Abstract
Background and Purpose
In this study, we compared patient outcomes between the 120-W thulium laser (Vela™XL) prostate enucleation (ThuLEP) and bipolar transurethral enucleation of the prostate (B-TUEP) techniques.
Methods
We excluded patients with concomitant prostate cancer and bladder cancer and prospectively analyzed patients with benign prostatic obstruction (BPO) who underwent ThuLEP and B-TUEP from October 2018 to January 2021 in our institution. Patients’ demographics, comorbidities, prostate volumes, prostate-specific antigen (PSA) levels, and International Prostate Symptoms Score (IPSS) were recorded. Perioperative outcomes including intraoperative blood loss, prostate resection percentage of the transition zone, postoperative pain score (numeric rating scale, NRS), complications, changes in postoperative uroflowmetry parameters, IPSS, and the rate of reuse of BPH medications were also evaluated.
Results
The data of a total of 111 patients (ThuLEP: 49, B-TUEP: 62) met the inclusion criteria were collected and analyzed prospectively. Our results revealed no significant differences between ThuLEP and B-TUEP in terms of operation time, prostate tissue enucleated, and days of hospitalization. However, patients in the ThuLEP group reported less pain after surgery than those in the B-TUEP group, and a higher proportion of patients in the B-TUEP group returned to the emergency department due to complications within one month postoperatively, with hematuria being the main cause. No significant differences were observed between the groups in changes in uroflowmetry parameters and IPSS at 2 weeks, 3 months, and 6 months postoperatively.
Conclusion
The efficacy of ThuLEP was comparable to that of B-TUEP in terms of maximal flow rate, voiding volume, IPSS, and quality of life. ThuLEP also had several advantages over B-TUEP, including less blood loss and less postoperative pain. Therefore, ThuLEP can be considered a treatment of choice for BPH/bladder outlet obstruction, specifically for patients with a bleeding tendency and fear of pain.
Introduction
Symptomatic benign prostatic obstruction (BPO) is bladder outlet obstruction (BOO) secondary to benign prostatic enlargement.Citation1 Benign prostatic hyperplasia (BPH) is characterized by the development of the epithelial and stromal cells within the transition zone of the prostate gland, and it is the most common etiology of BPO. For decades, transurethral resection of the prostate (TURP) has been the gold standard surgical treatment for lower urinary tract symptoms secondary to BPH. However, many novel techniques that minimize potential complications related to TURP, such as clot retention, urinary tract infection (UTI), urinary retention, urethral strictures, and bladder neck contractures, have been developed.Citation2 Although improvements in the instruments used in TURP have reduced complications, the high recurrence rate remains a concern. To overcome this problem, new surgical techniques such as endoscopic enucleation were developed. Compared with bipolar TURP, the new bipolar transurethral enucleation of the prostate (B-TUEP) technique has comparable surgical outcomes, shorter operating times, lower hospitalization rate, and fewer complications.Citation3 Laser enucleation involves fewer bleeding complications and has thus increasingly replaced conventional TURP worldwide.Citation4–Citation6 However, studies comparing bipolar and laser transurethral enucleation of the prostate are few. In this study, we compared patient outcomes between the 120 W thulium laser (Vela™XL) enucleation of the prostate (ThuLEP) and bipolar transurethral enucleation of the prostate (B-TUEP) techniques.
Materials and Methods
Patients
The ThuLEP and B-TUEP techniques performed by a single skilled surgeon from October 2018 to January 2021 were prospectively compared to evaluate their efficacy and safety. Patients were free to select the method of operation and signed consent forms before the operation. All the patients enrolled in this study met the TURP surgical indications and had been on medications for at least 3 months before surgery. The study was fully complies with the Declaration of Helsinki and accredited by the Institutional Review Board Statement: Ethical approval for this study has been obtained from the Chang Gung Memorial Hospital (ID 201800120BO, Aproval date: IRB No.: 201900094B0C502, 2020).
