Abstract
Background:
The purpose of this study was to compare electrophysiologically guided and traditional nerve stimulator analgesia femoral nerve block after total knee arthroplasty.
Methods:
Patients scheduled for unilateral total knee arthroplasty were randomized to electrophysiologically guided or traditional nerve stimulator analgesia by pre-emptive single injection femoral nerve block with corresponding assistance. We assessed pain scores using a visual analog scale (VAS, 0 = no pain, 100 = the worst pain) and the volumes of morphine consumed at 4, 24, 48, and 72 hours after total knee arthroplasty.
Results:
Of the 60 patients enrolled, eight withdrew from the study. The remaining 52 patients were randomized to the electrophysiologically guided group (n = 27) or traditional nerve stimulator analgesia (n = 25) group. Four hours after total knee arthroplasty, VAS scores were significantly lower in the electrophysiologically guided group than in the traditional nerve stimulator group at rest (4.8 ± 1.4 versus 5.9 ± 0.8, P < 0.01) and while moving (6.2 ± 1.1 versus 6.9 ± 0.9, P < 0.01). The total volumes of morphine injected at 24, 48, and 72 hours were significantly decreased in the electrophysiologically guided group (P < 0.05 each). Variable × time interaction of VAS was significant in the electrophysiologically guided group (P < 0.05), with each VAS score at 24, 48, and 72 hours being significantly lower than the baseline score (P < 0.05). VAS scores at every time point were significantly lower in the electrophysiologically group guided than in the traditional nerve stimulator group (P < 0.05).
Conclusion:
Electrophysiologically guided single injection femoral nerve block may provide better postoperative analgesia and a greater reduction in the demand for pain killers than femoral nerve block using traditional nerve stimulator analgesia.
Introduction
Poorly controlled pain after total knee arthroplasty may hinder early rehabilitation. Although continuous femoral nerve block is considered the ideal method of analgesia after total knee arthroplasty,Citation1 it may have clinical disadvantages, including an increased risk of infection and reduced ambulation. The incidence of serious falls related to continuous femoral nerve block is increased within the four days postoperatively.Citation2,Citation3 Single injection femoral nerve block is easier and less costly to perform than continuous femoral nerve block. A recent meta-analysis showed that although both single injection and continuous femoral nerve block were superior to patient-controlled analgesia, the two former methods require further comparison.Citation4
Given that the degree of neural blockage is proportional to the amount of local anesthetic, the anesthetic should be injected as close to the nerve as possible. Although femoral nerve block has been performed using a traditional nerve stimulator, the patellar motor response is not sufficiently reliable to quantify the degree of stimulation, except by phonomyography.Citation5 Electrophysiologically guided suprascapular nerve block has been shown to be more effective than traditional suprascapular nerve block in relieving shoulder pain in patients with adhesive capsulitis.Citation6
We hypothesized that electrophysiologic guidance would more accurately localize the target nerve than would a traditional nerve stimulator. We therefore compared the effects on postoperative analgesia of electrophysiologically guided femoral nerve block with those of femoral nerve block using a traditional nerve stimulator. To our knowledge, this is the first prospective, double-blinded, randomized, positive-controlled clinical trial evaluating electrophysiologic guidance for femoral nerve block in total knee arthroplasty.
Materials and methods
This prospective, randomized, double-blinded, parallel-group, positive-controlled clinical trial was performed in an inpatient clinic in the department of orthopedic surgery at a general hospital in Asia from July 2006 to October 2008.
Patients scheduled for elective classic unilateral total knee arthroplasty were included. We excluded patients weighing < 50 kg or >100 kg, those with a coagulation or neurologic disease, those who were hypersensitive to local anesthetics, those not classified as American Society of Anesthesiologists (ASA) physical status I–III, and those unable to understand the pain scales or use patient-controlled analgesia. Prior to total knee arthroplasty, patients were randomized 1:1 to the electrophysiologically guided or traditional nerve stimulator groups using a random assignment generator with sequentially numbered containers (Wichmann-Hill random number generator, randomization@com). The protocol was approved by our institutional review board (approval number UUH-06-11), and all patients provided their written informed consent.
