Abstract
Purpose
The need to respond to accreditation institutes’ and patients’ requirements and to align health care results with increased medical knowledge is focusing greater attention on quality in health care. Different tools and techniques have been adopted to measure and manage quality, but clinical errors are still too numerous, suggesting that traditional quality improvement systems are unable to deal appropriately with hospital challenges. The purpose of this paper is to grasp the current tools, practices, and guidelines adopted in health care to improve quality and patient safety and create a base for future research on this young subject.
Methods
A systematic literature review was carried out. A search of academic databases, including papers that focus not only on lean management, but also on clinical errors and risk reduction, yielded 47 papers. The general characteristics of the selected papers were analyzed, and a content analysis was conducted.
Results
A variety of managerial techniques, tools, and practices are being adopted in health care, and traditional methodologies have to be integrated with the latest ones in order to reduce errors and ensure high quality and patient safety. As it has been demonstrated, these tools are useful not only for achieving efficiency objectives, but also for providing higher quality and patient safety. Critical indications and guidelines for successful implementation of new health managerial methodologies are provided and synthesized in an operative scheme useful for extending and deepening knowledge of these issues with further studies.
Conclusion
This research contributes to introducing a new theme in health care literature regarding the development of successful projects with both clinical risk management and health lean management objectives, and should address solutions for improving health care even in the current context of decreasing resources.
Introduction
Quality in health care
Society is no longer prepared to accept the number of clinical errors that are reported by the mass media. Nowadays, accreditation requirements, the needs and expectations of patients, and social and ethical values demand continuous improvement in the quality of health care, while maintaining costs the same time.
The literature provides different definitions of quality in health care. These are usually generic or disaggregated, and different features of quality are usually highlighted from the diverse perspectives of stakeholders.Citation1,Citation2
Martin has defined quality as meeting or exceeding predefined standards;Citation3 other authors have described quality as the extent to which the desired health outcomes or the expectations of patients and other customers of health care services are met.Citation4,Citation5 According to the Agency for Healthcare Research and Quality,Citation6 it is doing the right thing at the right time in the right way for the right person and having the best possible results. Based on the work of Spear and BowenCitation7 in an industrial context, Condel et alCitation8 and Printezis and GopalakrishnanCitation9 have added that health care services should be: guaranteed every time, defect-free, and provided in a safe environment at the lowest cost and without waste. In particular, the Agency for Healthcare Research and QualityCitation10 and a report by the Institute of MedicineCitation11 have underscored that to ensure high quality, health care services should be: safe, timely, patient-centered, efficient, effective, and equitable. One of the most cited definitions considers health care quality as the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge”.Citation12
DonabedianCitation13 has recognized that different quality measurement and management systems have to be associated with different definitions of quality, according to different perspectives. In the last two decades, several quality improvement approaches have been implemented in hospitals. However, these have yielded unsatisfactory results, with errors remaining a feature of health care. Such errors are mainly due to the way employees work. Traditional quality improvement initiatives that assume a retrospective and not system-wide approach do not allow proper reduction and prevention of errors. They include quality control, quality assurance, continuous improvement, and six sigma (SS).Citation14–Citation17
VincentCitation18 defined clinical risks as the “dark side” of quality, so to improve quality it is necessary to reduce and/or avoid errors in health care. According to McCulloch et al,Citation19 an error can be defined as any unintended or unexpected incident that could harm one or more patients.
