Abstract
Background
In Spain, hospital medicines are assessed and selected by local Pharmacy and Therapeutics committees (PTCs). Of all the drugs assessed, cancer drugs are particularly important because of their budgetary impact and the sometimes arguable added value with respect to existing alternatives. This study analyzed the PTC drug selection process and the main objective was to evaluate the degree of compliance of prescriptions for oncology drugs with their criteria for use.
Methods
This was a retrospective observational study (May 2007 to April 2010) of PTC-assessed drugs. The variables measured to describe the committee’s activity were number of drugs assessed per year and number of drugs included in any of these settings: without restrictions, with criteria for use, and not included in formulary. These drugs were also analyzed by therapeutic group. To assess the degree of compliance of prescriptions, a score was calculated to determine whether prescriptions for bevacizumab, cetuximab, trastuzumab, and bortezomib were issued in accordance with PTC drug use criteria.
Results
The PTC received requests for inclusion of 40 drugs, of which 32 were included in the hospital formulary (80.0%). Criteria for use were established for 28 (87.5%) of the drugs included. In total, 293 patients were treated with the four cancer drugs in eight different therapeutic indications. The average prescription compliance scores were as follows: bevacizumab, 83% for metastatic colorectal cancer, 100% for metastatic breast cancer, and 82.3% for non-small-cell lung cancer; cetuximab, 62.0% for colorectal cancer and 50% for head and neck cancer; trastuzumab, 95.1% for early breast cancer and 82.4% for metastatic breast cancer; and bortezomib, 63.7% for multiple myeloma.
Conclusion
The degree of compliance with criteria for use of cancer drugs was reasonably high. PTC functions need to be changed so that they can carry out more innovative tasks, such as monitoring conditions for drug use.
Introduction
The ongoing inclusion of new medications in hospital formularies is a key factor explaining the increase in health care spending;Citation1,Citation2 however, new medications do not always result in better health outcomes,Citation3 with very few actually offering significant advantages over existing therapies in terms of efficacy and safety. For example, a study published in the French independent journal Prescrire International found that in the 5 years leading up to 2012, no new drugs licensed represented a significant advance for patients, and of 82 new drugs evaluated in 2012, only one represented a real advance and three offered an advantage.Citation4
In the European Union, the procedure for authorizing the sale of new drugs does not require a comparison with standard treatments, so companies need only to prove that the risk–benefit balance of a new drug is favorable.Citation5 Further, the procedure does not include a review of a drug’s cost-effectiveness or place in therapy.Citation6
It is therefore necessary to carry out these analyses in an additional study. Most of the drugs available in Spain are funded by the public health service and there is no national government agency, such as the National Institute for Health and Care Excellence in the UK, which carries out a centralized evaluation and makes decisions about funding.Citation7
The Spanish National Health Service has a decentralized structure whereby autonomous regions make their own decisions about health care spending and manage their budgets through their regional ministries of health. There are centers that evaluate new drugs, but they merely provide recommendations, which hospitals and prescribers are in no way obliged to follow.
So neither the national nor the regional health ministries set out shared guidelines to rationalize the use of medicines in the Spanish National Health Service based on criteria relating to effectiveness, appropriate use, and efficiency. Drugs are therefore assessed and selected locally. In recent years, regional health ministries have published new legislation to carry out baseline assessments for their regions, and some of them have established centralized PTCs that take some decisions mandatory for the whole region. Also, the Ministry of Health is currently in the process of conducting a cooperative national initiative project assessing comparative efficacy and safety and introducing use criteria for new drugs or existing drugs seeking approval for new indications.
Drugs used in hospitals (those administered to inpatients and outpatients attending the hospital for drug administration, and drugs that can only be dispensed by the hospital pharmacy service) are assessed by Pharmacy and Therapeutics committees (PTCs). These committees select the drugs to be used, generally taking into account pharmacoeconomic criteria and the relative efficiency of drugs compared with the alternatives available. The drugs that are selected are added to the formulary for each hospital.Citation8
Once a drug has been selected, the PTC may establish conditions for its use so that the drug is only used in subgroups of patients where it will have clinically significant benefits and where the cost has been taken into account. Use of the drug must then be monitored to ensure that it meets the established criteria.
