Abstract
Diabetes is a complex and progressive disease that has a major societal and economic impact. The most common form of diabetes, type 2 diabetes mellitus (T2DM), is a multifactorial disease, the pathophysiology of which involves not only the pancreas but also the liver, skeletal muscle, adipose tissue, gastrointestinal tract, brain, and kidney. Novel therapies with mechanisms of action that are different from most existing drugs are emerging. One such class consists of compounds that inhibit renal sodium-glucose cotransporter 2, which is responsible for the bulk of glucose reabsorption by the kidneys. This new class of compounds improves glycemic control independently of insulin and promotes weight reduction, providing an additional tool to treat patients with T2DM. This review discusses the underlying pathophysiology of T2DM, clinical guidelines, and available and emerging treatment options, with particular emphasis on sodium-glucose cotransporter 2 inhibitors.
Introduction
Diabetes is a complex and potentially debilitating disease that affects an estimated 8.3% of the adult population or 382 million people worldwide.Citation1 The region with the highest number of adults with diabetes, ie, 138 million, is the Western Pacific, which includes the People’s Republic of China.Citation1 It is estimated that 29.1 million people in the USA (9.3% of the population) have diabetes.Citation2 If current trends continue, it is estimated that 592 million people worldwide will have diabetes by 2035.Citation1
Diabetes care has a major economic impact in both developed and developing countries. Estimated global health care costs to treat and prevent diabetes were at least $548 billion in 2011.Citation1 In the USA, the total cost of diabetes was estimated to be $245 billion in 2012Citation2 and may exceed $500 billion by 2025.Citation3
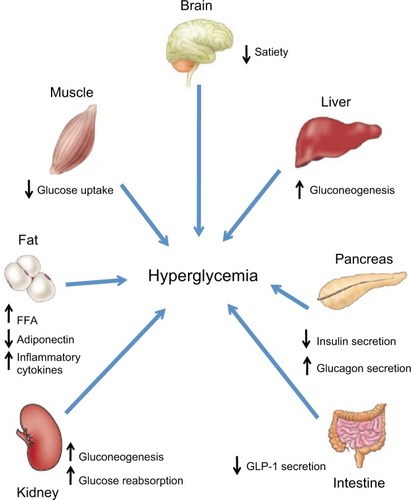
Type 2 diabetes mellitus (T2DM) accounts for 90%–95% of new cases of diabetes.Citation2 T2DM pathophysiology involves at least seven organs and tissues, including the pancreas, liver, skeletal muscle, adipose tissue, brain, gastrointestinal tract, and kidney ().Citation4 Reduced sensitivity to insulin (ie, impaired insulin-mediated glucose disposal or insulin resistance) in liver, muscle, and adipose tissue, and a progressive decline in pancreatic β-cell function leading to impaired insulin secretion, eventually result in hyperglycemia, the hallmark feature of T2DM. The purpose of this review is to discuss the underlying pathophysiology of T2DM, clinical treatment guidelines, and available and emerging treatment options, with emphasis on the newest class of antihyperglycemic drugs, the sodium-glucose cotransporter 2 (SGLT2) inhibitors.
Figure 1 Multiorgan and tissue pathophysiology of type 2 diabetes.
Abbreviations: FFA, free fatty acids; GLP-1, glucagon-like peptide-1.
Pathophysiology
Pancreas
Impairment of insulin action and of β-cell function occurs very early in the development of T2DM.Citation5 Insulin resistance can be detected in individuals with normal glucose tolerance who are at higher risk for development of T2DM 10–20 years before the disease is diagnosed.Citation6 Further, individuals who are transitioning from impaired glucose tolerance to T2DM may have already lost up to 80% of their β-cell function.Citation4 Mechanisms thought to play a role in the decline of β-cell function include the following:
Genetics
The clustering of T2DM in families has long been recognized.Citation7 A number of genes associated with insulin and β-cell dysfunction have been identified in patients with T2DM, including genetic variants associated with pancreatic development and insulin storage and secretion.Citation8 With insulin resistance comes an increased need for biosynthesis and release of insulin. It has been proposed that a genetic polymorphism in patients predisposed to T2DM results in failure of the β cell to adapt to the increased demand for insulin.Citation9
Age
Numerous studies have demonstrated an age-related decline in β-cell function and insulin secretion.Citation10 This is consistent with the increased prevalence of T2DM with aging.Citation2
Diet and exercise
Obesity and physical inactivity are major factors in the increased prevalence of T2DM worldwideCitation11 and are associated with insulin resistance.Citation4 Diets high in rapidly absorbable carbohydrates result in elevated insulin and blood glucose levels,Citation11 and the deposition of fat in liver and muscle increases insulin resistance in these tissues.Citation4 These factors increase the demand for insulin, and in the long term may lead to progressive β-cell failure.Citation4,Citation11
Glucotoxicity
Chronic exposure to elevated glucose concentrations impairs β-cell function and insulin secretion. The mechanisms involved in glucotoxicity remain to be elucidated but likely involve impairment of insulin gene expression, chronic oxidative stress, and apoptosis.Citation12
Lipotoxicity
Elevated plasma concentrations of free fatty acids (FFAs) impair insulin secretion in patients at risk for development of T2DM.Citation13,Citation14 Elevated FFAs in β-cells lead to increased oxidative stress and apoptosis.Citation15
Liver
The liver is the main organ responsible for glucose production.Citation16 Hepatic glucose production and release into the circulation comes from both gluconeogenesis and glycogenolysis.Citation16,Citation17 In patients with T2DM, the liver overproduces glucose because it becomes resistant to the suppressive effects of insulin.Citation4 Other factors, such as lack of suppression of postprandial glucagon secretion from pancreatic α cells in patients with T2DM,Citation18 increased circulating glucagon, and increased sensitivity of the liver to glucagon, also contribute to increased hepatic glucose production.Citation4
