Abstract
Objective
The objective of the study was to evaluate the dose-related influence of metoprolol on cardiac performance, motor function, quality of life (QoL), and mental status in Chinese patients with chronic heart failure (CHF).
Patients and methods
This was a prospectively designed single-center study which enrolled CHF patients with resting heart rate (HR) >80 bpm belonging to the New York Heart Association (NYHA) III/IV functional classification. Patients were initiated with 12.5 mg of metoprolol, and every second week, the dose was escalated until the target HR level (60–70 bpm) was achieved during the follow-up at 1st, 3rd, 6th, and 12th months. Patients were divided into two groups depending on the doses administered: 47.5 mg (n=37) and 118.75 mg (n=74), respectively, for comparison in terms of change in cardiac function, motor function, QoL, and mental status.
Results
Among the 111 patients with CHF, no significant difference was shown between the two doses administered. Irrespective of the dose, the cardiac performance, motor function, QoL, and anxiety improved and there was an increase in depression, whereas the effect on burnout, calculated as Copenhagen Burnout Inventory (CBI), equally was insignificant throughout the 1-year follow-up period in both the CHF patient groups.
Conclusion
Lower dose of metoprolol (47.5 mg) is as effective as higher dose (118.75 mg) in Chinese population with CHF to improve the cardiac function, motor function, QoL, and mental status.
Introduction
Chronic heart failure (CHF) has been emerging as a major public health issue with a wide prevalence of about 5.8 million in the United StatesCitation1 and over 4.2 million in China.Citation2,Citation3 The incidence of heart failure (HF) increases the risk of morbidity and mortality substantially, despite the advances in management. Clinical epidemiology data show that over 2.4 million patients who are hospitalized have HF as a primary or secondary diagnosis, and nearly 300,000 deaths annually are directly attributable to HF.Citation1 Furthermore, awareness of HF and preserved left ventricular ejection fraction (LVEF) is increasing. HF and preserved LVEF now represent >50% of HF cases, leading to poor outcomes similar to those associated with HF and reduced LVEF; however, it does not have a proven effective management strategy yet.Citation4–Citation6
Beta-blockers have been shown to reduce mortality in older patients with complex ventricular arrhythmias associated with prior myocardial infarction and reduced LVEF.Citation7,Citation8 These beneficial effects of beta-blockers for left ventricular function in HF are experimentally shown to be only due to reduction in heart rate (HR).Citation9 Bristow et al demonstrated dose-related improvements of left ventricular HF and survival with carvedilol in patients with systolic HF.Citation10 Bradycardia occurs due to blockade of both β1- and β2-adrenergic receptors and reduction of cardiac and/or systemic adrenergic drive.Citation11 In a dose-relationship study with beta-blocker, a higher dose was associated with a significant reduction in all-cause hospitalization and all-cause death, even after adjusting for important prognostic covariates.Citation12 Bisoprolol has also shown dose-related improvement in left ventricular function, reduction in mortality, and hospitalization rate in patients with HF.Citation13 In general, beta-blockers (nonselective, cardio-selective, and nonselective with ancillary properties) are known to counteract the effects of prolonged sympathetic stimulation in patients with failing HF. Therefore, it leads to improvement in the left ventricular systolic and diastolic functions, reversal remodeling, HR control, effective prevention of the malignant arrhythmias, and lowering of both cardiac afterload and preload.Citation14 Although beta-blockers are known to improve the HR,Citation15 systolic blood pressure (SBP),Citation16 ejection fraction (EF),Citation17,Citation18 quality of life (QoL),Citation19,Citation20 and NYHA class,Citation21 these could be affected by the presence of depression.Citation22,Citation23 Very little literature is available on the effect of beta-blockers correlating the heart and motor functions, QoL, and mental status of patients with CHF in Chinese population. Therefore, this study evaluated the dose-related impact of metoprolol on HR, cardiac performance, motor function, and effect on different mental status in Chinese patients with CHF belonging to NYHA III/IV functional classification.
Patients and methods
Study design, selection of patients, and grouping
This prospectively designed single-center study was conducted from February 2013 to April 2016 and enrolled patients as their own controls. The study protocol was approved by the Institutional Review Board of the Second Affiliated Hospital of Kunming Medical University, China and conformed to the declaration of Helsinki and its subsequent revisions.