Of all the drugs assessed by PTCs, cancer drugs are particularly important because of their budgetary impactCitation9,Citation10 and their sometimes arguable added value with respect to existing alternatives, which is measured in terms of improved rates of survival or quality of life.Citation11
To date, no studies have been published that monitor the real conditions of use of oncology drugs in Spanish National Health Service hospitals or that ascertain whether they are used in accordance with the PTC criteria set out by the hospital.
The aims of this study were to analyze the selection of new drugs by the PTC of a large secondary care hospital in Spain and to assess the degree to which the cancer drugs included in the hospital’s formulary were used in accordance with the criteria for use set out by the PTC (compliance).
Materials and methods
Study design and setting
A retrospective observational longitudinal study was carried out between May 1, 2007 and April 30, 2010 in the setting of Cabueñes Hospital, a Spanish National Health Service general secondary care hospital. The hospital serves a population of 303,038 in the Spanish region of Asturias. Oncology treatments for the whole area are administered at this hospital. The PTC of Cabueñes Hospital was created in 1974. It is a multidisciplinary committee made up of physicians, pharmacists, and nurses, as well as members of the hospital’s management team. At the request of clinicians, the PTC assesses drugs for inclusion in the hospital formulary using the methodology proposed by the Group for Innovation, Assessment, Standardization and Research in the Selection of Drugs (GENESIS) of the Spanish Society of Hospital Pharmacy.Citation12 The PTC can make one of three decisions for each drug: not included, included without criteria for use, and included with criteria for use.
Drug selection by the PTC
The study examined the selection of all new drugs assessed by the PTC during the study period. Drugs were selected for inclusion in the study by consulting the minutes of the PTC meetings.
Two main variables were collected in order to evaluate the selection activities of the PTC, ie, number of drugs assessed per year and number of drugs included in any of these settings: without restrictions, with criteria for use, and not included in formulary. The drugs were also analyzed by therapeutic group.
Compliance with drug inclusion criteria
All oncology drugs approved by the PTC were included in the study. The drugs were bevacizumab, cetuximab, trastuzumab, and bortezomib, and their use was assessed from the time each one was approved by the PTC (bevacizumab May 20, 2008; cetuximab March 18, 2008; trastuzumab February 19, 2008; and bortezomib July 17, 2007).
Patients treated with any of the four cancer drugs (bevacizumab, cetuximab, trastuzumab, and bortezomib) were identified by consulting the pharmacy service database for the prescription, validation, and preparation of cytostatic drugs. Any other information required was retrieved from patients’ notes. Patients taking part in a clinical trial and those taking any of the drugs for an off-label purpose as current national regulations lay down or for indications other than the treatment of cancer were excluded from the study. When a patient had used a drug for two different episodes, he or she was considered to be two respective patients. Identifying information was removed from patient records to maintain confidentiality; thus, approved of an investigational review board was not required.
In order to assess the degree to which prescriptions complied with the criteria for use stipulated by the PTC, the actual conditions under which each drug was being used were compared with the PTC’s criteria for use. Compliance was analyzed based on a series of variables for each drug: diagnosis (tumor location) and compliance with criteria for use in terms of stage of the disease, life expectancy, treatment regimen (in combination with other drugs), line of treatment (preferred order for treatment options available), previous treatments, duration of treatment, and presence of certain gene mutations. When a drug was not used for the approved diagnosis (used off-label without asking for permission to use it, or for an indication not approved by the PTC), the rest of the variables were not assessed.
For each of the four drugs and for each of the clinical indications, a score was calculated using previous criteria-for-use variables. Each criterion had the same weighting and could be assigned one of two values: yes (=1) or no (=0). The final score for each drug and clinical indication was determined by calculating the sum of the scores for the criteria-for-use variables, expressed as a percentage (). This score represented compliance with the PTC criteria for use. This scoring system has been previously used by García Robredo et al.Citation13 The number and percentage of patients meeting all of the criteria were calculated for each drug and indication.
