
- KraemerDFKradjanWABiancoTMLowJAA randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER studyJ Pharm Pract201225216917921987530
- JamesonJPBatyPJPharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trialAm J Manag Care201016425025520394460
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementAnn Intern Med2009151426426919622511
- The World Bank [webpage on the Internet] Data Available from: https://data.worldbank.org/income-level/high-incomeAccessed July 26, 2017
- The Editorial Team of Effective Practice and Organisation of Care (EPOC), Cochrane Effective Practice and Organisation of Care (EPOC) [webpage on the Internet]EPOC Resources for Review AuthorsCochrane Library2017 Available from: http://epoc.cochrane.org/epoc-resources-review-authorsAccessed July 26, 2017
- HarbordRMEggerMSterneJAA modified test for small-study effects in meta-analyses of controlled trials with binary endpointsStat Med200625203443345716345038
- EggerMDavey SmithGSchneiderMMinderCBias in meta-analysis detected by a simple, graphical testBMJ199731571096296349310563
- MakeenHAClinical pharmacists as medication therapy experts in diabetic clinics in Saudi Arabia – not just a perception but a needSaudi Pharm J201725693994328951682
- CheungBMOngKLChernySSShamPCTsoAWLamKSDiabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006Am J Med2009122544345319375554
- FarsaeiSSabzghabaeeAMZargarzadehAHAminiMEffect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trialJ Res Med Sci2011161434921448382
- Obreli-NetoPRGuidoniCMde Oliveira BaldoniAEffect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patientsInt J Clin Pharm201133464264921544559
- MahwiTOObiedKARole of the pharmaceutical care in the management of patients with type 2 diabetes mellitusIJPSR20134413631369
- SamtiaAMRasoolMFRanjhaNMUsmanFJavedIA multifactorial intervention to enhance adherence to medications and disease-related knowledge in type 2 diabetic patients in Southern Punjab, PakistanTrop J Pharm Res2013125851856
- WishahRAAl-KhawaldehOAAlbsoulAMImpact of pharmaceutical care interventions on glycemic control and other health-related clinical outcomes in patients with type 2 diabetes: randomized controlled trialDiabetes Metab Syndr20159427127625301007
- CaniCGLopesLSQueirozMNeryMImprovement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospitalClinics201570210210625789518
- Jahangard-RafsanjaniZSarayaniANosratiMEffect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trialDiabetes Educ201541112713525420946
- LimPCLimKEmbeeZCHassaliMAThiagarajanAKhanTMStudy investigating the impact of pharmacist involvement on the outcomes of diabetes medication therapy adherence program Malaysia PakJ Pharm Sci2016292595601
- MourãoAOFerreiraWRMartinsMAPharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trialInt J Clin Pharm2013351798623161124
- JarabASAlqudahSGMukattashTLShattatGAl-QirimTRandom-ized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in JordanJ Manag Care Pharm201218751652622971205
- QuinnCCShardellMDTerrinMLBarrEABallewSHGruber-BaldiniALCluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose controlDiabetes Care20113491934194221788632
- BuDPanEWalkerJBenefits of information technology-enabled diabetes managementDiabetes Care20073051137114217322483
- AlhodaibH[webpage on the Internet]Information Technology in DM: DIAPEDIA: The living Textbook of Diabetes2014 Available from: https://www.diapedia.org/81040851628/rev/7Accessed July 26, 2017
- KicklighterCENelsonKMHumphriesTLDelateTAn evaluation of a clinical pharmacy-directed intervention on blood pressure controlPharm Pract (Granada)20064311011625214896
- KontopantelisESpringateDAReevesDA re-analysis of the Cochrane Library data: the dangers of unobserved heterogeneity in meta-analysesPLoS One201387e6993023922860
- KontopantelisEReevesDPerformance of statistical methods for meta-analysis when true study effects are non-normally distributed: a simulation studyStat Methods Med Res201221440942621148194
- JaberLAHalapyHFernetMTunmalapalliSDiwakaranAEvaluation of a pharmaceutical care model on diabetes managementThe Annals of Pharmacotherapy1996302382438833557