Shortly before the surgery, each patient was aseptically draped, with subsequent topical anesthesia using 1 mL of 1% lidocaine. Patients were injected with a single dose of ropivacaine for femoral nerve block according to the landmarks of Winnie et al.Citation7 No sedative was administered.
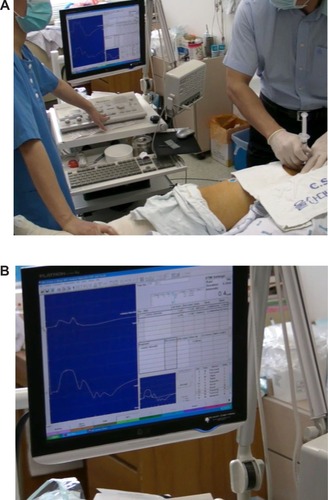
The medical equipment (Medelec Synergy, Vickers Medical, Surrey, UK) used comprised three parts, the first being to stimulate the nerve, the second being to take up the electrical signal, and the third being to display the signal on the screen as a graph.
Patients in the electrophysiologically guided group were placed in the supine position, and the femoral artery was palpated below the inguinal ligament. A 7 mm, 22 gauge, Teflon-coated, electrically conductive, double-lumen, beveled cannula (Myojet disposable hypodermic needle electrode, TECA Accessories, New York, NY, USA) was inserted just lateral to the femoral artery and into the iliopsoas muscle. This cannula enabled both femoral nerve stimulation and injection of local anesthetic. A recording electrode was placed on the skin above the motor point of the vastus medialis showing the maximum electrical signal of muscle contraction. The femoral nerve was located by nerve stimulation at a frequency of 1 Hz, a duration of 0.2 msec, and an intensity of 5 mA, while monitoring the change in amplitude of the electrical signal. Once the electrical signal was found, the stimulation intensity was reduced stepwise by moving the cannula back and forth and side to side until the highest amplitude could be induced by a stimulation intensity < 0.5 mA. After the aspiration test showed no evidence of blood, 10 mL of 0.375% ropivacaine was injected. To confirm the correct level of analgesia, we monitored the disappearance of the electrical signal by stimulation with an intensity of 5 mA shortly after injection and by assessment of the integumentary sensation in the dermatome of the femoral nerve by pinprick tests ().
Patients in the traditional nerve stimulator group received a single injection femoral nerve block as described for the electrophysiologically guided group, using the same medical equipment, nerve stimulation of equal parameters, and downward adjustment of intensity below 0.5 mA, while monitoring brisk cephalic patellar tilting, a marker for contractions of the quadriceps femoris. Loss of sensation was determined upon completion of femoral nerve block.
General anesthesia was induced by injection of alfentanil 15 μg/kg, propofol 2–2.5 mg/kg, and rocuronium 0.6–0.8 mg/kg, maintained with 40%–60% oxygen-nitrous oxide and 1%–2% sevoflurane, and reversed with neostigmine 40 μg/kg and glycopyrrolate 7 μg/kg. Alfentanil 0.25 mg was injected intravenously if mean arterial pressure or heart rate was >125% of preoperative values.
Supplemental postoperative analgesia after total knee replacement was standardized.Citation8 The morphine dose was half that recorded for Caucasians, due to the smaller body weight and volume of Asian. Pain was controlled by intravenous patient-controlled analgesia morphine in 1 mg increments, with a 5-minute lockout time up to a total limit of 4 mg.
