Abstract
Purpose:
Combined treatment with alendronate and alfacalcidol is more useful to increase bone mineral density (BMD) than alendronate or alfacalcidol alone. A retrospective study was conducted to investigate the 3-year outcome of combined treatment with alendronate and alfacalcidol in patients with severe bone loss (BMD ≤ 50% of the young adult mean) and osteoporotic fracture.
Methods:
Thirty-four patients (six men and 28 postmenopausal women) with primary or secondary osteoporosis who had been treated with alendronate and alfacalcidol for more than 3 years were analyzed. The lumbar spine or total hip BMD and bone turnover markers were monitored, and the incidence of osteoporotic fractures was assessed.
Results:
The urinary level of cross-linked N-terminal telopeptides of type I collagen and serum level of alkaline phosphatase significantly decreased (−42.5% at 3 months and −18.9% at 3 years), and the lumbar spine BMD, but not the total hip BMD, significantly increased (14.8% at 3 years), compared with the baseline values. However, the incidence of vertebral and nonvertebral fractures was 26.5% and 2.9%, respectively, suggesting a high incidence of vertebral fractures.
Conclusion:
The results of the present study suggest that combined treatment with alendronate and alfacalcidol may be useful to reduce bone turnover and increase the lumbar spine BMD in patients with severe bone loss and osteoporotic fracture. However, its efficacy against vertebral fractures appears not to be sufficient. Thus, anabolic agents such as teriparatide should be taken into consideration as first-line drugs in patients with severe osteoporosis.
Introduction
Alendronate (ALN) is widely used for the treatment of postmenopausal, glucocorticoid-induced, and male osteoporosis. The Fracture Intervention Trial demonstrated the efficacy of ALN against vertebral, nonvertebral, hip, and wrist fractures in postmenopausal women with osteoporosis.Citation1,Citation2 Furthermore, a recent systematic review analyzing 11 randomized controlled trials (RCTs) representing 12,068 women confirmed both clinically important and statistically significant reductions in vertebral, nonvertebral, hip, and wrist fractures for secondary prevention (gold-level evidence).Citation3 ALN has also been reported to reduce the incidence of vertebral fractures in patients treated with glucocorticoid or patients with male osteoporosis.Citation4,Citation5
The incidence of vertebral fractures is higher and that of hip fractures is lower among elderly Japanese people than among elderly Western people.Citation6 ALN is regarded as a first-line drug for the treatment of postmenopausal osteoporosis in Japan, because RCTs in postmenopausal Japanese women with osteoporosis revealed that ALN treatment (1–3 years) suppressed bone turnover, increased the bone mineral density (BMD), and reduced the incidence of vertebral fractures.Citation7–Citation10 RCTs in Japanese patients treated with glucocorticoid showed that ALN treatment (1–2 years) sustained or increased the lumbar spine BMD.Citation11–Citation13 Furthermore, a RCT in Japanese men with osteoporosis or osteopenia and clinical risk factors of fractures confirmed that ALN treatment (1 year) increased the total hip BMD.Citation14
In Japan, patients are diagnosed as having osteoporosis according to the Japanese diagnostic criteria.Citation15,Citation16 Namely, patients with a BMD < 70% of young adult mean (YAM) or 70%–80% of YAM along with a history of osteoporotic fractures were diagnosed as having osteoporosis. We have confirmed the long-term (4–7 years) efficacy and safety of ALN treatment in postmenopausal Japanese women or men with osteoporosis or osteopenia and clinical risk factors of fractures.Citation17–Citation19 In our clinical practice, however, patients with severe bone loss (BMD ≤ 50% of YAM) are not common, and the effects of ALN treatment on BMD, bone turnover markers, and fracture incidence remain to be established in such patients.
The AAC-Trial demonstrated that combined treatment with ALN and alfacalcidol (ALF) exhibited superiority in terms of BMD, overall fractures, rate of falls, and back pain over either ALN in combination with plain vitamin D or ALF alone in established postmenopausal or male osteoporosis.Citation20 An RCT conducted by Felsenberg et alCitation21 revealed that ALF increased the efficacy of ALN treatment in osteopenic/osteoporotic postmenopausal women on spine BMD, cortical and trabecular BMD of the tibia, and bending stiffness of the tibia. This line of evidence suggests the beneficial effect of combined treatment with ALN and ALF in patients with osteoporosis. A retrospective study was conducted to investigate the 3-year outcome of combined treatment with ALN and ALF in patients with severe bone loss (BMD ≤ 50% of YAM) and osteoporotic fracture. The incidences of osteoporotic fractures, including morphometric vertebral fractures and clinical vertebral and nonvertebral (hip, distal radius, and proximal humerus) fractures, were also assessed.
