Abstract
Background
When prescribing antiplatelet agents, physicians face the challenge of protecting patients from thromboembolic events without inducing bleeding damage. However, especially in the perioperative period, the use of these medications requires a carefully balanced assessment of their risks and benefits.
Objective
To conduct a systematic review to check whether the antiplatelet agent is to be maintained or suspended in the perioperative period of noncardiac surgeries.
Search strategy
A comprehensive literature search using Science Direct, Scopus, MEDLINE-PubMed, and Web of Science was undertaken.
Selection criteria
Clinical trials of noncardiac surgeries with patients taking regular anti-platelet therapy, published between 2013 and 2018.
Results
A total of 1,302 studies were initially identified, with only four meeting the inclusion criteria. The selected studies were conducted in different countries such as, including India (2), Serbia (1), and the USA (1). The age group was similar in all studies, from 61 to 75 years. The most frequent surgery was related to tooth extraction and transurethral resection of bladder cancer. There was a group of patients who used single antiplatelet agents and groups who used single therapy and double therapy. Acetylsalicylic acid was the common drug in all studies.
Conclusion
It was concluded that the clinical trials were classified as good quality and that it was not necessary to suspend antiplatelet therapy prior to surgical procedures such as dental extraction and transurethral resection of bladder cancer. It should be noted that it is necessary to jointly evaluate the type of antiplatelet agent, the thrombotic risk of the patient, and the hemorrhagic risk of the surgical procedure.
Introduction
Cardiovascular diseases (CVD) are the leading cause of premature morbidity and mortality in the world, with accelerated growth in developing countries.Citation1–Citation3 It is believed that by 2020, more than 80% of CVD will occur in low- and middle-income countries.Citation4 Major cardiovascular complications (acute myocardial infarction – AMI – nonfatal, cardiac arrest, and cardiovascular death) during the perioperative period have been observed, which are also strongly associated with mortality at 30 days after a noncardiac surgical procedure.Citation5–Citation9
In 2014, Botto et alCitation10 affirmed that cardiac complications are the main cause of postoperative death in patients undergoing noncardiac surgeries, and millions of patients with high cardiovascular risk are subjected annually to these types of surgeries.Citation11–Citation13 Parallel to this, the use of antiplatelet agents for secondary prevention of cardio- and cerebrovascular diseases has increased considerably.Citation14
While providing protection ischemic, antiplatelet drugs expose patients to a degree of risk of bleeding,Citation15–Citation17 a justification that leads many surgeons to recommend to patients the interruption of these medications preoperatively. On the other hand, the withdrawal of the antiplatelet agent in the perioperative period may be associated with mortal thrombotic complications.Citation16,Citation18,Citation19
Thus, surgeons are frequently confronted with decision-making on whether or not to discontinue antiplatelet therapy during the perioperative period for noncardiac surgeries,Citation15,Citation17,Citation20 because they must take into account the potential protective effect of antiplatelet therapy vs the risk of bleeding caused by these drugs;Citation15,Citation17 so, there is no unanimous opinion among medical professionals, regardless of whether the patient’s use of antiplatelets is intended for primary or secondary prevention of cardiovascular events.Citation20,Citation21
The present systematic review is justified by the perspective of helping surgeons, mainly, in the decision-making regarding the dilemma of maintaining or not the antiplatelet agents in the perioperative period of noncardiac surgeries. Thus, its main objective is to conclude, through clinical trials, whether the antiplatelet agents should be maintained or suspended in the perioperative period of noncardiac surgeries.
Methods
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement and supplemented by guidance from the Cochrane Collaboration Handbook. A protocol of this systematic review was designed a priori and was registered in the PROSPERO database (registration number 93420).
Search strategy
Four databases (Internet sources) were used to search for appropriate papers that fulfilled the purpose of this study. Those included the National Library of Medicine (MEDLINE-PubMed), Science Direct, Web of Science, and Scopus, using different combinations of the following keywords: “platelet aggregation inhibitors,” “antiplatelet agent,” “clinical trial,” “surgery.” The databases were searched for studies conducted from January 2013 to February 2018. The research strategy was designed to identify studies on patients undergoing noncardiac surgeries who regularly use antiplatelet agents. Citations were manually limited to clinical trials of noncardiac surgeries. Additional papers were included in our study after analyses of all references from the selected articles. We did not contact the investigators nor did we try to identify unpublished data.