Errors can be divided into the following: sentinel events (that give rise to legal action), adverse events (unfavorable patient outcome, but not severe), no-harm events (affects patients but does not harm them), and near-misses (errors prevented thanks to timely corrective actions, usually through direct observations).Citation20,Citation21 To ensure patient safety, health care structures or processes are needed to reduce the probability of adverse events resulting from exposure to the health care system.Citation17 It is necessary to focus on processes and systems and to implement new practices and barriers using an organization-wide approach.Citation9,Citation22,Citation23 “Errare humanum est” (“to err is human”) and the human condition cannot be changed. However, the conditions under which people work can be changed to help them avoid mistakes, even in complex settings. Verbano and TurraCitation24 and Verbano and VenturiniCitation25 have stated that different tools can be adopted in a clinical risk management (CRM) approach. Others report that systematic methods from the industrial sector could be effective in reducing medical errors, such as total quality management (TQM), quality function deployment, plan do check act (PDCA), zero defects, and lean thinking.Citation26,Citation27 Lean thinking is a philosophy and an organizational way of work; following its recent meaning, it also incorporates SS.Citation8,Citation27
Lean management (LM) principles according to Womack and JonesCitation28 are: precisely specify value, identify the value stream, make value flow without interruptions, pull approach, and continuous improvement pursuing perfection. LikerCitation29 has classified them in a different way, suggesting a 4P model, which includes: problem-solving (continuous improvement), people (respect, challenge, and grow), process (waste elimination), and philosophy (long-term thinking). Some new practices connected to LM that should overcome unsatisfactory results with previous tools are: lean total quality management (LTQM),Citation30 the Henry Ford production system (HFPS),Citation31 lean six sigma (LSS),Citation27,Citation31–Citation33 and the Toyota production system (TPS).Citation9
In health care, the definition given for health lean management (HLM) is:
“A management philosophy to develop a hospital culture characterized by increased patient and other stakeholder satisfaction through continuous improvements, in which all employees (managers, physicians, nurses, laboratory people, technicians, office people etc) actively participate in identifying and reducing non-value-adding activities (waste).”Citation34
HLM practices were originally adopted mainly to improve efficiency, but they have the potential to improve quality and reduce errors, decrease time and costs, increase staff productivity, and improve patient outcomes and employee and customer satisfaction.Citation27
HLM, in fact, could be described as a managerial approach for identifying and eliminating waste while improving the flow of activities to maximize customer value.Citation35,Citation28 It includes standardization and specification of work processes and organization in such a way that unexpected events can be spotted and activities that find and fix mistakes can be developed. Within these mistakes, clinical errors could be included, but, most of all, HLM can be used for clinical process analysis, which is necessary for detecting clinical risks, and tools and practices of HLM could also contribute to reducing errors (eg, use of mistake proofing [poka-yoke], 5S, and so on, could create a context that prevents risks of harm). HLM could be a way of reducing costs while maintaining high levels of patient safety and quality, eliminating any of the typical waste that we find in hospitals, such as overproduction, overprocessing, transportation, inventory, movement, waiting times, and defective products.Citation36–Citation38
The need for improved performance is the result of the hospital funding crisis, spending reviews, and increasing health care costs, mainly due to an aging population, the use of more advanced technologies, the lack of cost-containment measures, inefficiencies, and medical errors.Citation9,Citation39–Citation43 Kumar and SteinebachCitation44 have recognized the direct costs (higher health care expenditures) and indirect costs (lower productivity, disability, and personal care) of poor quality. Others have noted that poor quality has financial implications and leads to low patient trust and low staff and patient satisfaction.Citation9 Some authors have emphasized that quality improvement can offer financial benefits for the whole health system.Citation43,Citation45 The adoption of HLM and other managerial tools and practices could be useful for achieving these results.
Based on the aforementioned issues, the purpose of this paper is to investigate the new practices and the key critical factors adopted and suggested in the literature not only to reduce costs, but also to ensure a high level of quality and safety. In particular, two main purposes will be pursued:
To give an overview of the managerial techniques, tools, and practices adopted for the implementation of projects connecting, even partially, HLM and CRM.
To grasp from the literature review the key critical factors that have to be considered for successful implementation of HLM projects that have an impact on CRM.
The intention of this work is to draw up potential/hypothetical guidelines from the literature review to be tested and, if necessary, integrated into future studies, conducting empirical research in the field.
Methods
In order to achieve the aims described in the previous section, a systematic review of the literature was conducted, drawing on current methodologies.Citation46–Citation49 and answering the question: what are the tools, practices, and key critical factors needed to successfully implement HLM, stressing safety performance? In addition, our intention is to provide directions for fruitful future research.
The protocol for the systematic literature review included the following steps: a) conceptual discussion of the problem, b) definition of the literature review objective, c) search strategy, d) paper selection criteria, e) single-paper analysis, f) description of the main characteristics of the extracted papers, and f) synthesis of interesting content and lessons learned.