Subjects and methods
Subjects
Thirty-four Japanese patients who had been treated with ALN and ALF for more than 3 years were recruited at the outpatient clinic of Keiyu Orthopaedic Hospital (Gunma, Japan) during the 3-month period between January 4 and April 4, 2011. The inclusion criteria were primary or secondary osteoporosis, patients with severe bone loss (BMD ≤ 50% of YAM) and osteoporotic vertebral, hip, distal radius, or proximal humerus fracture at the start of treatment. The exclusion criteria were histories of reflux esophagitis, gastric or duodenal ulcer, and renal failure.
The assessment prior to combined treatment with ALN and ALF included a medical history, physical examination, plain X-rays of the thoracic and lumbar spine, lumbar spine or total hip BMD measurement, and blood and urinary biochemical tests including serum calcium, phosphorus, and alkaline phosphatase (ALP), and urinary cross-linked N-terminal telopeptides of type I collagen (NTX). The serum calcium, phosphorus, and ALP levels were measured using the standard laboratory technique, and the urinary NTX levels were measured using enzyme-linked immunosorbent assay. The lumbar spine or total hip BMD was measured using dual-energy X-ray absorptiometry (DXA) as described below.
The patients had been treated with ALN (5 mg daily or 35 mg weekly) plus ALF (1 μg daily). The doses indicated in the parentheses above are the doses used in Japan for the treatment of postmenopausal women with osteoporosis and have been recognized as being safe and effective.Citation7–Citation10,Citation22 Daily ALN was available throughout the study period, but weekly ALN only became available after October 2006. All the patients had been treated with daily ALN and then switched to weekly ALN just after October 2006. The effects of daily and weekly ALN on the BMD and bone turnover markers as well as the incidence of side effects were reported to be similar in postmenopausal Japanese women with osteoporosis.Citation10
The urinary levels of NTX were measured at 3 months after the start of treatment, based on the results of our previous study.Citation23 A urinary NTX measurement performed 3 months after the start of ALN treatment provides important information and is sufficient to monitor the effects of treatment for osteoporosis.Citation23 The serum levels of calcium, phosphorus, and ALP and the lumbar spine or total hip BMD were measured every 6 months after the start of treatment. The outcome of combined treatment with ALN and ALF for 3 years was evaluated. The present study was approved by the Ethics Committee of Keiyu Orthopaedic Hospital.
Assessment of morphometric vertebral fractures
Plain lateral X-ray films of the thoracic and lumbar spine were obtained at baseline to detect evidence of morphometric vertebral fractures. According to the Japanese criteria, a vertebral fracture was defined according to the vertebral height on lateral X-ray films.Citation15,Citation16 Briefly, the vertebral height was measured at the anterior (A), central (C), and posterior (P) parts of the vertebral body, and the presence of a vertebral fracture was confirmed when (1) a reduction in the vertebral height of more than 20% (A, C, and P) compared with the height of the adjacent vertebrae was observed, (2) the C/A or C/P was less than 0.8, or (3) the A/P was less than 0.75. The assessment for vertebral fractures was performed at the T4–L4 level.
Assessment of clinical vertebral and nonvertebral fractures
Low-traumatic osteoporotic clinical fractures were assessed. Clinical vertebral fractures were determined based on clinical symptoms and radiographs or magnetic resonance images of the lumbar and thoracic spine. Nonvertebral fractures in terms of osteoporotic fractures at the distal radius, proximal humerus, and hip, were determined based on clinical symptoms and radiographs of the wrist, shoulder, and hip joints, respectively.