Inclusion criteria for the study were as follows: 1) patients with CHF with resting HR >80 bpm; 2) patients newly diagnosed with neuropsychiatric disorders such as depression and anxiety, which were measured using the hospital anxiety and depression scale (HADS) questionnaire; and 3) high burnout status, measured using CBI scores, with the patients belonging to NYHA III/IV functional classification. Patients were briefed about the benefits and possible limitations of the study in writing and orally in their language, and signed informed consent was obtained before the start of the study.
Patients who were excluded from the study were those with bradycardia (resting HR <60 bpm), SBP <90 mm Hg, those who have used metoprolol in the previous 3 months, those with <6 months of expected survival time, pacemaker-dependent patients, those with contraindications to beta-blocker, those who are currently using class I or class III anti-arrhythmic agents, tricyclic antidepressants, anxiolytics, or any other central nervous system medications, and those who have undergone coronary bypass surgery or experienced a recent heart attack.
Patients were divided into two groups: “A” and “B,” depending on the doses administered; 47.5 mg (n=37) and 118.75 mg (n=74) for comparison, respectively.
Treatment intervention and follow-up
Baseline data were collected from patients before treatment with initial once daily, oral 12.5 mg dose of metoprolol continuous release tablets (Betaloc® ZOK (Metoprolol); Astra-Zeneca, Södertälje, Sweden). The dose was escalated every second week, and for long-term treatment, the dose was fixed at 190 mg or maximum tolerated dose until the target HR level (60–70 bpm) was achieved during the follow-up. Final outcome measurements from interventions were obtained by following up at 1, 3, 6, and 12 months for all patients.
Study outcomes
The outcomes were as follows: change in cardiac function as measured in terms of HR (bpm), SBP (mm Hg), EF (%), and cardiac index (CI, [L/min⋅m2]). Change in motor functions or exercise tolerance was measured by a standard 6-minute walk test (6MWT) and Veterans Specific Activity Questionnaire (VSAQ). QoL was measured by an 8-item short-form questionnaire (SF-8) and the Minnesota Living with Heart Failure Questionnaire (MLHFQ). Mental status was measured by the HADS depression/anxiety scores, and high burnout status was measured using the CBI average scores in CHF patients with clinical psychiatric disorders. At enrollment, all patients were asked to take the VSAQ questionnaire for baseline values.
Cardiac performance measured in terms of HR, SBP, CI, and EFCitation24 and responses of the questionnaires for VSAQ, SF-8, and MLHFQ scores,Citation24 and HADS depression/anxiety and CBI scoresCitation25,Citation26 are as per the previous studies reported by Meng et al,Citation24 Liu et al,Citation25 and Huang et al.Citation26
6MWT
Values of 6MWT at baseline and after the use of metoprolol were recorded. It is a standardized test of functional exercise capacity used to assess mobility in aged people with cardiopulmonary diseases. It provides a global assessment of exercise capacity and reflects better daily activity compared with laboratory tests. The average 6-minute walk distance in patients with HF ranges from 310 to 427 m. Statistical analyses were performed as per the previously described methods by Meng et al,Citation24 Liu et al,Citation25 and Huang et al.Citation26
Ethical statement
This study was approved by the Institutional Review Board of the Second Affiliated Hospital of Kunming Medical University, China.
Results
Baseline characteristics
Baseline characteristics are presented in . Totally, 169 patients were enrolled, of which 11 were excluded as they were intolerant to metoprolol dose increments and four were lost to follow-up. Finally, data for 154 patients were obtained. Study flow of the patients is presented in . Most of the patients were classified as NYHA class III/IV (n=145). Among these patients, 111 of them were divided into two groups depending on the doses administered: 47.5 mg (n=37) and 118.75 mg (n=74) to assess the impact of two different doses of metoprolol on CHF patients.
Figure 1 Study flowchart.