The academic databases searched were: Business Source Premier (EBSCO), Compendex (Ei Village 2), Inspec (Ei Village 2), Web of Science (ISI), and PubMed. The keywords employed are reported in the second column of , which also presents the selection criteria for the papers and the results of the search strategy. In particular, research was carried out by two researchers that followed the same steps. After cutting out any duplications and reading the title and the abstract of the papers, each researcher, working independently, eliminated papers that did not consider managerial aspects or LM. Papers that did not go in depth (eg, opinion papers, lecture notes, papers of 2–3 pages) were not included in the analysis. Following the context, interventions, mechanisms and outcomes (CIMO) logic suggested by Denyer et alCitation48 for organization and management research, after the full reading of articles, other papers were deleted from the database. The context of the research is a hospital, so papers not focusing on this context were excluded and, according to the purpose of the research, only papers that analyzed lean health care and its relationship with patient safety (for example in defining objectives or analyzing results obtained) were included in order to study the adopted interventions and mechanisms and the achieved outcomes (IMO).
Table 1 Search strategy and paper selection
In the single-paper analysis, the following was recorded: citations, authors, title of the paper, year, keywords, principal theme, name of the journal, impact factor and H-index of the journal, research methodology, aim of the paper, results, authors’ backgrounds, context of applicability, notes about key concepts, number of authors, and country where the study was conducted. Papers were examined based on their descriptive characteristics, and content analysis was then conducted to identify the main issues and lessons learned in the existing literature.
shows the main characteristics of the papers included in the review. Most of the papers had more than one author, and all the journals but one had an H-index greater than 8, even if not all of them were present in the ISI list. With respect to the workplace of the first author, most of the papers were from the US (78%), followed by the UK (9%) and Sweden (4%). With regard to the year of publication, a positive trend emerged: 13% of the papers were published from 2004 to 2005, 17% from 2006 to 2007, 24% from 2008 to 2009, and 46% from 2010 to 2013. As for the adopted methodology, most of the papers conducted case or action research (63%); there was just one simulation and no surveys. Literature reviews were included as they study previous experiences and/or because they give new suggestions for future research that could be useful, considering the scope of this research. Regarding the context of applicability, 67% of papers focused only on a single unit or department of a hospital (mostly laboratory department, emergency department, radiology and gynecology departments), 24% studied a hospital as a whole (HG), 7% analyzed a single care process (PC), and 2% dealt with the collaboration and the alignment between the emergency department and other areas of a hospital.
Table 2 Characteristics of the selected papers
Content analysis of previous studies
In , the main purposes of the papers, the tools and practices considered, and the benefits of their application are reported. Managerial tools and practices are categorized as follows:
Table 3 Purposes of the papers, tools, practices, and benefits
– Information and communication technologies (ICT), including, for example, pathology informatics, electronic medical records (EMR), optical character recognition, 24-hour hotlines, web-based reporting systems, new tools for communication and teamwork, online medication ordering systems, and decision-support systems (DSS), such as event monitoring, alarms and alerts systems, “andon”, patient safety alerts, and decision-making models.
– Process management. These tools and practices are classified according to the phases where they are usually adopted: understanding and mapping (eg, value stream analysis), planning (eg, hoshin planning, “to be” map, corrective action plan), standardization and specification (eg, instructions and guidelines, standardized reporting, and nomenclature), improvement (eg, rapid improvement events, kaizen, 5S), and monitoring and control (eg, visual control, weekly audit, management dashboards).
– Quality management, including indicators of quality, quality control, quality assurance, use of six sigma and define, measure analyze, improve, and control (DMAIC), quality management systems (QMS), continuous quality improvement programs, total quality management (TQM) practices, quality function deployment/house of quality (QFD/HOQ), and ISO 9000.
– Compliance consists of auditing to monitor the results of compliance, and adopting well-accepted guidelines, universal protocols.
– Error management. These tools and practices are classified according to four phases: identification (eg, error reporting and error detection system, error documentation, error inspection), analysis (eg, RCA, FMEA, risk assessment tool, 5 whys, Ishikawa diagram, etc), prevention and correction (eg, poka-yoke, stop the line), and monitoring and control (eg, error audit and feedback).
– People and culture, including use of an adequate team, black belt/consultant, employee training and education, lean facilitator and sensei (clinical champions), trystorming and brainstorming, learning organization, involvement and empowerment, employee satisfaction, top management commitment and support, development of the right culture and philosophy, and human quality management (model of behavior change).
– Customer/patient management. These tools and practices refer to the valorization of patients (add value, maximizing value for customer), customer-supplier connections and communication, complaints management, early patient involvement, and patient education.
