Abstract
Thyroid eye disease (TED) is a complex, debilitating autoimmune disease that causes orbital inflammation and tissue remodeling, resulting in proptosis, diplopia, and in severe cases, loss of vision. TED can lead to facial disfigurement and severely impact patients’ quality of life. Although the course of TED was identified over 60 years ago, effective treatment options have proved to be challenging. Current treatments such as glucocorticoid therapy and orbital radiation focus on reducing orbital inflammation. However, these therapies fail to modify the disease outcomes, including proptosis and diplopia. Recent advances in the understanding of the molecular basis of TED have facilitated the development of targeted molecular therapies such as teprotumumab, an insulin-like growth factor-1 receptor inhibiting monoclonal antibody. In recent phase 2 and phase 3 randomized placebo-controlled trials, teprotumumab rapidly achieved improvement in clinical endpoints defining TED, including improved proptosis and diplopia. Dramatic improvement in clinical outcomes achieved after teprotumumab therapy during active TED are heretofore singular and comparable only to surgical therapies achieved during the inactive phase of TED. The advent of effective medical therapy can lead to a paradigm shift in the clinical management of TED. This review will provide an overview of TED, its epidemiology, insight into the molecular biology of the disease, clinical characteristics and diagnosis, and current and emerging treatment modalities.
Introduction
Thyroid eye disease (TED) is a complex autoimmune disease characterized by orbital inflammation (active disease), with subsequent tissue remodeling and fibrosis when the disease becomes inactive.Citation2,Citation3 As TED progresses, it leads to proptosis, strabismus, corneal ulceration, and even optic neuropathy.Citation2,Citation4,Citation5
Several treatment strategies are available, which focus on immune suppression.Citation1 Though some provide short-term relief, they do not necessarily lead to disease course modification.Citation2 The management of TED remains a major clinical and therapeutic challenge, as insufficient treatment can negatively impact patients’ quality of life (QoL).Citation2,Citation6,Citation7 Consequently, there is still an unmet need for an effective disease-modifying treatment with a balanced safety-risk profile.Citation2,Citation8,Citation9 This review provides an overview of TED, its epidemiology, molecular biology, clinical characteristics and diagnosis, and current and emerging treatment modalities, including teprotumumab, an insulin-like growth factor-1 receptor (IGF-1R) inhibitor antibody.
Thyroid Eye Disease Epidemiology
TED is most often associated with Graves’ disease (GD), but also can occur in association with hypothyroidism, euthyroidism, and Hashimoto’s thyroiditis.Citation1,Citation10–Citation13 GD affects approximately 1% to 2% of the adult population,Citation8 with an estimated 40% of GD patients subsequently developing TED over the course of their lifetime.Citation14 The onset of TED typically occurs between 30 and 50 years of age, with the disease course more severe after age 50.Citation10,Citation15
TED often occurs within 18 months following a GD diagnosis.Citation16 It can, however, be diagnosed simultaneously or even before the diagnosis of GD.Citation17
In Europe, the reported prevalence of active and inactive TED is 10/10,000 individuals.Citation18 The only US study on incidence of TED was completed in the 1990s and indicates that the age-adjusted incidence rate for females is 16 cases/100,000 population/year, and 2.9 cases/100,000 population/year for males.Citation19 TED is 2.5- to 6-fold more common among women than men, but is on average, more severe in men.Citation15 Active TED is much less prevalent due to its defined disease course and moderate-to-severe TED occurs in less than 5/10,000 individuals.Citation18 About 37% of the overall TED population has active disease at any one time.Citation20
Risk Factors
Untreated thyroid dysfunction (hyper- or hypothyroidism) is associated with the development and progression of TED.Citation21 Smoking is the strongest risk factor associated with TED. The risk of developing TED has a greater association with the amount of cigarettes smoked following the diagnosis of GD rather than the cumulative cigarettes smoked.Citation22 Further, radioactive iodine, a commonly used treatment for hyperthyroidism, is also a known risk factor for both development and progression of TED.Citation23 Concomitant glucocorticoid usage appears to decrease the risk of the development or worsening of TED associated with radioactive iodine therapy.Citation21,Citation24
Molecular Biology Of Thyroid Eye Disease
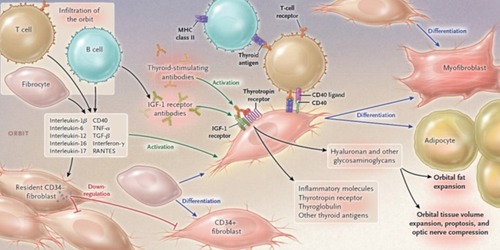
A complete understanding of the pathophysiology of TED has not been delineated, but evidence suggests that disease pathogenesis is related to loss of self-tolerance to thyroid-stimulating hormone receptor (TSH-R) and overexpression of IGF-1R.Citation8,Citation25–Citation27 The autoimmune orbital response occurs in TED because of cross-reactivity against antigens that are present in both the thyroid gland and orbital tissue, although the exact pathophysiology is still unclear.Citation11,Citation28 It appears that the production of thyroid-stimulating immunoglobulins (TSIs) mimics thyroid-stimulating hormone (TSH), leading to excessive thyroid hormone production and amplified actions on target tissues expressing TSH-R (ie, orbital fat, extraocular muscle, and orbital fibroblasts).Citation25 While TSI levels tend to be higher in patients with severe, active TED, a significant correlation between TSI levels and the disease course is lacking.Citation14 Therefore, measuring TSI levels is not considered a predictable biomarker to guide the clinical management of TED.Citation14
Investigations to determine the underlying cause of TED have recently focused on IGF-1R, as IGF-1R autoantibodies have been detected in GD patients.Citation29 IGF-1R, which is overexpressed in TED, forms a physical and functional interactive complex with TSH-R in orbital fibroblasts.Citation27 TSH-R and IGF-1R are involved in orbital tissue reactivity and remodeling via production of proinflammatory cytokines and synthesis of hyaluronan ().Citation8,Citation25–Citation27,Citation30–Citation32 IGF-1R is overexpressed in T cells, B-cells, fibroblasts, myofibroblasts, and fibrocytes in patients with GD.Citation33–Citation36 Furthermore, both IGF-1 and Graves’ disease-IgG increase hyaluronan concentrations to a similar extent in orbital fibroblasts from GD patients, but not in those from normal controls. These findings indicate an important role for IGF-1R in the pathogenesis of TED.Citation37
Figure 1 Pathophysiology of thyroid eye disease. In TED, B-lymphocytes, T-lymphocytes, and CD34+ fibrocytes infiltrate the orbit. CD34+ fibroblasts, originating from bone marrow-derived fibrocytes, further differentiate into myofibroblasts or adipocytes. Both CD34+ and residential CD34− fibroblasts are present within the orbit, and depending upon microenvironment-mediated signaling, can produce cytokines, including IL-1β, IL-6, IL-8, IL-16, TNF-α, RANTES, and CD40 ligand, which activate orbital fibroblasts. CD34+ fibroblasts express low levels of TSH-R, thyroglobulin, and additional thyroid antigens. TSIs activate the TSH-R/IGF-1R complex inducing inflammatory molecule expression and glycosaminoglycan synthesis. Furthermore, immunoglobulins directed against IGF-1R induce orbital fibroblast signaling, thereby increasing cytokine and hyaluronan production, and subsequent orbital tissue expansion, leading to proptosis and compression of the optic nerve. Adipogenesis also leads to orbital fat expansion. From N Engl J Med, Smith TJ, Hegedus L, Graves’ disease, 375(16), 1552–1565. Copyright © (2016) Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.Citation4
