Abstract
Purpose
Percutaneous endoscopic transforaminal lumbar interbody fusion (PE-TLIF) has become one of the most popular minimally invasive surgeries today. However, the issue of hidden blood loss (HBL) in this surgery has received little attention. This study aims to examine the HBL in PE-TLIF surgery and the effect of tranexamic acid (TXA) on blood loss.
Methods
In our research, We conducted a retrospective analysis of 300 patients who underwent PE-TLIF from September 2019 to August 2023. They were divided into 2 groups based on whether they received intravenous TXA injection before surgery. The variables compared included: demographic data, pre-and postoperative hemoglobin (HB), hematocrit (HCT), platelets (PLT), red blood cells (RBC), total blood loss (TBL), visible blood loss (VBL), HBL, operation time, postoperative hospital stay, inflammatory markers, coagulation parameters, and adverse events.
Results
Regarding demographic characteristics, besides the operation time, no significant differences were observed between the two groups. Compared with the control group, the TXA group showed a significant reduction trend in TBL, HBL, and VBL (P < 0.05). On the first day after surgery, there were significant differences in prothrombin (PT), activated partial thromboplastin time (APTT), and D-dimer (D-D) levels between the two groups. Similarly, HCT also found similar results on the third day after surgery. No adverse events occurred in either group.
Conclusion
Research has found that there is a significant amount of HBL in patients undergoing PE-TLIF. Intravenous injection of TXA can safely and effectively reduce perioperative HBL and VBL. Additionally, compared to the control group, the TXA group shows a significant reduction in operation time.
Introduction
With the increase in the aging population, the incidence of degenerative lumbar disease has been rising year by year.Citation1,Citation2 PE-TLIF, due to its minimal trauma, fast recovery, and fewer complications, is widely used in the treatment of degenerative lumbar disease, particularly favored by middle-aged and elderly patients.Citation3–5 However, the bleeding situation of this minimally invasive surgery is often overlooked, especially HBL. The recent researchCitation6 found that the HBL of endoscopic transforaminal lumbar interbody fusion (Endo-TLIF) can reach 91% of TBL, with an average of approximately 717.9 ± 220.1 mL. Similarly, Zhou L et alCitation7 found that the HBL during oblique lateral interbody fusion (OLIF) accounted for 92.4% of the TBL, averaging around 809.0 ± 358.8 mL. Massive HBL can increase the risk of infection, anemia, blood transfusion, and other complications, which significantly affect the speed of postoperative recovery, increase medical expenses, and even endanger the patient’s life.Citation8 Therefore, finding effective ways to reduce HBL has become a major concern in PE-TLIF surgery.
Tranexamic acid (TXA) is a synthetic analogue of lysine that reduces intraoperative bleeding by inhibiting plasminogen activation and blocking fibrinolysis.Citation9,Citation10 At the same time, TXA also has certain anti-inflammatory effects and the ability to regulate the body’s immune response.Citation11–13 Some studies have shown that TXA can effectively reduce blood loss and blood transfusion requirements in surgical procedures, such as total hip arthroplasty and total knee arthroplasty.Citation14,Citation15 Furthermore, multiple studiesCitation16–18 have demonstrated that the intravenous injection of TXA in spinal surgery can effectively and safely reduce blood loss without increasing related complications. Although TXA is widely used in surgical procedures, its impact in PE-TLIF surgery has not been clearly confirmed.
TXA has multiple routes of administration, including preoperative intravenous infusion, local administration, and intravenous combined with local administration.Citation19,Citation20 However, preoperative intravenous injection of TXA can more effectively inhibit the dissolution of blood clots, thereby reducing bleeding.Citation21 In addition, TXA can pass through physiological barriers about 15 minutes after intravenous injection and accumulate at surgical and trauma sites.Citation22 Therefore, the purpose of this study is to explore the impact of intravenous TXA on HBL in patients undergoing PE-TLIF through retrospective research methods.