Most of the analyzed papers aimed to describe the implementation of new managerial techniques and methodologies applied in health care, with the main purpose of achieving high quality and patient safety by improving workflows and efficiency and reducing errors. shows the objectives, tools, and practices considered and the benefits of the research. It underscores that techniques relating to process management are always adopted, especially for process understanding and mapping (87% of papers), and that different LM tools are used for process improvement. Within the area of people and culture, team building, employee education, and culture are also emphasized, while ICT is often adopted as a support instrument. The benefits obtained mostly relate to higher productivity and efficiency, a reduced amount of time spent in executing activities, reduced costs, improved accuracy, and fewer errors.
In , it can be observed that in all cases tools and practices of the process management type are used (100% of papers). Also widely used are those of the people and culture category (89%), followed by error management (72%), quality (54%), and ICT and DSS (48%).
Table 4 Category of tools and practices adopted in literature per field of applications considered in literature
Moreover, it is interesting to observe that error management techniques are frequently used in hospitals as a whole, laboratory units, and emergency departments, while quality management tools and practices are mostly used in laboratory units and when the focus is the whole hospital. ICT and DSS are used in preference if the focus is the whole hospital. Finally, customer/patient management tools are much used practices when focusing on emergency departments.
Discussion
This review has highlighted critical factors in planning and implementing safe, lean projects, meaning process improvement projects, following an HLM approach and stressing safety performance, in addition to traditional cost and time benefits. These critical factors have been identified examining recurrent lessons learned from the reviewed literature. They are detailed in four categories as follows:
Culture, organization, and communication. Before starting a lean project, it is important to overcome resistance by developing an appropriate organizational climate and culture. Resistance can be surmounted by adopting models of behavior change. The hierarchical blame and shame culture should be replaced with one of safety and continuous improvement, and developing a learning organization. Staff have to be improved through education, training, motivation, involvement, empowerment, and valorization. An appropriate multidisciplinary team should be built and facilitators, champions, sponsors, and change agents should be identified.
Furthermore, changes should be implemented by employees identifying leaders and problem solvers inside the health care organization, with scholars, consultants, experts, and external stakeholders being involved as key collaborators. In addition, instead of focusing on short-term results, a long-term perspective should be adopted, with the aim of developing a culture of quality and safety reporting and continual and structured problem-solving that avoids a quick-fix mentality. HLM can be applied at all levels, but benefits for the whole organization will be achieved when it is applied at a strategic level. The HLM approach should be aligned with the hospital’s strategy and values. The ethics and culture of professionals should be consistent with those of the organization. To achieve successful outcomes, clear, consistent, direct, multidimensional, and frequent communication should take place among providers and between patients and providers, creating a climate of transparency and honesty. To obtain satisfactory results, the top management needs to provide commitment and support. The leadership of individuals appropriately trained and with the right culture is also paramount.
Process management (PM). With respect to PM, a systematic and proactive approach should be adopted, including the following phases: understanding (each step and task should be described with all competencies, standards of performance), managing, improving (usually changing the process design, standardizing, and specifying), and controlling to prevent system failures. It is also important to valorize the planning phase. Most problems are the result of system design issues. These can be solved through improved and simplified process redesign, with better connections and QMS, highlighting problems in real time and continually striving to understand their root causes, solving them immediately and adopting a system-wide approach. HLM can help enhance the ability to identify changes needed, especially with regard to policies and practices, in order to implement and sustain the desired quality improvements. Tools and practices connected with PM contribute to reducing errors and variations, in addition to improving the operational performance, effectiveness, and efficiency of clinical processes.
Error management (EM). The literature provides useful indications for EM. First, risks should be detected and then prevented by revising the risk-assessment process and developing a prevention strategy that should give priority to basic and cost-effective preventive care, instead of therapy care, following LSS and common sense. The tools need to focus mostly on the identification, prevention, and mitigation of errors. In particular, mechanisms of error detection are important because they increase awareness and process reliability. To better detect risks and errors, everyone should be involved (including families of patients) in safety and quality reporting, and a culture of proactive error reduction with double checks should be developed.
Patient/customer management. Focusing on adding and creating value for patients and listening to patients’ voices are fundamental for overcoming resistance to changes. The implementation of HLM differs, depending on how the customer and customer value are defined. However, the most important point is that the customer-supplier connection should not be ambiguous and that the response to the customer has to be on-demand, defect-free, one-by-one, waste free, immediate, and safe.