Table 1 Indicator calculations
Statistical analysis
Data on drug selection by the PTC were summarized in a frequency and percentage table. In order to assess the degree of compliance for each drug and indication, the average compliance percentage was calculated for each criterion for the group of patients treated in each case. The percentage of patients meeting all of the criteria for each drug and indication was calculated. The 95% confidence interval (CI) was computed. Both of these summarized measures were illustrated in bar graphs. The analysis was carried out and graphs were created using statistics program R (version 3.0.1, R Foundation for Statistical Computing, Vienna, Austria).Citation14
Results
Drug selection by the PTC
Between May 2007 and April 2010, the PTC received requests for inclusion of 40 drugs in the hospital formulary (17 in the first year, eleven in the second, and 12 in the third), of which 32 were included (80.0%). Criteria for use were established for 28 (87.5%) of the drugs included. The four drugs included without criteria for use were assessed during the first year of the study.
By therapeutic group, the highest percentages of requests were for the Anatomical Therapeutic Chemical classification systemCitation15 group L (antineoplastic and immunomodulation agents), with seven requests, and group J (anti-infective agents for systemic use), also with seven requests, followed by group M (musculoskeletal system), with five requests. Of the eight drugs not included in the formulary, four were in group M. All of the drugs in groups L and J were included with criteria for use ().
Table 2 Drugs requested for inclusion in hospital formulary
Compliance with drug use
The baseline characteristics of all patients are shown in . The degree of compliance for the four drugs with criteria for use defined by the PTC is described in .
Figure 1 Indicator scores for the degree of compliance of prescriptions for cancer drugs with criteria for use.
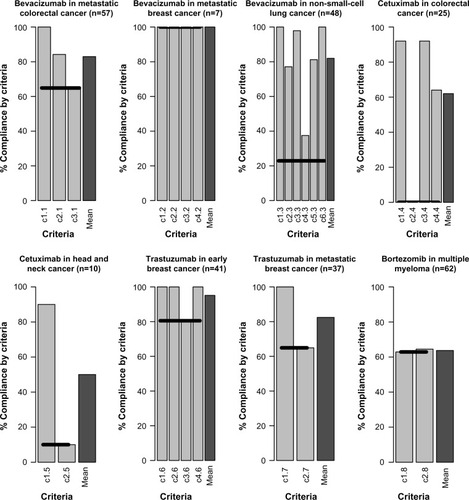
Table 3 Patient baseline characteristics
Bevacizumab
Bevacizumab was used in 114 patients. For 112 (98.2%), it was used for the following PTC-approved indications: colorectal cancer in 57 patients (50.0%), breast cancer in seven patients (6.1%), and lung cancer in 48 patients (42.1%). It was also used in two patients with renal cancer, an indication that is approved in the drug’s summary of product characteristics but was not approved by the PTC.
All of the patients who were prescribed bevacizumab for metastatic colorectal cancer (n=57) were assumed to have a life expectancy of more than 3 months. In nine patients, it was not used concomitantly with capecitabine + oxaliplatin, and in 20 it was not used as a first-line treatment, so the average compliance score for this indication was 83% (95% CI, 76.4%–89.5%). In the case of metastatic breast cancer, bevacizumab met all of the criteria for use and scored 100% for compliance. The degree of compliance in non-small-cell lung cancer was 82.3% (95% CI, 78.4%–85.5%) because, although in all cases it was prescribed to patients without hemoptysis and with non-squamous cancer and to just one patient with brain metastasis, in nine patients it was not used as a first-line treatment, in eleven it was used in stages earlier than those approved, and in 30 of the 48 patients it was used in a chemotherapy regimen other than cisplatin + gemcitabine.
Cetuximab
During the study period, 35 patients started treatment with cetuximab, of whom 25 (71.4%) had colorectal cancer and ten (28.6%) had head and neck cancer. Therefore, 100% of prescriptions for cetuximab were for diseases included in the criteria for use set out by the PTC.
The compliance score for colorectal cancer was 62% (95% CI, 55.6%–68.4%). None of the patients with this type of cancer underwent epidermal growth factor receptor (EGFR) expression testing, all but two had metastases, and all but two had previously undergone chemotherapy with oxaliplatin or irinotecan. Cetuximab was administered in combination with irinotecan in 16 of the 25 patients.
In the case of head and neck cancer, only one of the ten patients was not taking cetuximab concomitantly with radiotherapy. All but one of the patients could have undergone treatment with cisplatin, but instead received cetuximab in combination with paclitaxel; this reduced the compliance score to 50% (95% CI, 35.4%–64.6%).