Patients aged 60–90 years old who were diagnosed as having clinical BPH and had at least one of the following conditions were included in the study: acute or recurrent urinary retention, gross hematuria, UTI, and significant lower urinary tract symptoms that were unresponsive to medication treatments. We excluded patients with concomitant prostate cancer, bladder cancer, or another active malignant disease and those older than 90 years with ECOG performance status >1Citation7 and with a history of prostate surgery or reconstruction surgery of the urinary system. Each patient provided detailed informed consent before the relevant interventions.
Perioperative outcomes including the amount of blood loss, prostate enucleated percentage of the transition zone, postoperative pain score (numeric rating scale, NRS), surgical complications, changes in postoperative uroflowmetry, International Prostate Symptoms Score (IPSS), and prostate-specific antigen (PSA) level, and the rate of reuse of BPH medications were evaluated. Blood loss was calculated based on the method proposed by Ungjaroenwathana et al.Citation7,Citation8 Foley catheter traction was not applied to reduce postoperative bleeding in both the groups. On the second postoperative day, all Foley catheters were scheduled to be removed. Postoperative prophylactic antibiotic use or adjustment was determined based on urine culture results of effective antibiotics.Citation9 The NRS was used to measure the patients’ subjective postoperative pain.Citation10 All patients were treated with acetaminophen for pain relief after surgery. If acetaminophen failed to relieve pain, intramuscular nalbuphine hydrochloride injection was administered as an analgesic. Following surgery, all patients received tamsulosin 0.4 mg once daily for one week. After discharge from the hospital, the patients returned to the clinic at the second week, third month, and sixth month after the operation, with measurement of the IPSS and uroflowmetry at each visit. Medication may be restarted based on the patient’s micturition status and at the urologist’s discretion. In addition to the 3 scheduled visits, the patients could visit the outpatient clinic for checkups and in-time management if they faced any discomfort.
Surgical Procedure
The patients in the B-TUEP group were operated on using the technique described by Liu et al.Citation10,Citation11 Our instruments included an Olympus SurgMaster UES-40 bipolar generator and an OES-Pro bipolar resectoscope (Olympus Europe, Hamburg, Germany). The cutting and coagulation energy settings were 200 and 120 W, respectively.
In the ThuLEP group, the patients were operated on using the technique described by Herrmann et al.Citation5,Citation12 A 120-W thulium laser (VelaTM XL, Boston Scientific, Marlborough, Massachusetts, USA) was used at a continuous wavelength of 1.94 μm. The laser fiber was introduced using an Olympus 26F continuous-flow resectoscope. Enucleation and resection were performed at different energy settings of 60W and 120W, respectively. The enucleated prostate tissue was ground using a Wolf Piranha Morcellator (Richard Wolf GmbH, Knittlingen, Germany).
Sodium chloride solution (0.9%; normal saline) was used for irrigation. After the operation, a 22-F, 3-way Foley catheter was placed without external traction, and the bladder was continuously irrigated with normal saline to maintain a clear urine flush. The Foley catheter was intended to be withdrawn on postoperative day 2 once the patients’ hematuria stopped.
Statistical Analysis
Statistical analysis of the results was performed using SPSS 25.0. The student’s t-test was used to compare perioperative quantitative variables; all numerical results are presented as mean ± standard deviation.The chi-square test was used to analyze qualitative variables. The Kaplan-Meier plot was used to compute and compare the two groups’ medication-free survival rates over time. Differences with P values of < 0.05 were considered statistically significant.