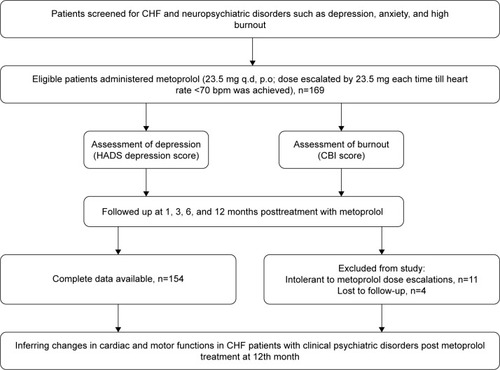
Table 1 Baseline characteristics
Change in HR and SBP
The average metoprolol dose to reach the target HR goal was 99.75 mg. Baseline values of average resting HR, as measured by resting electrocardiogram, decreased significantly from 84.59±7.12 to 65.03±3.47 bpm (P<0.0001) at the 12th month post-metoprolol treatment in patients of group A receiving 47.5 mg and decreased from 81.12±6.06 to 64.59±2.99 bpm (P<0.0001) in patients of group B (). Similarly, there was a significant drop in SBP from the baseline value of 127.01±13.18 to 122.70±6.53 mm Hg (P=0.01) at the 12th-month follow-up for the patients in group B (). However, no significant change occurred in SBP in the 12th month in the patients treated with 47.5 mg of metoprolol in group A. Also, there were no significant changes in the HR and SBP when the two doses were compared at baseline and followed up at 12th month.
Table 2 Impact of dose on HR, SBP, EF, and CI
Cardiac performance
After treatment with 47.5 mg of metoprolol in group A, the EF significantly decreased from a baseline value of 39.35±5.93 to 35.73±7.19 (P=0.02) at 1st-month follow-up and to 35.00±4.55 (P=0.0007) at 3rd-month follow-up. However, it significantly increased to 48.08±3.9 (P<0.0001) and 51.41±3.75 (P<0.0001) in the 6th- and 12th-month follow-ups, respectively. Similarly, after an initial decrease from the baseline value of 37.13%±5.79% to 34.56%±5.51% (P=0.006) in the 1st-month follow-up, EF continued to significantly increase to 47.35%±4.67% (P<0.0001) and 50.08%±4.36% (P<0.0001) at 6th- and 12th-month followups, respectively, in patients of group B ().
In terms of CI, a significant decrease from the baseline (1.82±0.22) to 1st-month follow-up (1.69±0.27 [P=0.02]) was observed in group A, with a constant increase to 2.29±0.21 (P<0.0001), 2.62±0.18 (P<0.0001), and 2.76±0.23 (P<0.0001) at the 3rd-, 6th-, and 12th-month, respectively. However, post-metoprolol treatment in group B, CI constantly increased only from the 3rd-month onwards, from the baseline value of 1.78±0.20 to 2.24±0.20 L/min/m2 (P<0.0001) and to 2.61±0.19 (P<0.0001) and 2.68±0.27 L/min/m2 (P<0.0001) in 6th- and 12th-month, respectively, (). However, there was no significant change in cardiac functions measured as EF and CI throughout the 12th-month period between both the doses.
Motor function
When tested for changes in motor function, the distance covered during the 6MWT significantly increased at 6th- and 12th-month follow-ups from a baseline value of 362.16±36.51 to 402.76±20.72 (P<0.0001) and 420.65±19.97 m (P<0.0001), respectively, in group A. In group B, a significant decrease in 6MWT was observed from the baseline value of 368.96±33.74 to 334.18±31.07 m (P<0.0001) at the 1st-month follow-up, followed by an increase to 354.77±32.38 m (P<0.01 vs 1st-month follow-up) at the 3rd-month follow-up and further showed a significant steady rise to 398.84±21.56 (P<0.0001) and 417.74±20.69 m (P<0.0001) at the 6th- and 12th-month follow-ups, respectively, ().
Table 3 Impact of dose on motor function and QoL
Furthermore, the exercise tolerance recorded that VSAQ score decreased from a baseline value of 6.43±1.02 to 5.03±1.03 (P<0.0001) at the 1st-month follow-up and increased to 5.69±1.14 (P=0.004 vs 1st-month) at 3rd-month follow-up, and then showed steady increment to 7.97±1.08 (P<0.0001) and 8.49±0.96 (P<0.0001) at the 6th- and 12th-month follow-ups, respectively, in patients treated with 47.5 mg of metoprolol group A. Similar trend in the scores of VSAQ was observed for the patients treated with 118.75 mg of metoprolol with a decrease from a baseline value of 6.56±1.09 to 4.90±0.82 (P<0.0001) at the 1st-month follow-up and an increase to 5.40±0.92 (P<0.0001 vs 1st-month follow-up) at the 3rd-month follow-up, and then a steady significant increase to 7.71±1.09 (P<0.0001) and 8.19±0.95 (P<0.0001) at the 6th- and 12th-month followups, respectively, (). There was no significant change in the motor functions measured as 6MWT and VSAQ between the groups posttreatment with metoprolol.