Study selection
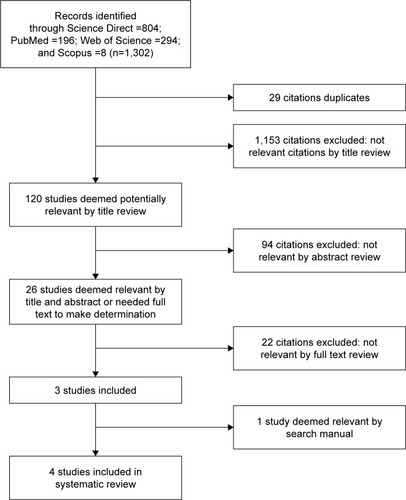
All electronic search titles, selected abstracts, and full-text articles were independently reviewed by a minimum of two reviewers (JMDM and FOC). Disagreements over inclusion/exclusion criteria were resolved by reaching a consensus. The following inclusion criteria were applied: clinical trials, human studies, noncardiac surgeries, regular use of anti-platelet agents, and studies between 2013 and 2018. Studies were excluded according to the following exclusion criteria: studies that did not fit the above characteristics, review articles, meta-analyses, abstracts, conference proceedings, editorials/letters, and case reports ().
Table 1 Description of each included RCT: country, population, type of surgery, description of control group, and outcomes measures
Data extraction and risk of bias assessment
Data were extracted by one reviewer using standardized forms and were checked by a second reviewer. The following information was extracted from all studies: population (n) of each study, average age (in years), type of surgery, use of antiplatelet agents (the studies did not indicate how many days the patients had to interrupt the therapy with the anti-platelet agent before the surgeries), results, limitations of the study, and conclusions.
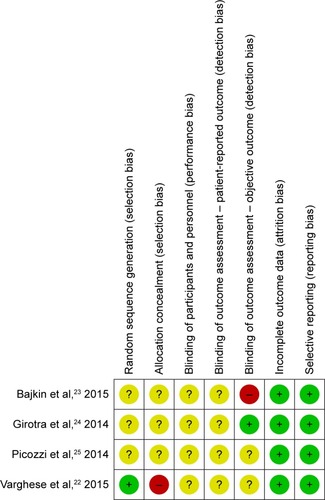
We assessed the risk of bias according to the Cochrane guidelines for randomized controlled trials. We assessed seven domains for evaluation: sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other potential sources of bias. We rated the risk of bias as low, unclear, or high according to established criteria. And the total score was obtained by assigning 1 point for each “low” answer and 0 points for “unclear” or “high” answers, for a total quality score ranging from 0 to 7. A study was considered with low quality when <2 of 7 items were met. Two investigators independently (JMDM and FOC) conducted this assessment, and any disagreements were resolved by consensus.
Results
Selection of studies
The process followed for article selection is presented in . We found 804 studies on Science Direct, 8 on the Scopus, 294 on the Web of Science, and 196 on PubMed, so a total of 1,302 articles were identified. After rejecting duplicate articles, we proceeded with the reading of 1,273 titles and abstracts. Finally, 26 articles were selected for full reading. After the assessment of and rejection of articles not shown in full, duplicates, letters to the reader, case studies, articles published before the year 2013, articles that were not in English, Spanish, or Portuguese, or those whose theme did not include the approach of this study, three articles remained. At the end, we added one article found on manual searching of the literature, and so four remaining articles were finally selected (). There was a high level of agreement on inclusion/exclusion between the two investigators who screened the retrieved articles (κ index >88%).
Characteristics of included studies
The selected studies were conducted in different countries such as India (2), Serbia (1), and the USA (1). They were published between the years 2013 and 2015 ().
The sample size of each study varied a little: there was an article covering 160 patients to one study with 1,121 patients, but the age group was similar in all studies, from 61 to 75 years. The most frequent surgery was related to tooth extractionCitation22–Citation24 and transurethral resection of bladder cancer.Citation25 Acetylsalicylic acid (ASA) was the common drug in all studies.