Muscle
Insulin-stimulated transport of glucose into skeletal muscle is the primary mechanism for the disposal of an exogenous glucose load.Citation19 The major transporter involved in the uptake of glucose into skeletal muscle, glucose transporter 4 (GLUT4),Citation19 is also expressed in adipocytes and cardiac muscle and is responsible for insulin-stimulated glucose uptake into these tissues.Citation20 Insulin and exercise acutely stimulate the translocation of GLUT4 to the membrane of muscle cells, resulting in increased glucose uptake.Citation19,Citation20 In patients with T2DM, skeletal muscle is resistant to the actions of insulin because of defects in insulin signaling and often a low level of physical activity.Citation21 This leads to a decrease in glucose uptake that contributes to the development of hyperglycemia.
Adipose tissue
In patients with T2DM, adipocytes are resistant to the antilipolytic effect of insulin, resulting in elevation of circulating FFAs. Chronic increases in FFAs stimulate gluconeogenesis, induce hepatic and muscle insulin resistance, and impair insulin secretion.Citation22 These lipid-induced changes in T2DM are part of a constellation of changes induced by excess FFAs, termed lipotoxicity.Citation15 Dysfunctional adipose tissue produces excessive amounts of inflammatory and atherogenic cytokines that can induce insulin resistance and concurrently fails to adequately secrete insulin-sensitizing adipocytokines.Citation22
Much interest has recently been focused on “brown fat”, a very metabolically active adipose tissue previously thought to be present only in small mammals and newborn humans, where it functions in cold-induced or diet-induced heat production.Citation23 However, recent studies have shown that brown fat is also present in human adults.Citation24–Citation27 In contrast with white adipose tissue, which stores excess energy as triglycerides,Citation23 brown adipose tissue uses small intracellular triglyceride vacuoles as a main energy source to produce heat.Citation28 The mass of brown fat has been shown to be directly related to resting metabolic rateCitation26 and inversely correlated with age, total body fat, and body mass index.Citation24–Citation26 In addition, exercise has been shown to induce the “browning” of white adipose tissue.Citation29 These findings suggest that brown fat may play an important role in energy metabolism and in body weight control. However, the role of brown fat in the pathogenesis of T2DM is unclear.
Brain
Insulin can cross the blood-brain barrier and, by modulating the expression of various neuropeptides involved in food intake, suppress appetite.Citation30 In patients with T2DM, the brain may become insulin resistant, such that the inhibitory effect of insulin on appetite is lost.Citation30 In fact, central insulin resistance may develop in individuals at risk for T2DM who are otherwise healthy.Citation31
Amylin, a peptide synthesized and cosecreted with insulin from β cells, decreases food intakeCitation32 by sensitizing the area postrema and nucleus of the solitary tract to other metabolic signals that reduce food intake, such as cholecystokinin and glucose.Citation33 Amylin also slows gastric emptying, and reduces postprandial glucagon release.Citation32 In patients with T2DM, as β-cell function progressively declines, amylin secretion is reduced and its satiety-producing effects wane.Citation32
Leptin and ghrelin are two other hormones that act centrally to control food intake and body weight homeostasis. Leptin is mainly produced and secreted by adipocytes,Citation34 and its blood concentration is proportional to the percentage of body fat.Citation35 A major effect of leptin is to decrease food intake and body weight by acting on areas in the hypothalamus involved in feeding behavior and energy balance.Citation36 Many individuals with T2DM are obese, have high circulating levels of leptin, and are resistant to exogenous leptin.Citation34 However, a subset of obese individuals has low levels of leptin and in these individuals exogenous leptin improves obesity.Citation37 Although exogenous leptin prevents insulin resistance in animal models of diabetes,Citation38 treatment of obese patients with T2DM did not improve insulin sensitivity.Citation39
Ghrelin is secreted mainly by the stomach during fasting or caloric restriction and acts in the central nervous system to promote food intake.Citation40 Ghrelin and its receptor are also present in pancreatic islet cells.Citation41,Citation42 In healthy humans, exogenous ghrelin reduces insulin secretionCitation43,Citation44 and causes hyperglycemia.Citation43,Citation45 In a population-based study, low plasma ghrelin concentrations were associated with increased fasting insulin concentrations, insulin resistance, and an increased prevalence of T2DM.Citation46
Gastrointestinal tract
Glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) are hormones released by the gastrointestinal tract (incretins) in response to nutrient ingestion.Citation47 GLP-1 and GIP act on β cells to stimulate the release of insulin and are responsible for up to 60% of insulin secretion following a meal.Citation48 GLP-1 also promotes satiety, slows gastric emptying, and inhibits glucagon secretion, thus reducing hepatic glucose production.Citation49 Patients with T2DM have impaired secretion of GLP-1 and reduced responsiveness to GIP.Citation48 This results in increased gastrointestinal motility, decreased glucose-dependent insulin secretion, increased glucagon secretion, and increased liver glucose release, all of which adversely affect glycemic control.