Pain while at rest and moving was assessed using a visual analog scale (VAS, 0 = no pain, 100 = the worst pain) and postoperative pain score (0 = no pain; 1 = moderate pain only while moving; 2 = moderate pain while resting or severe pain while moving; 3 = continuous severe pain)Citation9 at hours 4, 24, 48, and 72 after the end of the surgery. If the VAS pain score exceeded 4 after 4 mg of morphine, 1 mg increments were allowed until the score was reduced to 4. Each patient was administered two tablets of acetaminophen 250 mg plus codeine 10 mg one hour after surgery, followed by one tablet three times per day. The number of intravenous patient-controlled analgesia doses and the total amount of morphine every 3 days were recorded. Nausea and vomiting were recorded only if an antiemetic drug was used. Major side effects of ropivacaine, including convulsions and hypotension, were recorded,Citation10 as were urinary retention needing catheterization or prolonged muscle paralysis.
Patients in both groups started an identical physiotherapy regimen the day after surgery. All staff members, including the surgical teams, nurses, assessors, and physiotherapists, were blinded to patient assignment.
Statistical analysis
All statistical analyses were performed using SPSS version 19.0 for Windows (SPSS Inc, Chicago, IL, USA). An alpha level < 0.05 was considered to be statistically significant. The power value was determined to be 80%, with an assumed dropout rate of 20%. A preliminary study found a standardized difference of 0.8. Using Lehr’s formula, we calculated that 60 patients would be required. Demographic factors were compared using the Chi-square and two-sample Student’s t-tests. Variable × time and variable × group interactions of the pain scales were evaluated by repeated-measures analysis of variance. Total amounts of morphine consumed and pain scores were evaluated by two-sample paired t-tests or Student’s t-tests.
Results
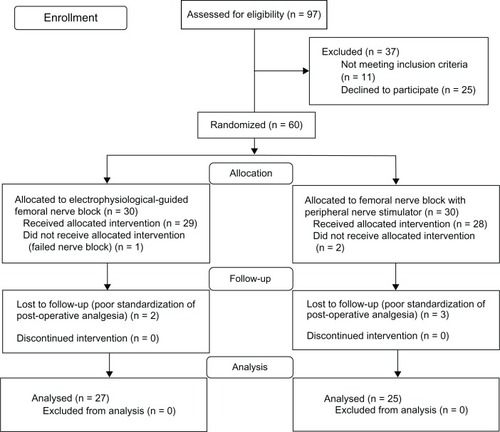
Of the 97 patients screened, 37 were excluded. Sixty patients were recruited from July 2006 to September 2008, with 30 assigned to each group. Three patients in the electrophysiologically guided group were lost to follow-up, one due to no femoral nerve block and two due to poor standardization of postoperative analgesia, as were five patients in the traditional nerve stimulator group, two due to no femoral nerve block and three due to poor standardization of postoperative analgesia. Therefore, our per-protocol analysis included 27 patients in the electrophysiologically guided group and 25 in the traditional nerve stimulator group ().
Pain scores and morphine consumption were assessed in the recovery room and the general ward at 4, 24, 48, and 72 hours after the end of surgery. There were no failures of femoral nerve block, except for one patient with severe anxiety.
The two groups were well matched in terms of demographics and preoperative pain scores (P = 0.23–0.97, ). There was no regulation of the gender ratio recruited.
Table 1 Demographic data
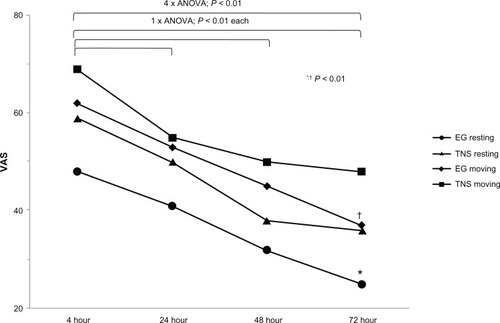
All patients in both groups showed improvement in pain scores 4 hours after total knee arthroplasty (P < 0.01). Postoperative VAS score was significantly lower in the electrophysiologically guided group than in the traditional nerve stimulator group at 4 hours, both while at rest (48 ± 1.4 versus 59 ± 0.8, P < 0.01) and while moving (62 ± 1.1 versus 69 ± 0.9, P < 0.01, ). However, postoperative pain scores at 4 hours did not differ significantly.