QoL outcomes posttreatment
The QoL, as measured by the SF-8 scores, significantly decreased from a baseline value of 43.97±2.27 to 40.00±1.47 (P<0.0001) and 41.59±2.03 (P<0.0001) at the 1st- and 3rd-month follow-ups, respectively, and displayed a significant increase to 48.95±1.25 (P<0.0001) and 51.97±1.88 (P<0.0001) at the 6th- and 12th-month follow-ups, respectively, in group A. Similarly, in group B, the scores significantly decreased from the baseline in 1st-month follow-up (43.99±2.91-39.08±1.90; P<0.0001) and significantly increased at 6th-(48.85±1.20; P<0.0001) and 12th-month follow-ups (52.34±2.06; P<0.0001).
The MLHFQ scores significantly increased from a baseline value of 74.08±3.85 to 88.24±3.37 (P<0.0001) and 86.35±5.14 (P<0.0001) at the 1st- and 3rd-month follow-ups, respectively, and further decreased below the baseline value to 63.95±4.18 (P<0.0001) and 53.51±10.67 (P<0.0001) at the 6th- and 12th-month follow-ups, respectively, in patients of group A who were administered 47.5 mg of metoprolol (). Similarly, the MLHFQ scores significantly increased from a baseline value of 74.04±3.86 to 89.18±4.38 (P<0.0001) and 86.93±4.88 (P<0.0001) at the 1st- and 3rd-month follow-ups, respectively, in patients of group B who were administered 118.5 mg of metoprolol, and it decreased below the baseline value to 64.32±3.32 (P<0.0001) and 53.41±7.35 (P<0.0001) at the 6th- and 12th-month follow-ups, respectively (). However, posttreatment, the SF-8 and MLHFQ scores did not vary significantly with the change in dose from 47.5 mg in group A to 118.5 mg in group B.
Change in mental status
Metoprolol treatment resulted in a significant increase in the HADS depression score only in the patients of group B who were administered 118.5 mg of metoprolol. There was an increase from baseline value of 8.92±2.82 to 10.04±3.02 (P=0.02) at 1st-month follow-up and an increase to 10.15±3.01 (P=0.01) and 10.18±2.93 (P=0.008) at 3rd- and 6th-month follow-ups, respectively; however, there was a decrease to 9.92±2.49 (P=0.02 vs 6th-month follow-up) at the 12th-month ().
Table 4 Impact of dose on mental status
In contrast to the depressive effects, HADS anxiety score significantly decreased from a baseline of 8.19±2.09 to 7.11±1.20 (P<0.0001) at 3rd-month, which further decreased to 7.05±1.05 (P<0.0001) and 6.97±1.01 (P<0.0001) through 6th- and 12th-month follow-ups (P<0.0001), respectively, for the patients of group A treated with 47.5 mg of metoprolol. Similarly, the trend of HADS anxiety score continued post-metoprolol treatment with the patients of group B, who were administered 118.75 mg of metoprolol, with a significant decrease in the baseline value from 8.23±2.05 to 7.09±1.09 (P<0.0001) in the 3rd-month follow-up to 7.07±1.02 (P<0.0001) and 7.15±0.95 (P<0.0001) in 6th-and 12th-month follow-ups, respectively, ().
Post-metoprolol treatment, the change in burnout status as measured by CBI average scores was insignificant in both groups A and B treated with 47.5 and 118.75 mg in patients with CHF, respectively (). In contrast, there was no significant change in mental status as measured by HADS depression/anxiety and CBI scores between the two doses of metoprolol studied in patients with CHF.
Discussion
We have initially reported the effect of metoprolol on the cardiac and motor functions, QoL, and the mental status of patients with CHF, and CHF patients with clinically diagnosed depression or anxiety disorder.Citation24–Citation26 Currently, there is no comprehensive evidence on dose comparison of metoprolol succinate in correlation with all the aforementioned parameters. Thus, this study examined the impact of two different doses of metoprolol on Chinese patients with CHF. Owing to the mechanism of metoprolol’s competitive antagonistic action on beta-adrenergic receptors (β1-blocking), a reduction in HR was observedCitation27 in both groups A and B treated with 47.5 and 118.75 mg of metoprolol, respectively, from 1st-month through 12th-month follow-ups.