Trastuzumab
Trastuzumab was used in 80 patients, but in two cases (2.5%) the drug was used in nonapproved indications (stomach cancer and sweat gland cancer). The highest compliance score was for early breast cancer (95.1%; 95% CI, 92.1%–98.2%), because all of the criteria were met in all but eight patients who were on a regimen other than carboplatin + docetaxel + trastuzumab. Thirteen of the 37 patients with metastatic breast cancer were using trastuzumab in an unapproved chemotherapy regimen, resulting in a final compliance score for this indication of 82.4% (95% CI, 74.3%–90.2%).
Bortezomib
Bortezomib was used in 64 patients, but in two cases the drug was used for indications not approved by the PTC (mantle cell lymphoma and Waldenström’s macroglobulinemia). Of the 62 patients undergoing treatment with bortezomib for multiple myeloma, it was used as a second-line or subsequent treatment in only 39. In one of these patients, the later lines of treatment were not administered as a result of relapse or resistance but because of side effects, which meant the previous line had to be stopped. The final compliance score was therefore 63.7% (95% CI, 51.6%–75.7%).
Discussion
The percentage of requested drugs that were included in the hospital formulary was similar to that found in previous national studies.Citation16 This may be because of the tendency in Spain to standardize assessment methodologies, as encouraged by the Group for Innovation, Assessment, Standardization and Research in the Selection of Drugs.Citation17 This means that different hospitals and PTCs may use similar selection systems and procedures.
The number of drugs assessed decreased in the second and third years of the study because the PTC was not operational in 2006. This meant that extra effort was made in 2007 to assess the drugs requested during the committee’s period of inactivity. All of the oncologic drugs were assessed during this first year as a need to give priority to cancer treatments over other drugs for less serious illnesses. The number of drugs assessed in the subsequent 2 years is consistent with the findings of other studies, and contrasts with the high number of drugs on the market.Citation18–Citation21 According to Puigventós Latorre et al,Citation22 this could be because the request, assessment, and approval process limits the number of drugs that can be assessed, so priority is given to those that could offer significant advances. This would also explain the high approval rate.
The high percentage of drugs included with criteria for use in this study also illustrates how the function of the PTC has evolved to perform more innovative tasks, such as establishing conditions for drug use. Further development of the process needs to include monitoring of drug use, drug switching protocols, indirect comparisons, and drawing up protocols or clinical guidelines.Citation23,Citation24
With regard to compliance, the highest compliance scores were for bevacizumab and trastuzumab, possibly because they are used in more prevalent cancers (breast, colorectal, and lung cancers)Citation25 that incur higher costs, so budgetary protocols are more likely to exist and be adhered to for these cancers.
The top compliance score was for bevacizumab in the treatment of metastatic breast cancer. Interestingly, in 2011, the US Food and Drug AdministrationCitation26 withdrew this indication, which had been approved in 2008 as part of its accelerated approval program, because subsequent studies showed that progression-free survival was lower than initially calculated and with significant adverse effects; therefore, the benefits of treatment no longer outweighed the risks. In 2010, the European Medicines Agency withdrew its indication combined with docetaxel, but kept the combination with paclitaxel and later added the indication for first-line treatment in combination with capecitabine for patients in whom treatment with taxanes or anthracyclines was not considered appropriate.Citation27
The average compliance score for cetuximab in patients with colorectal cancer was 62.0%. This relatively low score was because none of the patients met the EGFR expression criterion; this test is no longer performed for this tumor type following reports from various studies that the presence of the EGFR mutation does not determine cetuximab activity.Citation28 After the drug was approved by the PTC, the European Medicines AgencyCitation29 changed the indication to EGFR- positive patients with the wild-type KRAS gene. This is a good example of why PTC criteria need to be regularly reviewed and amended where appropriate. The lowest compliance score was for cetuximab in head and neck cancer (50.0%), where all but one of the patients could have received cisplatin, but an unapproved regimen (paclitaxel + cetuximab) was used instead. This is important because one of the ways to make cancer treatments more affordable is to monitor and reduce off-label use, which is used sometimes, according to Sullivan et al,Citation30 in scenarios where there is little benefit and more toxicity compared with drugs that cost much less. If the compliance results had been assessed as the percentage of patients meeting all criteria defined by the PTC, the result would have been much lower, especially in the case of cetuximab. One of the criteria for use of bortezomib was that patients needed to have relapsed or be resistant to at least one treatment. In August 2008, the European Medicines Agency authorized a new indication for previously untreated patients not eligible for high-dose chemotherapy with bone marrow transplant.Citation31
The new indications approved by regulatory agencies after drugs are included in formularies show that drugs need to be reassessed by the PTC, and if appropriate, their criteria for use amended. The PTC should also carry out studies on the way in which approved drugs are used, in order to measure the degree of compliance with criteria for use, as recommended in the American Society of Health-System Pharmacists guidelines.Citation32
The foremost limitation of the current study is that the results were interpreted retrospectively. A second limitation was the small number of patients with some low-prevalence cancers that could only have been resolved by increasing the length of the study period, as all of the patients treated after a drug was included in the formulary were included in the study. However, the 3-year study period was the maximum length at the time the study began because, as mentioned above, the PTC was inoperative for a year and when it became active again new working guidelines were established. Third, the results are limited because the study was done in one center and with very specific drugs. If the study had been done in another setting with other drugs, the results could have been different, which compromises the external validity of the study.