Materials and Methods
Study Design
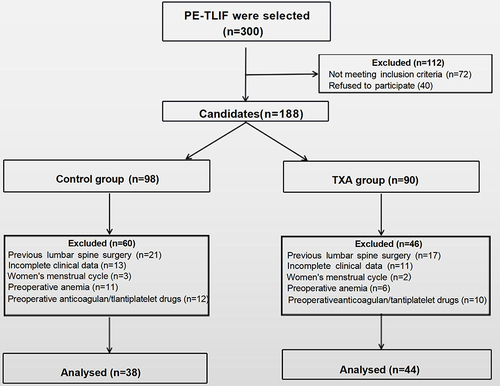
This is a retrospective study following the Helsinki Declaration principles and approved by the Ethics Committee of Zhejiang Provincial People’s Hospital (QT2024043). Considering the retrospective nature of the study, the committee has decided to waive the requirement for written informed consent. The aim of this study is to analyze patients who underwent PE-TLIF surgery in our hospital from September 2019 to August 2023. Of the 300 patients initially screened, 40 lacked follow-up data and 72 did not meet the inclusion criteria. The patients were divided into the TXA group and the control group based on whether TXA was used preoperatively. Specifically, 1g of TXA or an equal amount of 0.9% saline was intravenously injected into the two groups of patients 15 minutes before skin incision. If the surgery lasted more than 2 hours, another dose was administered. Of note, this study used a double-blind design, that is, patients, surgeons, and anesthesiologists were not informed of the specific treatment received by patients. Ultimately, there were 44 patients in the TXA group and 38 patients in the control group ().
The inclusion criteria were as follows: (1) patients aged between 18 years or older; (2) patients diagnosed with lumbar disc herniation, lumbar spinal stenosis, or lumbar spondylolisthesi; (4) patients who underwent PE-TLIF treatment; (5) single-level lumbar surgery.
The exclusion criteria were as follows: (1) history of lumbar spine surgery; (2) lumbar vertebral tumors, tuberculosis, infection, or lumbar vertebral fracture; (3) severe liver, kidney disease, and coagulation dysfunction; (4) patients taking anticoagulant or antiplatelet drugs before or after surgery; (5) allergic to TXA; (6) incomplete data patients; (7) patients who receive blood transfusions during or after surgery; (8) patients with a history of thromboembolism; and (9) preoperative anemia (HB < 110 g/L in females; HB< 120 g/L in males).
Data Collection
The patient’s age, gender, height, weight, body mass index (BMI), bone condition, patient’s blood volume (PBV), disease type, surgical segment, operation time, and postoperative hospital stay were record in the two groups. Record relevant data before surgery, as well as on the first and third days following the procedure, including HB, RBC, PLT, HCT, C-reactive protein (CRP), PT, APTT, TT, and fibrinogen (FIB). Furthermore, blood transfusion and adverse events were documented.
Calculation of HBL
The calculation of HBL is as follows: HBL = TBL - VBL + blood transfusion volume; VBL = intraoperative blood loss + postoperative drainage volume; TBL was calculated using the Gross formula,Citation23 TBL = PBV × (HCT-pre - HCT-post)/HCT-ave, HCT-pre = the preoperative HCT level, HCT-post = the HCT on the third postoperative day, HCT-ave = the average of the HCT-pre and HCT-post, PBV was calculated using the Nadel formula,Citation24 PBV (L) = k1 × height (m)3 + k2 × weight (kg) + k3 (male k1 = 0.3669, k2 = 0.03219, k3 = 0.6041; female k1 = 0.3561, k2 = 0.03308, k3 = 0.1833).
Since no blood transfusion was given during and after the surgery, HBL = TBL - VBL. Meanwhile, no drainage was performed in any patients post-operatively, VBL = intraoperative blood loss. The intraoperative blood loss includes the drainage volume in the drainage bottle minus the volume of flushing fluid during the operation, as well as the net increase in weight of the hemostatic gauze. In conclusion, HBL can be preliminarily estimated.
Surgical Technique
After the anesthesia is done, place the patient in a prone position and raise both sides of the abdomen to facilitate surgery. C-arm fluoroscopy is used to locate the surgical segment and mark the decompression incision, usually 4–6 cm from the midline. This incision is also a pedicle screw skin incision that can be adjusted according to the patient’s condition. Subsequently, puncture localization was performed under fluoroscopy, and the soft tissue around the articular process was separated using the gradually expanding catheter, which was then inserted into the endoscope. Extensive bone decompression was performed using the endoscopic circular saw and laminar rongeur to remove the upper articular process and part of the vertebral lamina, thereby enlarging the intervertebral foramen. The ligamentum flavum was separated and removed to fully expose the dural sac and nerve roots, ensuring adequate decompression. Replace the fusion sleeve to safeguard the nerve root, and expose and remove the intervertebral disc to handle the intervertebral space. Next, introduce autologous or allogeneic bone into the intervertebral space, and position a suitable interbody fusion Cage. Meanwhile, use a C-arm machine to ensure the correct position. Then, double check if the nerve root has been fully decompressed. Finally, percutaneous placement of pedicle screws and bilateral connecting rods was performed. All patients undergo surgery by the same spine surgeon. In addition, all patients adopted a similar perioperative management plan.