Clinical Characteristics And Diagnostic Criteria Of Thyroid Eye Disease
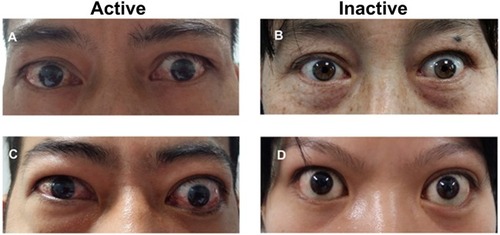
Clinical manifestations of active TED can vary and may include conjunctival chemosis and injection, lid swelling, lid retraction, proptosis, strabismus, exposure keratopathy, and optic neuropathy ().Citation38 Common symptoms may include eye pain, excessive lacrimation, diplopia, photophobia, and blurry vision.Citation39 According to a cohort of patients with TED in Minnesota, eyelid retraction was the most common clinical finding (90.8% of patients).Citation39 Upper eyelid retraction was present in >70% of patients, followed by proptosis (62%), restrictive myopathy (43%), and optic neuropathy (6%).Citation39 Upper eyelid retraction, along with proptosis resulting in lagophthalmos, can cause exposure keratopathy and ulceration. Dysfunction of Bell’s phenomenon due to inferior rectus restriction can further worsen corneal exposure.Citation1,Citation40 Soft tissue expansion and swelling of the brow fat and the premalar region can also occur in patients with TED, though with a much lower occurrence rate (2%).Citation41,Citation42
Figure 2 Clinical characteristics of thyroid eye disease. (A) Moderate active TED: lid retraction with evidence of orbital tissue inflammation; (B) Moderate inactive TED: lid retraction; (C) Severe active TED: upper eyelid retraction and binocular soft tissue inflammation; (D) Severe inactive TED: lid retraction with proptosis. Reproduced from Li Q, Ye H, Ding Y, et al. Clinical characteristics of moderate-to-severe thyroid associated ophthalmopathy in 354 Chinese cases. PLoS One. 2017;12(5):e0176064. Creative Commons License and Disclaimer available from: http://creativecommons.org/licenses/by/4.0/legalcode.Citation38
The most feared complication of TED is dysthyroid optic neuropathy. Risk factors include older age, male gender, and smoking.Citation43,Citation44 The onset of dysthyroid optic neuropathy can be gradual and subtle, with decreased color vision as the most common presenting feature. Visual field defects may also be present.Citation45 A European Group on Graves’ Orbitopathy (EUGOGO) study investigated characteristics of patients with dysthyroid optic neuropathy.Citation46 A significant portion of these patients lacked severe inflammation and congestion, as 28% of patients with TED had a clinical activity score (CAS) of three or less.Citation1,Citation46 Therefore, clinical activity score should not be considered as a correlate to optic neuropathy in clinical management, as it can potentially delay treatment. Further, color vision was abnormal in the majority of patients. Exophthalmometry was greater than 20 mm in two-thirds of the patients. Visual field defects included arcuate or altitudinal defects, central/paracentral scotomas, or generalized depression.Citation40 Most of these patients had normal appearing optic nerves.Citation46 Apical muscle crowding was seen in 88% of patients with dysthyroid optic neuropathy.Citation46 If there is a delay in treatment, patients can develop permanent optic nerve atrophy and irreversible vision loss.
The clinical course of TED frequently follows a pattern first described over 60 years ago by Francis Rundle ().Citation47 Active TED is an inflammatory, progressive disease characterized by orbital or periorbital inflammation. It generally lasts from 6 to 24 months, but can be present for up to 3 years. The disease then progresses to stable, chronic, fibrotic, inactive disease. Despite reduced inflammation, permanent damage may result and patients do not typically experience significant clinical improvement, responding only to surgery at this point.Citation11
Figure 3 An approximation of a curve depicting severity of thyroid eye disease over time that is based on a concept by Rundle.Citation110
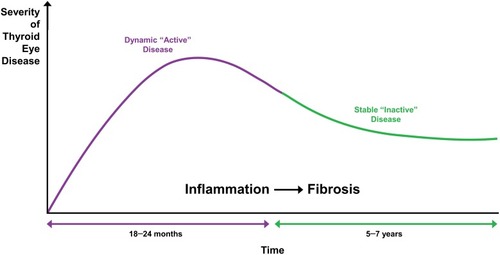
Once the patient’s disease progresses to inactive TED, their clinical course is typically stable. A small percentage (5–16%) of patients can experience reactivation of the inflammatory phase, with worsening proptosis as the most common clinical presentation.Citation48,Citation49 Risk factors include smoking during initial TED presentation, periocular surgery, pregnancy, and uncontrolled hypo- or hyperthyroidism.Citation48–Citation51
Various outcome assessment scales are used in clinical trials, and to a lesser extent in practice, to evaluate effectiveness of therapies for TED.Citation1 CAS assesses the presence of inflammatory symptoms and was initially developed to identify active inflammation to help predict glucocorticoid therapy response ().Citation16 It is used to help identify active TED patients and document their response to treatment over time.Citation52 A list of seven inflammatory orbital symptoms representing pain, redness, and swelling constitute the CAS with the presence of three or more indicating the patient is active.Citation52 The list can be expanded to 10 symptoms for follow-up.Citation52 There are several classification systems in rather limited use (eg, NOSPECS [No physical signs or symptoms, Only signs, Soft tissue involvement, Proptosis, Extraocular muscle signs, Corneal involvement, and Sight loss; ], VISA [Vision, Inflammation, Strabismus, and Appearance], and EUGOGO).Citation11,Citation52
Table 1 Clinical Activity Scorea
Table 2 NOSPECS Classification
In clinical practice, TED is generally diagnosed via a combination of medical history, presenting symptoms, radiographic imaging, and laboratory results (eg, TSH, TSI, thyroid peroxidase antibody, and TSH-R antibody levels).Citation1,Citation11 However, not every clinician chooses the same combination of diagnostic tools, and there continues to be a lack of standardization. Improved assessment techniques in the future may be beneficial to better guide clinicians.Citation16
Treatment Modalities For Thyroid Eye Disease
Treatment options for TED generally depend on disease activity and severity ().Citation1,Citation53 Active and inactive TED can vary in severity, typically described as mild, moderate-to-severe, or sight-threatening.Citation1 In active, mild TED, ocular lubricants, sunglasses, and prisms are used for supportive management.Citation10,Citation53 For active, moderate or severe disease, a variety of treatment strategies are used, sometimes resulting in short-term relief. However, there is still an unmet need for disease-modifying treatments with an optimal safety profile and long-term benefits.Citation1,Citation2
Table 3 Current And Emerging Therapies For Thyroid Eye Disease
Orbital Radiation
Orbital radiation (OR) has been used for the treatment of TED for several decades, and is generally well-tolerated.Citation54 The rationale for its use is two-fold. The first lies in its nonspecific anti-inflammatory effect, and the second is the radio-sensitivity of orbit-infiltrating lymphocytes.Citation54,Citation55 Additionally, OR may target fibroblasts leading to reduced glycosaminoglycan synthesis and secretion.Citation56
However, due to non-standardized protocols and relative lack of randomized clinical trial results, the use of OR is not without controversy. Three randomized clinical trials found differing results. While Gorman et al did not find a difference between OR and sham therapy,Citation57 Mourits et al found OR to be superior to sham.Citation58 Prummel et al found OR to be effective in reducing diplopia and improving extraocular muscle motility in patients with mild TED, although there was no effect on QoL or disease progression.Citation59 Further studies evaluating concomitant OR with intravenous (IV) or oral glucocorticoids also yielded dissimilar results.Citation60–Citation63 A report from the American Academy of Ophthalmology concluded that there is considerable heterogeneity and variability in the quality of studies assessing the benefit of OR for the treatment of TED.Citation64 Overall, OR appears to offer little, if any, long-term clinical benefit.