Results
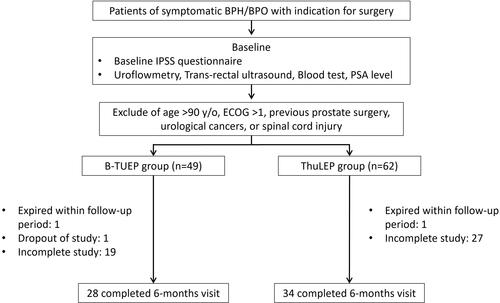
presents a flowchart of patient treatment. The data of 132 patients who underwent B-TUEP and ThuLEP were prospectively collected and analyzed. Among them, 111 met our inclusion criteria and were included in the final analysis (ThuLEP: 49, B-TUEP: 62). The patients’ demographics, comorbidities, preoperative prostate volumes, PSA level, and IPSS were comparable between the groups, as shown in . Our results revealed that ThuLEP and B-TUEP exhibited no significant differences in terms of operation time (84.5 min vs 77.7 min, P = 0.241), prostate tissue enucleated (70.4% vs 70.7%, P = 0.957), and days of postop hospitalization (2.1 days and 2.5 days, P = 0.118; ). However, compared with B-TUEP, ThuLEP was associated with lower intraoperative blood loss (82.4 and 199.2 mL, respectively, P< 0.001). None of our patients in both the groups required blood transfusions due to severe anemia following surgery (). Only one patient in the B-TUEP group returned to the operation room for transurethral endoscopic hemostasis due to severe hematuria. Within one month after surgery, 5 patients in the B-TUEP group but none in the ThuLEP group returned to the emergency room due to hematuria.
Table 1 Baseline Characteristics-1
Table 2 Baseline Characteristics-2
Table 3 Perioperative Results
In terms of postoperative pain, on the first and second postoperative day, a higher proportion of patients in the ThuLEP group reported no pain at all (NRS = 0) than in the B-TUEP group (postop day 1: 72.6% vs 32.7%, P< 0.001; postop day 2: 80.6% vs 51.0%, P = 0.001), indicating that the patients in the ThuLEP group experienced less postoperative pain. A higher proportion of the patients in the B-TUEP group returned to the emergency department due to complications within postop one month (24.4% vs 8.1%, P = 0.032), with hematuria being the main cause.
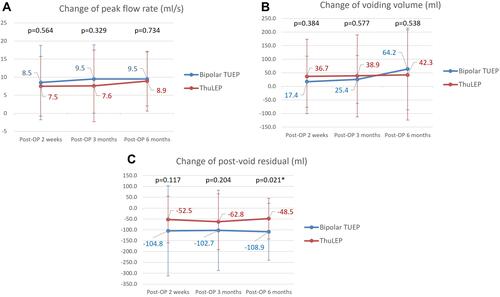
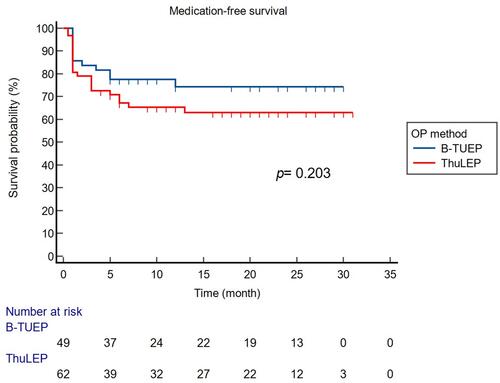
A total of 62 of our included patients (ThuLEP: 28, B-TUEP: 34) completed all follow-up assessments over a 6-month period and were then kept tracked in our outpatient clinic, as shown in . At follow-up, significant improvements in the IPSS, IPSS QOL, and uroflowmetry parameters were observed in both the surgical groups, indicating that both surgical methods are equally effective in terms of the extent of improvement (). No significant difference was noted between the groups in terms of changes in uroflow and IPSS at 2 weeks, 3 months, and 6 months postoperatively, except for postvoid residual volume at 6 months, which was significantly decreased in the B-TUEP group (−48.5 mL, −108.9 mL, P = 0.021) compared with the ThuLEP group, as shown in . The medication-free survivals of the two groups were also compared because the optimal surgical result for BPO is postoperative urologic medication-free. In our study, the term “post-operative medication-free” meant that the patients were no longer taking any medications that interfere with urination, such as alpha-blockers, antimuscarinics, Beta-3 agonists, or parasympathomimetic choline carbamate. Our data revealed that, following surgery, no significant difference was observed between the 2 groups in terms of the need for prolonging medication due to lower urinary tract symptoms, as shown in (p = 0.203).