In a study performed in the United States,Citation25 transfusion support was required during four transurethral resection procedures of bladder cancer performed in patients who used antiplatelet therapy in the perioperative period and during two procedures for the control group (P=0.242). In another studyCitation22 carried out in India, none of the patients subjected to dental extraction had uncontrollable bleeding after the procedure, a result seen both in the group that used interrupted antiplatelet therapy and in the group that had the therapy 5 days before the surgical procedure. In both studies, no cardiac events or complications related to anesthesia occurred in the evaluated patients nor was there a need to rehospitalize any of them.
In the studies comparing the occurrence and/or level of bleeding after surgical procedures of patients on dual-platelet antiplatelet therapy and those on single therapy, the case of a patient who used concomitant ASA and clopidogrel daily (nonsuspended) for the surgical procedure and after tooth extraction, presented mild bleeding easily controlled by local hemostasis.Citation23 Another studyCitation24 showed that the risk of prolonged bleeding in the postoperative dental period was higher for patients who used double antiplatelet therapy; however, with hemostatic measures, bleeding was easily controlled, without the need for blood transfusion.
In the four studies selected, only one study,Citation25 which dealt with transurethral bladder cancer resection procedures, mentioned that patients who maintained antiplatelet therapy were previously evaluated by a urologist, surgeon, anesthesiologist, and cardiologist before undergoing the surgical procedure.
Regarding the limitations of the studies, they were not reported in two of them,Citation22,Citation25 however, the study carried out in SerbiaCitation23 pointed out as limitations, the fact that the sample is small, and the surgical procedures performed are low risk of bleeding (single and multiple dental extractions). On the other hand, the study carried out in India by Girotra et alCitation24 determined as a limitation the fact that the platelet aggregation test was not used because it was very expressive, as well as the nonquantification of intraoperative bleeding to estimate and compare blood loss between the study group and control group.
Risk of bias
provides a summary of the bias risk of the four studies. Only one study was adequate for random sequence generation, the other three presented a risk of uncertain bias because they did not inform the randomization process; one study had a high risk of allocation concealment (selection bias) and another three presented a risk of uncertain bias; The four studies presented a risk of uncertain bias in relation to the blindness of participants and professionals. In the case of risk of blindness in the evaluation of the results, all studies presented a risk of uncertain bias in the outcome evaluation reported by the patient, and only one study presented a low risk of blindness bias in the objective outcome evaluation, two other studies presented a risk of bias uncertain for the same assessment, and the fourth study had a high risk of bias. All the clinical trials cited here presented a low risk of incomplete outcomes and of a selective outcome. In addition, all the tests were included in the criteria adopted by these authors of quality score of at least two points and could be classified as being of good quality.
Discussion
In contemporary surgical practice, the management of platelet antiaggregation therapy is a fundamental condition.Citation26,Citation27 In our review, we selected four clinical trials from different countries dealing with the subject, two of which were from India, probably because in the past 50 years several epidemiological studies have been available that define the prevalence of CVD, in which more recent data show that this is the leading cause of death in the Indian population, followed by diseases such as asthma, diarrhea, perinatal diseases, and respiratory infections.Citation28,Citation29 In addition, studies evaluating the use of ASA and clopidogrel in this population have also been observed,Citation30 as it is currently considered that the Indian pharmaceutical field is the third largest with regard to the volume of antiplatelet agents.Citation31
One of the clinical trials analyzed in our review was conducted in the United States, probably because almost a third of the North American population uses ASA, which is a cause for concern for physicians, because parallel to this there was also the increase in the number of noncardiac surgeries undergone by these patients in this country.Citation14,Citation20,Citation26,Citation32 The other and last clinical trial was carried out in Serbia, a finding that can be understood by the results of the EPICOR study published in 2012,Citation33 which sought to identify regional differences in the use of antiplatelet agents for the treatment of acute coronary syndrome and showed that North and South Europe represent more expressive consumption of these drugs than countries of Eastern Europe and Latin America.