At the same time, there was a reduction in SBP from the baseline to 12th-month follow-ups as seen in other studies.Citation28,Citation29 This effect could be due to the selective action of metoprolol on beta-1 blocking, where cardiac norepinephrine stimulates sympathetic activity facilitated by beta-2 receptors and unopposed alpha-mediated vasoconstriction.Citation30,Citation31
There was a biphasic response in EF change with both the doses of metoprolol. After a decrease from baseline in the 1st- and 3rd-month follow-ups, the EF increased above the baseline in the 6th- and 12th-month follow-ups. The HR decreased by 16–20 bpm at the 12th-month follow-up in this study with both doses of metoprolol, and as a compensatory mechanism, the LVEF was amplified from 6th-month follow-up onwards through 12th-month in both the dose groups with an average increase of 12% and this is consistent with the previously published reports.Citation30,Citation32,Citation33 The initial delay in the augmentation of EF could be explained by the fact that hemodynamic responses to beta-adrenergic blockade often require more than 2 months to develop as per reports of Williams et al and Floras et al.Citation34,Citation35 Similar outcomes have been shown in patients with NYHA II–IV grade CHF with improved EF, lowered LVEF, and cardiac frequency.Citation36
In this study, CHF patients with NYHA III/IV criteria, who had a decompensated LVEF with the inability of the heart to pump sufficient oxygenated blood, in which consequences such as decreased CI often existed, were admitted.Citation37 The biphasic response persisted in the cardiac response as measured by CI. After an initial decline in CI in the 1st-month follow-up, there was a steady rise in 3rd-, 6th-, and 12th-month followups with an overall increased magnitude of 0.9 L/min⋅m2 for both patient groups A and B, who were administered 47.5 and 118.75 mg of metoprolol, respectively. These outcomes are supported by the benefits of beta-blocker use in CHF patients with reduced LVEF and preserved LVEF,Citation38,Citation39 which employ multiple mechanisms.Citation40 There are not many significant changes in heart functions measured as HR, SBP, EF, and CI with the administration of the two doses: 47.5 and 118.75 mg post-metoprolol intervention in patients with CHF.
Motor function, as calculated in terms of 6MWT and VSAQ, showed an initial reduction in 1st- and 3rd-month follow-ups tailed by growth at 6th- and 12th-month follow-ups post-metoprolol treatment. This improvement at 12th month with 58 and 48 m in 6MWTCitation41 and 2.1 and 1.6 in VSAQ scoreCitation42 in patients treated with 47.5 and 118.5 mg of metoprolol, respectively, are in-line with the previous studies reported. Also, there was a proportionate increase of 6MWT and VSAQ scores with an increase in EF and CI at the 6th- and 12th-month follow-ups. This improvement in motor functions is in direct correlation with the improvement of heart function due to innate mechanism of beta-blockers.Citation37–Citation40 QoL as assessed with SF-8 scores diminished at 1st-month follow-up and gradually amplified at 3rd-, 6th-, and 12th-month follow-ups. In contrast, the MLHFQ scores increased at 1st-month follow-up and progressively reduced at 3rd-, 6th-, and 12th-month follow-ups. These trends do not significantly correlate with the improvements in cardiac and motor functions as shown by metoprolol in this study. However, other studies with metoprolol have reported good correlation of QoL with clinical outcomes.Citation43–Citation45 One of the studies by Waagstein et al has shown a significant improvement in QoL in correlation with heart and motor functions in patients with CHF, with metoprolol intervention.Citation46 Nevertheless, no significant metoprolol dose-related changes were observed in motor functions studied as 6MWT, VSAQ, QoL deliberated as SF-8, and MLHFQ in patients with CHF.