Table 4 Postoperative IPSS and QoL Changes
Discussion
Transurethral endoscopic prostate enucleation, due to its efficacy (irrespective of size and the advantage of complete adenoma removal), is being increasingly used for the treatment of BPH and is predicted to become the new standard. Bipolar TURP, also known as transurethral plasma kinetic resection of the prostate and which is performed using a bipolar loop and physiological normal saline irrigation, was developed to replace the traditional monopolar TURP, thereby reducing the risk of TURP syndrome. Bipolar TURP involves prolonged operation times, which allows a more careful and effective removal of the anatomical prostatic tissue by the surgeon.Citation13
Hiraoka and Akimoto pioneered transurethral enucleation for BPH in 1989 by using a detaching blade to separate the adenoma from the surgical capsule, thereby minimizing the chances of capsular perforation compared with standard TURP.Citation14 Then, Gilling et alCitation13 developed the Holmium laser enucleation of the prostate in combination with transurethral tissue morcellation and reported effective and safe results.Citation15 Subsequently, various laser energies were introduced into the endoscopic enucleation procedure. Bach et alCitation14 were the first to introduce the ThuLEP technique.Citation16
Compared with TURP, ThuLEP has the advantages of lower blood loss, higher intraoperative safety, less normal saline irrigation, shorter catheterization, and shorter hospital stay, but involves longer operating times.Citation17 Feng et alCitation16 demonstrated that ThuLEP resulted in a smaller hemoglobin decrease than plasma kinetic enucleation of the prostate (PKEP).Citation18 Based on the known long procedure learning curve, determining the speed and manner of performance of experienced surgeons could shorten the operation times.Citation19 Estimating blood loss in TURP was previously difficult because it could only be assessed based on hemoglobin levels before and after surgery or the physician’s subjective determination. We calculated perioperative blood loss by using the concept of equivalent solute mass by measuring the volume and the hematocrit of the irrigating fluid and the hematocrit of the preoperative blood sample. The calculated results revealed that ThuLEP involved considerably less intraoperative blood loss than B-TUEP. Our results showed that the 2 procedures were comparable in terms of perioperative safety and operation times.
In our previous retrospective study, we compared the postoperative pain condition between ThuLEP and bipolar TURP and found that ThuLEP was associated with significantly lower short-term postoperative pain than bipolar TURP.Citation20 However, no other study has compared postoperative pain in patients treated with ThuLEP and those treated with B-TUEP. In the current study, we evaluated pain in the patients using the NRS, which is widely used in clinical practice. The patients in the ThuLEP group reported less pain on the first- and second-day following surgery than those in the B-TUEP group (P< 0.001 on postoperative day 1, P = 0.002 on postoperative day 2). No difference in the proportion of patients who required injected analgesics during hospitalization (P = 0.730) or who continued to use painkillers for more than one week following surgery (P = 0.095) was observed between the 2 groups.
According to Yuan et alCitation19, the thulium laser is operated in a continuous-wave mode with a wavelength close to the peak absorption of water (1.94 μm), resulting in less damage to surrounding tissues.Citation21 In a canine prostate tissue vaporization study, the thulium laser generated a thermal coagulation zone ranging from 500 to 2000 μm (in a continuous-wave mode), which provided adequate hemostasis during the operation and helped control the thermal damage zone in prostate tissues.Citation22 In comparison, the penetrating thermal depth of bipolar TURP is approximately 2.4 mm, which is considerably greater than that of the thulium laser.Citation23 The disparity in postoperative pain outcomes may be explained by the difference in the penetrating depth of the techniques in tissue injury.
Unlike photoselective vaporization with the green light laser, which vaporizes the prostate tissue and makes it inaccessible for pathological analysis,Citation23 ThuLEP and B-TUEP techniques preserve the resected pathological tissue and help detect potential early stage prostate cancer. In our study, 6.1% of our participants had prostatic adenocarcinomas, and they were omitted from the analysis because they would have to undergo further treatment.
