Abstract
Purpose
Hyperleptinemia has been independently associated with human cardiovascular (CV) diseases. Accordingly, we evaluate the association between serum leptin and future CV events in patients with coronary artery disease (CAD).
Patients and methods
This study enrolled 98 patients with CAD from January to December 2012. The primary endpoint included incidences of major adverse CV events and hospitalization. Patients follow-up had been completed on June 30, 2017.
Results
After a median follow-up of 52 months, 43 CV events had occurred. Patients with CV events had higher systolic blood pressure (P = 0.030), total cholesterol (P = 0.034), C-reactive protein (P = 0.018), and serum leptin levels (P = 0.001) than those without CV events. Kaplan–Meier analysis showed greater cumulative incidences of CV events in the high leptin group (median leptin concentration >6.03 ng/mL) than in the low leptin group (log-rank P = 0.012). Multivariate Cox regression analysis showed that triglyceride (HR: 1.010; 95% CI: 1.001–1.018; P = 0.022) and leptin levels (HR: 1.054; 95% CI: 1.026–1.082; P < 0.001) were independently associated with CV events in patients with CAD.
Conclusion
Serum leptin levels could serve as a biomarker for future CV events in patients with CAD.
Introduction
Coronary artery disease (CAD), one of the leading causes of death and disability worldwide, has been a significant health problem and global burden.Citation1 According to data from the United States, an estimated 15.4 million Americans over the age of 20 had developed CAD from 2007 to 2010, with the reported prevalence increasing with age for both genders.Citation1 Another study also reported an estimated 17.5 million deaths in 2005 due to CAD alone, a number that is expected to increase by 137% in males and 120% in females by 2020 in developing countries.Citation2 Patients with CAD usually remain asymptomatic until their first clinically significant manifestation of pathogenic conditions, such as myocardial infarction (MI), cardiac arrest, stroke, or death from cardiovascular (CV) events.
Leptin, a 16-kDa obese gene product primarily secreted by white adipocytes, is the most prominent appetite- and energy-regulating peptide discovered in the early 1990s.Citation3 Hyperleptinemia has been implicated in inflammatory, metabolic, and homeostatic factors involved in obesity, hypertension, and cardiovascular disease (CVD).Citation4,Citation5 Studies have revealed that leptin and its receptor’s isoforms are expressed in cardiomyocytes, vascular smooth muscle cells, and endothelia.Citation6–Citation9 Moreover, leptin resistance with hyperleptinemia has been involved in enhancing endothelial oxidative stress, stimulating the proliferation of vascular smooth muscle cells, inducing neointimal and medial thickening of injured arterial vascular walls, stimulating the formation of reactive oxygen species, and activating the renin–angiotensin–aldosterone system, which together result in the imbalance between vasoconstriction and vasodilatation with the consequent development of CVD.Citation5,Citation9
Although the link between adipokines and CAD has been well documented, the association between serum leptin and long-term CV outcomes in patients with CAD has been rarely reported.Citation4,Citation10 Moreover, conflicting data are available concerning the association of leptin with future development of CVD.Citation11–Citation13 In LIPID study, plasma leptin was a significant and independent predictor of recurrent CVD in men with earlier acute coronary syndromes.Citation11 Another study also noted high plasma leptin levels predict the congestive heart failure or cardiac death and acute coronary syndrome or stroke in patients with CAD that were followed up for two years.Citation12 However, serum leptin level is not associated with risk of CVD but is associated with risk of diabetes in elderly.Citation13 Therefore, the current study aims to determine the relationship between serum leptin levels and cardiometabolic risk factors among patients with CAD.