In this study, mental status of patients was measured with the scale of HADS depression/anxiety and CBI. These scales rate both the dose groups A and B of patients with CHF, treated with 47.5 and 118.75 mg, respectively, equally. There was an increment in HADS depression score while HADS anxiety score diminished through the 12th-month follow-up, which shows that metoprolol can lead to depression or also amplify the preexisting depression in patients with CHF. However, at the same time, it improved the anxiety symptoms in these patients, which are in accordance with earlier findings.Citation47,Citation48 Burnout measured as change in CBI equally in both the groups A and B was insignificant in the 1-year period. However, in our previous study, we have reported for the first time that metoprolol treatment worsens the already existing high burnout.Citation25 The challenge here lies in identifying the preexisting mental status and cautious administration of metoprolol although the exact mechanism of such changes in depression/anxiety is not clear.Citation49,Citation50 No correlation of these scores could be identified with the heart and motor functions in this study. At the same time, there was no significant dose-related changes in mental status seen with 47.5 and 118.75 mg of metoprolol in patients with CHF. However, in previous published literature, the metoprolol continuous release tablets are found to improve the well-being of patients with survival outcomes and reduced hospitalizations due to CHF.Citation21,Citation51
The strength of this study was that we could compare effects of the two doses, 47.5 and 118.75 mg, of metoprolol on various parameters: HR, SBP, EF, and CI for heart function; 6MWT and VSAQ for motor function; SF-8 and MLHFQ for QoL; and HADS depression/anxiety and CBI equally for mental status in patients with CHF for the 1st-, 3rd-, 6th-, and 12th-month. However, there are certain limitations in this study: 1) placebo or an active control (other beta-blockers effective in CHF) was not used and patients were their own controls, and thus few findings might have been overlooked; 2) results would have varied if the questionnaire approach was an interview-based method instead of being self-administered; 3) the mortality and long-term influence of metoprolol on these parameters could not be captured due to a limited follow-up period of 12 months; 4) age of the patients could have played as a confounding factor on the study outcomes; 5) the sample size may not be adequate to conclude these findings; 6) patients with CHF, who are likely to be on other medications such as antihypertensives, anti-arrhythmic agents, or antidepressants can show potentially varied findings as these drugs may pose contraindications; and 7) these controlled-release formulations of metoprolol could also be compared with immediate-release formulations to draw further conclusions.
Conclusion
Although current guidelines recommend up-titration of beta-blockers to the target dose, a lower dose of 47.5 mg was seen to be as effective as the higher dose of 118.75 mg in the current study as there was no significant difference between the two doses studied. Within the limitations of this study cited earlier, there is a lot of scope for further studies in Chinese population to evaluate the effect of metoprolol.
Author contributions
QZ and YM conceived the study and wrote the basic protocol. QS, LW, and RZ contributed to the design, development of the study protocol, and data acquisition. QZ drafted the first manuscript with contributions from YM and QS. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Abbreviations
| CBI | = | Copenhagen Burnout Inventory |
| CHF | = | chronic heart failure |
| CI | = | cardiac index |
| EF | = | ejection fraction |
| HADS | = | Hospital Anxiety and Depression Scale |
| HR | = | heart rate |
| LVEF | = | left ventricular ejection fraction |
| MLHFQ | = | Minnesota Living With Heart Failure Questionnaire |
| NYHA | = | New York Heart Association |
| QoL | = | quality of life |
| SBP | = | systolic blood pressure |
| VSAQ | = | Veterans Specific Activity Questionnaire |
Disclosure
The authors report no conflicts of interest in this work.
References
- WRITING GROUP MEMBERSLloyd-JonesDAdamsRJAmerican Heart Association Statistics Committee and Stroke Statistics SubcommitteeHeart disease and stroke statistics – 2010 update: a report from the American Heart AssociationCirculation20101217e46e21520019324
