 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Prone positioning for breast radiotherapy is preferable when the aim is a reduction of the dose to the ipsilateral lung or the heart in certain left-sided cases.
Materials and methods
In 100 breast cancer cases awaiting postoperative whole-breast radiotherapy, conformal radiotherapy plans were prospectively generated in both prone and supine positions. The axillary nodal region (levels I–III) and internal mammary (IM) lymph-node region in the upper three intercostal spaces were retrospectively contoured. The mean doses to the nodal regions and the volume receiving 25 Gy (V25Gy), V45Gy, and V47.5Gy were compared between the two treatment positions.
Results
In most cases, the doses to axillary levels I–III and the IM lymph nodes were inadequate, regardless of the treatment position. The nodal doses were significantly lower in the prone than in the supine position. The radiation doses to levels II–III and IM nodes were especially low. The V45Gy and V47.5Gy of the level I axillary lymph nodes were 54.6% and 40.2%, respectively, in the supine, and 3.0% and 1.7%, respectively, in the prone position. In the supine position, only 17 patients (17%) received a mean dose of 45 Gy to the axillary level I nodes.
Conclusion
The radiation dose to the axillary and IM lymph nodes during breast radiotherapy is therapeutically insufficient in most cases, and is significantly lower in the prone position than in the supine position.
Background
Prone breast radiotherapy is being increasingly utilized in consequence of its favorable effects on the dose to the organs at risk (OARs), such as the ipsilateral lung and the heart in left-sided cases.Citation1–Citation5 All patients with right-sided breast cancer benefit from prone positioning because of the dramatic reduction in the ipsilateral lung dose, and at least 60% of patients with left-sided breast cancer benefit from lower dose to the heart and/or left anterior descending coronary artery.Citation1–Citation3,Citation5 Prone breast radiotherapy has proved feasible, and may be performed with good repositioning accuracy.Citation3,Citation6,Citation7 Breast radiotherapy in either the prone or the supine position ensures good coverage of the operated breast, and similar dose homogeneity.Citation3,Citation4,Citation8 Prone breast radiotherapy provides a long-term outcome (local/regional control and toxicity) similar to that of treatment in the supine position.Citation9
The radiotherapy of regional lymph nodes contributes to improved relapse-free and overall survival in patients with axillary lymph node-positive breast cancer.Citation10–Citation12 The extent of survival benefit has been found by the Danish Breast Cancer Group to be similar in one to three and four or more lymph node-positive cases.Citation12 In sentinel lymph node-positive patients, the role of radiotherapy has not been fully clarified. The noninferiority of whole-breast radiotherapy versus complete axillary block dissection plus breast radiotherapy in cases with one to two positive sentinel lymph nodes was demonstrated in the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial.Citation13 Equal local and regional control rates have been ascribed to the irradiation of the level I axillary lymph nodes,Citation13,Citation14 though no solid data exist as yet to support this hypothesis. The extent to which the patients in the ACOSOG studyCitation13 received nodal radiotherapy is currently undergoing retrospective evaluation. The management of internal mammary (IM) nodes is controversial.Citation15 In axillary node-positive cases, the risk of IM-node involvement increases significantly with the number of positive lymph nodes. The role of IM nodal irradiation in these high-risk patients, however, is still a subject of ongoing large randomized multicenter (European Organisation for Research and Treatment of Cancer [EORTC] and National Cancer Institute of Canada [NCIC]) trials.Citation16,Citation17 Approximately a quarter of the sentinel nodes are located in the IM chain, but their routine removal is not widely practised.Citation18 Elective irradiation of the IM chain after sentinel biopsy may seem justified in rare cases.Citation19,Citation20 As the need to irradiate the nodal regions varies individually, careful control of the nodal dose is important in each case. A number of research groups have demonstrated that the dose to the axillary or sentinel lymph-node areas during supine breast irradiation with tangential fields is usually insufficient “therapeutically”.Citation21–Citation26 In the prone position, the axillary nodal doses are further decreased.Citation21,Citation22
In this retrospective study, the goal was to analyze the radiation dose to the nodal regions, including the axillary and IM nodes, in a large set of 3-D conformal radiotherapy plans generated for whole-breast irradiation in either the prone or supine position.