Patients and methods
Patients
Patients with >50% stenosis in any segment after coronary angiography were identified as having CAD. After reviewing the patients’ medical records between January and December 2012, 112 participants with CAD in a medical center in Hualien, eastern Taiwan were enrolled; 14 participants were excluded because of acute infection (n = 3), malignancy (n = 3), coronary bypass graft surgery (n = 2), and refusal to provide informed consent (n = 6). Finally, a total of 98 participants with CAD had been enrolled in this cross-sectional study. Using standard mercury sphygmomanometers with appropriate cuff sizes, morning BP levels of all participants who had rested for at least 10 minutes were measured on the right arm by trained staff. Systolic blood pressure (SBP) and Diastolic blood pressure (DBP) were measured three times at 5-minute intervals and were averaged for analysis. Hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mmHg or having received any anti-hypertensive drugs in the past two weeks according to the Eighth Joint National Committee guideline. Patients having fasting plasma glucose levels ≥126 mg/dL or those using oral hypoglycemic medications or insulin were diagnosed with diabetes mellitus (DM).Citation14 This study had been approved by the Protection of the Human Subjects Institutional Review Board of Tzu Chi University and Hospital. All participants gave written informed consent prior to study participation.
Anthropometric analysis
Body weight and height were measured to the nearest 0.5 kg and 0.5 cm, respectively, with participants in light clothing without shoes. Body mass index was calculated using Quetelet’s formula: weight in kilograms divided by the height in meters squared.Citation5,Citation15–Citation17
Biochemical investigations
After an eight-hour overnight fast, blood samples (approximately 5 mL) collected from all participants were immediately centrifuged at 3,000 g for 10 minutes. Serum levels of blood urea nitrogen, creatinine, fasting glucose, total cholesterol (TCH), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and C-reactive protein (CRP) were determined using an autoanalyzer (COBAS Integra 800; Hoffmann-La Roche Ltd., Basel, Switzerland).Citation5,Citation15–Citation17 Serum leptin concentrations were determined using a commercially available enzyme immunoassay (SPI Bio Inc., Sherbrooke, QC, Canada).Citation5,Citation15 The estimated glomerular filtration rate was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.Citation16,Citation17
CV event monitoring
The primary endpoint was the incidence of major adverse cardiovascular events (MACEs), including death from CV causes, cardiac arrest, MI, stroke, nonfatal stroke or other arterial thrombotic events, and hospitalization due to CV conditions such as unstable or progressive angina and heart failure. The follow-up time interval (months) had not been estimated until the last hospital outpatient or inpatient record had been reviewed or the last telephone interview had been conducted (June 30, 2017). Moreover, the event time (months) had not been counted until the first MACE had occurred. Patient follow-up had been performed by a study nurse who was unaware of the participants’ baseline measurements and the study protocol.
Statistical analysis
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 19.0 (IBM Corporation, Armonk, NY, USA). The distribution pattern of the variables was determined using the Kolmogorov–Smirnov test. Normally distributed variables were expressed as mean ± standard deviation and with differences between patients being compared using the Student’s independent t-test (two-tailed). Data not normally distributed were expressed as medians and interquartile ranges with differences between patients being compared using the Mann–Whitney U test (TG, fasting glucose, creatinine, CRP, and leptin). Data regarding the number of patients were analyzed using the chi-squared test. Kaplan–Meier survival curves with a log-rank test were used to estimate event-free survival during follow-up based on median leptin concentrations. Univariate and multivariate Cox regression models were used to examine factors associated with CV events. All covariates were included in the multivariate Cox regression model. A P-value <0.05 was considered statistically significant.
Results
Demographic, clinical, and biochemical characteristics of the 98 patients with CAD are shown in . A total of 47 (48.0%) and 76 (77.6%) patients had DM and hypertension, respectively. The high leptin group (median leptin concentration >6.03 ng/mL) was older (P = 0.024), had higher serum levels of CRP (P = 0.015) and leptin (P<0.001), and was shorter in height (P = 0.027) than the low leptin group (median leptin concentration ≤6.03 ng/mL). Drugs used by the patients included angiotensin-converting enzyme inhibitors (ACEi; n = 29; 29.6%), angiotensin receptor blockers (ARB; n = 37; 37.8%), β-blockers (n = 58; 59.2%), calcium channel blockers (CCB; n = 33; 33.7%), statins (n = 71; 72.4%), and fibrate (n = 14; 14.3%). No statistically significant difference in sex, comorbidity with DM or hypertension, and use of ACEi, ARB, β-blockers, CCB, statins, or fibrate had been found between the two leptin groups.