Statistical Methods
This study employed SPSS 23.0 software for statistical analysis. Normally distributed data was presented as mean ± standard deviation and analyzed using independent samples t-test. Non-normally distributed data was presented as M [P25; P75] and compared using Mann–Whitney U-test. Furthermore, chi-square test was utilized to determine the relationship between categorical variables. P < 0.05 was deemed statistically significant.
Results
During the study, a total of 82 patients who met the inclusion criteria were enrolled. Out of these, 44 individuals were in the TXA group, while the control group consisted of 38 people. Statistical analysis shows that the TXA group required less surgical time compared to the control group, with statistical significance. Additionally, there were no statistically significant differences in the remaining baseline characteristics between the two groups ().
Table 1 The Baseline Data of the Two Groups
No statistically difference in coagulation indicators was observed between the two groups of patients before and on the third day after surgery. However, the PT, APTT, and D-D levels in the group receiving TXA treatment on the first day after surgery were significantly lower than those in the control group (). In addition, TXA did not have a significant impact on changes in CRP.
Table 2 Coagulation and Inflammatory Parameters of the Two Groups
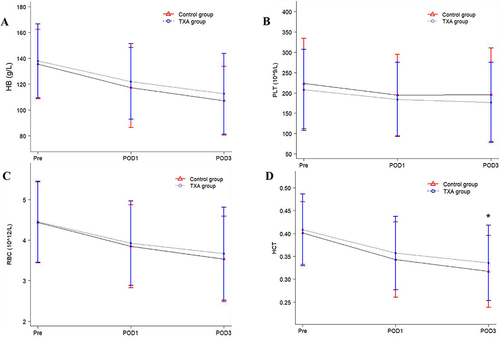
No statistically significant difference of preoperative level of HB, RBC, PLT, and HCT levels were detected between the two groups. However, on the third day post-surgery, a notable difference in HCT was observed between the two groups. Moreover, patients receiving TXA treatment exhibited a slower decline in HB, RBC, and HCT compared to the control group ().
Figure 2 Changes in HB (A), PLT (B), (C) RBC and (D) HCT on preoperative and postoperative days 1, 3 in both groups.
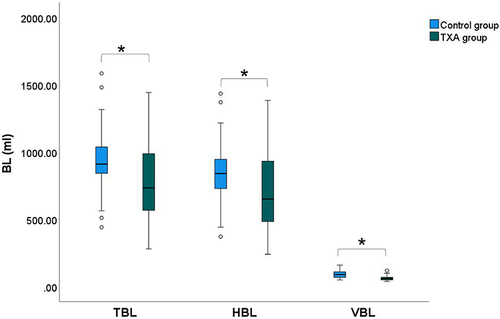
During the perioperative period, the TBL, VBL, and HBL of the TXA group were significantly lower than those of the control group (774.702 ± 309.244 vs 937.523 ± 244.714 mL, 66.136 ± 23.049 vs 93.158 ± 28.674 mL, 708.565 ± 307.985 vs 844.366 ± 237.963 mL, P < 0.05) (). In addition, no adverse events or TXA related side effects occurred among all participants during the study.