The Spanish reimbursement process is changing, and the new process intends to rationalize, standardize, and expedite the assessment of new drugs. This study was conducted some years ago, so it would be interesting to do it again to see if the results would be similar nowadays.
Conclusion
The degree of compliance with criteria for use of cancer drugs is reasonably high. PTCs need to regularly review their criteria for use of individual drugs in light of clinical guidelines and newly approved indications. PTCs also need to continue to evolve and adapt their activities with regard to drug assessment, monitoring, and development of protocols. Further research should be carried out to investigate the clinical and financial benefits of establishing criteria for use as part of the drug selection process.
Acknowledgments
We would like to thank Gemma Cherry from the University of Liverpool who read and commented on a draft version of this paper.
Disclosure
The authors declare that they have no conflict of interest in this work.
References
- HartmanMMartinABBensonJCatlinANational health spending in 2011: overall growth remains low, but some payers and services show signs of accelerationHealth Aff (Millwood)2013321879923297275
- RamliAAljunidSMSulongSMd YusofFANational Drug Formulary review of statin therapeutic group using the multiattribute scoring toolTher Clin Risk Manag2013949150424353428
- ZhangYSoumeraiSBDo newer prescription drugs pay for themselves? A reassessment of the evidenceHealth Aff (Millwood)200726388088617485770
- [No authors listed]New drugs and indications in 2012. Sluggish progress, timid measures to protect patientsPrescrire Int20132213710510723662323
- Directive 2004/27/EC of the European Parliament and the Council of March 31, 2004 amending Directive 2001/83/EC on the Community code relating to medicinal products for human use (Text with EEA relevance), 2004Official Journal L136, 30/4/200420042683457 Available from: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:32004L0027:EN:HTMLAccessed February 15, 2014
- PignattiFGravanisIHeroldRVamvakasSJonssonBMartyMThe European Medicines Agency: an overview of its mission, responsibilities, and recent initiatives in cancer drug regulationClin Cancer Res201117165220522521844037
- Soto AlvarezJTherapeutic and social usefulness of medicines: how can it be evaluated and quantified?Med Clin (Barc)20091323104105 Spanish19211062
- FullertonDSPAtherlyDSFormularies, therapeutics, and outcomes: new opportunitiesMed Care200442Suppl 4III39III4415026670
- DrummondMFMasonAREuropean perspective on the costs and cost-effectiveness of cancer therapiesJ Clin Oncol200725219119517210939
- McCabeCBergmannLBosanquetNMarket and patient access to new oncology products in Europe: a current, multidisciplinary perspectiveAnn Oncol200920340341218854550
- SmithTJHillnerBEBending the cost curve in cancer careN Engl J Med2011364212060206521612477
- Group for Innovation Assessment Standardisation and Research in the Selection of Drugs (GENESIS) of the Spanish Association of Hospital PharmacyMADRE Programme. Procedures Manual. PDF 3.0 version2005 Available from: http://gruposdetrabajo.sefh.es/genesis/index.php?option=com_content&view=article&id=11&Itemid=13Accessed February 15, 2014
- García RobredoBCalleja HernándezMALuque VegaMIUbago PérezRFaus DáderMJCompliance of prescriptions for chronic obstructive pulmonary disease patients given upon hospital dischargeFarm Hosp2010344188193 Spanish20537931
- R Core TeamR: A language and environment for statistical computingR Foundation for Statistical ComputingVienna, Austria Available from: http://www.R-project.org/Accessed February 15, 2014