Table 1 Clinical variables of the 98 coronary artery disease patients according to serum leptin levels
After a median follow-up of 52 months, 43 CV events had occurred. Patients with CV events had higher SBP (P = 0.030), serum TCH (P = 0.034), CRP (P = 0.018), and leptin (P = 0.001) levels than those without CV events. No statistically significant differences in sex, comorbidity with DM or hypertension, and use of ACEi, ARB, β-blockers, CCB, statins, or fibrate had been observed between those with and without CV events ().
Table 2 Clinical variables of the 98 coronary artery disease patients with or without cardiovascular event
Kaplan–Meier analysis showed that the cumulative incidence of CV events was greater in the high leptin group (median leptin concentration >6.03 ng/mL) than in the low leptin group (log-rank P = 0.012) (). Univariate Cox regression analysis revealed that SBP (HR: 1.018; 95% CI: 1.003–1.034; P = 0.021), TCH (HR: 1.010; 95% CI: 1.001–1.020; P = 0.035), TG (HR: 1.004; 95% CI: 1.001–1.006; P = 0.006), CRP (HR: 4.329; 95% CI: 2.027–9.246; P < 0.001), and leptin (HR: 1.043; 95% CI: 1.025–1.062; P < 0.001) levels were positively associated with CV events in patients with CAD. Furthermore, multivariate Cox regression analysis showed that TG (HR: 1.010; 95% CI: 1.001–1.018; P = 0.022) and leptin (HR: 1.054; 95% CI: 1.026–1.082; P < 0.001) levels were independently associated with CV events in patients with CAD ().
Figure 1 Kaplan–Meier analysis of cardiovascular events in 98 patients with coronary artery disease according to median serum leptin levels.
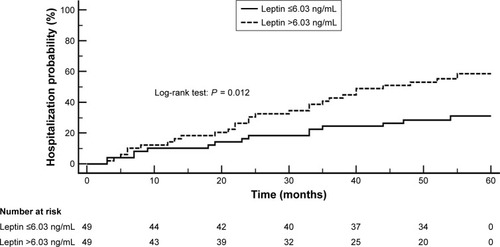
Table 3 Cox regression of univariate and multivariate significant predictors of cardiovascular events among the 98 patients with coronary artery disease
Discussion
The results presented herein revealed that patients with CAD who developed MACEs during follow-up had higher fasting leptin levels than those who did not. Moreover, fasting serum leptin and TG levels were independently associated with increased risk for MACEs among patients with CAD.
Aging is usually associated with hyperleptinemia and leptin resistance, which may aggravate age-associated pathologies, including metabolic syndrome and CVD.Citation18,Citation19 The present study also revealed that patients in the high leptin group were older than those in low leptin group. Hypertension has been a major independent risk factor for CAD across all age, gender, and race groups.Citation20 A previous large-scale meta-analysis involving approximately 1 million adults had revealed that BP was correlated with fatal CAD across all ages and that an overall SBP increase of 20 mmHg doubles the risk for fatal coronary events.Citation21 A recent systematic review and meta-analysis had also confirmed that intensive BP reductions had additional benefits on major CV events and all-cause mortality.Citation22 Accordingly, the present study also revealed that patients with CAD who developed a new MACE had significantly higher SBP than those who did not, suggesting that BP reduction is important for preventing further MACE development in patients with CVD. Several previous studies have suggested that inflammation and dyslipidemia may play important roles in not only the occurrence and progression of coronary atherosclerotic lesions but also treatment outcome after intervention.Citation23–Citation25 The present study also observed significantly higher CRP values in the high serum leptin group than in low leptin group. Moreover, significantly higher TCH and CRP levels were found in those who developed a new MACE than in those who did not, which is consistent with a previous study by Xu et al.Citation25
In contrast with traditional risk factors for CAD, growing evidence has revealed that leptin resistance with hyperleptinemia, a phenomenon encountered in obesity and insulin resistance, plays an important role in the occurrence, severity, and extent of CV events.Citation10,Citation15,Citation26,Citation27 Although the definitive role of leptin in the development of CVD remains to be clarified. One study noted lower serum leptin level that measured 7 days after acute MI onset is associated with a high incidence of adverse events in Japanese patients.Citation28 Another study noted low serum leptin level is independent predictors of high risk coronary anatomy as defined by an integrated coronary computed tomography angiography risk score in patients with stable chest pain.Citation29 Our previous study and several other reports had found that high circulating leptin levels were positively correlated with the number of stenotic coronary arteries.Citation15,Citation26 Hyperleptinemia was associated with heart failure and impaired diastolic function in patients with CAD.Citation30 In addition, leptin exhibited profibrotic effects on the myocardium, which could induce myocardial fibrosis and aggravate the severity of heart disease.Citation31 Leptin is also an independent predictor of CV event recurrence in males with earlier acute coronary syndromes, while hyperleptinemia has been positively associated with restenosis rate after percutaneous coronary intervention.Citation11 Moreover, after both univariate and multivariate Cox regression analyses, a very recent study revealed that circulating leptin levels could significantly predict the occurrence of not only MACEs, such as short-term congestive heart failure events, cardiac deaths, or acute coronary syndromes, but also strokes.Citation12 Our present findings also revealed that patients with CAD who developed a new MACE had significantly higher serum leptin levels than those who did not. Taken together, whether the complex interaction of leptin with metabolic and CV system could account for a “CAD progression” effect needs further study.