Immunosuppression
Glucocorticoids
In Europe, glucocorticoids are considered the first-line treatment for active TED to reduce edema and orbital inflammation, as recommended by the EUGOGO guidelines.Citation1 IV pulse glucocorticoid administration is preferred to oral administration, as it has a more favorable efficacy and safety profile.Citation8,Citation10 However, high-dose systemic glucocorticoid therapy can have undesired adverse effects, including the development of Cushingoid features, hypertension, hyperglycemia, mood instability, weight gain, and osteoporosis.Citation10 Although glucocorticoids are frequently used in the treatment of TED, their therapeutic efficacy has not been confirmed by adequate placebo-controlled trials to date.Citation14 In a study investigating three cumulative IV doses of methylprednisolone (2.25 g, 4.98 g, and 7.47 g) in patients with active, moderate-to-severe TED, the 7.47 g dose (over a 12-week period) reduced CAS and mildly improved ocular motility.Citation65 However, it did not improve proptosis or diplopia significantly and was associated with significant adverse events (AEs), such as diabetes mellitus, psychosis, and depression.Citation65 Furthermore, the only placebo-controlled trial showed that methylprednisolone pulse therapy did not significantly improve mean proptosis or diplopia.Citation66 Diplopia improved in 50% (2/4) of methylprednisolone-treated patients compared with 0% (0/5) of placebo-treated patients, although the improvement was not statistically significant (P = 0.073). Proptosis improved in 40% (2/5) of methylprednisolone-treated patients and in 29% (2/7) of placebo-treated patients, which was also not statistically significant (P = 0.68).Citation66
Periocular and orbital glucocorticoid administration are alternative proposed treatment options that can limit systemic side effects. A multicentered, randomized, controlled study found that patients who received four inferolateral orbital injections of 20 mg of triamcinolone acetate 40 mg/mL (24 patients vs 17 patients in the control group) experienced improvement in diplopia, with radiographic imaging showing a reduction in the size of extraocular muscles.Citation67 Although patients also reported fewer side effects, these treatments failed to demonstrate consistent efficacy. Larger trials are needed to fully evaluate the efficacy of locally administered glucocorticoids.Citation67
Mycophenolate
Mycophenolate mofetil (MMF), an immunosuppressant, is converted to mycophenolic acid (MPA) via the action of hepatic esterase and inhibits guanosine monophosphate synthesis (de novo purine synthesis).Citation68,Citation69 MPA potently inhibits the type 2 isoform of inosine monophosphate dehydrogenase, thereby inhibiting lymphocyte proliferation.Citation68,Citation70 This immune modulatory effect led to the evaluation of MPA for the treatment of TED.Citation68–Citation70
The safety of MPA in patients with active, moderate-to-severe TED was evaluated in a prospective longitudinal study over 24 weeks, with concomitant intravenous steroids during the first 12 weeks.Citation68 AEs were reported in 68% (36/53) of patients.Citation68 Serious AEs were reported in 13% (7/53) of patients, but none were considered treatment-related.Citation68
Mycophenolate was subsequently evaluated in combination with methylprednisolone in active, moderate-to-severe TED in a randomized, observer-masked, multicenter, open-label 36-week trial.Citation70 The primary outcome was not met, although statistically significant improvements were noted in the methylprednisolone plus mycophenolate groups at both 24 and 36 weeks in post hoc analyses.Citation70 Overall, cumulative results suggest that MMF may be a well-tolerated option to treat TED, but it appears to offer minimal long-term benefit.Citation69
Cyclosporine
Cyclosporine, alone or in combination with glucocorticoid therapy, has been proposed as an effective treatment for TED.Citation71,Citation72 A randomized controlled trial compared cyclosporine plus prednisone to prednisone only for 10 weeks.Citation72 A greater improvement in CAS and visual acuity were observed with combination therapy at 10 weeks when compared with prednisone monotherapy at 10 weeks (P <0.001 and P <0.01, respectively).Citation72 However, after 10 weeks, there were no significant improvements in proptosis, CAS, or visual acuity. Moreover, relapses occurred in 40% (8/20) of patients in the prednisone group during the following 6 months and in 5% (1/20) in the combined treatment group at 9 months.Citation72 AEs included increased liver enzymes and hypertension.Citation72 In another study, the response in total eye score after 12 weeks with prednisone alone was 61% (11/18) as compared with 22% (4/18) for the cyclosporine only group (P = 0.018).Citation71 However, neither group had significant improvement in proptosis or eye muscle score.Citation71 Patients in both groups who did not respond received combination therapy of cyclosporine and a low dose of prednisone for an additional 12 weeks and overall response was improved in some patients. Again, there was no consistent benefit in mean proptosis or eye muscle score from 12 to 24 weeks.Citation71 Therefore, cyclosporine may offer improved anti-inflammatory potential, but there is no data to suggest long-term clinical improvement in proptosis or strabismus.
Others
Studies have shown that high dose IV immunoglobulin is as effective as high doses of oral glucocorticoids.Citation73,Citation74 However, this is not routinely used today for the treatment of TED. Other immunosuppressive medications, such as somatostatin analogues, azathioprine, and ciamexone have, in aggregate, been found ineffective in the treatment of TED.Citation75–Citation80
Surgical Management Of Thyroid Eye Disease
Surgical intervention for TED is typically a multi-staged approach of sequential orbital decompression, eye muscle surgery, and/or eyelid surgery.Citation1 Most patients with TED will not require surgical intervention, with previous reports showing that 20% of patients undergo ≥1 surgical procedures.Citation81 The probability of undergoing surgery was 5% at 1 year after diagnosis, 9.3% at 2 years, 15.9% at 5 years, and rose to 21.8% at 10 years.Citation81 Up to 27% of patients are offered surgery after the disease becomes inactive.Citation20 The need for surgical intervention increased with age, with patients aged ≥50 years having a 2.6-times greater risk.Citation81
Surgical decompression is generally performed on TED patients with inactive stable disease, but also can be used for active patients when vision is threatened by compression optic neuropathy.Citation11,Citation16 The orbital surgeon may decide to perform fat decompression as well as bony decompression.Citation1 In general, between 5% and 20% of TED patients will undergo decompression surgery.Citation82 Unfortunately, orbital surgery can reactivate inflammation, exacerbating ophthalmopathy, and orbital decompression can cause strabismus in one-third of patients.Citation2,Citation83
The enlargement and fibrosis of extraocular muscles in TED can cause restrictive strabismus and diplopia, which can significantly affect QoL.Citation84 The inferior and medial recti muscles are most commonly affected. Strabismus surgery is typically performed following orbital decompression, due to the risk of worsening of diplopia.Citation1 The primary goal of strabismus surgery is for binocular vision in primary gaze and down gaze, and secondarily to improve the window of single binocular vision.Citation85 The typical surgical plan includes recession of the restricted muscle. It is important to discuss expectations, as patients may need additional strabismus surgery or require the aid of prisms.
Upper eyelid retraction is the most common feature of TED.Citation86 Its pathophysiology includes GD-induced sympathetic excess and eyelid fibrosis. Upper eyelid retraction, along with proptosis, can cause exposure keratopathy and ulceration due to lagophthalmos. There are various techniques to correct upper eyelid retraction, including graded müllerectomy or full thickness blepharotomy.Citation87,Citation88 Good, predictable results have been achieved with these different procedures, and treatment decision is ultimately guided by surgeon preference and experience.
Similarly, lower eyelid retraction is theorized to be caused by sympathetic overstimulation and fibrosis.Citation89 A transconjunctival approach is typically favored, in which the lower eyelid retractors are recessed or separated. Spacer grafts (homologous, autologous, or alloplastic material) can be used if the retraction is severe.Citation90,Citation91
Smoking Cessation
As previously mentioned, cigarette smoking is a significant risk factor for the development and progression of TED.Citation92 Microarray analysis of intra-orbital fat from both smokers and nonsmokers with active TED revealed differences in gene expression, including 103 genes that were upregulated and 54 genes that were downregulated.Citation93 In particular, IL-1β and IL-6 expression were upregulated 2.3-fold (P = 0.03) and 2.4-fold (P = 0.004), respectively, in intraorbital fat from smokers with TED compared with their nonsmoker counterparts.Citation93
A prospective study demonstrated the negative impact of smoking on the treatment response following OR or glucocorticoid therapy in patients with active, moderate TED. A greater number of nonsmokers had improved motility (60% vs 24%, P <0.017) and reduction in CAS compared with smokers after 12 months (P <0.05).Citation22 However, no significant changes were observed in proptosis after 12 months.Citation22 Patients should be advised that smoking exacerbates the severity of ophthalmopathy and lessens the response to treatment.Citation94
Selenium
Selenium was evaluated as a therapeutic option in a randomized, double-blind, placebo-controlled trial in euthyroid patients with mild TED.Citation95 Patients were treated with 100 µg sodium selenite twice per day for 6 months with an additional 6-month follow-up period.Citation95 The selenium-treated patients had a significant improvement in QoL and CAS, compared with placebo at 6 and 12 months (P <0.001). Symptomatic improvement was observed in 61% (33/54) of the selenium-treated patients compared with 36% (18/50) of the placebo group.Citation95 Furthermore, only 7% (4/54) of patients in the selenium group had disease progression, compared with 26% (13/50) in the placebo group.Citation95 Selenium was not associated with any AEs.Citation95 However, no significant changes in proptosis at 6 or 12 months were reported.Citation95 Limitations of this study included the lack of serum selenium assessment at baseline and throughout the study.Citation95 Since most patients originated from areas where the general population has marginally reduced selenium levels, a slight selenium deficiency may have confounded a beneficial effect upon supplementation.Citation95 The reported beneficial effects of selenium have not been demonstrated in a selenium-rich or nondeficient population to date.