Measurement of lumbar spine or total hip BMD
The BMD of the lumbar spine or total hip in the antero-posterior view was measured using DXA with a Hologic QDR 1500W apparatus (Hologic Inc, Bedford, MA). The coefficient of variation of five measurements with repositioning within 72 hours each time was less than 1.2% in three persons. Primarily, the lumbar spine (L1–L4) was chosen as a skeletal site for BMD measurement. However, the first lumbar vertebra (L1) was omitted for patients whose lumbar spine radiographs showed callus formation after L1 vertebral fracture. In this case, the lumbar spine (L2–L4) BMD was adopted. The total hip BMD was measured for patients whose lumbar spine radiographs showed severe spondylosis, severe scoliosis, callus formation after L2, L3, or L4 vertebral fracture, or severe aortic calcification. The lumbar spine BMD was measured for 30 patients, and the total hip BMD for four patients (two men and two postmenopausal women).
Statistical analysis
Data were expressed as the mean ± standard deviation. A one-way analysis of variance (ANOVA) with repeated measurements was used to determine the significance of longitudinal changes in the BMD and biochemical markers. A two-way ANOVA with repeated measurements was used to compare longitudinal changes in the BMD and biochemical markers between men and postmenopausal women. A Fisher’s exact test was used to compare the incidence of fractures between men and postmenopausal women. All the statistical analyses were performed using the Stat View-J5.0 (Abacus Concepts Inc, Berkeley, CA) program on a Windows® computer. A significance level of P < 0.05 was used for all the comparisons.
Results
Characteristics of the study subjects at the start of treatment
Six patients were men and 28 patients were postmenopausal women. Twelve patients had diseases that might affect bone metabolism: glucocorticoid use due to asthma or subacute thyroiditis (n = 4), hyperthyroidism (n = 2), gastrectomy (n = 2), breast cancer-induced bone loss due to aromatase inhibitors (n = 1), warfarin used after valve transplantation of the heart (n = 1), osteogenesis imperfecta (n = 1), and Parkinson’s disease (n = 1). shows the characteristics of the study subjects at the start of the treatment. The mean age of all the subjects was 67.4 years (range: 41–80 years). The mean percentage of the YAM in the lumbar spine and total hip BMD was 45.8% and 43.8%, respectively. The mean levels of serum calcium, phosphorus, and ALP were within the normal ranges (8.4–10.2 mg/dL, 2.5–4.5 mg/dL, and 100–340 IU/L, respectively). The mean level of urinary NTX was higher than the normal range for Japanese women (9.3–54.3 nmol BCE/mmol Cr),Citation24 indicating a high turnover characteristic of osteoporosis. All patients had osteoporotic vertebral or nonvertebral (hip, distal radius, and proximal humerus) fractures. The number of women with prevalent vertebral fractures was 30 (88.2%), and the number of patients with a history of nonvertebral fractures was six (17.6%).
Table 1 Characteristics of study subjects at the start of treatment
Changes in lumbar spine and total hip BMD
shows that the lumbar spine BMD continued to increase for 3 years. A one-way ANOVA with repeated measurements showed significant longitudinal changes in the lumbar spine BMD (P < 0.0001). The mean rates of change in the lumbar spine BMD after 1, 2, and 3 years of treatment were +11.3%, +12.4%, and +14.8%, respectively. However, total hip BMD did not change significantly (P = 0.8706). The mean rates of change in the total hip BMD after 1, 2, and 3 years of treatment were −0.5%, +3.2%, and +6.4%, respectively.
Figure 1 Changes in lumbar spine and total hip BMD.
Abbreviations: ANOVA, analysis of variance; BMD, bone mineral density.
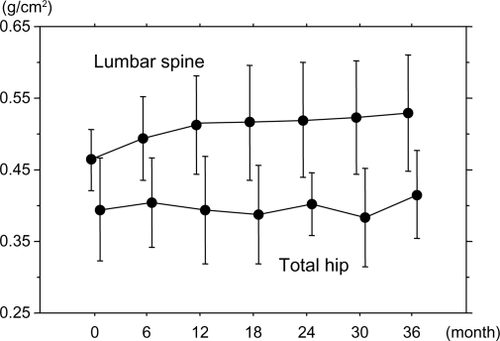
A two-way ANOVA with repeated measurements showed that longitudinal changes in the BMD did not differ significantly between men and postmenopausal women (P = 0.8423 for the lumbar spine and P = 0.1971 for the total hip).