Other guidelines that support these four categories deserve to be underscored:
Quality management has to become integral,Citation17 and HLM should be adopted to improve quality, rather than lower costs, following the patients’ view of quality;Citation23,Citation68,Citation76
the adoption of ICT and DSS can support PM in all its phases; for example, in computerized physician ordering systems, barcoding, timeline monitoring systems, patient or specimen tracking, patient identification, and EMR databases.Citation26,Citation31,Citation44,Citation50,Citation53,Citation54,Citation56–Citation58,Citation61,Citation65,Citation70,Citation71,Citation74,Citation78 According to Sloane and Gehlot,Citation71 ICT and some simulation tools should become a routine part of risk management. Moreover, robust data mining environments should be created and the use of ICT should be enlarged, as these could facilitate patient safety and error reduction and support the measurement of HLM effectiveness.Citation21,Citation26,Citation50,Citation65 However, investments in new technologies and automation should be considered only after process redesign.Citation33,Citation66,Citation67
Several authors have highlighted that positive results could be attributed to the Hawthorne effect.Citation19,Citation22,Citation56,Citation63,Citation74 This is a temporary effect due to participation in the studies of particular contexts, as Wickström and BendixCitation79 have discussed in depth. However, Raab et alCitation67 have asserted that it is possible to achieve sustained improvements with HLM. To ensure sustainability and successful implementation of projects, the following key steps should be addressed: setting a focused aim, articulating time frames, identifying measurable goals, and following a properly planned iterative approach.Citation26,Citation73,Citation59 Furthermore, new processes should be implemented in off-peak times, and interventions should be executed following a logical sequence.Citation63 Periodically reviewing metrics leads to long-term sustainability.Citation26 More research is needed using appropriate and consistent metrics to understand and measure the impact of HLM on quality, patient safety, and employee satisfaction and wellbeing.Citation19,Citation21,Citation56,Citation62,Citation76
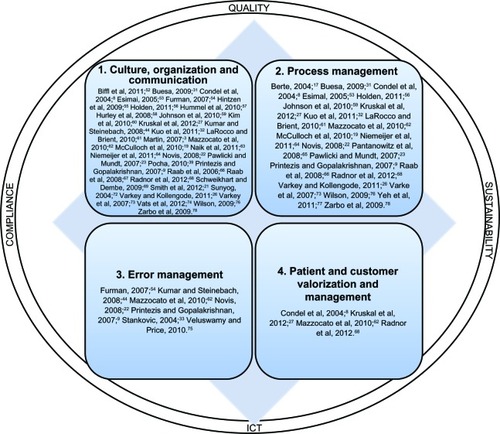
depicts the four main categories of guidelines with their associated references for critical factors and the supporting areas.
Conclusion
The purpose of this paper was to describe the techniques, tools, and practices adopted in health care to improve quality and patient safety and reduce costs and errors. The results of the literature review demonstrate that a variety of managerial tools are being implemented to achieve these aims. Traditional methodologies are accompanied by ongoing quality control and quality assurance, as well as proactive quality improvement and process improvement approaches, such as SS and LM. All these techniques should be implemented, together with others, such as TQM, and supported by ICT to reduce errors and ensure high quality and patient safety.Citation20,Citation30,Citation65,Citation73
In all the papers considered, tools and practices are being adopted for process man agement, especially for understanding and mapping processes. It is interesting to also underscore the widespread use of tools and practices of error management. According to some scholars, HLM implementation should be reported, and the results should be disseminatedCitation14,Citation22,Citation56 because positive and negative results and details of the implementation in various sectors can suggest and drive replications in other organizations.Citation56,Citation62,Citation72,Citation74 In addition, factors that lead to positive changes or failures and contextual factors should be studied in depth.Citation21,Citation62 Some authors doubt whether HLM can be appreciated and replicated in other departments or organizations; an appropriate adaptation should be outlined. However, application of HLM stimulates discussion about how to solve system and process issues and improve quality and patient safety.Citation22,Citation60,Citation68,Citation74 Most of the analyzed papers have underscored the limits of HLM and barriers to its implementation,Citation9,Citation21,Citation31,Citation32,Citation39,Citation52,Citation54,Citation56,Citation57,Citation60,Citation62,Citation63,Citation65,Citation66,Citation68,Citation78 demonstrating that HLM can not be successfully implemented without considering the proper critical factors and precautions highlighted in the previous section of this paper.
In conclusion, the guidelines that have emerged from this research concern (): 1) culture, organization, and communication; 2) process management; 3) error management; and 4) customer/patient management and the issues that support it, such as ICT, quality, sustainability, and compliance.