Others
Other antioxidants, such as allopurinol and nicotinamide, have been suggested to improve visual acuity, reduce differential pressure, and improve ocular motility in patients with TED. However, there is insufficient clinical data to demonstrate benefits or efficacy.Citation96,Citation97 These antioxidants are not routinely used in clinics and are not approved for treatment of TED.
Novel, Targeted Biological Therapies
Thyroid-Stimulating Hormone Receptor Inhibitors
Antibodies that inhibit the TSH-R are under consideration as potential treatment options for TED.Citation25 An array of small-molecule TSH-R antagonists have been tested in vitro and in vivo in preclinical models, but no robust clinical trials have been conducted to date.Citation25
Tocilizumab
Tocilizumab, an IL-6 receptor monoclonal antibody, is approved for the treatment of active, moderate-to-severe rheumatoid arthritis and giant cell arteritis and is under consideration as a potential treatment for TED.Citation9,Citation98,Citation99 IL-6 is a proinflammatory cytokine produced by a variety of cells, including fibroblasts, monocytes, and T and B lymphocytes, which are implicated in the disease process of TED.Citation9 It is found in high concentrations in the serum of patients with TEDCitation100 A small study showed that tocilizumab reduced inflammation in patients who were unable to tolerate glucocorticoids.Citation101 A more recent randomized clinical trial (NCT01297699) showed that 93.3% of patients treated with tocilizumab vs 58.8% receiving placebo met the primary endpoint of reduction of CAS by ≥2 points at week 16 (P = 0.04; odds ratio, 9.8; 95% confidence interval [CI] 1.3–73.2).Citation102 However, tocilizumab did not significantly improve diplopia. In addition, although tocilizumab significantly improved median proptosis at week 16 compared with placebo (P = 0.003), the magnitude of the reduction from baseline was only 1.5 mm, which may not be a clinically significant reduction.Citation102 At week 40, 93 AEs were reported among 27 patients; the most common being headache (11 tocilizumab vs 4 placebo) and infections (17 vs 7). There were serious AEs in 2 patients receiving tocilizumab (one with a moderate increase in transaminase levels, attributed to latent tuberculosis, and another with acute pyelonephritis).Citation102
Anti-tumor Necrosis Factor-Alpha Agents
In a small retrospective, off-label study, there was subjective improvement in diplopia, pain, and swelling in 40% (4/10) of patients; following 3 months of adalimumab therapy (an initial injection of 80 mg followed by 40mg injections twice per week). However, there were no significant improvements in proptosis or extraocular movement restriction.Citation103 A case report showed that an infliximab infusion improved symptoms (pain related to corneal exposure and ocular movement), visual acuity, color vision, and CAS.Citation104 While these findings suggest that anti-tumor necrosis factor-alpha agents may benefit some TED patients, larger studies are needed to confirm their efficacy and safety.Citation105
Rituximab
Rituximab is a chimeric monoclonal antibody targeting CD20, a membrane-embedded protein expressed on the surface of pre-B and mature B lymphocytes.Citation106 Since rituximab depletes CD20-carrying B-cells, it was proposed as a potential treatment for TED.Citation8 Two small controlled trials were conducted to evaluate the efficacy of rituximab,Citation80,Citation107 with inconsistent results. In one study, rituximab (500 mg or 2000 mg) and IV methylprednisolone (7.5 g) both decreased CAS (more pronounced in the rituximab group compared to IV methylprednisolone at 16, 20, and 24 weeks).Citation107 After 24 weeks, 15/15 (100%) patients on rituximab improved (decrease of ≥2 points in CAS and CAS <3), compared with 11/16 (69%) patients with CAS <3 (P <0.05) and 12/16 (75%) with a CAS decrease by ≥2 points (NS) in the IV methylprednisolone group.Citation107 However, none of the patients receiving rituximab had ≥2 mm reductions in proptosis at week 24.Citation107 In the second study, 25 patients were administered 2 infusions of rituximab (1000 mg each) or IV normal saline 2 weeks apart.Citation80 At 24 and 52 weeks, rituximab did not significantly improve CAS, proptosis, diplopia, or QoL, and did not reduce orbital fat/muscle volume.Citation80 In summary, rituximab was associated with AEs and has shown no benefits over placebo with respect to the major serious outcomes of TED, such as proptosis and diplopia.Citation80
Teprotumumab
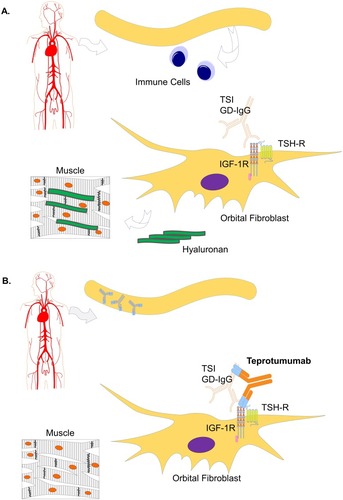
Teprotumumab, an IGF-1R inhibitory antibody, binds with high affinity and specificity to IGF-1R,Citation35 inducing internalization and degradation of the antibody-receptor complex.Citation14 In vitro studies show that IGF-1R and TSH-R form a physical complex.Citation2,Citation27,Citation35 Production of proinflammatory cytokine (eg, IL-6 and IL-8) is increased via IGF-1R/TSH-R–mediated activation of fibroblasts.Citation35 In vitro studies showed that teprotumumab attenuates such TSH-mediated cytokine production by reducing IGF-1R and TSH-R cell surface expression.Citation35 Moreover, teprotumumab inhibits IGF-1 and TSH-mediated Akt phosphorylation, thereby attenuating IGF-1R and TSH-R–mediated signaling.Citation35 Therefore, teprotumumab reduces hyaluronan production and cytokine stimulation in orbital fibroblasts,Citation32,Citation35 leading to reduced intraorbital hyaluronan accumulation and reduced adipogenesis and muscle expansion ().Citation2
Figure 4 Mechanism of action of teprotumumab. (A) Evidence suggests that TED occurs due to upregulation of the TSH-R/IGF-1R complex consequential to pathogenic autoantibody (GD-IgG and TSI) stimulation of fibroblasts. Such activation leads to the production of glycosaminoglycans (eg, hyaluronan), and expansion of fat and muscle next to the eye.Citation2 (B) Teprotumumab attenuates pathogenic autoantibody-mediated stimulation of orbital fibroblasts, thereby inhibiting TSH-R signaling, and correcting active TED endpoints, including proptosis and diplopia.Citation35,Citation108 Modified from Douglas RS. Teprotumumab, an insulin-like growth factor-1 receptor antagonist antibody, in the treatment of active thyroid eye disease: a focus on proptosis. Eye (Lond). 2019;33(2):183–198. Creative Commons License and Disclaimer available from: http://creativecommons.org/licenses/by/4.0/legalcode.Citation2