Changes in biochemical markers
shows the changes in the biochemical markers. The mean urinary NTX level decreased to the normal range for Japanese women (9.3–54.3 nmol BCE/mmol Cr)Citation24 after 3 months of treatment, and the mean serum ALP level decreased but remained within the normal range (135–310 IU/L) during the 3-year period. A one-way ANOVA with repeated measurements showed significant longitudinal changes in the serum ALP and urinary NTX levels (both P < 0.0001). The mean rates of change in the urinary NTX level after 3 months of treatment were −42.5%. The mean rates of change in the serum ALP level after 1, 2, and 3 years of treatment were −26.1%, −20.5%, and −18.9%, respectively. However, the serum calcium and phosphorus levels did not change significantly (P = 0.0760 and 0.8799, respectively).
Figure 2 Changes in biochemical markers.
Abbreviations: ANOVA, analysis of variance; ALP, alkaline phosphatase; NTX, cross linked N-terminal telopeptides of type I collagen; BCE, bone collagen equivalent; Cr, creatinine.
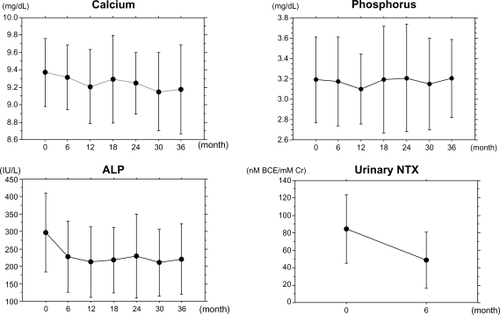
A two-way ANOVA with repeated measurements showed that longitudinal changes in the serum calcium, phosphorus, and ALP and urinary NTX levels did not differ significantly between men and postmenopausal women (P = 0.1832 for calcium, P = 0.9447 for phosphorus, P = 0.3251 for ALP, and P = 0.4121 for urinary NTX).
Incidence of osteoporotic fractures
shows that during the 3-year treatment period, nine patients (26.5%) experienced vertebral fractures (morphometric fractures in seven patients [20.6%] and clinical fractures in two patients [5.9%]). One patient (2.9%) experienced nonvertebral fracture (proximal humerus fracture).
Table 2 Incidence of vertebral and nonvertebral fractures
A Fisher’s exact test showed that the incidence of fractures did not differ significantly between men and postmenopausal women (16.7% for men and 32.1% for postmenopausal women, P = 0.4502).
Adverse events
No serious adverse events, including osteonecrosis of the jaw, femoral diaphysis atypical fractures, and atrial fibrillation,Citation25–Citation35 were observed.
Discussion
Combined treatment with ALN and ALF increased the lumbar spine BMD (+11.3%, +12.4%, and +14.8% at 1, 2, and 3 years, respectively) subsequent to reductions in the urinary NTX level (−42.5% at 3 months) and the serum ALP level (−26.1%, −20.5%, and −18.9% at 1, 2, and 3 years, respectively). RCTs have shown that ALN treatment (5 mg daily or 35 mg weekly) decreases the urinary NTX (−45% at 3 months) and serum ALP (about −20% at 3 years) levels and increases the lumbar spine BMD (+9.2% at 3 years) in postmenopausal Japanese women with osteoporosis.Citation8,Citation10 Our previous two studies also showed that ALN treatment in postmenopausal women with osteoporosis and men with osteoporosis increased the lumbar spine BMD (+5.8% at 1 year and +9.4% at 3 years, respectively) subsequent to reductions in the urinary NTX level (−39.2% and −40.0%, respectively, at 3 months) and the serum ALP level (−17.8% at 1 year and −21.2% at 3 years, respectively).Citation36,Citation37 On the other hand, an RCT showed that ALF mildly increased the lumbar spine BMD (1.35% at 1 year) without significantly influencing bone turnover markers in postmenopausal women with osteoporosis.Citation9 The increase in the lumbar spine BMD in the present study appears to be greater than those in the previous studies regarding ALN treatment, despite the similar reductions in bone turnover markers, suggesting the additive effect of ALN and ALF on the lumbar spine BMD.
The results of the Fracture Intervention Trial revealed that ALN effectively reduced the fracture risk in postmenopausal women with vertebral fractures and low BMD, including those women at the highest risk because of advanced age or severe osteoporosis.Citation38 Although the relative risk for vertebral fracture was compared between age <75 years and ≥75 years, femoral neck BMD < 0.59 g/cm2 and ≥0.59 g/cm2, one existing vertebral fracture and ≥2 existing vertebral fractures, or history of postmenopausal fracture and no history of postmenopausal fracture in this analysis, the incidence of vertebral fractures after ALN treatment was not compared among groups.