Regarding the type of surgical procedure, we observed a higher prevalence of dental extractive surgery in both clinical trials conducted in India and in Serbia, as well as performed in elderly patients, the predominant age group in our study. These findings can be understood by the fact that India has 76 million elderly people and, along with the rapid aging of the population, there have been a number of difficulties in terms of general and oral health.Citation34–Citation36 Accordingly, the need for dental extractions as preventive and curative measures for several diseases, among them caries, a disease that affects the majority of adults in most industrialized countries according to the World Health Organization (2000),Citation37 and oral cancer, leads India to have the highest index in the world.Citation34 Oral health care is also an important activity in Serbia, where dental health care has a long tradition.Citation38 Serbia began to develop after the Second World War intensively and extensively.Citation39 In 2010, of 5 million visits to the public dental service in Serbia, more than 700 thousand were referrals for surgeries for dental extraction.Citation40
The other type of surgical procedure described in this review was conducted in the United States and refers to urologic surgery of the transurethral resection type of bladder cancer, probably because bladder cancer accounts for about 14,000 cancer-related deaths among men in this country, with almost 60,000 new cases diagnosed each year.Citation41 In addition, the antiplatelet agents aspirin and clopidogrel, as well as the nonsteroidal anti-inflammatory drugs are the drugs most used by the North American population.Citation42
In addition to the increase in the number of noncardiac surgical procedures, the number of patients adding risk factors for CVD is increasing with the indication of using antiplatelet agents continuously. These two situations contribute to clinicians, surgeons and anesthesiologists often finding themselves in the dilemma between maintaining or suspending these drugs in the preoperative period. Decision-making in this context involves analysis of the different types of risks (thrombosis and bleeding) and, therefore, should be based on the best evidence available.Citation21
In our systematic review, the four selected clinical trials evaluated the risk of perioperative bleeding with ASA or clopidogrel alone, and one of them also evaluated the use of ticoplidina;Citation23 two of them also assessed the risk of bleeding with dual antiaggregation therapies (aspirin + clopidogrel, aspirin + ticlopidine, and aspirin + prasugrel).Citation22,Citation23 In all the trials, it was concluded that there is no need to suspend the medications prior to procedures such as dental extraction and transurethral resection of the bladder, because according to these studies there is no need to expose the patient to the risk of thromboembolism, cerebrovascular accidents or AMI interrupting the platelet antiaggregation therapy prior to small surgical procedures.Citation22–Citation25
In agreement with the findings of this review, the American College of Physicians of the Thorax and the Brazilian Society of Cardiology argue that patients who use ASA for secondary prevention and who will undergo noncardiac surgical procedures must continue it in use.Citation43–Citation45 This was confirmed in other studies, which revealed that there was no significant difference in the occurrence of bleeding events,Citation46,Citation47 even among those using dual antiplatelet therapy,Citation48 when the platelet antiaggregant(s) is/are maintained in the perioperative period.