The phase 2 multicenter, double-masked, placebo-controlled, randomized clinical trial (NCT01868997) evaluating the efficacy and safety of teprotumumab enrolled 88 patients with recent onset, active, moderate-to-severe TED.Citation108 Patients were randomized (1:1) to receive teprotumumab or placebo.Citation108 Patients received a total of 8 infusions over the 24-week observation period, with 1 IV infusion every 3 weeks, (first dose: 10 mg per kg; subsequent doses: 20 mg per kg; last dose at week 21).Citation108 The primary endpoint was a decrease in CAS of ≥2 points and a reduction in proptosis of ≥2 mm, without an equal deterioration in the nonstudy eye.Citation108 The teprotumumab-treated patients improved significantly compared with the placebo group at 6, 12, 18, and 24 weeks (all P <0.001), with 69% of teprotumumab-treated patients achieving the outcome at 24 weeks (vs 20% of placebo).Citation108 Furthermore, the effect observed after 6 weeks was following only 2 infusions.Citation108 Additionally, 71.4% of teprotumumab-treated patients (vs 20.0% of placebo-treated patients) had ≥2 mm reduction in proptosis at week 24 (P <0.001).Citation2 The greatest improvement was seen in the more severely affected patients,Citation2 with 40% (17/42) of patients receiving teprotumumab experiencing a ≥4 mm reduction in proptosis at week 24 vs 0 (0/45) patients in the placebo group.Citation108 To reduce the chances of variability in evaluation of proptosis, the same type of exophthalmometer was used at each study site and the same site observer completed each patient evaluation. Strikingly, this degree of amelioration in proptosis is consistent with that observed following surgical intervention.Citation2,Citation83,Citation108
QoL was significantly improved vs placebo at each visit following teprotumumab treatment, as determined by the overall Graves’ ophthalmopathy (GO)-QoL scores.Citation108 In addition, a higher number of teprotumumab-treated patients had an improvement in subjectively evaluated diplopia, compared to placebo-treated patients.Citation108 Teprotumumab continued to exert beneficial effects 7 weeks after the final infusion, with the number of patients with reduced CAS and proptosis continuing to increase.Citation108 Furthermore, teprotumumab was well-tolerated and the majority of AEs were mild, well-controlled, and resolved without treatment.Citation108 Hearing impairment was observed in 3 (7%) teprotumumab-treated and 0 placebo-treated patients.Citation108 Hyperglycemia occurred in a small number of patients in both groups. In the teprotumumab-treated group, hyperglycemia was grade 1 in patients with no history of diabetes.Citation108 In diabetic patients, hyperglycemia was grade 2 or 3, and resolved with adjustment of diabetes medication.Citation108 In the teprotumumab-treated patients, hyperglycemia was thought to be due to IGF-1R inhibition, although teprotumumab lacks affinity for the insulin receptor.Citation108 Consequently, recommendations include close monitoring of diabetic patients treated with teprotumumab.Citation108
The findings from the phase 2 trial were recently confirmed with the initial release of results from the phase 3 placebo-controlled trial, which indicated a significant reduction in the primary outcome, defined as the percentage of patients with a ≥2-mm reduction in proptosis at week 24 with teprotumumab vs placebo.Citation109
Conclusion
TED was described over 60 years ago,Citation47 but there have been few advancements in the effective therapeutic management of the disease since.Citation2 Recent developments in the understanding of the molecular basis of TED have led to the development of targeted therapies, such as teprotumumab, which appears to regress the historically resistant progressive outcomes of muscle and fat expansion.Citation2,Citation108 The phase 2 findings, confirmed with the initial release of the phase 3 data, demonstrated dramatic improvement in proptosis and diplopia over the 24-week study periods, and were similar to those obtained with surgery, indicating that there may be yet a viable therapeutic option for patients with active TED.Citation2,Citation108,Citation109
Abbreviations
AE, adverse event; CAS, clinical activity score; GD, Graves’ disease; IGF-1R, insulin-like growth factor-1 receptor; IL, interleukin; MMF, mycophenolate mofetil; MPA, mycophenolic acid; OR, orbital radiation; QoL, quality of life; TED, thyroid eye disease; TNF-α, tumor necrosis factor alpha; TSH-R, thyroid-stimulating hormone receptor; TSI, thyroid stimulating immunoglobulins.
Acknowledgments
The authors would like to thank Robert J. Holt, PharmD, MBA; and Megan Francis-Sedlak, PhD, Medical Affairs, Horizon Therapeutics plc, for helpful discussions. Medical writing and editorial support were provided by Marie-Louise Ricketts, PhD; and Claire Daniele, PhD, of AlphaBioCom, LLC, King of Prussia, PA. Support for preparation of this manuscript was provided by Horizon, Lake Forest, IL. The funder was not involved in writing the article or the decision to submit the article for publication.
Disclosure
Raymond S. Douglas is a consultant for Horizon Therapeutics, plc. The authors report no other conflicts of interest in this work.
References
- Bartalena L, Baldeschi L, Boboridis K, et al. The 2016 European Thyroid Association/European group on Graves’ orbitopathy guidelines for the management of graves’ orbitopathy. Eur Thyroid J. 2016;5(1):9–26. doi:10.1159/00044382827099835
- Douglas RS. Teprotumumab, an insulin-like growth factor-1 receptor antagonist antibody, in the treatment of active thyroid eye disease: a focus on proptosis. Eye (Lond). 2019;33(2):183–198. doi:10.1038/s41433-018-0321-y30575804
- Smith TJ. New advances in understanding thyroid-associated ophthalmopathy and the potential role for insulin-like growth factor-I receptor. F1000Res. 2018;7:134. doi:10.12688/f1000research29744034
- Smith TJ, Hegedus L. Graves’ disease. N Engl J Med. 2016;375(16):1552–1565. doi:10.1056/NEJMra151003027797318
- Verity DH, Rose GE. Acute thyroid eye disease (TED): principles of medical and surgical management. Eye (Lond). 2013;27(3):308–319. doi:10.1038/eye.2012.28423412559
- Kahaly GJ, Petrak F, Hardt J, Pitz S, Egle UT. Psychosocial morbidity of Graves’ orbitopathy. Clin Endocrinol (Oxf). 2005;63(4):395–402. doi:10.1111/j.1365-2265.2005.02352.x16181231
- Park JJ, Sullivan TJ, Mortimer RH, Wagenaar M, Perry-Keene DA. Assessing quality of life in Australian patients with Graves’ ophthalmopathy. Br J Ophthalmol. 2004;88(1):75–78. doi:10.1136/bjo.88.1.7514693779
- Minakaran N, Ezra DG. Rituximab for thyroid-associated ophthalmopathy. Cochrane Database Syst Rev. 2013;5:CD009226.