Kidney
Under normal conditions, more than 99% of glucose filtered by the kidneys is reabsorbed in the proximal tubule.Citation50 The bulk of glucose is reabsorbed by the SGLT2, in concert with a facilitative glucose transporter, GLUT2.Citation50 Once plasma glucose concentrations exceed the renal threshold for reabsorption (approximately 180 mg/dL in healthy individuals), glucose starts to appear in the urine.Citation51 A recent study demonstrated that the capacity of the kidney to reabsorb glucose is increased in patients with T2DM compared with matched healthy individuals.Citation52 Therefore, in patients with T2DM, the kidneys reabsorb glucose in excess and return it to the circulation, potentially worsening hyperglycemia.
The liver and kidneys are the only organs that possess the requisite enzymes for gluconeogenesis and that subsequently release newly formed glucose into the circulation.Citation16 In the postabsorptive (fasting) state in healthy humans, renal gluconeogenesis accounts for approximately 20% of total glucose released into the circulation, with the liver contributing the remainder.Citation16,Citation53 It has been suggested that renal glucose synthesis is increased in patients with T2DM relative to healthy individuals.Citation54 Therefore, in patients with T2DM, the kidneys may further exacerbate hyperglycemia by continued glucose reabsorption and increased production of glucose.
Treatment goals
T2DM is a major risk factor for the development of cardiovascular disease,Citation55 as well as microvascular complications, including chronic kidney disease,Citation56 end-stage renal disease requiring dialysis or transplantation,Citation57 and blindness.Citation2 Hyperglycemia is the key determinant of microvascular complications. Randomized controlled trials have shown that intensive glycemic control can reduce the risk of microvascular complications in patients with T2DM.Citation58–Citation60 Therefore, the major treatment goal for T2DM is to reduce hyperglycemia and to manage comorbidities, especially those associated with cardiovascular disease (hypertension and dyslipidemia). Lifestyle changes (diet and exercise) and intensive pharmacotherapy of hyperglycemia and of multiple risk factors substantially reduce the rates of death, cardiovascular events, and progression to end-stage renal disease and retinopathy in patients with T2DM.Citation61
Hyperglycemia should be monitored over the long term by measurement of glycated hemoglobin (A1C) at least twice a year in all patients with diabetes and at least four times yearly in patients who are not at target.Citation62 Management of hyperglycemia should be individualized based on life expectancy, duration of T2DM, presence of comorbidities or vascular complications, potential for hypoglycemia or other adverse events, and patients’ attitudes and access to support systems.Citation62,Citation63 The American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) and the American Association of Clinical Endocrinologists (AACE) recommend general A1C target levels <7.0% and ≤6.5%, respectively, for most patients.Citation62,Citation63 Strict control of blood pressure (BP) and lipids is also recommended.
Pharmacotherapy
Lifestyle changes that include a healthy diet, weight loss, increased physical activity, self-monitoring of blood glucose, and diabetes self-management education have broad benefits in controlling hyperglycemia and cardiovascular risk factors in patients with T2DM.Citation64 Moreover, early intervention with intensive lifestyle changes can prevent or delay the development of T2DM in susceptible individuals.Citation65 However, lifestyle changes may not be adequate to control hyperglycemia in the long term, and most patients will require pharmacotherapy to achieve and maintain glycemic control.Citation64
Patients with T2DM usually require multiple medications to adequately treat their diabetes and associated comorbidities. There is currently no single agent available that affects all seven organs and tissues involved in the pathogenesis of T2DM; most drugs target up to four of the physiologic abnormalities.Citation64 The major classes of drugs, mechanisms of action, and major contraindications are shown in . The ADA/EASD treatment recommendations () stress the importance of individualization of treatment and treatment intensification with combination therapy if A1C goals are not attained. The ADA/EASD recommendations are based on the glucose-lowering effect, actions that may reduce long-term complications, tolerability, safety, ease of use, and expense of glucose-lowering medications.Citation62 The AACE algorithm for the treatment of T2DM also emphasizes the importance of individualized glycemic goals and treatment regimens, and stratifies treatment options based on initial A1C.Citation63
Figure 2 General recommendations for the treatment of type 2 diabetes from the American Diabetes Association/European Association for the Study of Diabetes.