- YangYNMaYTLiuFIncidence and distributing feature of chronic heart failure in adult population of XinjiangZhonghua Xin Xue Guan Bing Za Zhi2010385460464 Chinese20654109
- HuSSKongLZGaoRLEditorial BoardOutline of the report on cardiovascular disease in China, 2010Biomed Environ Sci201225325125622840574
- BhatiaRSTuJVLeeDSOutcome of heart failure with preserved ejection fraction in a population-based studyN Engl J Med2006355326026916855266
- MassieBMCarsonPEMcMurrayJJI-PRESERVE InvestigatorsIrbesartan in patients with heart failure and preserved ejection fractionN Engl J Med2008359232456246719001508
- OwanTEHodgeDOHergesRMJacobsenSJRogerVLRedfieldMMTrends in prevalence and outcome of heart failure with preserved ejection fractionN Engl J Med2006355325125916855265
- Al-GobariMEl KhatibCPillonFGueyffierFβ-Blockers for the prevention of sudden cardiac death in heart failure patients: a meta-analysis of randomized controlled trialsBMC Cardiovasc Disord2013135223848972
- BristowMRTreatment of chronic heart failure with β-adrenergic receptor antagonists: a convergence of receptor pharmacology and clinical cardiologyCirc Res2011109101176119422034480
- NagatsuMSpinaleFGKoideMBradycardia and the role of beta-blockade in the amelioration of left ventricular dysfunctionCirculation2000101665365910673258
- BristowMRGilbertEMAbrahamWTCarvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. MOCHA InvestigatorsCirculation19969411280728168941106
- BristowMRbeta-adrenergic receptor blockade in chronic heart failureCirculation2000101555856910662755
- FiuzatMWojdylaDKitzmanDRelationship of beta-blocker dose with outcomes in ambulatory heart failure patients with systolic dysfunction: results from the HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training) trialJ Am Coll Cardiol201260320821522560018
- SimonTMary-KrauseMFunck-BrentanoCLechatPJaillonPBisoprolol dose-response relationship in patients with congestive heart failure: a subgroup analysis in the cardiac insufficiency bisoprolol study (CIBIS II)Eur Heart J200324655255912643888
- PrijicSBuchhornRMechanisms of beta-blockers action in patients with heart failureRev Recent Clin Trials201492586025198736
- RoyDTalajicMNattelSAtrial Fibrillation and Congestive Heart Failure InvestigatorsRhythm control versus rate control for atrial fibrillation and heart failureN Engl J Med2008358252667267718565859
- Montero-Perez-BarqueroMFlatherMRoughtonMInfluence of systolic blood pressure on clinical outcomes in elderly heart failure patients treated with nebivolol: data from the SENIORS trialEur J Heart Fail20141691009101525044535
- FloreaVGRectorTSAnandISCohnJNHeart failure with improved ejection fraction: clinical characteristics, correlates of recovery, and survival: results from the valsartan heart failure trialCirc Heart Fail201697e00312327413037
- EdelmannFMusial-BrightLGelbrichGCIBIS-ELD Investigators and Project Multicenter Trials in the Competence Network Heart FailureTolerability and feasibility of beta-blocker titration in HFpEF versus HFrEF: insights from the CIBIS-ELD trialJACC Heart Fail20164214014926682793
- TateCW3rdRobertsonADZoltyRQuality of life and prognosis in heart failure: results of the Beta-Blocker Evaluation of Survival Trial (BEST)J Card Fail200713973273717996821
- DobreDvan JaarsveldCHDejongsteMJHaaijer RuskampFMRanchorAVThe effect of beta-blocker therapy on quality of life in heart failure patients: a systematic review and meta-analysisPharmacoepidemiol Drug Saf200716215215916555368
- HjalmarsonAGoldsteinSFagerbergBEffects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study GroupJAMA2000283101295130210714728
- BoyleSHSamadZBeckerRCDepressive symptoms and mental stress-induced myocardial ischemia in patients with coronary heart diseasePsychosom Med201375982283124163385
- RanchordAMSpertusJABuchananDMGoschKLChanPSInitiation of β-blocker therapy and depression after acute myocardial infarctionAm Heart J2016174374226995368
- MengYLiuXLiuJChengXA prospective study on the impact of heart rate control achieved with metoprolol on cardiac performance, motor function and quality of life in Chinese chronic heart failure patientsInt J Cardiol201722726727127843047
- LiuXLouXChengXMengYImpact of metoprolol treatment on mental status of chronic heart failure patients with neuropsychiatric disordersDrug Des Devel Ther201711305312
- HuangJZhangRLiuXMengYImpact of metoprolol treatment on cardiac function and exercise tolerance in heart failure patients with neuropsychiatric disordersCurr Med Res Opin201834114114828532169
- GorreFVandekerckhoveHBeta-blockers: focus on mechanism of action. Which beta-blocker, when and why?Acta Cardiol201065556557021125979