However, the Guidelines of the European Society of Cardiology, published in 2014, argue that the maintenance of aspirin in the perioperative period increases the risk of hemorrhagic complications by 50% and may need to be discontinued for more than 7 days before certain ophthalmologic, neurological, or spinal surgeries. However, in individuals at risk for CVD, nonadherence or withdrawal of ASA tripled the risk of a major adverse cardiovascular event. Thus, these guidelines conclude that the use of low-dose ASA before noncardiac surgeries should be individualized, balancing perioperative bleeding and thrombotic risk against cardiovascular benefit.Citation13
Also, the American Society’s recommendations are that it is not beneficial to initiate or continue the use of ASA prior to noncardiac surgeries in patients with no history of coronary stenting unless the risk of ischemic events outweighs the risk of surgical bleeding.Citation19,Citation49 In a randomized multicenter international study conducted between 2010 and 2013, involving 135 hospitals from 23 different countries, totaling more than 10,000 patients, it was concluded that the use of ASA in the preoperative period of noncardiac surgeries and immediately in the postoperative period does not have a significant effect on the prevention of cardiac complications and even nonfatal AMI, but it considerably increases the risk of bleeding in this period.Citation26
In many of these studies, including the guidelines themselves from different countries, medical procedures are not specified by type of noncardiac surgical procedure to which the patient will be subjected. Thus, the information is more generalized, with the exception of neurological surgeries and transurethral prostatectomies, since the literature is unanimous in stating that even if the patient is using aspirin and/or clopidogrel for secondary prevention, they must be suspended for 7 days before the procedure, since the occurrence of bleeding in these types of procedures can be fatal.Citation44
Based on the results of that review, compared with the findings of other studies, it is understood that the maintenance of antiplatelet therapy in perioperative of noncardiac surgery should be based on the type of medicine, the surgical risk, and the thrombotic risk of each patient. The guidelines of the Brazilian Society of Cardiology for a patient who makes continuous use of clopidogrel for secondary prevention is that the risk of bleeding from the type of surgery should be considered. Thus, when the risk of bleeding is moderate or high, clopidogrel should be discontinued before the procedure, and when the risk is low the antiaggregant should be maintained in the perioperative period.Citation44,Citation50 With a more robust analysis, as advocated by the authors of this review, the Consensus Guide “Perioperative management of the patient receiving antiplatelet” of Anesthesiology Portuguese Society takes into account both the antiplatelet that the patient is in use as well as the hemorrhagic risk of surgery, and also the thrombotic risk of each patient.Citation50
In this sense, considering that tooth extraction surgeries present in this review are considered to be of low hemorrhagic risk, as stated in the SPA Consensus Guide (2014),52 antiplatelets alone or in double therapies should not be suspended – a result proven in clinical trials.Citation22–Citation24 However, despite the fact that urological surgeries are of high hemorrhagic risk, which was the subject of a study by Picozzi et al,Citation25 it was confirmed in this trial that transfusion support was required during four procedures performed on patients taking platelet antiaggregation therapy and during two procedures in the control group (P=0.242); also, no cardiac events nor complications related to anesthesia occurred. Three patients in the treatment group and two patients in the control group required reintervention to ensure hemostasis during the postoperative period. However, none of the patients in any group were rehospitalized for hematuria after leaving the hospital, and it was concluded that continued use of antiplatelet monotherapy does not increase the risk of general bleeding or reintervention for patients undergoing transurethral resection neoplasms of the bladder and that suspending aspirin prior to such procedure is therefore unnecessary.
Finally, we believe that this systematic review constitutes a valuable addition to the research and practice in health interventions regarding the prescription of antiplatelet drugs in surgeries, since our findings provide a basis for the surgeon, the dental surgeon, the anesthesiologist, and the cardiologist to make decisions on the prescription of antiplatelet agents in the perioperative period of small noncardiac surgeries, and thus ensure patient safety regarding the prevention of thrombotic and hemorrhagic events. However, although the trials included in this review were considered to be of good quality and thus corroborated for the construction of other studies, all trials presented a risk of uncertain bias in some of the criteria analyzed, and two of the trials had high risk of bias,Citation22,Citation23 which serves as an alert for other studies that are developed in this line to have these criteria very well defined in its description.
Conclusion
It is unnecessary to compromise the patient’s life by subjecting him/her to the risk of thromboembolism, stroke, or AMI due to the suspension of antiplatelet therapy before surgical procedures such as dental extraction and transurethral resection of bladder cancer. These were the main findings of our review, which involved four clinical trials, classified as good quality, and corroborated with the results of other types of studies available in the literature. However, we note that further studies involving other types of surgeries are necessary, and that determinations regarding the prescribing of antiplatelet in the perioperative period of noncardiac surgeries should be based on the type of antiplatelet agent, the thrombotic risk of the patient, and the hemorrhagic risk of the surgical procedure.
Disclosure
The authors report no conflicts of interest in this work.