Table 2 VAS at postoperative hours 4, 24, 48, and 72
Variable × group interactions of VAS score did not differ significantly, indicating that constant VAS intervals were present at each endpoint in the two groups. Variable × time interactions of VAS score differed significantly while at rest (F[2.1, 102.9] = 96.8, P < 0.01) and while moving (F[2.4, 118.2] = 99.9, P < 0.01), showing significant sequential changes within the groups over time. Within each group, VAS score was significantly lower at 24, 48, and 72 hours than at baseline, both while at rest and while moving (P < 0.01). At all four time points, ie, 4, 24, 48, and 72 hours after total knee arthroplasty, the mean VAS score was significantly lower in the electrophysiologically guided group than in the traditional nerve stimulator group (P < 0.01, , ). Variable × time and variable × group interactions for postoperative pain score were not significant.
Figure 3 Mean postoperative VAS changes over 3 days.
Abbreviations: EG, electrophysiologically guided; TNS, traditional nerve stimulator; VAS, visual analog score.
The total amounts of morphine consumed were significantly lower in the electrophysiologically guided group than in the traditional nerve stimulator group at 24 (5.9 ± 1.8 mg versus 6.9 ± 1.7 mg, P < 0.05), 48 (2.9 ± 1.6 mg versus 3.5 ± 2.0 mg, P < 0.05), and 72 (1.9 ± 1.6 mg versus 3.2 ± 1.9 mg, P < 0.05) hours ().
Table 3 Morphine consumption
Side effects
No patient experienced any serious adverse effects, such as seizure, hypotension, urinary retention, or prolonged motor palsy. Two patients in the traditional nerve stimulator group required injections of antiemetic drugs within 24 hours.
Discussion
We have evaluated the relative effects of electrophysiologically guided and traditional nerve stimulator femoral nerve block. The major finding of this study was that electrophysiologically guided preoperative femoral nerve block reduced postoperative pain and morphine consumption more than did the traditional nerve stimulator.
Femoral nerve block has been performed by checking contractions of the quadriceps femoris or brisk patellar tilting induced by a traditional nerve stimulator. However, visual determination of muscle retraction is not ideal for quantification. Although electrodiagnostic methods have been used to evaluate neurologic disease, they have not been used previously to assess peripheral nerve blockade, although a few recent trials have described the use of an electrophysiologic approach.Citation11,Citation12
Electrodiagnostic studies of motor nerves rely on the magnifying effect. Stimulating one motor axon can induce activation of many adjacent muscle fibers simultaneously, depending on the innervation ratio of the target muscle. Amplified electrical impulses are recorded and displayed on a screen in the form of a graph. Electrodiagnostic methods can assist in determining the maximum amplitude of electrical signals generated by stimulation with a minimum intensity, enabling real-time quantification.Citation13 Theoretically, electrophysiologic guidance can be superior to visual assessment in standardization, with more precise quantification, resulting in better nerve location and more accurate nerve blockage.
In patients undergoing knee arthroscopy, ultrasound guidance has been reported to reduce the minimum effective volume of anesthetic required to block the sciatic nerve when compared with a traditional nerve stimulator.Citation14 Continuous femoral nerve block with ultrasound reduced the volumes of local anesthetics and morphine consumption, as well as postoperative pain scores, when compared with a traditional nerve stimulator.Citation15 Thus, regardless of the type of modality, accurate localization can enhance the efficacy of nerve blockade.