The incidence of vertebral fractures was 26.5% (morphometric fracture 20.6% and clinical fracture 5.9%) in patients (mean age: 67.8 years) with severe bone loss (100% with a history of osteoporotic fracture). Our previous study revealed that the incidence of vertebral fractures after 3-year ALN treatment was 13.3% (morphometric fracture 9.6% and clinical fracture 3.7%) in postmenopausal women (mean age: 67.4%) with osteoporosis (37% with a history of osteoporotic fracture).Citation36 Thus, despite the greater increase in the lumbar spine BMD, the incidence of vertebral fractures was considered to be higher in patients with severe bone loss and osteoporotic fracture than those with postmenopausal osteoporosis. This result suggests the importance of BMD and preexisting osteoporotic fractures at baseline in the prevention of vertebral fractures by bisphosphonate treatment. Shiraki et alCitation39 reported that traditional risk factors such as older age, low BMD, and preexisting osteoporotic fractures were recognized as risks for incident fractures in postmenopausal osteoporotic women treated with bisphosphonates, supporting our suggestion. Thus, anabolic agents, such as teriparatide, which are able to vigorously increase lumbar spine BMDCitation40 should be considered as the first-line drugs in the treatment of severe osteoporosis.
The total hip BMD did not change significantly from the baseline values in four patients (two men and two postmenopausal women). Our previous study showed that 1-year treatment with ALN increased the total hip BMD by 2.3% from the baseline values in men with osteoporosis or osteopenia and clinical risk factors of fractures.Citation14 However, the effect of ALN on total hip BMD has been less established in postmenopausal Japanese women with osteoporosis. In the present study, the mean rates of change in total hip BMD after 1, 2, and 3 years of treatment were −0.5%, +3.2%, and +6.4%, respectively, which was not statistically significant. This result may be attributable to the small sample size. Further studies are needed to establish the effect of ALN treatment with or without ALF on the total hip BMD in men and postmenopausal women with osteoporosis in Japan.
A couple of German studies showed that combined treatment with ALN and ALF improved physical function (chair rising time and time up and go) and back pain in elderly patients with a high risk of falls and fractures.Citation41,Citation42 Although we did not assess the risk of falls and back pain, it would be of interest to investigate the effect of combined treatment with ALN and ALF on fall incidence and subsequent fractures in frail patients with severe osteoporosis.
An epidemiological study has indicated that the incidence of vertebral fractures is higher and that of hip fractures is lower among elderly Japanese people than among elderly Western people.Citation6 In the present study, no patients suffered from distal radius or hip fractures, although the incidence of vertebral fractures was considered to be high. Vitamin D supplementation is linked to a decreased risk of falls in ambulatory and institutionalized elderly patients, because muscle tissue has highly specific nuclear receptors for 1,25-dihydroxyvitamin D.Citation43 Bischoff-Ferrari et al.Citation44,Citation45 have shown that vitamin D supplementation appears to reduce the risk of falls and hip and any non-vertebral fractures in ambulatory or institutionalized elderly persons. Thus, ALF might have played a significant role in reducing the risk of falls and subsequent fractures in the present study.
There is a notable limitation. Because the present study was a retrospective study with a small sample size, the results might be biased. RCTs are needed to confirm the effect of combined treatment with ALN and ALF on severe osteoporosis.
In conclusion, the present retrospective study showed that combined treatment with ALN and ALF suppressed bone turnover and increased lumbar spine BMD, compared with baseline values, over the course of a 3-year treatment period without causing any severe adverse events in patients with severe bone loss and osteoporotic fracture. However, its efficacy against vertebral fractures may not be sufficient. Thus, anabolic agents such as teriparatide should be taken into consideration as first-line drugs in patients with severe osteoporosis.
Disclosure
The authors report no funding sources or conflicts of interest in this work.