Abbreviations: DPP-4i, dipeptidyl peptidase-4 inhibitor; GLP-1 RA, glucagon-like peptide-1 receptor agonist; A1C, glycated hemoglobin; Met, metformin; SGLT2i, sodium-glucose co-transporter 2 inhibitor; SU, sulfonylurea; TZD, thiazolidinedione.
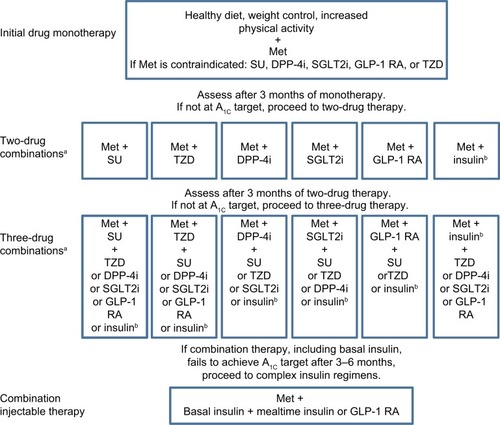
Table 1 Drugs available for type 2 diabetes mellitus
Despite the availability of several glucose-lowering drug classes, a recent survey of patients with diagnosed diabetes from 1999 to 2006 found that only 57% achieved an A1C <7%, and only 12% achieved the recommended A1C, BP, and low-density lipoprotein cholesterol goals.Citation66 The reasons for failure to achieve recommended treatment goals may include lack of treatment initiation and intensification, patient nonadherence,Citation67 and progressive decline in β-cell function, rendering therapies dependent on insulin secretion or action less effective over time.Citation5 Accordingly, new pharmacologic therapies with mechanisms of action that are independent of insulin secretion or action and with acceptable safety profiles and a low risk of hypoglycemia and weight gain may enhance the ability of patients to achieve and maintain glycemic control.
New and emerging therapies
SGLT2 inhibitors
As discussed above, the kidney plays an important role in glucose homeostasis. Inhibition of the major transporter involved in glucose reabsorption by the kidney, SGLT2,Citation68 is an attractive, insulin-independent mechanism for increasing urinary glucose excretion in the setting of hyperglycemia.Citation69 Because the actions of SGLT2 inhibitors are independent of insulin, there is less risk of major hypoglycemic eventsCitation70 compared with agents dependent on insulin action, and there is also the potential for effectiveness in advanced disease. Moreover, increased excretion of glucose and associated calories by SGLT2 inhibitors decreases body weight.Citation71 Finally, there is a potential for combination therapy with other classes of agents with complementary mechanisms of action to optimize treatment.Citation72 However, because the mechanism of action of SGLT2 inhibitors depends on the filtration of glucose by the kidney, as the glomerular filtration rate (GFR) declines, the amount of glucose filtered is reduced, which decreases glucosuria and the efficacy of these drugs.Citation73 A number of selective SGLT2 inhibitors are in various stages of clinical development for the treatment of T2DM.Citation74
Dapagliflozin
Dapagliflozin (AstraZeneca, Wilmington, DE, USA) is approved as a treatment for T2DM in the European Union, USA, and other countries. In Phase III trials, dapagliflozin reduced A1C (up to approximately −0.7%, placebo-corrected), fasting plasma glucose (FPG, up to approximately −27 mg/dL), and in most studies, body weight by 2–3 kg in patients with T2DM who were inadequately controlled with diet and exercise,Citation75 metformin,Citation76,Citation77 glimepiride,Citation78 pioglitazone,Citation79 sitagliptin with and without metformin,Citation80 and insulin.Citation81 In addition, combination of dapagliflozin (5 or 10 mg/day) and metformin extended release as initial therapy in treatment-naïve patients was more effective than either drug alone in reducing A1C; dapagliflozin 10 mg alone was also noninferior to metformin.Citation82 Finally, in patients inadequately controlled with metformin, dapagliflozin (≤10 mg/day) was noninferior to glipizide (≤20 mg/day) in reducing A1C.Citation77
In patients with T2DM and moderate renal impairment (estimated GFR [eGFR] 30–59 mL/min/1.73 m2), mean decreases in A1C were similar for placebo (−0.32%) and for dapagliflozin 5 mg/day (−0.41%) and 10 mg/day (−0.44%) after 24 weeks of treatment.Citation83 Although there was no significant effect on glycemic parameters in these patients, a mean reduction from baseline in body weight was observed with dapagliflozin 5 mg/day (−1.3 kg) and 10 mg/day (−1.7 kg) versus an increase (0.7 kg) with placebo.