The failure rate of femoral nerve block is about 5%,Citation16 with one important reason being anatomic variation.Citation17 For example, anatomic variation in the femoral nerve have been reported in 35% of patients,Citation18 with variable muscular branches or slips dividing the nerve. None of our patients experienced failure of femoral nerve block. Electrophysiologic guidance, which displays the shape of electrical impulses on a screen, has the advantage of finding nerve variations (compound motor action potential). Given that normal curves are biphasic,Citation13 a division of the first peak into two or more peaks would suggest the presence of an anatomic variation. Thus, electrophysiologic guidance may reduce the failure rate of femoral nerve block.
The rate of femoral nerve injury due to puncture or intraneural injection has been reported to be 0.7% in 709 femoral nerve blocks.Citation19 None of our patients experienced femoral neuritis or neuropathy. Conduction block, defined as an inhibition in the spread of an electrical current resulting in a reduction in amplitude to 80%–90%, may be induced if stimulation with an intensity > 1.0 mA is performed within 2 mm of the epineurium in rat sciatic nerve.Citation12 The extraneural threshold for activation ranges from 0.3 to 0.6 mA in humans, with an intraneural threshold of 0.3 mA.Citation20,Citation21 However, there have been no reports to date on the range of amplitude in which conduction blocks occur in humans. It is difficult to detect a small reduction (10%–20%) in amplitude by observing muscle contractions or patellar movement. Electrophysiologic guidance can allow quantitative comparison of amplitude, thus avoiding injury to the nerve. Because eight patients violated the protocol, we utilized per-protocol analysis rather than intention-to-treat analysis. However, per-protocol analysis may overestimate results.Citation22
Knee pain can originate from the distribution of obturator or lateral femoral cutaneous nerves.Citation7 Fascia iliaca block (“3-in-1”) has been developed for complete analgesia, with large volumes (20–60 mL) required. The volume we used (10 mL) may be insufficient for complete blockade of two nerves. Moreover, injection of sufficient volume may not completely block two nerves.Citation23,Citation24 Because we did not determine whether the obturator or lateral femoral cutaneous nerve was blocked, the result we observed may not represent the only effect of femoral nerve block. In addition, sciatica and hip joint disorders may mask the pain of osteoarthritis knee joint, and we did not exclude patients with comorbidities of the spine and hip.
The clinical effectiveness of femoral nerve block has been assessed using functional outcomes such as length of hospital stay and range of motion.Citation25,Citation26 However, we did not functionally evaluate our patients. Although total knee arthroplasty is performed predominantly in female patients in our country, the gender ratio of our patients may not represent that of patients undergoing total knee arthroplasty. Another limitation may be poor standardization of other factors affecting pain induction, such as duration of surgery and amount of opioid or pain killers used during surgery.
Conclusion
Electrophysiologically guided single injection femoral nerve block can provide better pain relief than traditional nerve stimulator femoral nerve block in patients undergoing total knee arthroplasty, as well as reducing the consumption of analgesics, suggesting that the electrophysiologically guided approach may prove more efficacious in localizing nerves. Except for its greater cost, the electrophysiologically guided approach may be a good alternative, especially for physicians experienced in electrodiagnosis.
Acknowledgements
Authors are grateful to Geum Mi Lee, nurse practitioner, for collection of data and coordination for scheduling and Mi Jeong Kim, medical technologist, and Dae-Sik Son and Jin Wan Seong, residents, for their valued assistance on the electrophysiological intervention.
Disclosure
The authors report no conflicts of interest in this work.