The present study showed that hyperleptinemia and hypertriglyceridemia independently and significantly increased the risk of MACE in patients with CAD after univariate and multivariate Cox regression analyses. The mechanism by which leptin induces adverse CV events among patients with CAD is likely to be multifactorial. Leptin had also been identified as an adipokine that could potentially be involved in crosstalk between adipose tissues and the vascular wall.Citation7,Citation8,Citation31 Hyperleptinemia had been associated with intima–media thickness of the common carotid artery, smooth muscle cell migration and proliferation, and coronary artery calcification, all of which were markers of asymptomatic atherosclerosis and important pathological vascular changes in patients with hypertension and CAD.Citation7,Citation31–Citation33 The direct influence of hypertension on future CV events has been well documented. A previous study also reported that hyperleptinemia was positively associated with hypertension.Citation34 Based on findings from Cox regression analyses, the present study confirmed that elevated SBP increased the risk of MACEs among patients with CAD, suggesting that hyperleptinemia may aggravate hypertension-induced MACEs.
CRP, a well-established biomarker of inflammation, has been positively associated with CAD presence and progression.Citation24 Previous studies had revealed that high leptin and CRP levels increase the risk for CV death in Western countries and Taiwan.Citation35,Citation36 Leptin has been associated with a pro-inflammatory, atherogenic milieu, while several studies had reported that serum leptin levels were positively correlated with hs-CRP levels.Citation37,Citation38 Our previous study also revealed that elevated CRP levels were independent predictors of hyperleptinemia among patients with hypertension.Citation5 Accordingly, the current study revealed that among patients with CAD, those who developed a new MACE had significantly higher CRP levels than those who did not. Associations between leptin and pro-atherogenic blood lipids, along with leptin’s pro-inflammatory activity and role in insulin resistance and endothelial dysfunction, comprise the major mechanisms for triggering atherosclerosis and further aggravating CVD.Citation10
Limitations
Some limitations to the present study are worth mentioning. First, the limited number of patients with MACE, uneven distribution of sex, not included obesity subjects, obtained from a single center, as well as the lack of evaluation regarding some lifestyle habits that could influence the occurrence of MACE, such as smoking or alcohol drinking, may restrict the predictive power of the current study. Second, although several of the medications used by our study population may influence their atherosclerotic and inflammatory status, the present study showed that ACEi, ARB, β-blockers, CCB, statins, and fibrates had no influence on circulating leptin levels or new MACE development. Many independent studies have reported that the pleiotropic effects of statins included modulation of serum leptin levels, while treatment with atorvastatin lowered circulating leptin levels in patients with CAD.Citation39,Citation40 A previous study also revealed that lipid profiles, including TG, TCH, LDL-C, and HDL-C, have poor predictive values for the severity of coronary diseases due to the influence of drug therapy.Citation41 Further studies are needed to evaluate the impact of the aforementioned medication on serum leptin concentrations and new MACE development among patients with CAD.