During hospitalization, only one patient in the B-TUEP group required endoscopic hemostasis, no difference in the length of hospital stay was observed between the 2 groups (P = 0.118).
No patient in both the groups required postoperative blood transfusion due to anemia. Moreover, no difference in the proportion of Foley catheter reinsertion after Foley catheter removal (P = 1.000) or the proportion of postoperative UTI (P = 0.306) was noted between the 2 groups.
Compared with the ThuLEP group, considerably higher number of patients in the B-TUEP group returned to the emergency room within one month after discharge. Five patients in the B-TUEP group presented with hematuria compared with none in the ThuLEP group, and one patient in the B-TUEP group presented with bladder tamponade compared with none in the ThuLEP group.
According to our study results, both the studied surgical methods are safe. In particular, no significant difference in the incidence of postoperative blood transfusion, urine retention, and UTI was observed between the 2 groups. However, the probability of returning to the emergency room after surgery was significantly lower in the ThuLEP group than in the B-TUEP group, the most important factor for which was hematuria. Thus, ThuLEP may allow more efficient control of blood loss than B-TUEP.
This study had some limitations. First, the sample size was not sufficiently large. Only 62 of the included patients completed every follow-up data we set within 6 months following surgery, except for two patients who died during the follow-up period and one who was lost to follow-up. The main reason is that many patients, particularly those who had good surgical outcomes, are unwilling to return to the hospital for repeating the same exams and questionnaires during the Covid-19 pandemic. This made obtaining all of the patients’ IPSS scores as well as the urodynamic study data challenging. Second, surgical grouping was based on patient preference rather than random assignment, which may have resulted in bias and did not allow double blinding. Third, this study only analyzed preliminary data, and the follow-up duration was short. However, because this is an ongoing research, we are continually collecting more clinical data for long-term follow-up. Despite the aforementioned study limitations, we believe that our research is valid and practical and is the first prospective head-to-head case–control study comparing the surgical outcomes between B-TUEP and ThuLEP, to the best of our knowledge.
Conclusions
The efficacy of ThuLEP was comparable to that of B-TUEP in terms of Qmax, VV, IPSS, and QoL, and it had several advantages over B-TUEP, including less blood loss and less postoperative pain. Thus, ThuLEP can be considered a treatment of choice for BPH/BOO, particularly for patients with a bleeding tendency and fear of pain.
Acknowledgments
Institutional Review Board Statement: Ethical approval for this study has been obtained from the Chang Gung Memorial Hospital (ID 201800120BO, Approval date: IRB No.: 201900094B0C502, 2020) Institutional Review Boards (IRB) in Taiwan. Informed Consent Statement: Inform consent was obtained from all study patients. The authors thank Wallace Academic Editing for editing this manuscript.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Funding
References
- Abrams P. LUTS, BPH, BPE, BPO: a plea for the logical use of correct terms. Rev Urol. 1999;1(2):65.
- Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol. 2006;50(5):969–79; discussion 980. doi:10.1016/j.eururo.2005.12.042
- Arcaniolo D, Manfredi C, Veccia A, et al. Bipolar endoscopic enucleation versus bipolar transurethral resection of the prostate: an ESUT systematic review and cumulative analysis. World J Urol. 2020;38(5):1177–1186. doi:10.1007/s00345-019-02890-9
- Gilling PJ. Laser enucleation is increasingly becoming the standard of care for treatment of benign prostatic hyperplasia of all sizes. Eur Urol. 2013;63(5):868–9; discussion 870–871. doi:10.1016/j.eururo.2013.01.001
- Herrmann TR, Bach T, Imkamp F, et al. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol. 2010;28(1):45–51. doi:10.1007/s00345-009-0503-0
- Chow R, Zimmermann C, Bruera E, et al. Inter-rater reliability in performance status assessment between clinicians and patients: a systematic review and meta-analysis. BMJ Support Palliat Care. 2020;10(2):129–135. doi:10.1136/bmjspcare-2019-002080
- Ungjaroenwathana W, Bunyaratavej C, Tosukhowong P, et al. Estimation of blood loss in transurethral resection of prostate (TUR-P) by urine-strip. J Med Assoc Thai. 2007;90(11):2409–2415.