In a pooled analysis of 12 Phase II/III trials, dapagliflozin 10 mg/day reduced systolic BP from baseline by −4.4 mmHg and diastolic BP by −2.1 mmHg compared with changes of −0.9 mmHg in systolic BP and −0.5 mmHg in diastolic BP with placebo.Citation84 Dapagliflozin treatment was associated with significant weight reduction of up to 3 kg over 24 weeks.Citation76,Citation78,Citation79,Citation81 The reduction in body weight with dapagliflozin is largely the result of a reduction in body fat.Citation71 The positive effects of dapagliflozin on hyperglycemia and body weight were sustained for up to two years when added to insulinCitation85 or metformin therapy.Citation86,Citation87
Dapagliflozin was generally well tolerated, and adverse events were balanced across treatment groups.Citation75–Citation79,Citation81 There was a low incidence of hypoglycemia when dapagliflozin was used as monotherapyCitation75 or as add-on to metformin,Citation76,Citation77 pioglitazone,Citation79 or sitagliptin.Citation80 The proportion of patients with hypoglycemia was higher in the dapagliflozin groups than in the placebo groups when added to glimepirideCitation78 or insulin therapy,Citation81 and was significantly lower compared with glipizide.Citation77
In a 12-week randomized, double-blind study in patients with T2DM and normal renal function, dapagliflozin 10 mg/day reduced the measured GFR from baseline by −10.8% compared with −2.9% with placebo.Citation88 Mean eGFR decreased from baseline up to week 2 and tended to return toward baseline by 12 weeks. In an analysis of 12 randomized placebo-controlled trials involving more than 4,000 patients with preserved renal function, dapagliflozin was associated with a reduction in eGFR at week 1 that slowly returned to baseline by week 24 and was maintained at that level for 2 years.Citation89 The acute reductions in GFR may be due to reversible hemodynamic effects such as a decrease in BP or plasma volume as a result of the modest diuretic action of dapagliflozin.Citation88 Because of the reduced efficacy in patients with renal impairment, dapagliflozin is not recommended in patients with moderate to severe renal impairment (eGFR <60 mL/min/1.73 m2).Citation84
In data pooled from 12 randomized, placebo-controlled trials, dapagliflozin 2.5, 5, or 10 mg once daily was accompanied by an increased risk of vulvovaginitis or balanitis (4.1%–5.7% versus 0.9% with placebo).Citation90 Diagnosed urinary tract infections occurred more frequently with dapagliflozin 5 mg (5.7%) and 10 mg (4.3%) compared with placebo (3.7%).Citation91
Canagliflozin
Canagliflozin (Janssen Pharmaceuticals, Inc., Titusville, NJ, USA) is approved for the treatment of T2DM in the USA, European Union, and other countries. In Phase III trials, treatment with canagliflozin (100 and 300 mg/day) for 26 or 52 weeks increased glucose excretion and decreased A1C (maximum change versus placebo or comparator −1.16%) and FPG (−43 mg/dL) in patients with T2DM when used as monotherapy,Citation92 as add-on therapy to metformin,Citation93 or as add-on to metformin and sulfonylurea.Citation94 In patients stabilized on metformin, canagliflozin 100 mg/day was noninferior (mean difference −0.01%; 95% confidence interval (CI) −0.11%, 0.09%) and 300 mg/day was superior (mean difference −0.12%; 95% CI −0.22%, −0.02%) to glimepiride (6 to 8 mg/day) in reducing A1C.Citation93 Absolute decreases in body weight of up to 4.2 kg after 52 weeks of therapy with 300 mg/day have been reported.Citation93 Canagliflozin (300 mg/day) as add-on to metformin and sulfonylurea was more effective than sitagliptin (100 mg/day) in reducing body weight, FPG, and systolic BP.Citation95
In patients with T2DM and chronic kidney disease (eGFR ≥30 and <50 mL/min/1.73 m2), treatment with canagliflozin for 26 weeks reduced A1C from baseline by −0.33% with 100 mg/day and by −0.44% with 300 mg/day compared with −0.03% with placebo.Citation96 Transient decreases in eGFR (−4 to −6 mL/min/1.73 m2) with canagliflozin were observed at 3 weeks and trended toward baseline at 26 weeks. As expected, based on the mechanism of action, these reductions in A1C in patients with impaired renal function were less than those reported in patients with normal renal function.Citation92–Citation95,Citation97
In addition to inhibiting SGLT2, canagliflozin is a weak inhibitor of SGLT1, the transporter responsible for intestinal glucose absorption.Citation98 In healthy individuals, canagliflozin reduced postprandial plasma glucose and insulin and delayed the appearance of oral glucose in plasma following a mixed-meal tolerance test.Citation99 These results suggest that canagliflozin reduces postprandial glucose and insulin by increasing renal glucose excretion via SGLT2 inhibition and by delaying the intestinal absorption of glucose, possibly by inhibiting SGLT1.