This literature review has analyzed the main research efforts that have considered aspects of both HLM and CRM, providing references to key published works worldwide. The results from these studies were employed to provide an overview of the managerial practices and tools used to overcome current managerial health care challenges and the critical factors that must be considered for successful implementation of safety and lean projects. Starting from the key concepts and indications highlighted in this paper ( and ), both future research (conducted by academics) and safety and lean projects in a health care context (conducted by managers) should be developed.
Although the current study provides an important contribution to the field, the available knowledge of its issues is insufficient at this early stage, and practical and academic studies are still limited. Despite the proposed guidelines should be further tested with empirical research, they suggest potential tools, practices, and critical factors to be considered to achieve successful implementation of lean and safety projects, as they emerged from literature analysis. Future research should further test, formalize, and develop knowledge and experience in the field to determine the potential synergy between HLM and CRM, developing in depth the reference scheme in and defining operative guidelines. In particular, the next steps suggested for future studies are to:
– map other experiences in the field in order to understand which tools, practices, and critical analyses are being considered, validating and integrating the guidelines proposed in this research;
– a larger database of previous experiences should permit analysis and verification in a quantitative way of the connections between objectives, tools, and results, also expanding the context of applications (other organizational units, care process, etc);
– develop indicators and measures that should be adopted to evaluate the costs and quality results obtained after the implementation of projects;
– investigate the possibility of creating a comprehensive synergic methodology that combine the benefits of HLM and CRM.
Future developments based on the indications and lessons developed from this literature review could provide solutions to help society obtain a higher level of health care in today’s difficult economic and political climate of decreasing resources.
Disclosure
The authors report no conflicts of interest in this work.
References
- CampbellSMRolandMOBuetowSADefining quality of careSoc Sci Med200051111611162511072882
- BlumenthalDPart 1: quality of care – what is it?N Engl J Med1996335128918948778612
- MartinWSpecial report: quality of care survey. Quality models: selecting the best model to deliver resultsPhysician Exec2007333243117539559
- LaffelGBlumenthalDThe case for using industrial quality management science in health care organizationsJAMA198926220286928732810623
- LohrKNDonaldsonMSHarris-WehlingJMedicare: a strategy for quality assurance, V: Quality of care in a changing health care environmentQRB Qual Rev Bull19921841201261630793
- Agency for Healthcare Research and QualityTestimony on Health Care QualityRockvilleAHRQ Publications1997 Available from: http://archive.ahrq.gov/news/test1028.htmAccessed May 10, 2013
- SpearSBowenHKDecoding the DNA of the Toyota production systemHarv Bus Rev19997796108
- CondelJLSharbaughDTRaabSSError-free pathology: applying lean production methods to anatomic pathologyClin Lab Med200424486589915555747
- PrintezisAGopalakrishnanMCurrent pulse: can a production system reduce medical errors in health care?Qual Manag Health Care200716322623817627218
- Agency for Healthcare Research and QualityNational Health Care Disparities ReportRockvilleAHRQ Publications2011 Available from: http://www.ahrq.gov/research/findings/nhqrdr/nhqr11/nhqr11.pdfAccessed May 10, 2013
- Institute of MedicineCrossing the Quality Chasm: A New Health System for the 21st CenturyWashingtonNational Academy Press2001
- LohrKNMedicare: A Strategy for Quality Assurance Volume IWashingtonNational Academies Press1990
- DonabedianAThe quality of care. How can it be assessed?JAMA199926012174317483045356
- HerringLLean experience in primary careQual Prim Care200917427127519807960
- National Priorities PartnershipNational Priorities and Goals: Aligning our Efforts to Transform America’s HealthcareWashingtonNational Quality Forum2008
- SchwappachDLFrequency of and predictors for patient-reported medical and medication errors in SwitzerlandSwiss Med Wkly2011141w1326221971822