- Qiang W, Jianchen W, MacDonald R, et al. Antibiotic prophylaxis for transurethral prostatic resection in men with preoperative urine containing less than 100,000 bacteria per mL: a systematic review. J Urol. 2005;173(4):1175–1181. doi:10.1097/01.ju.0000149676.15561.cb
- Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi:10.1111/j.1365-2702.2005.01121.x
- Liu C, Zheng S, Li H, et al. Transurethral enucleation and resection of prostate in patients with benign prostatic hyperplasia by plasma kinetics. J Urol. 2010;184(6):2440–2445. doi:10.1016/j.juro.2010.08.037
- Hu Y, Dong X, Wang G, et al. Five-year follow-up study of transurethral plasmakinetic resection of the prostate for benign prostatic hyperplasia. J Endourol. 2016;30(1):97–101. doi:10.1089/end.2015.0506
- Hiraoka Y, Akimoto M. Transurethral enucleation of benign prostatic hyperplasia. J Urol. 1989;142(5):1247–1250. doi:10.1016/S0022-5347(17)39047-X
- Le Duc A, Gilling PJ. Holmium laser resection of the prostate. Eur Urol. 1999;35(2):155–160. doi:10.1159/000019836
- Bach T, Wendt-Nordahl G, Michel MS, et al. Feasibility and efficacy of Thulium: YAGlaser enucleation (VapoEnucleation) of the prostate. World J Urol. 2009;27(4):541–545. doi:10.1007/s00345-008-0370-0
- Yang Z, Wang X, Liu T. Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology. 2013;81(2):396–400. doi:10.1016/j.urology.2012.08.069
- Feng L, Zhang D, Tian Y, et al. Thulium laser enucleation versus plasmakinetic enucleation of the prostate: a randomized trial of a single center. J Endourol. 2016;30(6):665–670. doi:10.1089/end.2015.0867
- Shah HN, Mahajan AP, Sodha HS, et al. Prospective evaluation of the learning curve for holmium laser enucleation of the prostate. J Urol. 2007;177(4):1468–1474. doi:10.1016/j.juro.2006.11.091
- Hou CP, Lin YH, Juang HH, et al. Clinical outcome of transurethral enucleation of the prostate using the 120-W thulium laser (Vela™ XL) compared to bipolar transurethral resection of the prostate (TURP) in aging male. Aging. 2020;12(2):1888–1898. doi:10.18632/aging.102720
- Yuan R, Zhou JJ, Shu XH, et al. Transurethral thulium laser enucleation versus resection of the prostate for treating benign prostatic hyperplasia: a retrospective study. Lasers Med Sci. 2019;34(2):329–334. doi:10.1007/s10103-018-2597-3
- Fried NM. High-power laser vaporization of the canine prostate using a 110 W Thulium fiber laser at 1.91 microm. Lasers Surg Med. 2005;36(1):52–56. doi:10.1002/lsm.20126
- Maddox M, Pareek G, Al Ekish S, et al. Histopathologic changes after bipolar resection of the prostate: depth of penetration of bipolar thermal injury. J Endourol. 2012;26(10):1367–1371. doi:10.1089/end.2012.0202
- Teng J, Zhang D, Li Y, et al. Photoselective vaporization with the green light laser vs transurethral resection of the prostate for treating benign prostate hyperplasia: a systematic review and meta-analysis. BJU Int. 2013;111(2):312–323. doi:10.1111/j.1464-410X.2012.11395.x
- Lee WC, Lin YH, Hou CP, et al. Prostatectomy using different lasers for the treatment of benign prostate hyperplasia in aging males. Clin Interv Aging. 2013;8:1483–1488. doi:10.2147/CIA.S52697