- Hamed Azzam S, Kang S, Salvi M, Ezra DG. Tocilizumab for thyroid eye disease. Cochrane Database Syst Rev. 2018;11:CD012984.30480323
- Douglas RS, Gupta S. The pathophysiology of thyroid eye disease: implications for immunotherapy. Curr Opin Ophthalmol. 2011;22(5):385–390. doi:10.1097/ICU.0b013e328349944621730841
- Bothun ED, Scheurer RA, Harrison AR, Lee MS. Update on thyroid eye disease and management. Clin Ophthalmol. 2009;3:543–551. doi:10.2147/opth.s522819898626
- Cyranska-Chyrek E, Olejarz M, Szczepanek-Parulska E, Stajgis P, Pioch A, Ruchala M. Severe unilateral orbitopathy in a patient with Hashimoto’s thyroiditis - a case report. BMC Ophthalmol. 2019;19(1):9. doi:10.1186/s12886-018-1018-530621642
- Perros P, Neoh C, Dickinson J. Thyroid eye disease. Br Med J. 2009;338:b560. doi:10.1136/bmj.b90219270020
- Mohyi M, Smith TJ. IGF1 receptor and thyroid-associated ophthalmopathy. J Mol Endocrinol. 2018;61(1):T29–T43. doi:10.1530/JME-17-027629273685
- Sahli E, Gunduz K. Thyroid-associated ophthalmopathy. Turk J Ophthalmol. 2017;47(2):94–105. doi:10.4274/tjo.8068828405484
- Gillespie EF, Smith TJ, Douglas RS. Thyroid eye disease: towards an evidence base for treatment in the 21st century. Curr Neurol Neurosci Rep. 2012;12(3):318–324. doi:10.1007/s11910-012-0256-922354545
- Khoo DH, Eng PH, Ho SC, et al. Graves’ ophthalmopathy in the absence of elevated free thyroxine and triiodothyronine levels: prevalence, natural history, and thyrotropin receptor antibody levels. Thyroid. 2000;10(12):1093–1100. doi:10.1089/thy.2000.10.109311201855
- Perros P, Hegedus L, Bartalena L, et al. Graves’ orbitopathy as a rare disease in Europe: a European Group on Graves’ Orbitopathy (EUGOGO) position statement. Orphanet J Rare Dis. 2017;12(1):72. doi:10.1186/s13023-017-0625-128427469
- Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477–588.7886878
- Perros P, Zarkovic M, Azzolini C, et al. PREGO (presentation of Graves’ orbitopathy) study: changes in referral patterns to European Group On Graves’ Orbitopathy (EUGOGO) centres over the period from 2000 to 2012. Br J Ophthalmol. 2015;99(11):1531–1535. doi:10.1136/bjophthalmol-2015-30673325953846
- Stan MN, Bahn RS. Risk factors for development or deterioration of Graves’ ophthalmopathy. Thyroid. 2010;20(7):777–783. doi:10.1089/thy.2010.163420578901
- Eckstein A, Quadbeck B, Mueller G, et al. Impact of smoking on the response to treatment of thyroid associated ophthalmopathy. Br J Ophthalmol. 2003;87(6):773–776. doi:10.1136/bjo.87.6.77312770979
- Roos JCP, Paulpandian V, Murthy R. Serial TSH-receptor antibody levels to guide the management of thyroid eye disease: the impact of smoking, immunosuppression, radio-iodine, and thyroidectomy. Eye (Lond). 2019;33(2):212–217. doi:10.1038/s41433-018-0242-930401900
- Bartalena L, Marcocci C, Bogazzi F, et al. Relation between therapy for hyperthyroidism and the course of Graves’ ophthalmopathy. N Engl J Med. 1998;338(2):73–78. doi:10.1056/NEJM1998010833802019420337
- Smith TJ. TSHR as a therapeutic target in Graves’ disease. Expert Opin Ther Targets. 2017;21(4):427–432. doi:10.1080/14728222.2017.128821528127991
- Smith TJ, Janssen JA. Building the case for insulin-like growth factor receptor-I involvement in thyroid-associated ophthalmopathy. Front Endocrinol (Lausanne). 2017;7:167. doi:10.3389/fendo.2016.0016728096798
- Tsui S, Naik V, Hoa N, et al. Evidence for an association between thyroid-stimulating hormone and insulin-like growth factor 1 receptors: a tale of two antigens implicated in Graves’ disease. J Immunol. 2008;181(6):4397–4405. doi:10.4049/jimmunol.181.6.439718768899
- Bahn RS, Dutton CM, Natt N, Joba W, Spitzweg C, Heufelder AE. Thyrotropin receptor expression in graves’ orbital adipose/connective tissues: potential autoantigen in Graves’ ophthalmopathy. J Clin Endocrinol Metab. 1998;83(3):998–1002. doi:10.1210/jcem.83.3.46769506762
- Weightman DR, Perros P, Sherif IH, Kendall-Taylor P. Autoantibodies to IGF-1 binding sites in thyroid associated ophthalmopathy. Autoimmunity. 1993;16(4):251–257.7517705
- Alsuhaibani AH, Nerad JA. Thyroid-associated orbitopathy. Semin Plast Surg. 2007;21(1):65–73. doi:10.1055/s-2007-96775120567660
- Smith TJ, Hegedus L, Douglas RS. Role of insulin-like growth factor-1 (IGF-1) pathway in the pathogenesis of Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab. 2012;26(3):291–302. doi:10.1016/j.beem.2011.10.00222632366
- Krieger CC, Neumann S, Place RF, Marcus-Samuels B, Gershengorn MC. Bidirectional TSH and IGF-1 receptor cross talk mediates stimulation of hyaluronan secretion by Graves’ disease immunoglobins. J Clin Endocrinol Metab. 2015;100(3):1071–1077. doi:10.1210/jc.2014-356625485727
- Douglas RS, Gianoukakis AG, Kamat S, Smith TJ. Aberrant expression of the insulin-like growth factor-1 receptor by T cells from patients with Graves’ disease may carry functional consequences for disease pathogenesis. J Immunol. 2007;178(5):3281–3287. doi:10.4049/jimmunol.178.5.328117312178
- Douglas RS, Naik V, Hwang CJ, et al. B cells from patients with Graves’ disease aberrantly express the IGF-1 receptor: implications for disease pathogenesis. J Immunol. 2008;181(8):5768–5774. doi:10.4049/jimmunol.181.8.576818832736
- Chen H, Mester T, Raychaudhuri N, et al. Teprotumumab, an IGF-1R blocking monoclonal antibody inhibits TSH and IGF-1 action in fibrocytes. J Clin Endocrinol Metab. 2014;99(9):E1635–E1640. doi:10.1210/jc.2014-158024878056
- Pritchard J, Horst N, Cruikshank W, Smith TJ. Igs from patients with Graves’ disease induce the expression of T cell chemoattractants in their fibroblasts. J Immunol. 2002;168(2):942–950. doi:10.4049/jimmunol.168.2.94211777993
- Smith TJ, Hoa N. Immunoglobulins from patients with Graves’ disease induce hyaluronan synthesis in their orbital fibroblasts through the self-antigen, insulin-like growth factor-I receptor. J Clin Endocrinol Metab. 2004;89(10):5076–5080. doi:10.1210/jc.2004-071615472208
- Li Q, Ye H, Ding Y, et al. Clinical characteristics of moderate-to-severe thyroid associated ophthalmopathy in 354 Chinese cases. PLoS One. 2017;12(5):e0176064. doi:10.1371/journal.pone.017606428472149
- Bartley GB, Fatourechi V, Kadrmas EF, et al. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996;121(3):284–290. doi:10.1016/s0002-9394(14)70276-48597271
- Albert D, Miller J, Azar D, Blodi B. Albert & Jakobiec’s Principles & Practice of Ophthalmology. 3rd ed. Philadelphia, PA: Saunders; 2008.
- Savar LM, Menghani RM, Chong KK, Chokron Garneau H, Goldberg RA. Eyebrow tissue expansion: an underappreciated entity in thyroid-associated orbitopathy. Arch Ophthalmol. 2012;130(12):1566–1569. doi:10.1001/archophthalmol.2012.254323229698
- Kim BJ, Kazim M. Prominent premalar and cheek swelling: a sign of thyroid-associated orbitopathy. Ophthalmic Plast Reconstr Surg. 2006;22(6):457–460. doi:10.1097/01.iop.0000244972.03781.c617117102
- Trobe JD, Glaser JS, Laflamme P. Dysthyroid optic neuropathy. clinical profile and rationale for management. Arch Ophthalmol. 1978;96(7):1199–1209. doi:10.1001/archopht.1978.03910060033007666628
- Hedges TR Jr, Scheie HG. Visual field defects in exophthalmos associated with thyroid disease. AMA Arch Ophthalmol. 1955;54(6):885–892.13268144
- Neigel JM, Rootman J, Belkin RI, et al. Dysthyroid optic neuropathy. The crowded orbital apex syndrome. Ophthalmology. 1988;95(11):1515–1521. doi:10.1016/s0161-6420(88)32978-73211460
- McKeag D, Lane C, Lazarus JH, et al. Clinical features of dysthyroid optic neuropathy: a European Group on Graves’ Orbitopathy (EUGOGO) survey. Br J Ophthalmol. 2007;91(4):455–458. doi:10.1136/bjo.2006.09460717035276
- Rundle FF, Wilson CW. Development and course of exophthalmos and ophthalmoplegia in Graves’ disease with special reference to the effect of thyroidectomy. Clin Sci. 1945;5(3–4):177–194.21011937
- Selva D, Chen C, King G. Late reactivation of thyroid orbitopathy. Clin Experiment Ophthalmol. 2004;32(1):46–50. doi:10.1046/j.1442-9071.2004.00756.x14746591
- Patel P, Khandji J, Kazim M. Recurrent thyroid eye disease. Ophthalmic Plast Reconstr Surg. 2015;31(6):445–448. doi:10.1097/IOP.000000000000037125621464