References
- MansurAPFavaratoDMortality due to cardiovascular diseases in Brazil and in the metropolitan region of São Paulo: a 2011 updateArq Bras Cardiol2012992755761 Article in English, Portuguese22735870
- MathersCDLoncarDProjections of global mortality and burden of disease from 2002 to 2030PLoS Med2006311e44217132052
- MansurAPFavaratoDSouzaMFTrends in death from circulatory diseases in Brazil between 1979 and 1996Arq Bras Cardiol2001766504510 Article in English, Portuguese
- MurrayCJLopezADGlobal mortality, disability, and the contribution of risk factors: Global Burden of Disease StudyLancet19973499063143614429164317
- Writing Committee for the VISION Study InvestigatorsDevereauxPJBiccardBMAssociation of Postoperative High-Sensitivity Troponin Levels With Myocardial Injury and 30-Day Mortality Among Patients Undergoing Noncardiac SurgeryJAMA2017317161642165128444280
- EkeloefSAlamiliMDevereauxPJGögenurITroponin elevations after non-cardiac, non-vascular surgery are predictive of major adverse cardiac events and mortality: a systematic review and meta-analysisBr J Anaesth2016117555956827799170
- van WaesJANathoeHMde GraaffJCMyocardial injury after noncardiac surgery and its association with short-term mortalityCirculation2013127232264227123667270
- Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study InvestigatorsDevereauxPJChanMTAlonso-CoelloPAssociation between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgeryJAMA2012307212295230422706835
- DevereauxPJXavierDPogueJCharacteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort studyAnn Intern Med2011154852352821502650
- BottoFAlonso-CoelloPChanMTMyocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomesAnesthesiology2014120356457824534856
- PearseRMMorenoRPBauerPMortality after surgery in Europe: a 7 day cohort studyLancet201238098471059106522998715
- WeiserTGRegenbogenSEThompsonKDAn estimation of the global volume of surgery: a modelling strategy based on available dataLancet2008372963313914418582931
- KristensenSDKnuutiJSarasteA2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA)Eur Heart J201435352383243125086026
- WiviottSDBraunwaldEMccabeCHPrasugrel versus clopidogrel in patients with acute coronary syndromesN Engl J Med2007357202001201517982182
- EikelboomJWHirshJSpencerFABaglinTPWeitzJIAntiplatelet drugs: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest20121412 Supple89Se119S22315278
- ArtangRDieterRSAnalysis of 36 reported cases of late thrombosis in drug-eluting stents placed in coronary arteriesAm J Cardiol20079981039104317437724
- Antithrombotic Trialists’ (ATT) CollaborationBaigentCBlackwellLCollinsRAspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trialsLancet200937396781849186019482214
- GersteinNSSchulmanPMGersteinWHPetersenTRTawilIShould more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndromeAnn Surg2012255581181922470078
- BurgerWChemnitiusJMKneisslGDRückerGLow-dose aspirin for secondary cardiovascular prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation – review and meta-analysisJ Intern Med2005257539941415836656
- ColumboJALambourAJSundlingRAA Meta-analysis of the Impact of Aspirin, Clopidogrel, and Dual Antiplatelet Therapy on Bleeding Complications in Noncardiac SurgeryAnn Surg2018267111028463896
- MagarãoRVQMarquesACFeitosa-FilhoGSAspirina no perioperatório de cirurgias não cardíacas: o dilema entre manter ou suspender* [Aspirin in the perioperative period of non-cardiac surgeries: the dilemma between maintaining or suspending]Rev Bras Clin Med. São Paulo201193218224 Portuguese
- VargheseKGManoharanSSadhanandanMEvaluation of bleeding following dental extraction in patients on long-term antiplatelet therapy: A clinical trialIndian J Dent Res201526325225526275190
- BajkinBVUrosevicIMStankovKMPetrovicBBBajkinIADental extractions and risk of bleeding in patients taking single and dual antiplatelet treatmentBr J Oral Maxillofac Surg2015531394325311541
- GirotraCPadhyeMMandlikGAssessment of the risk of haemorrhage and its control following minor oral surgical procedures in patients on anti-platelet therapy: a prospective studyInt J Oral Maxillofac Surg20144319910624074486