An increase in symptomatic urinary tract infectionsCitation92,Citation93,Citation96 and genital infectionsCitation92–Citation94,Citation96 was observed with canagliflozin. In addition, canagliflozin was associated with a modest increase in bone fractures and a dose-dependent increase in low-density lipoprotein cholesterol.Citation100
In patients with T2DM without kidney disease (eGFR >55 mL/min/1.73 m2), canagliflozin caused a small initial decrease in eGFR that was stable up to 52 weeks.Citation93 In an analysis of pooled data from four randomized, placebo-controlled trials, canagliflozin caused early transient decreases in eGFR that remained stable or were attenuated over the course of 26 weeks.Citation101 The changes in eGFR with canagliflozin 100 and 300 mg/day versus placebo were −1.6% and −3.0% versus −0.6% in patients <65 years of age and −2.6%, and −2.9% versus −0.4% in patients ≥65 years of age. Canagliflozin should not be used in patients with eGFR <45 mL/min/1.73 m2 and the dose is limited to 100 mg/day in patients with eGFR of 45–<60 mL/min/1.73 m2.Citation102
Empagliflozin
Empagliflozin (Boehringer Ingelheim, Ingelheim, Germany, and Eli Lilly, Indianapolis, IN, USA) is approved in the European Union and USA. In patients with T2DM, empagliflozin increased glucose excretion and decreased FPG (up to −32 mg/dL, placebo-corrected) and A1C (maximum of −0.69%) when used as monotherapy for 12 weeks,Citation103 as add-on to metformin for 12 weeks,Citation104 or as add-on to pioglitazone for 24 weeks.Citation105 As add-on therapy to metformin and sulfonylurea, placebo-corrected changes in A1C and FPG after 24 weeks were −0.65% and −0.60% for empagliflozin 10 and 25 mg/day, respectively.Citation106 Decreases in body weightCitation103–Citation106 and systolic BPCitation106 have also been reported. Improvements in glycemic control and weight reduction were sustained for up to 90 weeks.Citation107 An increased risk of genital and urinary tract infections was observed with empagliflozin.Citation103,Citation104,Citation106,Citation107
Ipragliflozin
Ipragliflozin (Astellas, Tokyo, Japan, and Kotobuki, Hanishina, Japan) is approved in Japan for the treatment of T2DM. In a 12-week dose-ranging study in patients with T2DM, ipragliflozin (12.5, 50, 150, and 300 mg/day) dose-dependently reduced A1C by up to 0.81% (placebo-corrected) and body weight by up to 1.7 kg. A decrease in A1C of −0.72% was seen with metformin.Citation108 In a similarly designed 12-week study in patients inadequately controlled on metformin (≥ 1,500 mg/day), ipragliflozin reduced A1C by a maximum of −0.48% at 300 mg.Citation109 Urinary tract and genital infections, as well as episodes of hypoglycemia, were similar with ipragliflozin and placebo. In patients with impaired renal function ± T2DM, a single dose of ipragliflozin increased urinary glucose excretion in patients with mild (eGFR ≥60 to <90 mL/min/1.73 m2), moderate (eGFR ≥30 to <60 mL/min/1.73 m2), and severe (eGFR ≤15 to <30 mL/min/1.73 m2) renal impairment. However, absolute glucose excretion decreased as eGFR declined.Citation110
Other SGLT2 inhibitors in earlier phases of clinical development that have been reported to have positive effects on glycemic parameters in patients with T2DM include luseogliflozin (Taisho, Tokyo, Japan),Citation111 tofogliflozin (Chugai/Roche, Tokyo, Japan),Citation112 ertugliflozin, (Pfizer, New York, NY, USA)Citation113 and the SGLT2/SGLT1 inhibitor LX4211 (Lexicon Pharmaceuticals, The Woodlands, TX, USA).Citation114
Receptor agonists
GPR119 agonists
The G-protein-coupled receptor (GPR)119 is expressed predominantly in the pancreas (β cells) and gastrointestinal tract in humans.Citation115 Although the endogenous ligand for this receptor is unknown, stimulation with synthetic ligands results in increased release of insulin, GLP-1, and GIP.Citation115 A number of GPR119 agonists are in development for T2DM,Citation116,Citation117 and published findings for JNJ-38431055 (Johnson & Johnson Research & Development, Inc., Raritan, NJ, USA) report that this agent caused an increase in post-meal GLP-1 and GIP in patients with T2DM and was not associated with hypoglycemia.Citation118
Free fatty acid receptor 1 activators
The free fatty acid receptor 1 (FFAR1, also known as GPR40) is expressed mainly in pancreatic β cells.Citation119 Activation of this receptor results in fatty acid–induced glucose-stimulated insulin secretion. In a 12-week Phase II clinical trial, the FFAR1 activator TAK-875 (Takeda, Osaka, Japan) significantly reduced A1C, compared with placebo, with no increase in hypoglycemia.Citation120
11β-hydroxysteroid dehydrogenase type 1 inhibitors
Excess glucocorticoids can cause insulin resistance and, in some individuals, can lead to the development of T2DM.Citation121 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) converts inactive cortisone to cortisol in target tissues. Therefore, inhibition of this enzyme may improve insulin sensitivity. In a randomized, placebo-controlled Phase II study of overweight or obese patients with T2DM exhibiting inadequate glycemic control with metformin, an 11β-HSD1 inhibitor, INCB13739 (Incyte, Wilmington, DE, USA), significantly reduced A1C and FPG compared with placebo.Citation122 Body weight, insulin resistance, and total cholesterol levels were also reduced with treatment.