- Baldeschi L, Lupetti A, Vu P, Wakelkamp IM, Prummel MF, Wiersinga WM. Reactivation of Graves’ orbitopathy after rehabilitative orbital decompression. Ophthalmology. 2007;114(7):1395–1402. doi:10.1016/j.ophtha.2006.10.03617320178
- Shadpour JM, Menghani RM, Douglas RS, Goldberg RA, Tsirbas A. Reactivation of thyroid-associated orbitopathy after cataract surgery. Jpn J Ophthalmol. 2009;53(1):44–46. doi:10.1007/s10384-008-0607-x19184309
- Barrio-Barrio J, Sabater AL, Bonet-Farriol E, Velazquez-Villoria A, Galofre JC. Graves’ ophthalmopathy: VISA versus EUGOGO classification, assessment, and management. J Ophthalmol. 2015;2015:249125.26351570
- Nicosia L, Reverberi C, Agolli L, et al. Orbital radiotherapy plus concomitant steroids in moderate-to-severe Graves’ ophthalmopathy: good results after long-term follow-up. Int J Endocrinol Metab. 2019;17(1):e84427.30881470
- Bartalena L, Pinchera A, Marcocci C. Management of Graves’ ophthalmopathy: reality and perspectives. Endocr Rev. 2000;21(2):168–199. doi:10.1210/edrv.21.2.039310782363
- Tanda ML, Bartalena L. Efficacy and safety of orbital radiotherapy for Graves’ orbitopathy. J Clin Endocrinol Metab. 2012;97(11):3857–3865. doi:10.1210/jc.2012-275822962421
- Kahaly G, Beyer J. Immunosuppressant therapy of thyroid eye disease. Klin Wochenschr. 1988;66(21):1049–1059. doi:10.1007/bf017119173070148
- Gorman CA, Garrity JA, Fatourechi V, et al. A prospective, randomized, double-blind, placebo-controlled study of orbital radiotherapy for Graves’ ophthalmopathy. Ophthalmology. 2001;108(9):1523–1534. doi:10.1016/s0161-6420(01)00632-711535445
- Mourits MP, van Kempen-Harteveld ML, Garcia MB, Koppeschaar HP, Tick L, Terwee CB. Radiotherapy for Graves’ orbitopathy: randomised placebo-controlled study. Lancet (London, England). 2000;355(9214):1505–1509. doi:10.1016/S0140-6736(00)02165-6
- Prummel MF, Terwee CB, Gerding MN, et al. A randomized controlled trial of orbital radiotherapy versus sham irradiation in patients with mild Graves’ ophthalmopathy. J Clin Endocrinol Metab. 2004;89(1):15–20. doi:10.1210/jc.2003-03080914715820
- Bartalena L, Marcocci C, Chiovato L, et al. Orbital cobalt irradiation combined with systemic corticosteroids for Graves’ ophthalmopathy: comparison with systemic corticosteroids alone. J Clin Endocrinol Metab. 1983;56(6):1139–1144. doi:10.1210/jcem-56-6-11396341388
- Ng CM, Yuen HK, Choi KL, et al. Combined orbital irradiation and systemic steroids compared with systemic steroids alone in the management of moderate-to-severe Graves’ ophthalmopathy: a preliminary study. Hong Kong Med J. 2005;11(5):322–330.16219950
- Marcocci C, Bartalena L, Bogazzi F, Bruno-Bossio G, Lepri A, Pinchera A. Orbital radiotherapy combined with high dose systemic glucocorticoids for Graves’ ophthalmopathy is more effective than radiotherapy alone: results of a prospective randomized study. J Endocrinol Invest. 1991;14(10):853–860. doi:10.1007/BF033479431802923
- Prummel MF, Mourits MP, Blank L, Berghout A, Koornneef L, Wiersinga WM. Randomized double-blind trial of prednisone versus radiotherapy in Graves’ ophthalmopathy. Lancet (London, England). 1993;342(8877):949–954. doi:10.1016/0140-6736(93)92001-a
- Bradley EA, Gower EW, Bradley DJ, et al. Orbital radiation for Graves ophthalmopathy: a report by the American Academy of ophthalmology. Ophthalmology. 2008;115(2):398–409. doi:10.1016/j.ophtha.2007.10.02818082885
- Bartalena L, Krassas GE, Wiersinga W, et al. Efficacy and safety of three different cumulative doses of intravenous methylprednisolone for moderate to severe and active Graves’ orbitopathy. J Clin Endocrinol Metab. 2012;97(12):4454–4463. doi:10.1210/jc.2012-238923038682
- van Geest RJ, Sasim IV, Koppeschaar HP, et al. Methylprednisolone pulse therapy for patients with moderately severe Graves’ orbitopathy: a prospective, randomized, placebo-controlled study. Eur J Endocrinol. 2008;158(2):229–237. doi:10.1530/EJE-07-055818230831
- Ebner R, Devoto MH, Weil D, et al. Treatment of thyroid associated ophthalmopathy with periocular injections of triamcinolone. Br J Ophthalmol. 2004;88(11):1380–1386. doi:10.1136/bjo.2004.04619315489477
- Riedl M, Kuhn A, Kramer I, Kolbe E, Kahaly GJ. Prospective, systematically recorded mycophenolate safety data in Graves’ orbitopathy. J Endocrinol Invest. 2016;39(6):687–694. doi:10.1007/s40618-016-0441-926886940
- Ye X, Bo X, Hu X, et al. Efficacy and safety of mycophenolate mofetil in patients with active moderate-to-severe Graves’ orbitopathy. Clin Endocrinol (Oxf). 2017;86(2):247–255. doi:10.1111/cen.1317027484048
- Kahaly GJ, Riedl M, Konig J, et al. Mycophenolate plus methylprednisolone versus methylprednisolone alone in active, moderate-to-severe Graves’ orbitopathy (MINGO): a randomised, observer-masked, multicentre trial. Lancet Diabetes Endocrinol. 2018;6(4):287–298. doi:10.1016/S2213-8587(18)30020-229396246
- Prummel MF, Mourits MP, Berghout A, et al. Prednisone and cyclosporine in the treatment of severe Graves’ ophthalmopathy. N Engl J Med. 1989;321(20):1353–1359. doi:10.1056/NEJM1989111632120022519530
- Kahaly G, Schrezenmeir J, Krause U, et al. Ciclosporin and prednisone v. prednisone in treatment of Graves’ ophthalmopathy: a controlled, randomized and prospective study. Eur J Clin Invest. 1986;16(5):415–422. doi:10.1111/j.1365-2362.1986.tb01016.x3100309
- Antonelli A, Saracino A, Alberti B, et al. High-dose intravenous immunoglobulin treatment in Graves’ ophthalmopathy. Acta Endocrinol (Copenh). 1992;126(1):13–23. doi:10.1530/acta.0.12600131736548
- Kahaly G, Pitz S, Muller-Forell W, Hommel G. Randomized trial of intravenous immunoglobulins versus prednisolone in Graves’ ophthalmopathy. Clin Exp Immunol. 1996;106(2):197–202. doi:10.1046/j.1365-2249.1996.d01-854.x8918563
- Perros P, Weightman DR, Crombie AL, Kendall-Taylor P. Azathioprine in the treatment of thyroid-associated ophthalmopathy. Acta Endocrinol (Copenh). 1990;122(1):8–12. doi:10.1530/acta.0.12200082305608
- Kahaly G, Lieb W, Muller-Forell W, et al. Ciamexone in endocrine orbitopathy. A randomized double-blind, placebo-controlled study. Acta Endocrinol (Copenh). 1990;122(1):13–21. doi:10.1530/acta.0.12200132305603
- Dickinson AJ, Vaidya B, Miller M, et al. Double-blind, placebo-controlled trial of octreotide long-acting repeatable (LAR) in thyroid-associated ophthalmopathy. J Clin Endocrinol Metab. 2004;89(12):5910–5915. doi:10.1210/jc.2004-069715579735
- Wemeau JL, Caron P, Beckers A, et al. Octreotide (long-acting release formulation) treatment in patients with Graves’ orbitopathy: clinical results of a four-month, randomized, placebo-controlled, double-blind study. J Clin Endocrinol Metab. 2005;90(2):841–848. doi:10.1210/jc.2004-133415562016
- Chang TC, Liao SL. Slow-release lanreotide in Graves’ ophthalmopathy: a double-blind randomized, placebo-controlled clinical trial. J Endocrinol Invest. 2006;29(5):413–422. doi:10.1007/BF0334412416794364
- Stan MN, Garrity JA, Carranza Leon BG, Prabin T, Bradley EA, Bahn RS. Randomized controlled trial of rituximab in patients with Graves’ orbitopathy. J Clin Endocrinol Metab. 2015;100(2):432–441. doi:10.1210/jc.2014-257225343233
- Fichter N, Guthoff RF, Schittkowski MP. Orbital decompression in thyroid eye disease. ISRN Ophthalmol. 2012;2012:739236. doi:10.5402/2012/73923624558591
- Victores AJ, Takashima M. Thyroid eye disease: optic neuropathy and orbital decompression. Int Ophthalmol Clin. 2016;56(1):69–79. doi:10.1097/IIO.000000000000010126626933
- Rootman DB, Golan S, Pavlovich P, Rootman J. Postoperative changes in strabismus, ductions, exophthalmometry, and eyelid retraction after orbital decompression for thyroid orbitopathy. Ophthalmic Plast Reconstr Surg. 2017;33(4):289–293. doi:10.1097/IOP.000000000000075827487726
- Yeatts RP. Quality of life in patients with Graves ophthalmopathy. Trans Am Ophthalmol Soc. 2005;103:368–411.17057811
- Jackson JL. Nonsurgical management of diplopia after orbital decompression surgery. Am Orthopt J. 2012;62:29–33.23002472
- Frueh BR, Musch DC, Garber FW. Lid retraction and levator aponeurosis defects in Graves’ eye disease. Ophthalmic Surg. 1986;17(4):216–220.3754942
- Ivekovic R, Novak-Laus K, Tedeschi-Reiner E, Masnec-Paskvalin S, Saric D, Mandic Z. Full-thickeness anterior blepharotomy and transpalpebral fat decompression in Graves’ orbitopathy. Coll Antropol. 2005;29(Suppl 1):33–36.