- WHO Collaborating Centre for Drug Statistics MethodologyGuidelines for ATC classification and DDD assignment 2011OsloWorld Health Organization2010 Available from: http://www.whocc.no/filearchive/publications/2011guidelines.pdfAccessed June 25, 2014
- PuigventósFSantos-RamosBOrtegaADurán-GarcíaEStructure and procedures of the pharmacy and therapeutic committees in Spanish hospitalsPharm World Sci201032676777520820918
- Ortega EslavaAPuigventós LatorreFSantos-RamosBCalderon HernanzBVilanova BoltóMClassification and variability of drug assessment reports on the GENESIS group (SEFH) webpageFarm Hosp2011353140147 Spanish21450502
- New Medicines: 2007 ReviewInformación Terapeútica del Sistema Nacional de Salud20083211725 Available from: http://www.msssi.gob.es/va/biblioPublic/publicaciones/docs/vol32_1NuevosPrincipiosActivos2007.pdfAccessed February 15, 2014 Spanish
- New Medicines: 2008 ReviewInformación Terapeútica del Sistema Nacional de Salud20093311522 Available from: http://www.msssi.gob.es/va/biblioPublic/publicaciones/recursos_propios/infMedic/docs/vol33_1ppiosActivos.pdfAccessed February 15, 2014 Spanish
- New Medicines: 2009 ReviewInformación Terapeútica del Sistema Nacional de Salud20103411225 Available from: http://www.msssi.gob.es/va/biblioPublic/publicaciones/recursos_propios/inf-Medic/docs/BoletinVol34n1_12a25.pdfAccessed February 15, 2014 Spanish
- New Medicines: 2010 ReviewInformación Terapeútica del Sistema Nacional de Salud20113512131 Available from: http://www.msssi.gob.es/va/biblioPublic/publicaciones/recursos_propios/infMedic/docs/vol35_1_Nuevos_PA.pdfAccessed February 15, 2014 Spanish
- Puigventós LatorreFSantos-RamosBOrtega EslavaADurán-GarcíaMEVariability in activity and results from drug assessments by pharmacy and therapeutics committees in Spanish hospitalsFarm Hosp2011356305314 Spanish21497125
- Durán-GarcíaESantos-RamosBPuigventos-LatorreFOrtegaALiterature review on the structure and operation of Pharmacy and Therapeutics CommitteesInt J Clin Pharm201133347548321416393
- HoffmannMThe right drug, but from whose perspective? A framework for analysing the structure and activities of drug and therapeutics committeesEur J Clin Pharmacol201369Suppl 1798723640192
- FerlayJShinH-RBrayFFormanDMathersCParkinDMEstimates of worldwide burden of cancer in 2008: GLOBOCAN 2008Int J Cancer2010127122893291721351269
- US Food Drug AdministrationPostmarket Drug Safety Information for Patients and Providers. Avastin (bevacizumab information)2011 Available from: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm193900.htmAccessed February 15, 2014
- European Medicines AgencyChanges since initial authorization of medicine. Avastin-H-C-582-II-33: EPAR Assessment Report – Variation Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000582/WC500108311.pdfAccessed February 15, 2014
- NgKZhuAXTargeting the epidermal growth factor receptor in metastatic colorectal cancerCrit Rev Oncol Hematol200865182018006328
- European Medicines AgencyChanges since initial authorization of medicine. Erbitux-H-C-558-II-20: EPAR Assessment report variation Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000558/WC500029117.pdfAccessed February 15, 2014
- SullivanRPeppercornJSikoraKDelivering affordable cancer care in high-income countriesLancet Oncol2011121093398021958503
- European Medicines AgencyChanges since initial authorization of medicine. Velcade-H-C-539-II-28: EPAR Assessment Report – Variation Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000539/WC500048473.pdfAccessed February 15, 2014
- TylerLSColeSWMayJRASHP guidelines on the Pharmacy and Therapeutics Committee and the formulary systemAm J Health Syst Pharm200865131272128318589893
- ReubenDBMorVHirisJClinical symptoms and length of survival in patients with terminal cancerArch Intern Med19881487158615913382303