Summary and conclusion
The significant burden that T2DM imposes on individuals and society reinforces the need for achieving and maintaining glycemic control in these patients. The key to optimal control is early diagnosis and intensive treatment with a combination of agents that address the various pathophysiologic abnormalities in T2DM, thereby lowering fasting and postprandial glucose concentrations. Novel medications with mechanisms of action different from those of most existing drugs and with acceptable safety profiles (low rates of hypoglycemia and no weight gain) are essential for long-term glycemic control and for improving disease outcomes and comorbidities. SGLT2 inhibitors are the newest treatment option for T2DM. These agents improve glycemic control, lower fasting glucose concentrations, and promote weight loss. This new class of diabetes medication with a novel mechanism of action provides an additional option to improve glycemic control in patients with T2DM. Whether the investigational GPR119 agonists, FFAR1 activators, and 11β-HSD1 inhibitors are safe and effective treatments for T2DM will be determined by the results of longer-duration, Phase III studies.
Disclosure
Dr Cornell has received non-continuing medical education honoraria from the Johnson & Johnson Diabetes Insititute and has served on advisory boards for Sanofi, Bristol-Myers Squibb, and AstraZeneca. Editorial support was provided by Richard M Edwards and Janet E Matsuura from Complete Healthcare Communications, Inc., and was funded by Bristol–Myers Squibb and AstraZeneca.
References
- International Diabetes Federation2013IDF Atlas Available from: http://www.idf.org/diabetesatlasAccessed July 10, 2014
- Centers for Disease Control and Prevention2014National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014 Available from: http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdfAccessed July 16, 2014
- RowleyWRBezoldCCreating public awareness: state 2025 diabetes forecastsPopul Health Manag20121519420022283662
- DeFronzoRABanting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitusDiabetes20095877379519336687
- FonsecaVADefining and characterizing the progression of type 2 diabetesDiabetes Care200932S151S15619875543
- WarramJHMartinBCKrolewskiASSoeldnerJSKahnCRSlow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parentsAnn Intern Med19901139099152240915
- MillsGWAveryPJMcCarthyMIHeritability estimates for beta cell function and features of the insulin resistance syndrome in UK families with an increased susceptibility to type 2 diabetesDiabetologia20044773273815298351
- GrantRWMooreAFFlorezJCGenetic architecture of type 2 diabetes: recent progress and clinical implicationsDiabetes Care2009321107111419460916
- KahnSEClinical review 135: the importance of beta-cell failure in the development and progression of type 2 diabetesJ Clin Endocrinol Metab2001864047405811549624
- ChangAMHalterJBAging and insulin secretionAm J Physiol Endocrinol Metab2003284E7E1212485807
- HuFBGlobalization of diabetes: the role of diet, lifestyle, and genesDiabetes Care2011341249125721617109
- PoitoutVRobertsonRPMinireview: secondary beta-cell failure in type 2 diabetes – a convergence of glucotoxicity and lipotoxicityEndocrinology200214333934211796484
- CarpentierAMittelmanSDBergmanRNGiaccaALewisGFProlonged elevation of plasma free fatty acids impairs pancreatic beta-cell function in obese nondiabetic humans but not in individuals with type 2 diabetesDiabetes20004939940810868961
- KashyapSBelfortRGastaldelliAA sustained increase in plasma free fatty acids impairs insulin secretion in nondiabetic subjects genetically predisposed to develop type 2 diabetesDiabetes2003522461247414514628
- UngerRHZhouYTLipotoxicity of beta-cells in obesity and in other causes of fatty acid spilloverDiabetes200150S118S12111272168
- GerichJEMeyerCWoerleHJStumvollMRenal gluconeogenesis: its importance in human glucose homeostasisDiabetes Care20012438239111213896
- HeitJALeibsonCLAshraniAAPettersonTMBaileyKRMeltonLJ3rdIs diabetes mellitus an independent risk factor for venous thromboembolism?: a population-based case-control studyArterioscler Thromb Vasc Biol2009291399140519542020
- ShahPVellaABasuABasuRSchwenkWFRizzaRALack of suppression of glucagon contributes to postprandial hyperglycemia in subjects with type 2 diabetes mellitusJ Clin Endocrinol Metab2000854053405911095432