Disscussion
PE-TLIF, as a minimally invasive lumbar fusion surgery technique, has received increasing attention from doctors and patients. Compared to traditional open surgery, minimally invasive surgery has the advantages of smaller incisions, less soft tissue invasion, less blood loss, faster postoperative recovery, and shorter hospital stay.Citation24,Citation25 This technique enters the intervertebral space through Kambin’s triangle and can clearly display the dura mater and nerve roots under endoscopy. This allows for safer and more effective decompression and endplate treatment, while avoiding the limited vision of the minimally invasive transforaminal lumbar interbody fusion (Mis-TLIF) technique.Citation26 However, in clinical practice, many patients who undergo this minimally invasive surgery still suffer from anemia or related diseases. Meanwhile, the severity of anemia in postoperative patients does not match the amount of blood loss. The HBL proposed by Sehat et al in 2000 may be related to these outcomes.Citation27 HBL is a special form of blood loss that cannot be directly observed and accurately estimated in clinical practice, so it is often overlooked.Citation28 Many studies have shown that neglecting HBL can not only lead to an increase in blood transfusion requirements, but also result in various complications, including anemia, delayed wound healing, prolonged postoperative recovery, and increased risk of infection.Citation29,Citation30 It seriously affects the safety and recovery of patients during the perioperative period. Therefore, HBL has become a growing concern for surgeons and patients.
Currently, the specific cause of HBL is still unclear. The cause of HBL after spinal fusion surgery may be related to residual blood entering the cavity, bone surface leakage after decompression, and storage of internal fixation systems composed of pedicle screws and rod instrumentation.Citation31 Previous studies have shown that spinal fusion surgery involves a significant amount of HBL. Smorgick Y et al reported that the HBL accounts for 42% of the TBL in posterior lumbar fusion.Citation32 The hidden blood loss of Mis-TLIF reported by Zhou Y et al was 488.4 ± 294.0 mL, which accounted for 52.5% of the total blood loss.Citation33 A similar result was also found in a study on extreme lateral interbody fusion (XLIF) research.Citation34 Interestingly, Zhang H et al found that minimally invasive spinal surgery has more HBL compared to open spinal surgery.Citation35 In our PE-TLIF study, HBL also reached 90% of the TBL, which is consistent with the research results of Ge M et al.Citation6 Therefore, how to effectively reduce HBL has become an urgent problem to be solved in PE-TLIF surgery.
TXA is extensively utilized in surgical procedures due to its proven ability to effectively reduce blood loss and transfusion rates throughout the perioperative period.Citation36,Citation37 During the start of the surgery, the process of fibrinolysis is activated, which is an important factor leading to intraoperative and postoperative bleeding.Citation38 This phenomenon is most pronounced 6–12 hours after surgery.Citation39 By targeting the lysine binding site on plasminogen, TXA effectively inhibits the interaction between plasminogen and fibrin, thereby achieving hemostatic effects.Citation40,Citation41 Moreover, Research has found that the route of administration of tranexamic acid is also another important factor affecting intraoperative and postoperative bleeding.Citation42 Preoperative intravenous injection of TXA can quickly act on the surgical or traumatic site and more effectively inhibit the blood clot breakdown.Citation21,Citation43 Therefore, in this study, preoperative intravenous TXA was used to evaluate the impact on perioperative blood loss in PE-TLIF patients.
Our research has found that in PE-TLIF surgery, HBL is a problem that requires urgent attention and cannot be ignored. The results showed that the HBL of the TXA group was 708.565 ± 307.985mL, VBL was 66.136 ± 23.049 mL, and TBL was 774.702 ± 309.244 mL, which were significantly lower than those of the control group. This result is consistent with the study by Hao S et al in PLIF, both of which significantly reduced HBL.Citation44 Furthermore, TXA is also beneficial for shortening surgical operation time. We also found the trend of HCT changes in the TXA group were relatively small, which is consistent with the research results of Dong W et al and Kelly M et alCitation45,Citation46 D-D can be a reliable indicator of the pre-thrombotic state.Citation47 Interestingly, the average level of D-D at postoperative day 1 in TXA group is significantly lower than that in control group [2815 (1717.5–4497.5) ug/L VS 6415 (3917.5–8482.5) ug/L, P < 0.001)]. This indicates that TXA can effectively reduce postoperative D-D levels, which is supported by Dong et al.Citation46 In addition, neither group of patients experienced any postoperative adverse events or TXA related complications. Therefore, it can be seen that TXA can safely and effectively reduce the HBL and VBL of PE-TLIF, thereby enabling patients to gain greater benefits.
Of course, our research also has some limitations. Firstly, this is a single center study with a relatively small sample size. Secondly, detailed subgroup analysis was not conducted. In addition, there is no unified standard for postoperative activity and dietary nutrition of patients.
Conclusion
This research indicates that there is a large amount of HBL in patients undergoing PE-TLIF. Preoperative intravenous injection of TXA not only effectively reduces HBL and VBL but also does not increase the risk of complications. Additionally, compared to the control group, the TXA group shows a significant reduction in operation time.