Materials and methods
This retrospective study was based on the 3-D conformal radiotherapy plans of 100 consecutive breast cancer patients requiring radiotherapy of the operated breast. The patients had been included in a clinical study approved by the Institutional Review Board of the University of Szeged to investigate the effects of patient-related anatomic features on optimal positioning (prone versus supine) in left-sided breast cancer.Citation4
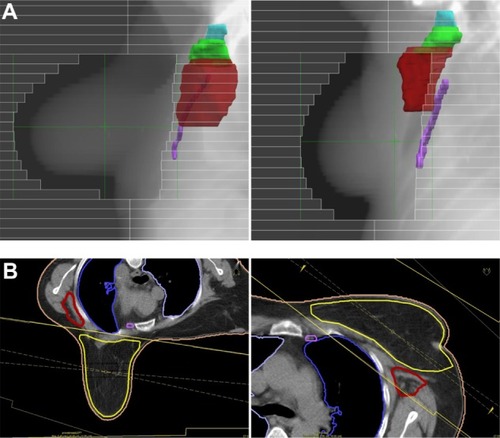
All relevant technical details have been published previously.Citation3,Citation4 Briefly, computed tomography (CT) images were acquired at 0.5 cm intervals throughout the entire planning volume. The target volume and OARs were contoured on the CT slices in the radiotherapy-planning system. The clinical target volume (operated breast) was contoured at the chest wall: breast parenchyma interface, 4 mm from the skin, cranially from the head of the clavicle, medially from the border of the sternum, and laterally and caudally from where the visible breast parenchyma and connective tissue verge. 3-D image reconstruction was used to check delineation. Planning target volumes (PTVs) were generated as described in Varga et al.Citation4 The level I–III axillary and ipsilateral IM lymph-node regions were retrospectively contoured according to the Radiation Therapy Oncology Group (RTOG) contouring atlas,Citation27 as shown in . IM nodes were contoured in the upper three intercostal spaces, with typically 18 slices being taken. The aim in either setup was equivalent target and nodal volume contouring.
Figure 1 (A and B) Left-sided whole-breast irradiation. (A) Beam’s eye view of the right anterior oblique field, with 3-D reconstruction of axillary levels I–III and internal mammary lymph-node regions in the prone and supine positions. (B) Typical field arrangements and their relation to the node regions.
CT-based 3-D treatment planning (XIO® version 4.2.0 convolution algorithm for photon-dose calculation; Elekta, Stockholm, Sweden) was performed in both the supine and prone positions, as detailed previously.Citation3,Citation4 Treatment plans were developed by applying conventional 6 MV tangential photon fields set up isocentrically, and a median of two (one to three) individually weighted 6/15 MV segmental fields superimposed on the tangential fields by using a multileaf collimator. All plans were generated by the same physicist (ZV) with the intent of ensuring similar coverage and dose homogeneity. A mean dose to the PTV of 50 Gy was aimed for.
For analysis of the dose distribution, the volume receiving 95%–107% of the total dose (V95%–107%), the doses received by 5% and 95% of the PTV (D5%/D95%), and the conformation number were calculated using the following equation:
where TV is target volume, ie, PTV, TVRI is the target volume covered by the reference isodose, and VRI is the volume of the reference isodose.Citation28
As regards the doses to the individual nodal regions, the mean doses and the volumes receiving >25 Gy (V25Gy), >45 Gy (V45Gy), and >47.5 Gy (V47.5Gy) were evaluated retrospectively. For the analysis of the relation between the anatomical features of the patient and dose to nodal regions, the PTV, body mass index (BMI), volume of level I axillary lymph-node region, and breast separationCitation3 were registered. The mean dose, V25Gy, V45Gy, and V47.5Gy of axillary level I and the homogeneity and conformity indices of the target volumes were compared in the prone versus supine position by using paired-sample t-tests.