References
- BlackDMCummingsSRKarpfDBRandomised trial of effect of alendronate on risk of fracture in women with existing vertebral fracturesLancet1996348153515418950879
- CummingsSRBlackDMThompsonDEEffect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention TrialJAMA1998280207720829875874
- WellsGACranneyAPetersonJAlendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal womenCochrane Database Syst Rev2008231CD00115518253985
- AdachiJDSaagKGDelmasPDTwo-year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids: a randomized, double-blind, placebo-controlled extension trialArthritis Rheum20014420221111212161
- RingeJDDorstAFaberHAlendronate treatment of established primary osteoporosis in men: 3-year results of a prospective, comparative, two-arm studyRheumatol Int20042411011313680141
- FujiwaraSKasagiFMasunariNFracture prediction from bone mineral density in Japanese men and womenJ Bone Miner Res2003181547155312929946
- KushidaKShirakiMNakamuraTThe efficacy of alendronate in reducing the risk of vertebral fracture in Japanese patients with osteoporosis: a randomized, double-blind, active-controlled, double-dummy trialCurr Ther Res Clin Exp200263606620
- KushidaKShirakiMNakamuraTAlendronate reduced vertebral fracture risk in postmenopausal Japanese women with osteoporosis: a 3-year follow-up studyJ Bone Miner Metab20042246246815316867
- ShirakiMKushidaKFukunagaMA double-masked multicenter comparative study between alendronate and alfacalcidol in Japanese patients with osteoporosisOsteoporos Int19991018319210525709
- UchidaSTaniguchiTShimizuTTherapeutic effects of alendronate 35 mg once weekly and 5 mg once daily in Japanese patients with osteoporosis: a double-blind, randomized studyJ Bone Miner Metab20052338238816133688
- KitazakiSMitsuyamaKMasudaJClinical trial: comparison of alendronate and alfacalcidol in glucocorticoid-associated osteoporosis in patients with ulcerative colitisAliment Pharmacol Ther20092942443019035979
- OkadaYNawataMNakayamadaSAlendronate protects premenopausal women from bone loss and fracture associated with high-dose glucocorticoid therapyJ Rheumatol2008352249225419031508
- TakedaSKaneokaHSaitoTEffect of alendronate on glucocorticoid-induced osteoporosis in Japanese women with systemic autoimmune diseases: versus alfacalcidolMod Rheumatol20081827127618427724
- IwamotoJSatoYUzawaMComparison of the effects of alendronate and alfacalcidol on hip bone mineral density and bone turnover in Japanese men having osteoporosis or osteopenia with clinical risk factors for fracturesYonsei Med J20095047448119718394
- OrimoHSugiokaYFukunagaMDiagnostic criteria of primary osteoporosisJ Bone Miner Metab199816139150
- OrimoHHayashiYFukunagaMfor the Osteoporosis Diagnostic Criteria Review Committee, Japanese Society for Bone and Mineral ResearchDiagnostic criteria for primary osteoporosis: year 2000 revisionJ Bone Miner Metab20011933133711685647
- IwamotoJMiyataASatoYFive-year alendronate treatment outcome in older postmenopausal Japanese women with osteoporosis or osteopenia and clinical risk factors for fracturesTher Clin Risk Manag2009577377919851524
- IwamotoJSatoYUzawaMSeven years’ experience with alendronate in postmenopausal Japanese women with osteoporosisTher Clin Risk Manag2010620120620463781
- IwamotoJSatoYUzawaMExperience with alendronate treatment for four years among Japanese men with osteoporosis or osteopenia and clinical risk factors for fracturesTher Clin Risk Manag2010659360021206758
- RingeJDFarahmandPSchachtESuperiority of a combined treatment of alendronate and alfacalcidol compared to the combination of alendronate and plain vitamin d or alfacalcidol alone in established postmenopausal or male osteoporosis (AAC-Trial)Rheumatol Int20072742543417216477
- FelsenbergDBockOBörstHAdditive impact of alfacalcidol on bone mineral density and bone strength in alendronate treated postmenopausal women with reduced bone massJ Musculoskelet Neuronal Interact201111344521364273
- OrimoHShirakiMHayashiYEffects of 1 alpha-hydroxyvitamin D3 on lumbar bone mineral density and vertebral fractures in patients with postmenopausal osteoporosisCalcif Tissue Int1994543703768062152