Conclusion
In addition to the traditional risk factors for CAD, hyperleptinemia may serve as a novel, independent risk factor for CV events among patients with CAD and may increase the predictive power for MACEs. Moreover, while a previous study revealed that circulating leptin levels could serve as an additional tool for short-term risk stratification of patients with CAD,Citation26 our results showed that such a finding could be further extended to include long-term CV events among patients with CAD. Further studies are needed to evaluate the direct cause-and-effect association between serum leptin and CAD can be established.
Acknowledgments
This study was supported by a grant from the Buddhist Tzu Chi General Hospital, Hualien, Taiwan (TCRD101-03). MC Chen, JH Wang, and BG Hsu conceived and designed the experiments. CJ Lee and JH Wang performed the experiments. CJ Lee and BG Hsu analyzed the data. MC Chen and BG Hsu wrote the manuscript. All authors reviewed and approved the final version of this paper.
Disclosure
The authors report no conflicts of interest in this work.
References
- GoASMozaffarianDRogerVLHeart disease and stroke statistics – 2014 update: a report from the American Heart AssociationCirculation20141293e28e29224352519
- JayashreeSArindamMVijayKVGenetic epidemiology of coronary artery disease: an Asian Indian perspectiveJ Genet201594353954926440097
- GhalandariHHosseini-EsfahaniFMirmiranPThe association of polymorphisms in leptin/leptin receptor genes and ghrelin/ghrelin receptor genes with overweight/obesity and the related metabolic disturbances: a reviewInt J Endocrinol Metab2015133e1907326425125
- WannametheeSGTchernovaJWhincupPPlasma leptin: associations with metabolic, inflammatory and haemostatic risk factors for cardiovascular diseaseAtherosclerosis2007191241842616712853
- ChenMCHsuBGLeeCJHyperleptinemia positively correlates with cardiometabolic syndrome in hypertensive patientsInt J Clin Exp Pathol201691295912967
- RajapurohitamVGanXTKirshenbaumLAKarmazynMThe obesity-associated peptide leptin induces hypertrophy in neonatal rat ventricular myocytesCirc Res200393427727912893740
- OdaATaniguchiTYokoyamaMLeptin stimulates rat aortic smooth muscle cell proliferation and migrationKobe J Med Sci200147314115011729375
- HeidaNMLeifheit-NestlerMSchroeterMRLeptin enhances the potency of circulating angiogenic cells via src kinase and integrin (alpha)vbeta5: implications for angiogenesis in human obesityArterioscler Thromb Vasc Biol201030220020619910644
- BouloumieAMarumoTLafontanMBusseRLeptin induces oxidative stress in human endothelial cellsFaseb J199913101231123810385613
- LiZYWangPMiaoCYAdipokines in inflammation, insulin resistance and cardiovascular diseaseClin Exp Pharmacol Physiol2011381288889621910745
- SöderbergSColquhounDKeechALeptin, but not adiponectin, is a predictor of recurrent cardiovascular events in men: results from the LIPID studyInt J Obes2009331123130
- PuurunenVPKiviniemiALepojärviSLeptin predicts short-term major adverse cardiac events in patients with coronary artery diseaseAnn Med201749544845428300429
- WelshPMurrayHMBuckleyBMLeptin predicts diabetes but not cardiovascular disease: results from a large prospective study in an elderly populationDiabetes Care200932230831019001191
- AlbertiKGZimmetPZDefinitionZPZDefinition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultationDiabet Med19981575395539686693
- TsaiJPWangJHChenMLAssociation of serum leptin levels with central arterial stiffness in coronary artery disease patientsBMC Cardiovasc Disord2016168027151106
- WangJHLeeCJYangCFChenYCHsuBGSerum resistin as an independent marker of aortic stiffness in patients with coronary artery diseasePLoS One2017128e018312328806778
- ChenMCHsuBGLeeCJYangCFWangJHHigh serum adipocyte fatty acid binding protein level as a potential biomarker of aortic arterial stiffness in hypertensive patients with metabolic syndromeClin Chim Acta201747316617228860092
- MaXHMuzumdarRYangXMAging is associated with resistance to effects of leptin on fat distribution and insulin actionJ Gerontol A Biol Sci Med Sci2002576B225B23112023258