Results
One hundred pairs of treatment plans were analyzed. The volumes of the treated breast, axillary levels I–III, and IM nodes are indicated in . No significant differences in the respective volumes were found between the prone and supine positions. The dose homogeneity within the PTV was better in the supine position: V95%–107% mean ± standard error was 89.08%±0.14% versus 91.92%±0.18% in the prone versus supine position (P<0.001); D5%/D95% (mean ± standard error) was 1.17±0.01 versus 1.13±0.01 in the prone versus supine position. Doses to the OARs were similar to those published previously for the whole study population.Citation4
Table 1 Volumes of the irradiated breast (PTV) and the nodal regions in the prone and supine positions
In most cases, doses to axillary levels I–III and the IM lymph nodes were insufficient, regardless of the treatment position. The doses were significantly lower in the prone than in the supine position ( and ). The radiation doses to levels II and III and the IM nodes were especially low. The V45Gy and V47.5Gy of the level I axillary lymph nodes were 54.6% and 40.2%, respectively, in the supine, and 3.0% and 1.7%, respectively, in the prone position. The number of patients who received a mean dose of ≥45 Gy to the level I axillary lymph nodes in the supine position was 17 (17%). No difference was found in the anatomical features of those whose axillary level I dose was higher or lower than 45 Gy (PTV, 1,073.3 versus 945.5 cm3; BMI, 28.6 versus 28.1 kg/m2; volume of level I axillary lymph-node region, 63.3 versus 62.5 cm3; breast separation, 22.3 versus 21.4 cm; respectively). None of the patients received ≥45 Gy to the other lymph-node regions.
Table 2 Mean doses to the nodal regions in the prone and supine positions
Table 3 Dosimetric values in the nodal regions in the prone and supine positions (P<0.001)
Discussion
Our results clearly reveal that the radiation dose to the axillary and IM lymph nodes during whole-breast irradiation is therapeutically insufficient in most cases, and is significantly lower in the prone position than in the supine position.
In certain situations, such as sentinel and/or axillary lymph-node and lymphovascular invasion negativity, irradiation of the lymph-node areas may obviously be neglected. In other cases, however, the benefit of complete or partial nodal irradiation should be considered. In sentinel lymph node-positive cases, the probability that further positive regional lymph nodes are present varies with the nature of the primary tumor (size, grade, hormone-receptor status, and the presence of multifocality or lymphovascular invasion) and the number/rate of positive sentinel nodes. Nomograms utilizing the aforementioned tumor-related data are available for estimation of the involvement of the axillary lymph nodes.Citation29 Rarely, the lymph-node status remains unknown. If the risk of axillary lymph-node positivity is high, complementary local treatment, such as axillary block dissection or regional irradiation, is justified in order to eradicate persistent regional disease. In such cases, an individualized approach has been suggested, with the identification and irradiation of different target volumes (axillary levels I–III and supraclavicular lymph nodes) in accordance with the risk of their involvement.Citation14 Sentinel lymph nodes are present in the IM region in about 20%–30% of cases, but their routine biopsy is not justified. If they become positive, radiotherapy of the IM region appears reasonable, but this approach (which certainly increases the lung and heart doses in left-sided cases) has not yet been validated in clinical practice. The results of the present study and other analysesCitation21–Citation26 demonstrate that when irradiation of any of the axillary lymph-node levels or the IM lymph nodes is required, special attention should be paid to the doses to these target volumes; in most cases, the conventional tangential fields must be modified to meet the dosimetric need. Although prone radiotherapy is traditionally limited to the operated breast, efforts have been made to extend prone radiotherapy to patients who need irradiation of the axillary and supraclavicular lymph-node regions, through the use of conformal radiotherapy,Citation30 helical tomotherapy,Citation31 or intensity-modulated radiation therapy.Citation32 Therefore, in order to maintain the advantages of prone positioning, the target volume could be extended to the lymph nodes; nevertheless, the feasibility and repositioning accuracy of the method need to be investigated.
In our study, nodal regions were contoured with regard to their anatomical boundaries based on the RTOG atlas.Citation27 In the supine position, around half of the axillary level I volume was exposed to 45 Gy on average, and the irradiation of such a significant part harboring residual disease may well be of clinical significance; this is obviously not the case if radiotherapy is performed in the prone position.
Our findings are consistent with those of two other conformal radiotherapy studies that compared doses to the three axillary lymph-node levels in the prone versus the supine position during whole-breast irradiation.Citation21,Citation22 Alonso-Basanta et al studied the radiation-treatment plans (prone or supine) of 20 patients,Citation21 and Leonard et al compared the plans for 23 patients in the prone and 23 patients in the supine position.Citation22 Both studies led to the conclusion that the coverage of the three axillary nodal levels was inadequate in either position, but the doses were even lower in the prone than in the supine position. Our study on 100 patients provides additional information indicating that breast radiotherapy does not provide relevant coverage of the IM nodes in either the prone or the supine position.