- IwamotoJTakedaTSatoYEarly changes in urinary cross-linked N-terminal telopeptides of type I collagen level correlate with one-year response of lumbar bone mineral density to alendronate in Japanese postmenopausal women with osteoporosisJ Bone Miner Metab20052323824215838627
- NishizawaYNakamuraTOhtaHfor the Committee on the Guidelines for the Use of Biochemical Markers of Bone Turnover in Osteoporosis Japan Osteoporosis SocietyGuidelines for the use of biochemical markers of bone turnover in osteoporosis (2004)J Bone Miner Metab2005239710415750686
- RuggieroSLDodsonTBAssaelLAfor the American Association of Oral and Maxillofacial SurgeonsAmerican Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws – 2009 updateJ Oral Maxillofac Surg20096721219371809
- LoJCO’RyanFSGordonNPfor the Predicting Risk of Osteonecrosis of the Jaw with Oral Bisphosphonate Exposure (PROBE) InvestigatorsPrevalence of osteonecrosis of the jaw in patients with oral bisphosphonate exposureJ Oral Maxillofac Surg20106824325319772941
- LenartBALorichDGLaneJMAtypical fractures of the femoral diaphysis in postmenopausal women taking alendronateN Engl J Med20083581304130618354114
- RizzoliRAkessonKBouxseinMSubtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group ReportOsteoporos Int20112237339021085935
- GiustiAHamdyNAPapapoulosSEAtypical fractures of the femur and bisphosphonate therapy: a systematic review of case/case series studiesBone20104716918020493982
- GiustiAHamdyNADekkersOMAtypical fractures and bisphosphonate therapy: a cohort study of patients with femoral fracture with radiographic adjudication of fracture site and featuresBone201148596697121195812
- ShaneEBurrDEbelingPRfor the American Society for Bone and Mineral ResearchAtypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral ResearchJ Bone Miner Res2010252267229420842676
- PazianasMCompstonJHuangCLAtrial fibrillation and bisphosphonate therapyJ Bone Miner Res20102521020091928
- HeckbertSRLiGCummingsSRUse of alendronate and risk of incident atrial fibrillation in womenArch Intern Med200816882683118443257
- PazianasMCooperCEbetinoFHLong-term treatment with bisphosphonates and their safety in postmenopausal osteoporosisTher Clin Risk Manag2010632534320668715
- VestergaardPSchwartzKPinholtEMRisk of atrial fibrillation associated with use of bisphosphonates and other drugs against osteoporosis: a cohort studyCalcif Tissue Int20108633534220309678
- IwamotoJTakedaTSatoYComparison of the effect of alendronate on lumbar bone mineral density and bone turnover in men and postmenopausal women with osteoporosisClin Rheumatol20072616116716565894
- IwamotoJSatoYUzawaMThree-year experience with alendronate treatment in postmenopausal osteoporotic Japanese women with or without type 2 diabetesDiabetes Res Clin Practice Epub 2011 Apr 25.
- EnsrudKEBlackDMPalermoLTreatment with alendronate prevents fractures in women at highest risk: results from the Fracture Intervention TrialArch Intern Med1997157261726249531231
- ShirakiMYamazakiYShirakiYHigh level of serum undercarboxylated osteocalcin in patients with incident fractures during bisphosphonate treatmentJ Bone Miner Metab20102857858420221651
- MiyauchiAMatsumotoTSugimotoTEffects of teriparatide on bone mineral density and bone turnover markers in Japanese subjects with osteoporosis at high risk of fracture in a 24-month clinical study: 12-month, randomized, placebo-controlled, double-blind and 12-month open-label phasesBone20104749350220580870
- RingeJDSchachtEDukasLPotency of a combined alfacalcidol-alendronate therapy to reduce the risk of falls and fractures in elderly patients with glucocorticoid-induced osteoporosisArzneimittelforschung20116110411121428245
- SchachtERingeJDRisk reduction of falls and fractures, reduction of back pain and safety in elderly high risk patients receiving combined therapy with alfacalcidol and alendronate: a prospective studyArzneimittelforschung201161405421355445
- BischoffHABorchersMGuadtFIn situ detection of 1,25-dihydroxyvitamin D3 receptor in human skeletal muscle tissueHistochem J200133192411352397
- Bischoff-FerrariHADawson-HughesBWillettWCEffect of vitamin D on falls: a meta-analysisJAMA20042911999200615113819
- Bischoff-FerrariHAWillettWCWongJBFracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trialsJAMA20052932257226415886381