Abbreviations
PE-TLIF, Percutaneous endoscopic transforaminal lumbar interbody fusion; HBL, Hidden blood loss; TXA, Tranexamic acid; HB, Hemoglobin; HCT, Hematocrit; PLT, Platelets; RBC, Red blood cells; TBL, Total blood loss; VBL, Visible blood loss; PT, Prothrombin; APTT, Activated partial thromboplastin time; D, D-dimer; Endo-TLIF, Endoscopic transforaminal lumbar interbody fusion; OLIF, Oblique lateral interbody fusion; BMI, Body mass index; PBV, Patient’s blood volume; CRP, C-reactive protein; FIB, Fibrinogen; Mis-TLIF, Minimally invasive transforaminal lumbar interbody fusion; XLIF, Extreme lateral interbody fusion.
Ethics Approval
The study was approved by Zhejiang Provincial People’s Hospital Research Ethics Committee.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Acknowledgment
We would like to express our gratitude to all the participants and their families who participated in this study. Additionally, we extend our thanks to the medical staff at the Zhejiang Provincial People’s Hospital for their valuable support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no competing interests in this work.
Data Sharing Statement
The datasets utilized or analyzed in this study can be obtained from the corresponding author, Tingxiao Zhao, upon reasonable request.
Additional information
Funding
References
- Brailsford JF. Deformities of the lumbosacral region of the spine. Br J Surg. 1929;16:562. doi:10.1002/bjs.1800166405
- Masharawi Y, Rothschild B, Dar G, et al. Facet orientation in the thoracolumbar spine: three-dimensional anatomic and biomechanical analysis. Spine. 2004;29(16):1755–1763. doi:10.1097/01.brs.0000134575.04084.ef
- Ahn Y, Youn MS, Heo DH. Endoscopic transforaminal lumbar interbody fusion: a comprehensive review. Expert Rev Med Devices. 2019;16(5):373–380. doi:10.1080/17434440.2019.1610388
- Kalff R, Ewald C, Waschke A, Gobisch L, Hopf C. Degenerative lumbar spinal stenosis in older people: current treatment options. Dtsch Arztebl Int. 2013;110(37):613–624. doi:10.3238/arztebl.2013.0613
- Brusko GD, Wang MY. Endoscopic Lumbar Interbody Fusion. Neurosurg Clin N Am. 2020;31(1):17–24. doi:10.1016/j.nec.2019.08.002
- Ge M, Zhang Y, Ying H, et al. Comparison of hidden blood loss and clinical efficacy of percutaneous endoscopic transforaminal lumbar interbody fusion and minimally invasive transforaminal lumbar interbody fusion. Int Orthop. 2022;46(9):2063–2070. doi:10.1007/s00264-022-05485-z
- Zhu L, Zhang L, Shan Y, Feng X, Zhang W. Analysis of hidden blood loss and its risk factors in oblique lateral interbody fusion surgery. Clin Spine Surg. 2021;34(9):E501–E505. doi:10.1097/BSD.0000000000001177
- Wu YS, Zhang H, Zheng WH, Feng ZH, Chen ZX, Lin Y. Hidden blood loss and the influential factors after percutaneous kyphoplasty surgery. Eur Spine J. 2017;26(7):1878–1883. doi:10.1007/s00586-017-4950-9
- Kumar PD. Prevention and treatment of major blood loss. N Engl J Med. 2007;357(12):1260–1261.