- CliffordRMBattyKTDavisTMEDavisWSteinGStewartGA randomised controlled trial of a pharmaceutical care programme in high-risk diabetic patients in an outpatient clinicInt J Pharm Pract2002108589
- RajiAGomesHBeardJOMacDonaldPConlinPRA randomized trial comparing intensive and passive education in patients with Diabetes MellitusArch Intern Med20021621301130412038949
- ChoeHMMitrovichSDubayDHaywardRAKreinSLVijanSProactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trialAm J Manag Care20051125326015839185
- CliffordRMDavisWABattyKTDavisTMEEffect of a Pharmaceutical Care Program on Vascular Risk Factors in Type 2 Diabetes: The Fremantle Diabetes StudyDiabetes Care20052877177615793171
- RothmanRMaloneRBryantBShintaniAKCriglerBDewaltDAA randomized trial of a primary care–based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetesThe American Journal of Medicine200511827628415745726
- SuppapitipornSChindavijakBOnsanitSEffects of Diabetes Drug Counseling by Pharmacist, Diabetic Disease Booklet and Special Medication Containers on Glycemic Control of Type 2 Diabetes MellitusJ Med Assoc of Thai200588Suppl 4S134S141
- FornosJA´sNFA´sJCAGuerraMMEgeaBA pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in SpainPharm World Sci200628657216791717
- ScottDMTBoydSStephanMAugustineSCReardonTPOutcomes of pharmacist-managed diabetes care services in a community health centerAm J Health-Syst Pharm2006632116212217057049
- KrassIArmourCLMitchellBBrillantMDienaarRHughesJThe Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in AustraliaDiabetic Medicine20072467768317523968
- PhumipamornSPongwecharakJSoorapanSPattharachayakulSEffects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetesPrim Care Diabetes200821313718684418
- MazrouiNRAKamalMMGhabashNMYacoutTAKolePLMcElnayJCInfluence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitusBr J Clin Pharmacol2008675547557
- KirwinJLCunninghamRJSequistTDPharmacist Recommendations to Improve the Quality of Diabetes Care: A Randomized Controlled TrialJ Manag Care Pharm201016210411320178395
- TaveiraTHFriedmannPDCohenLBDooleyAGKhatanaSAMPirragliaPAPharmacist-Led Group Medical Appointment Model in Type 2 DiabetesThe Diabetes Educator20103610911719966072
- CohenLBTaveiraTHKhatanaSAMDooleyAGPirragliaPAWuW-CPharmacist-Led Shared Medical Appointments for Multiple Cardiovascular Risk Reduction in Patients With Type 2 DiabetesThe Diabetes Educator201137800809
- MehuysEBortelLVBolleLDTongelenIVTongelenLAAnnemansLEffectiveness of a community pharmacist intervention in diabetes care: a randomized controlled trialJournal of Clinical Pharmacy and Therapeutics20113660261321143256
- SimpsonSLewanczukRMajumdarSSpoonerRTsuyukiRJohnsonJEffect of Adding Pharmacists to Primary Care Teams on Blood Pressure Control in Patients With Type 2 Diabetes: A random-ized controlled trialDiabetes Care201134202620929988
- SriramSChackLERamasamyRGhasemiARaviTKSabzghabaeeAMImpact of pharmaceutical care on quality of life in patients with type 2 diabetes mellitusJRMS201116412418
- AliMFSRobinsonPPhillipsGDohertyLMelnickPLamingLSinclairADhillonSImpact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled studyDiabetic Medicine2012c326c333
- ChanC-WSiuS-CWongCKWLeeVWYA Pharmacist Care Program: Positive Impact on Cardiac Risk in Patients With Type 2 DiabetesJournal of Cardiovascular Pharmacology and Therapeutics2012171576421335480
- JacobsMSherryPTaylorLAmatoMTataronisGCushingGPharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) studyJ Am Pharm Assoc2012525613621
- O’ConnorPSchmittdielJPathakRHarrisRNewtonKOhnsorgKRandomized trial of telephone outreach to improve medication adherence and metabolic control in adults with diabetesDiabete Care2014371233173324
- ChungWWChuaSSLaiPSMChanSPEffects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetesPatient Preference and Adherence201481185119425214772
- ChenJOuHLinTLaiEKaoYPharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: a randomized controlled trialInt J Clin Pharm2016381889526499503