- Dixon R. The surgical management of thyroid-related upper eyelid retraction. Ophthalmology. 1982;89(1):52–57. doi:10.1016/s0161-6420(82)34861-77070774
- Ribeiro SF, Shekhovtsova M, Duarte AF, Velasco Cruz AA. Graves lower eyelid retraction. Ophthalmic Plast Reconstr Surg. 2016;32(3):161–169. doi:10.1097/IOP.000000000000061326784547
- Gardner TA, Kennerdell JS, Buerger GF. Treatment of dysthyroid lower lid retraction with autogenous tarsus transplants. Ophthalmic Plast Reconstr Surg. 1992;8(1):26–31.1554649
- Oestreicher JH, Pang NK, Liao W. Treatment of lower eyelid retraction by retractor release and posterior lamellar grafting: an analysis of 659 eyelids in 400 patients. Ophthalmic Plast Reconstr Surg. 2008;24(3):207–212. doi:10.1097/IOP.0b013e318170684018520836
- Genere N, Stan MN. Current and emerging treatment strategies for Graves’ orbitopathy. Drugs. 2019;79(2):109–124. doi:10.1007/s40265-018-1045-930659423
- Planck T, Shahida B, Parikh H, et al. Smoking induces overexpression of immediate early genes in active Graves’ ophthalmopathy. Thyroid. 2014;24(10):1524–1532. doi:10.1089/thy.2014.015325135760
- Nita M, Grzybowski A. Smoking and eye pathologies. a systemic review. part ii. retina diseases, uveitis, optic neuropathies, thyroid-associated orbitopathy. Curr Pharm Des. 2017;23(4):639–654. doi:10.2174/138161282366617011109572328078992
- Marcocci C, Kahaly GJ, Krassas GE, et al. Selenium and the course of mild Graves’ orbitopathy. N Engl J Med. 2011;364(20):1920–1931. doi:10.1056/NEJMoa101298521591944
- Burch HB, Lahiri S, Bahn RS, Barnes S. Superoxide radical production stimulates retroocular fibroblast proliferation in Graves’ ophthalmopathy. Exp Eye Res. 1997;65(2):311–316. doi:10.1006/exer.1997.03539268599
- Bouzas EA, Karadimas P, Mastorakos G, Koutras DA. Antioxidant agents in the treatment of Graves’ ophthalmopathy. Am J Ophthalmol. 2000;129(5):618–622. doi:10.1016/s0002-9394(00)00359-710844053
- Smolen JS, Beaulieu A, Rubbert-Roth A, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet (London, England). 2008;371(9617):987–997. doi:10.1016/S0140-6736(08)60453-5
- ACTEMRA® (tocilizumab) [package insert] Injection, for Intravenous or Subcutaneous Use. Full Prescribing Information. South San Francisco, CA: Genentech, Inc.; 2019.
- Slowik M, Urbaniak-Kujda D, Bohdanowicz-Pawlak A, et al. CD8+CD28-lymphocytes in peripheral blood and serum concentrations of soluble interleukin 6 receptor are increased in patients with Graves’ orbitopathy and correlate with disease activity. Endocr Res. 2012;37(2):89–95. doi:10.3109/07435800.2011.63562222489922
- Russell DJ, Wagner LH, Seiff SR. Tocilizumab as a steroid sparing agent for the treatment of Graves’ orbitopathy. Am J Ophthalmol Case Rep. 2017;7:146–148. doi:10.1016/j.ajoc.2017.07.00129260102
- Perez-Moreiras JV, Gomez-Reino JJ, Maneiro JR, et al. Efficacy of tocilizumab in patients with moderate-to-severe corticosteroid-resistant Graves orbitopathy: a randomized clinical trial. Am J Ophthalmol. 2018;195:181–190. doi:10.1016/j.ajo.2018.07.03830081019
- Ayabe R, Rootman DB, Hwang CJ, Ben-Artzi A, Goldberg R. Adalimumab as steroid-sparing treatment of inflammatory-stage thyroid eye disease. Ophthalmic Plast Reconstr Surg. 2014;30(5):415–419. doi:10.1097/IOP.000000000000021124978425
- Durrani OM, Reuser TQ, Murray PI. Infliximab: a novel treatment for sight-threatening thyroid associated ophthalmopathy. Orbit. 2005;24(2):117–119. doi:10.1080/0167683059091256216191800
- Rajaii F, McCoy AN, Smith TJ. Cytokines are both villains and potential therapeutic targets in thyroid-associated ophthalmopathy: from bench to bedside. Expert Rev Ophthalmol. 2014;9(3):227–234. doi:10.1586/17469899.2014.91796025544859
- RITUXAN® (rituximab) [package insert] Injection, for Intravenous Use. Full Prescribing Information. South San Francisco, CA: Genentech, Inc.; 2019.
- Salvi M, Vannucchi G, Curro N, et al. Efficacy of B-cell targeted therapy with rituximab in patients with active moderate to severe Graves’ orbitopathy: a randomized controlled study. J Clin Endocrinol Metab. 2015;100(2):422–431. doi:10.1210/jc.2014-301425494967
- Smith TJ, Kahaly GJ, Ezra DG, et al. Teprotumumab for Thyroid-Associated ophthalmopathy. N Engl J Med. 2017;376(18):1748–1761. doi:10.1056/NEJMoa161494928467880
- Douglas RS, Sile S, Thompson EHZ, et al. Teprotumumab treatment effect on proptosis in patients with active thyroid eye disease: results from a phase 3, randomized, double-masked, placebo-controlled, parallel-group, multicenter study. Proceedings of the American Association of clinical endocrinologists. Endocr Pract. 2019;25(Supplement 1). doi:10.4158/EP-2018-0405
- Bartley GB. Rundle and his curve. Arch Ophthalmol. 2011;129(3):356–358. doi:10.1001/archophthalmol.2011.2921402995
- Zang S, Ponto KA,Kahaly GJ. Clinical review:Intravenous glucocorticoids for Graves' orbitopathy: efficacy and morbidity. J Clin Endocrinol Metab. 2011;96:320–332.21239515
- Marcocci C, Bartalena L, Tanda ML, Manetti L, Dell'Unto E, Rocchi R, Barbesino G, Mazzi B, Bartolomei MP, Lepri P, Cartei F, Nardi M, Pinchera A. Comparison of the effectiveness and tolerability of intravenous or oral glucocorticoids associated with orbital radiotherapy in the management of severe Graves' ophthalmopathy: results of a prospective, single-blind, randomized study. J Clin Endocrinol Metab. 2001;(86):3562–3567.11502779