References
- HadzicAHouleTTCapdevilaXIlfeldBMFemoral nerve block for analgesia in patients having knee arthroplastyAnesthesiology201011351014101520881593
- IlfeldBMDukeKBDonohueMCThe association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplastyAnesth Analg201011161552155420889937
- FeibelRJDervinGFKimPRBeaulePEMajor complications associated with femoral nerve catheters for knee arthroplasty: a word of cautionJ Arthroplasty200924Suppl 613213719553071
- PaulJEAryaAHurlburtLFemoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trialsAnesthesiology201011351144116220966667
- MichaudGTragerGDeschampsSHemmerlingTMMonitoring neuromuscular blockade at the vastus medialis muscle using phonomyographyCan J Anaesth200552879580016189329
- KaratasGKMerayJSuprascapular nerve block for pain relief in adhesive capsulitis: comparison of 2 different techniquesArch Phys Med Rehabil200283559359711994796
- WinnieAPRamamurthySDurraniZThe inguinal paravascular technic of lumbar plexus anesthesia: the “3-in-1 block”Anesth Analg19735269899964796576
- RitchieEDTongDChungFNorrisAMMiniaciAVairavanathanSDSuprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality?Anesth Analg1997846130613129174311
- SingelynFJGouverneurJMPostoperative analgesia after total hip arthroplasty: iv PCA with morphine, patient-controlled epidural analgesia, or continuous “3-in-1” block: a prospective evaluation by our acute pain service in more than 1,300 patientsJ Clin Anesth199911755055410624638
- SimpsonDCurranMPOldfieldVKeatingGMRopivacaine: a review of its use in regional anaesthesia and acute pain managementDrugs200565182675271716392884
- FuzierRRichezASChoquetOSingelynFElectrical nerve localization: non-linear relationship between intensity and pulse duration to stimulate a nerveAnn Fr Anesth Reanim20082710802807 French.18922669
- LiJKongXGozaniSNShiRBorgensRBCurrent-distance relationships for peripheral nerve stimulation localizationAnesth Analg2011112123624120966439
- WilbournAJNerve conduction studies. Types, components, abnormalities, and value in localizationNeurol Clin200220230533812152438
- DanelliGGhisiDFanelliAThe effects of ultrasound guidance and neurostimulation on the minimum effective anesthetic volume of mepivacaine 1.5% required to block the sciatic nerve using the subgluteal approachAnesth Analg200910951674167819843807
- AvelineCLe RouxALe HetetHVautierPCognetFBonnetFPostoperative efficacies of femoral nerve catheters sited using ultrasound combined with neurostimulation compared with neurostimulation alone for total knee arthroplastyEur J Anaesthesiol2010271197898420601891
- GurnaneyHGaneshACucchiaroGThe relationship between current intensity for nerve stimulation and success of peripheral nerve blocks performed in pediatric patients under general anesthesiaAnesth Analg200710561605160918042857
- KirchmairLLirkPColvinJMitterschiffthalerGMorigglBLumbar plexus and psoas major muscle: not always as expectedReg Anesth Pain Med200833210911418299090
- AnloaguePAHuijbregtsPAnatomical variations of the lumbar plexus: a descriptive anatomy study with proposed clinical implicationsJ Man Manip Ther2009174e107e11420140146
- SharmaSIorioRSpechtLMDavies-LepieSHealyWLComplications of femoral nerve block for total knee arthroplastyClin Orthop Relat Res2010468113514019680735
- HadzicAVlokaJDClaudioREHadzicNThysDMSantosACElectrical nerve localization: effects of cutaneous electrode placement and duration of the stimulus on motor responseAnesthesiology200410061526153015166574
- BigeleisenPEMoayeriNGroenGJExtraneural versus intraneural stimulation thresholds during ultrasound-guided supraclavicular blockAnesthesiology200911061235124319417603
- MelanderHAhlqvist-RastadJMeijerGBeermannBEvidence b(i) ased medicine – selective reporting from studies sponsored by pharmaceutical industry: review of studies in new drug applicationsBMJ200332674001171117312775615
- CauhepeCOliverMColombaniRRailhacNThe “3-in-1” block: myth or reality?Ann Fr Anesth Reanim198984376378 French.2817551
- MarhoferPNaselCSitzwohlCKapralSMagnetic resonance imaging of the distribution of local anesthetic during the three-in-one blockAnesth Analg200090111912410624991
- SingelynFJDeyaertMJorisDPendevilleEGouverneurJMEffects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplastyAnesth Analg199887188929661552
- WangHBoctorBVernerJThe effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacementReg Anesth Pain Med200227213914411915059