- Wong J, El Beheiry H, Rampersaud YR, et al. Tranexamic Acid reduces perioperative blood loss in adult patients having spinal fusion surgery. Anesth Analg. 2008;107(5):1479–1486. doi:10.1213/ane.0b013e3181831e44
- Draxler DF, Yep K, Hanafi G, et al. Tranexamic acid modulates the immune response and reduces postsurgical infection rates. Blood Adv. 2019;3(10):1598–1609. doi:10.1182/bloodadvances.2019000092
- Li Y, Xie H, Deng Z, et al. Tranexamic acid ameliorates rosacea symptoms through regulating immune response and angiogenesis. Int Immunophar. 2019;67:326–334. doi:10.1016/j.intimp.2018.12.031
- Zhang S, Xu H, Xie J, Cao G, Lei Y, Pei F. Tranexamic acid attenuates inflammatory effect and modulates immune response in primary total knee arthroplasty: a randomized, placebo-controlled, pilot trial. Inflammopharm. 2020;28(4):839–849. doi:10.1007/s10787-020-00695-6
- Huang F, Wu D, Ma G, Yin Z, Wang Q. The use of tranexamic acid to reduce blood loss and transfusion in major orthopedic surgery: a meta-analysis. J Surg Res. 2014;186(1):318–327. doi:10.1016/j.jss.2013.08.020
- Poeran J, Rasul R, Suzuki S, et al. Tranexamic acid use and postoperative outcomes in patients undergoing total Hip or knee arthroplasty in the United States: retrospective analysis of effectiveness and safety. BMJ. 2014;349(g4829):g4829–g4829. doi:10.1136/bmj.g4829
- Shi H, Ou Y, Jiang D, Quan Z, Zhao Z, Zhu Y. Tranexamic acid reduces perioperative blood loss of posterior lumbar surgery for stenosis or spondylolisthesis: A randomized trial. Medicine. 2017;96(1):e5718. doi:10.1097/MD.0000000000005718
- Yu CC, Gao WJ, Yang JS, et al. Can tranexamic acid reduce blood loss in cervical laminectomy with lateral mass screw fixation and bone grafting: A retrospective observational study. Medicine. 2017;96(5):e6043. doi:10.1097/MD.0000000000006043
- Yuan QM, Zhao ZH, Xu BS. Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J. 2017;26(1):131–139. doi:10.1007/s00586-016-4899-0
- Zhang Y, Wang X, Zhao Q, et al. Effect of intravenous tranexamic acid on perioperative hidden blood loss in percutaneous pedicle screw fixation for thoracolumbar fractures. Chin J Orthop Traum. 2018;20:291.
- Chang L, Xiong W, Liu H, et al. A clinical study on the topical application of tranexamic acid gelatin sponge in lumbar surgery. Chin J Bone Jt. 2017;6:786.
- Mu X, Wei J, Wang C, et al. Intravenous administration of tranexamic acid significantly reduces visible and hidden blood loss compared with its topical administration for double-segment posterior lumbar interbody fusion: A single-center, placebo-controlled. Random Trial World Neurosurg. 2019;122:e821–e827. doi:10.1016/j.wneu.2018.10.154
- Hsieh PW, Chen WY, Aljuffali IA, Chen CC, Fang JY. Co-drug strategy for promoting skin targeting and minimizing the transdermal diffusion of hydroquinone and tranexamic acid. Curr Med Chem. 2013;20(32):4080–4092. doi:10.2174/15672050113109990202
- Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58(3):277–280. doi:10.1097/00000542-198303000-00016
- Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51(2):224–232.
- Zhao XB, Ma HJ, Geng B, Zhou HG, Xia YY. Early clinical evaluation of percutaneous full-endoscopic transforaminal lumbar interbody fusion with pedicle screw insertion for treating degenerative lumbar spinal stenosis. Orthop Surg. 2021;13(1):328–337. doi:10.1111/os.12900
- Zhu L, Cai T, Shan Y, Zhang W, Zhang L, Feng X. Comparison of clinical outcomes and complications between percutaneous endoscopic and minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease. A Sys Rev Meta-Analysis Pain Phys. 2021;24(6):441–452.
- Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000;7(3):151–155. doi:10.1016/s0968-0160(00)00047-8
- Ban ZT, Liu RZ. Progress on hidden blood loss after lumbar interbody fusion. Zhongguo Gu Shang. 2018;31(11):1077–1080. doi:10.3969/j.issn.1003-0034.2018.11.018
- Foss NB, Kehlet H. Hidden blood loss after surgery for Hip fracture. J Bone Joint Surg Br. 2006;88(8):1053–1059. doi:10.1302/0301-620X.88B8.17534
- Ju H, Hart RA. Hidden blood loss in anterior lumbar interbody fusion (ALIF) surgery. Orthop Traumatol Surg Res. 2016;102(1):67–70. doi:10.1016/j.otsr.2015.10.003
- Ren Z, Li S, Sheng L, et al. Topical use of tranexamic acid can effectively decrease hidden blood loss during posterior lumbar spinal fusion surgery: a retrospective study. Medicine. 2017;96(42):e8233. doi:10.1097/MD.0000000000008233
- Smorgick Y, Baker KC, Bachison CC, Herkowitz HN, Montgomery DM, Fischgrund JS. Hidden blood loss during posterior spine fusion surgery. Spine J. 2013;13(8):877–881. doi:10.1016/j.spinee.2013.02.008
- Zhou Y, Fu X, Yang M, Ke S, Wang B, Li Z. Hidden blood loss and its possible risk factors in minimally invasive transforaminal lumbar interbody fusion. J Orthop Surg Res. 2020;15(1):445. doi:10.1186/s13018-020-01971-5
- Mima Y, Yagi M, Suzuki S, et al. Hidden blood loss in extreme lateral interbody fusion for adult spinal deformity. J Orthop Sci. 2023;28(3):509–514. doi:10.1016/j.jos.2022.01.003
- Zhang H, Chen ZX, Sun ZM, et al. Comparison of the total and hidden blood loss in patients undergoing open and minimally invasive transforaminal lumbar interbody fusion. World Neurosurg. 2017;107:739–743. doi:10.1016/j.wneu.2017.08.113
- Wu YG, Zeng Y, Yang TM, Si HB, Cao F, Shen B. The efficacy and safety of combination of intravenous and topical tranexamic acid in revision hip arthroplasty: A randomized, controlled trial. J Arthroplasty. 2016;31(11):2548–2553. doi:10.1016/j.arth.2016.03.059
- Xu X, Xie L, Yu H, Hu Y. Safety and efficacy of tranexamic acid with epinephrine for prevention of blood loss following surgery for trochanteric femoral fractures. Acta Orthop Traumatol Turc. 2020;54(2):132–137. doi:10.5152/j.aott.2020.02.135
- Blanié A, Bellamy L, Rhayem Y, et al. Duration of postoperative fibrinolysis after total Hip or knee replacement: a laboratory follow-up study. Thromb Res. 2013;131(1):e6–e11. doi:10.1016/j.thromres.2012.11.006
- Sharrock NE, Go G, Harpel PC, Ranawat CS, Sculco TP, Salvati EA. The John Charnley Award thrombogenesis during total hip arthroplasty. Clin Orthop Relat Res. 1995;(319):16–27.
- Mannucci PM, Wood AJJ. Hemostatic drugs. N Engl J Med. 1998;339(4):245–253. doi:10.1056/NEJM199807233390407
- Dunn CJ, Goa KL. Tranexamic acid: a review of its use in surgery and other indications. Drugs. 1999;57(6):1005–1032. doi:10.2165/00003495-199957060-00017
- Lin C, Qi Y, Jie L, et al. Is combined topical with intravenous tranexamic acid superior than topical, intravenous tranexamic acid alone and control groups for blood loss controlling after total knee arthroplasty: a meta-analysis [published correction appears in Medicine (Baltimore). Medicine. 2016;95(51):e5344. doi:10.1097/MD.0000000000005344
- Hao F, Yong T, Jianchang C, et al. Research progress in the application of tranexamic acid in the lumbar vertebra surgery. Chin Med Herald. 2017;14:31.
- Hao S, Li H, Liu S, et al. The effect of intravenous unit-dose tranexamic acid on visible and hidden blood loss in posterior lumbar interbody fusion: a randomized clinical trial. Sci Rep. 2023;13(1):4714. doi:10.1038/s41598-022-27307-3
- Kelly M, Turcotte J, Fowler MB, West M, Lashgari C, Gelfand J. Impact of tranexamic acid on clinical and hematologic outcomes following total shoulder arthroplasty. Shoulder Elbow. 2022;14(5):544–550. doi:10.1177/17585732211023053
- Dong W, Liang Y, Li D, et al. The effect of sequential perioperative intravenous tranexamic acid in reducing postoperative blood loss and hidden blood loss after posterior lumbar interbody fusion: a randomized controlled trial. Front Med Lausanne. 2023;10:1192971. doi:10.3389/fmed.2023.1192971
- Girolami A, Cosi E, Ferrari S, Lombardi AM, Girolami B. Prethrombotic, prothrombotic, thrombophilic states, hypercoagulable state, thrombophilia etc.: semantics should be respected even in medical papers. J Thromb Thrombolysis. 2017;43(3):390–393. doi:10.1007/s11239-016-1459-8