- BerteLMPatient safety: getting there from here – quality management is the best patient safety programClin Leadersh Manag Rev200418631131515597551
- VincentCRisk, safety, and the dark side of qualityBMJ19973147097177517769224069
- McCullochPKrecklerSNewSSheenaYHandaACatchpoleKEffect of a “Lean” intervention to improve safety processes and outcomes on a surgical emergency unitBMJ2010341c546921045024
- StankovicAKThe laboratory is a key partner in assuring patient safetyClin Lab Med20042441023103515555754
- SmithMLWilkersonTGrzybickiDMRaabSSThe effect of a lean quality improvement implementation program on surgical pathology specimen accessioning and gross preparation error frequencyAm J Clin Pathol2012138336737322912352
- NovisDAReducing errors in the clinical laboratory: a lean production system approachLab Med2008399521529
- PawlickiTMundtAJQuality in radiation oncologyMed Phys20073451529154017555234
- VerbanoCTurraFA human factors and reliability approach to clinical risk management: evidence from Italian casesSafety Sci2010485625639
- VerbanoCVenturiniKDevelopment paths of risk management: approaches, methods and fields of applicationJournal of Risk Research2011145519550
- VarkeyPKollengodeAA framework for healthcare quality improvement in India: the time is here and now!J Postgrad Med201157323724121941069
- KruskalJBReedyAPascalLRosenMPBoisellePMQuality initiatives: lean approach to improving performance and efficiency in a radiology departmentRadiographics201232257358722323617
- WomackJPJonesDTLean Thinking: Banish Waste and Create Wealth in your CorporationNew YorkFree Press2003
- LikerJKThe Toyota WayNew YorkMcGraw-Hill2004
- DasBValidation protocol: first step of a lean-total quality management principle in a new laboratory set-up in a tertiary care hospital in IndiaIndian J Clin Biochem201126323524322754186
- BuesaRJAdapting lean to histology laboratoriesAnn Diagn Pathol200913532233319751909
- KuoAMBoryckiEKushnirukALeeTSA healthcare Lean Six Sigma System for postanesthesia care unit workflow improvementQual Manag Health Care201120141421192203
- StankovicAKDiLauriEQuality improvements in the preanalytical phase: focus on urine specimen workflowClin Lab Med2008282339350viii18436075
- DahlgaardJJPettersenJDahlgaard-ParkSMQuality and lean health care: A system for assessing and improving the health of healthcare organisationsTotal Quality Management and Business Excellence2011226673689
- OhnoTToyota Production System: Beyond Large-Scale ProductionPortlandProductivity Press1988
- Institute for Healthcare ImprovementGoing Lean in Health Care. IHI Innovation Series White PaperCambridgeInstitute for Healthcare Improvement2005 Available from: http://www.entnet.org/Practice/qualityimprovement/upload/GoingLeaninHealthCareWhitePaper-3.pdfAccessed August 7, 2013
- BushRWReducing waste in US health care systemsJAMA2007297887187417327529
- JimmersonCWeberDSobekDKReducing waste and errors: piloting lean principles at Intermountain HealthcareJt Comm J Qual Patient Saf200531524925715960015
- PochaCLean Six Sigma in health care and the challenge of implementation of Six Sigma methodologies at a Veterans Affairs Medical CenterQual Manag Health Care201019431231820924252
- BodenheimerTHigh and rising health care costs. Part 1: seeking an explanationAnn Intern Med20051421084785415897535
- BarclaysUK healthcare. Sector outlook. Third quarter 2012LondonBarclays Bank PLC2012 Available from: http://www.barclayscorporate.com/content/dam/corppublic/corporate/Documents/sector_expertise/healthcare_outlook.pdfAccessed June 11, 2013
- OECDHealth at a Glance Europe 2012OECD Publishing2012 Available from: http://ec.europa.eu/health/reports/docs/health_glance_2012_en.pdfAccessed May 9, 2013
- MarshallMØvretveitJCan we save money by improving quality?BMJ Qual Saf2011204293296
- KumarSSteinebachMEliminating US hospital medical errorsInt J Health Care Qual Assur200821544447118785345
- ØvretveitJDoes Improving Quality Save Money? A Review of Evidence of which Improvements to Quality Reduce Costs to Health Service ProvidersLondonThe Health Foundation2009
- DenyerDTranfieldDProducing a Systematic ReviewThe SAGE handbook of organizational research methodsBuchananDABrymanALondonSAGE Publications Ltd2009670689
- PawsonREvidence-Based Policy: A Realist PerspectiveLondonSAGE Publications Ltd2006
- DenyerDTranfieldDVan AkenJEDeveloping design propositions through research synthesisOrgan Stud2008293393413