- Roszkowska-GancarzMJonasMOwczarzMAge-related changes of leptin and leptin receptor variants in healthy elderly and long-lived adultsGeriatr Gerontol Int201515336537124612398
- RosendorffCLacklandDTAllisonMTreatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of HypertensionCirculation201513119e435e47025829340
- LewingtonSClarkeRQizilbashNAge-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiesLancet200236093491903191312493255
- XieXAtkinsELvJEffects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysisLancet20163871001743544326559744
- WilsonPWEvidence of systemic inflammation and estimation of coronary artery disease risk: a population perspectiveAm J Med200812110 Suppl 1S15S2018926165
- ZairisMNAmbroseJAManousakisSJThe impact of plasma levels of C-reactive protein, lipoprotein (a) and homocysteine on the long-term prognosis after successful coronary stenting: The Global Evaluation of New Events and Restenosis After Stent Implantation StudyJ Am Coll Cardiol20024081375138212392824
- XuHYQiaoSBZhangJFDongQTLiJJDifferent impacts of C-reactive protein and lipid profile on coronary lesions following a percutaneous coronary interventionCoron Artery Dis201223318118722336660
- KhafajiHABenerABRizkNMAl SuwaidiJElevated serum leptin levels in patients with acute myocardial infarction; correlation with coronary angiographic and echocardiographic findingsBMC Res Notes2012526222642879
- MoritaYMaedaKKondoTImpact of adiponectin and leptin on long-term adverse events in Japanese patients with acute myocardial infarction. Results from the Nagoya Acute Myocardial Infarction Study (NAMIS)Circ J201377112778278523924849
- CaselliCde GraafMALorenzoniVHDL cholesterol, leptin and interleukin-6 predict high risk coronary anatomy assessed by CT angiography in patients with stable chest painAtherosclerosis20152411556125966440
- PuurunenVPLepojärviESPiiraOPHigh plasma leptin levels are associated with impaired diastolic function in patients with coronary artery diseasePeptides201684172127524739
- ZibadiSCordovaFSlackEHWatsonRRLarsonDFLeptin’s regulation of obesity-induced cardiac extracellular matrix remodelingCardiovasc Toxicol201111432533321744298
- CicconeMVettorRPannacciulliNPlasma leptin is independently associated with the intima-media thickness of the common carotid arteryInt J Obes Relat Metab Disord200125680581011439293
- LarsenBALaughlinGACumminsKBarrett-ConnorEWasselCLAdipokines and severity and progression of coronary artery calcium: findings from the Rancho Bernardo StudyAtherosclerosis20172651628825974
- WeissgerberAScholzMTerenAThe value of noncoronary atherosclerosis for identifying coronary artery disease: results of the Leipzig LIFE Heart StudyClin Res Cardiol2016105217218126362881
- AgataJMasudaATakadaMHigh plasma immunoreactive leptin level in essential hypertensionAm J Hypertens19971010 Pt 1117111749370390
- AmrockSMWeitzmanMEffect of increased leptin and C-reactive protein levels on mortality: results from the National Health and Nutrition Examination SurveyAtherosclerosis201423611624998933
- ChiuFHChuangCHLiWCWcLThe association of leptin and C-reactive protein with the cardiovascular risk factors and metabolic syndrome score in Taiwanese adultsCardiovasc Diabetol2012114022533665
- ViikariLAHuupponenRKViikariJSRelationship between leptin and C-reactive protein in young Finnish adultsJ Clin Endocrinol Metab200792124753475817878255
- NtyintyaneLPanzVRaalFJGillGLeptin, adiponectin, and high-sensitivity C-reactive protein in relation to the metabolic syndrome in urban South African blacks with and without coronary artery diseaseMetab Syndr Relat Disord20097324324819462476
- KrysiakRLabuzekKOkopieńBEffect of atorvastatin and fenofibric acid on adipokine release from visceral and subcutaneous adipose tissue of patients with mixed dyslipidemia and normolipidemic subjectsPharmacol Rep20096161134114520081249
- SunYMLiJLuanYWangLFEffect of statin therapy on leptin levels in patients with coronary heart diseasePeptides20103161205120720338208
- GumanovaNGGavrilovaNEChernushevichOIKotsAYMetelskayaVARatios of leptin to insulin and adiponectin to endothelin are sex-dependently associated with extent of coronary atherosclerosisBiomarkers2017223–423924527300270