- PicozziSMarenghiCRicciCRisks and complications of transurethral resection of bladder tumor among patients taking anti-platelet agents for cardiovascular diseaseSurg Endosc201428111612124002913
- DevereauxPJMrkobradaMSesslerDIAspirin in patients undergoing noncardiac surgeryN Engl J Med2014370161494150324679062
- StoneDHGoodneyPPSchanzerAClopidogrel is not associated with major bleeding complications during peripheral arterial surgeryJ Vasc Surg201154377978421571492
- GuptaRGupthaSSharmaKKGuptaADeedwaniaPRegional variations in cardiovascular risk factors in India: India heart watchWorld J Cardiol20124411212022558490
- GuptaRJoshiPMohanVReddyKSYusufSEpidemiology and causation of coronary heart disease and stroke in IndiaHeart2008941162618083949
- GuhaSSardarPGuhaPDual antiplatelet drug resistance in patients with acute coronary syndromeIndian Heart J2009611687319729693
- RashmiANerlekarSRajeevKStudy of variation in prices of oral anti-platelet drugs available in Indian marketInt J Basic Clin Pharmacol201653810813
- CannonCPHarringtonRAJamesSComparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomised double-blind studyLancet2010375971128329320079528
- BuenoHStoreyRFDanchinNCurrent regional differences in the use of antiplatelet drugs for the treatment of acute coronary syndromes. Results from the EPICOR studyPresented at: European Society of Cardiology (ESC) Congress 2012August 25–29, 2012Munich, Germany
- PanchbhaiASOral health care needs in the dependant elderly in IndiaIndian J Palliat Care2012181192622837606
- ChandraSChandraSText Book of Community Dentistry1st edNew DelhiJaypee Brothers Medical Publishers (P) Ltd India. Geriatric Dental Health Care2004239251
- HenryRGCeridanBDelivering dental care to nursing home and homebound patientsDent Clin North Am19943835375517926202
- World Health OrganizationWHO Global Oral Health Data Bank and WHO Oral Health Country/Area Profile ProgramGenevaWorld Health Organization2000
- AndelskiHObradovicMGolijaninMHistory of DentistryPancevo, SerbiaSchool of Dental Medicine2011
- AndelskiHTimoticBSystems for the provision of oral health care in the Black Sea countries. Part 11: SerbiaOral Health Dent Manag2012112515622692270
- Institute of Public Health of Serbia (IPHS)Statistical Yearbook of Health in the Republic of SerbiaBelgrade, SerbiaIPHS2010 Available from: http://www.batut.org.rs/index.php?content=77Accessed March 1, 2018
- SiegelRLMillerKDJemalACancer statistics, 2015CA Cancer J Clin201565152925559415
- KanakadandiVParasaSSihnPPatterns of antiplatelet agent use in the USEndosc Int Open2015303E173E17826171425
- Lorga FilhoAMBrazilian guidelines on platelet antiaggregants and anticoagulants in cardiologyArq Bras Cardiol20131013 Suppl195
- DouketisJDSpyropoulosACSpencerFAPerioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest20121412 Supple326Se350S22315266
- OscarssonAGuptaAFredriksonMTo continue or discontinue aspirin in the perioperative period: a randomized, controlled clinical trialBr J Anaesth2010104330531220150346
- JosephBRawashdehBAzizHAn acute care surgery dilemma: emergent laparoscopic cholecystectomy in patients on aspirin therapyAm J Surg2015209468969425064416
- WolfAMPucciMJGabaleSDSafety of perioperative aspirin therapy in pancreatic operationsSurgery20141551394623890963
- GuQDillonCFEberhardtMSWrightJDBurtVLPreventive Aspirin and Other Antiplatelet Medication Use Among U.S. Adults Aged ≥ 40 Years: Data from the National Health and Nutrition Examination Survey, 2011–2012Public Health Rep2015130664365426556936
- FleisherLAFleischmannKEAuerbachAD2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelinesJ Am Coll Cardiol20146422e77e13725091544
- Portuguese Anesthesiology SocietyManuseio peri-operatorio does doentes medicados com anticoagulantes e antiagegantes plaquetarios: resultado da 3ª reuniao de consenso da Sociedade Portuguesa de Anestesiologia [Peri-operative management of the patient medicated with antiplatelet agents: results of the 3rd consensus meeting of the Portuguese Society of Anesthesiology]Rev Soc Port Anestesiol20142337693 Portuguese