- HariaMPloskerGLMarkhamAFelodipine/metoprolol: a review of the fixed dose controlled release formulation in the management of essential hypertensionDrugs200059114115710718104
- Effects of metoprolol CR in patients with ischemic and dilated cardiomyopathy: the randomized evaluation of strategies for left ventricular dysfunction pilot studyCirculation2000101437838410653828
- PackerMAntonopoulosGVBerlinJAChittamsJKonstamMAUdelsonJEComparative effects of carvedilol and metoprolol on left ventricular ejection fraction in heart failure: results of a meta-analysisAm Heart J2001141689990711376302
- BergTβ1-Blockers lower norepinephrine release by inhibiting presynaptic, facilitating β1-adrenoceptors in normotensive and hypertensive ratsFront Neurol201455124795691
- GreenPAnshelevichMTalrejaALong-term effects of carvedilol or metoprolol on left ventricular function in ischemic and nonischemic cardiomyopathyAm J Cardiol20059591114111615842987
- MetraMNodariSParrinelloGGiubbiniRMancaCDei CasLMarked improvement in left ventricular ejection fraction during long-term beta-blockade in patients with chronic heart failure: clinical correlates and prognostic significanceAm Heart J2003145229229912595847
- WilliamsEMHassanMOFlorasJSSleightPJonesJVAdaptation of hypertensives to treatment with cardioselective and non-selective beta-blockers. Absence of correlation between bradycardia and blood pressure control, and reduction in slope of the QT/RR relationBr Heart J19804454734876108122
- FlorasJSHassanMOJonesJVSleightPAmbulatory blood pressure and its variability during randomised double-blind administration of atenolol, metoprolol, pindolol and long acting propranolol in subjects with mild to moderate hypertensionDrugs198325Supplement 21925
- de Figueiredo NetoJAMadyCGrupiCEffects of metoprolol tartrate therapy in patients with heart failureArq Bras Cardiol200687332933517057934
- ChaveyWEThe importance of beta blockers in the treatment of heart failureAm Fam Physician2000621124532462 English, Portuguese11130231
- LiuFChenYFengXTengZYuanYBinJEffects of beta-blockers on heart failure with preserved ejection fraction: a meta-analysisPLoS One201493e9055524599093
- ChatterjeeSBiondi-ZoccaiGAbbateABenefits of β blockers in patients with heart failure and reduced ejection fraction: network meta-analysisBMJ2013346f5523325883
- MetraMNodariSD’AloiaABeta-blocker therapy influences the hemodynamic response to inotropic agents in patients with heart failure: a randomized comparison of dobutamine and enoximone before and after chronic treatment with metoprolol or carvedilolJ Am Coll Cardiol20024071248125812383572
- ArslanSErolMKGundogduFPrognostic value of 6-minute walk test in stable outpatients with heart failureTex Heart Inst J200734216616917622362
- McAuleyPMyersJAbellaJFroelicherVEvaluation of a specific activity questionnaire to predict mortality in men referred for exercise testingAm Heart J20061514890.e1897.e1
- WerdanKEbeltHNudingSADDITIONS Study InvestigatorsIvabradine in combination with metoprolol improves symptoms and quality of life in patients with stable angina pectoris: a post hoc analysis from the ADDITIONS trialCardiology20161332839026501486
- PetersDHBenfieldPMetoprolol: a pharmacoeconomic and quality-of-life evaluation of its use in hypertension, post-myocardial infarction and dilated cardiomyopathyPharmacoeconomics19946437040010147474
- WiklundIWaagsteinFSwedbergKHjalmarssonAQuality of life on treatment with metoprolol in dilated cardiomyopathy: results from the MDC trial. Metoprolol in Dilated Cardiomyopathy trialCardiovasc Drugs Ther19961033613688877080
- WaagsteinFBristowMRSwedbergKBeneficial effects of metoprolol in idiopathic dilated cardiomyopathy. Metoprolol in Dilated Cardiomyopathy (MDC) Trial Study GroupLancet19933428885144114467902479
- RiedLDMcFarlandBHJohnsonREBrodyKKBeta-blockers and depression: the more the murkier?Ann Pharmacother19983266997089640490
- HayesPESchulzSCBeta-blockers in anxiety disordersJ Affect Disord19871321191302890677
- MacMahonKMLipGYPsychological factors in heart failure: a review of the literatureArch Intern Med2002162550951611871918
- RutledgeTReisVALinkeSEGreenbergBHMillsPJDepression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomesJ Am Coll Cardiol20064881527153717045884
- WallePOWestergrenGDimenäsEOlofssonBAlbrektsenTEffects of 100 mg of controlled-release metoprolol and 100 mg of atenolol on blood pressure, central nervous system-related symptoms, and general well beingJ Clin Pharmacol19943477427477929868