- BreretonPKitchenhamBABudgenDTurnerMKhalilMLessons from applying the systematic literature review process within the software engineering domainJ Syst Software2007804571583
- BecichMJGilbertsonJRGuptaDPatelAGrzybickiDMRaabSSPathology and patient safety: the critical role of pathology informatics in error reduction and quality initiativesClin Lab Med2004244913943vi15555749
- BenitezYForresterLHurstCTurpinDHospital reduces medication errors using DMAIC and QFDQual Prog20074013845
- BifflWLBenoMGoodmanP“Leaning” the process of venous thromboembolism prophylaxisJt Comm J Qual Patient Saf20113739910921500752
- EsimaiGLean six sigma reduces medication errorsQual Prog20053845157
- FurmanCCaplanRApplying the Toyota Production System: using a patient safety alert system to reduce errorJt Comm J Qual Patient Saf200733737638617711139
- HintzenBLKnoerSJVan DykeCJMilavitzBSEffect of lean process improvement techniques on a university hospital inpatient pharmacyAm J Health Syst Pharm200966222042204719890089
- HoldenRJLean Thinking in emergency departments: a critical reviewAnn Emerg Med201157326527821035904
- HummelJEvansPCLeeHMedication reconciliation in the emergency department: opportunities for workflow redesignQual Saf Health Care201019653153520554575
- HurleyBLevettJMHuberCTaylorTLUsing lean six sigma® tools to compare INR measurements from different laboratories within a communityQuality management in health care2008201415
- JohnsonCDMirandaRAakreKTRobertsCCPatelMDKreckeKNProcess improvement: what is it, why is it important, and how is it done?AJR Am J Roentgenol2010194246146820093610
- KimCSLukelaMPParekhVITeaching internal medicine residents quality improvement and patient safety: a lean thinking approachAm J Med Qual201025321121720357082
- LaRoccoMBrientKInterdisciplinary process improvement for enhancing blood transfusion safetyJ Healthc Qual2010322293420364648
- MazzocatoPSavageCBrommelsMAronssonHThorJLean thinking in healthcare: a realist review of the literatureQual Saf Health Care201019537638220724397
- NaikTDuroseauYZehtabchiSA structured approach to transforming a large public hospital emergency department via lean methodologiesJ Healthc Qual2011342869722188582
- NiemeijerGCDoesRJde MastJTripAvan den HeuvelJGeneric project definitions for improvement of health care delivery: a case-based approachQual Manag Health Care201120215216421467902
- PantanowitzLHornishMGoulartRAInformatics applied to cytologyCytojournal200851162719495402
- RaabSSAndrew-JajaCCondelJLDabbsDJImproving Papanicolaou test quality and reducing medical errors by using Toyota production system methodsAm J Obstet Gynecol20061941576416389010
- RaabSSAndrew-JajaCGrzybickiDMDissemination of Lean methods to improve Pap testing quality and patient safetyJ Low Genit Tract Dis200812210311018369303
- RadnorZJHolwegMWaringJLean in healthcare: the unfilled promise?Soc Sci Med201274336437121414703
- SchweikhartSADembeAEThe applicability of Lean and Six Sigma techniques to clinical and translational researchJ Investig Med2009577748755
- SerranoLHeggePSatoBRichmondBStahnkeLUsing LEAN principles to improve quality, patient safety, and workflow in histology and anatomic pathologyAdv Anat Pathol201017321522120418676
- SloaneEBGehlotVUse of coloured petri net models in planning, design, and simulation of intelligent wireless medical device networks for safe and flexible hospital capacity managementIJNVO200742118129
- SunyogMLean Management and Six-Sigma yield big gains in hospital’s immediate response laboratory. Quality improvement techniques save more than $400,000Clin Leadersh Manag Rev200418525525815493100
- VarkeyPRellerMKResarRKBasics of quality improvement in health careMayo Clin Proc200782673573917550754
- VatsAGoinKHVillarrealMCYilmazTFortenberryJDKeskinocakPThe impact of a lean rounding process in a pediatric intensive care unitCrit Care Med201240260861721983366
- VeluswamyRPriceRI’ve fallen and I can’t get up: reducing the risk of patient fallsPhysician Exec2010363505320499522
- WilsonGImplementation of Releasing Time to Care – the productive wardJ Nurs Manag200917564765419575723
- YehHLLinCSSuCTWangPCApplying lean six sigma to improve healthcare: An empirical studyAJBM20115311235612370
- ZarboRJTuthillJMD’AngeloRThe Henry Ford Production System: reduction of surgical pathology in-process misidentification defects by bar code-specified work process standardizationAm J Clin Pathol2009131446847719289582
- WickströmGBendixTThe “Hawthorne effect” – what did the original Hawthorne studies actually show?Scand J Work Environ Health200026436336710994804