In the prone position, the geography of the breast and the chest wall changes, and the conformity of the treatment plan is improved as less volume is irradiated outside the PTV.Citation4 In fact, not only are the conventionally identified OARs better spared from irradiation, but the volumes containing the regional lymph nodes are nearly completely excluded from the irradiated volume. While we found a mean dose of 45 Gy to the level I axillary lymph nodes in 17% of the patients in the supine position, none of the patients in the prone position received a relevant dose to any of the regional lymph nodes. The difference of nodal coverage between the two positions should be considered, since the irradiation of the regional lymph nodes may be individually beneficial or unnecessary. The supine position should be preferred, and the dose to the level I axillary nodes should be carefully checked if its therapeutic irradiation is an aim. Due to the changes of the shape of the irradiated breast, however, in accordance with our previous findings,Citation3 the dose inhomogeneity within the target volume was higher in the prone position, which may be considered as a disadvantage of the technique. Similarly, despite the different dose-prescription strategy and the use of the field-in-field technique in the prone position only, worse homogeneity index values and larger maximum dose, indicating greater dose inhomogeneity, were found in the prone position in the dosimetric study of Ramella et al.Citation33
Conclusion
The radiation dose to the axillary and IM lymph nodes during breast radiotherapy is therapeutically insufficient in most cases, and is lower in the prone than in the supine position. Attention should be paid to the specific targeting of lymph-node areas if this is clinically necessary.
Author contributions
MC participated in the preparation, acquisition, analysis, and interpretation of data, and made contributions to the drafting of the manuscript. DU participated in the preparation, acquisition, analysis, and interpretation of data. AC was involved in the design and conception of the study, and checked the preparation of the data. ZK participated in the conception and design of the study, the analysis and interpretation of the data, and the drafting of the manuscript. ZV participated in the conception and design of the study, carried out the collection and analysis of the data, was involved in the drafting of the manuscript, and carried out all statistical analyses. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- FormentiSCGidea-AddeoDGoldbergJDPhase I–II trial of prone accelerated intensity modulated radiation therapy to the breast to optimally spare normal tissueJ Clin Oncol2007252236224217470849
- FormentiSCDeWyngaertJKJozsefGGoldbergJDProne vs supine positioning for breast cancer radiotherapyJAMA201230886186322948692
- VargaZHideghétyKMezoTNikolényiAThurzóLKahánZIndividual positioning: a comparative study of adjuvant breast radiotherapy in the prone versus supine positionInt J Radiat Oncol Biol Phys2009759410019304405
- VargaZCserhátiARárosiFIndividualized positioning for maximum heart protection during breast irradiationActa Oncol201453586423544358
- KirbyAMEvansPMDonovanEMConveryHMHavilandJSYarnoldJRProne versus supine positioning for whole and partial-breast radiotherapy: a comparison of non-target tissue dosimetryRadiother Oncol20109617818420561695
- MitchellJFormentiSCDeWyngaertJKInterfraction and intrafraction setup variability for prone breast radiation therapyInt J Radiat Oncol Biol Phys2010761571157719910134
- KirbyAMEvansPMHelyerSJA randomised trial of supine versus prone breast radiotherapy (SuPr study): comparing set-up errors and respiratory motionRadiother Oncol201110022122621159397
- Fernández-LizarbeEMonteroAPoloAPilot study of feasibility and dosimetric comparison of prone versus supine breast radiotherapyClin Transl Oncol20131545045923143949
- StegmanLDBealKPHuntMAFornierMNMcCormickBLong-term clinical outcomes of whole-breast irradiation delivered in the prone positionInt J Radiat Oncol Biol Phys200768738117337131
- RagazJOlivottoIASpinelliJJLocoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy:20-year results of the British Columbia randomized trialJ Natl Cancer Inst20059711612615657341
- WhelanTJOlivottoIAckermanINCIC-CTG MA.20: an intergroup trial of regional nodal irradiation in early breast cancerJ Clin Oncol201129SupplLBA1003
- OvergaardMNielsenHMOvergaardJIs the benefit of postmastectomy irradiation limited to patients with four or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG 82 b&c randomized trialsRadiother Oncol20078224725317306393
- GiulianoAEHuntKKBallmanKVAxillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trialJAMA201130556957521304082
- HafftyBGHuntKKHarrisJRBuchholzTAPositive sentinel nodes without axillary dissection: implications for the radiation oncologistJ Clin Oncol2011294479448122042942
- HennequinCBossardNServagi-VernatSTen-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomyInt J Radiat Oncol Biol Phys20138686086623664327
- MatzingerOHeimsothIPoortmansPEORTC Radiation Oncology & Breast Cancer Groups. Toxicity at three years with and without irradiation of the internal mammary and medial supraclavicular lymph node chain in stage I to III breast cancer (EORTC trial 22922/10925)Acta Oncol2010491243420100142
- OlivottoIAChuaBElliottEAA clinical trial of breast radiation therapy versus breast plus regional radiation therapy in early-stage breast cancer: The MA20 trialClin Breast Cancer2003436136314715112
- PostmaELvan WieringenSHobbelinkMGSentinel lymph node biopsy of the internal mammary chain in breast cancerBreast Cancer Res Treat201213473574122678155
- CoombsNJBoyagesJFrenchJRUngOAInternal mammary sentinel nodes: ignore, irradiate or operate? Eur J Cancer20094578979419121579
- BourreJCPayanRCollombDCan the sentinel lymph node technique affect decisions to offer internal mammary chain irradiation? Eur J Nucl Med Mol Imaging20093675876419142635
- Alonso-BasantaMKoJBabcockMDewyngaertJKFormentiSCCoverage of axillary lymph nodes in supine vs prone breast radiotherapyInt J Radiat Oncol Biol Phys20097374575118687534
- LeonardKLSolomonDHepelJTHiattJRWazerDEDiPetrilloTAAxillary lymph node dose with tangential whole breast radiation in the prone versus supine position: a dosimetric studyRadiat Oncol201277222607612
- KrasinMMcCallAKingSOlsonMEmamiBEvaluation of a standard breast tangent technique: a dose-volume analysis of tangential irradiation using three-dimensional toolsInt J Radiat Oncol Biol Phys20004732733310802356
- ReedDRLindsleySKMannGNAxillary lymph node dose with tangential breast irradiationInt J Radiat Oncol Biol Phys20056135836415667953
- ReznikJCicchettiMGDegaspeBFitzgeraldTJAnalysis of axillary coverage during tangential radiation therapy to the breastInt J Radiat Oncol Biol Phys20056116316815629607
- BelkacemiYAllab-PanQBigorieVThe standard tangential fields used for breast irradiation do not allow optimal coverage and dose distribution in axillary levels I–II and the sentinel node areaAnn Oncol2013242023202823616280
- LiXATaiAArthurDWVariability of target and normal structure delineation for breast cancer radiotherapy: an RTOG multi-institutional and multiobserver studyInt J Radiat Oncol Biol Phys20097394495119215827
- FeuvretLNoëlGMazeronJJBeyPConformity index: a reviewInt J Radiat Oncol Biol Phys20066433334216414369
- ZhuLJinLLiSWhich nomogram is best for predicting non-sentinel lymph node metastasis in breast cancer patients? A meta-analysisBreast Cancer Res Treat201313778379523292085
- GieldaBTStraussJBMarshJCTurianJVGriemKLA dosimetric comparison between the supine and prone positions for three-field intact breast radiotherapyAm J Clin Oncol20113422323020562590
- KainzKWhiteJChenGPHermandJEnglandMLiXASimultaneous irradiation of the breast and regional lymph nodes in prone position using helical tomotherapyBr J Radiol201285e899e90522457317
- SethiRANoHSJozsefGKoJPFormentiSCComparison of three-dimensional versus intensity-modulated radiotherapy techniques to treat breast and axillary level III and supraclavicular nodes in a prone versus supine positionRadiother Oncol2012102748121993404
- RamellaSTrodellaLIppolitoEWhole-breast irradiation: a subgroup analysis of criteria to stratify for prone position treatmentMed Dosim20123718619122195735