- HuangSCzechMPThe GLUT4 glucose transporterCell Metab2007523725217403369
- HermanMAKahnBBGlucose transport and sensing in the maintenance of glucose homeostasis and metabolic harmonyJ Clin Invest20061161767177516823474
- CusiKMaezonoKOsmanAInsulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscleJ Clin Invest200010531132010675357
- BaysHMandarinoLDeFronzoRARole of the adipocyte, free fatty acids, and ectopic fat in pathogenesis of type 2 diabetes mellitus: peroxisomal proliferator-activated receptor agonists provide a rational therapeutic approachJ Clin Endocrinol Metab20048946347814764748
- SaelyCHGeigerKDrexelHBrown versus white adipose tissue: a mini-reviewGerontology201258152321135534
- CypessAMLehmanSWilliamsGIdentification and importance of brown adipose tissue in adult humansN Engl J Med20093601509151719357406
- SaitoMOkamatsu-OguraYMatsushitaMHigh incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposityDiabetes2009581526153119401428
- van Marken LichtenbeltWDVanhommerigJWSmuldersNMCold-activated brown adipose tissue in healthy menN Engl J Med20093601500150819357405
- VirtanenKALidellMEOravaJFunctional brown adipose tissue in healthy adultsN Engl J Med20093601518152519357407
- OuelletVLabbeSMBlondinDPBrown adipose tissue oxidative metabolism contributes to energy expenditure during acute cold exposure in humansJ Clin Invest201212254555222269323
- BostromPWuJJedrychowskiMPA PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesisNature201248146346822237023
- PagottoUWhere does insulin resistance start? The brainDiabetes Care200932S174S17719875547
- TschritterOPreisslHHennigeAMThe cerebrocortical response to hyperinsulinemia is reduced in overweight humans: a magnetoencephalographic studyProc Natl Acad Sci U S A2006103121031210816877540
- RothJDMaierHChenSRolandBLImplications of amylin receptor agonism: integrated neurohormonal mechanisms and therapeutic applicationsArch Neurol20096630631019273748
- WoodsSCLutzTAGearyNLanghansWPancreatic signals controlling food intake; insulin, glucagon and amylinPhilos Trans R Soc Lond B Biol Sci20063611219123516815800
- FriedmanJMLeptin at 14 y of age: an ongoing storyAm J Clin Nutr200989973S979S19190071
- ConsidineRVSinhaMKHeimanMLSerum immunoreactive-leptin concentrations in normal-weight and obese humansN Engl J Med19963342922958532024
- MortonGJSchwartzMWLeptin and the central nervous system control of glucose metabolismPhysiol Rev20119138941121527729
- FarooqiISO’RahillySLeptin: a pivotal regulator of human energy homeostasisAm J Clin Nutr200989980S984S19211814
- GermanJPWisseBEThalerJPLeptin deficiency causes insulin resistance induced by uncontrolled diabetesDiabetes2010591626163420424233
- MittendorferBHorowitzJFDePaoliAMMcCamishMAPattersonBWKleinSRecombinant human leptin treatment does not improve insulin action in obese subjects with type 2 diabetesDiabetes2011601474147721411512
- HeppnerKMTongJMechanisms in endocrinology: regulation of glucose metabolism by the ghrelin system: multiple players and multiple actionsEur J Endocrinol2014171R21R3224714083
- DateYNakazatoMHashiguchiSGhrelin is present in pancreatic alpha-cells of humans and rats and stimulates insulin secretionDiabetes20025112412911756331
- VolanteMAlliaEGugliottaPExpression of ghrelin and of the GH secretagogue receptor by pancreatic islet cells and related endocrine tumorsJ Clin Endocrinol Metab2002871300130811889202
- BroglioFArvatEBensoAGhrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humansJ Clin Endocrinol Metab2001865083508611600590
- TongJPrigeonRLDavisHWGhrelin suppresses glucose-stimulated insulin secretion and deteriorates glucose tolerance in healthy humansDiabetes2010592145215120584998
- GarinMCBurnsCMKaulSCappolaARClinical review: the human experience with ghrelin administrationJ Clin Endocrinol Metab2013981826183723533240
- PöykköSMKellokoskiEHörkköSKaumaHKesäniemiYAUkkolaOLow plasma ghrelin is associated with insulin resistance, hypertension, and the prevalence of type 2 diabetesDiabetes2003522546255314514639
- FreemanJSRole of the incretin pathway in the pathogenesis of type 2 diabetes mellitusCleve Clin J Med200976S12S1919952298
- NauckMABallerBMeierJJGastric inhibitory polypeptide and glucagon-like peptide-1 in the pathogenesis of type 2 diabetesDiabetes200453S190S19615561910
- DunganKBuseJBGlucagon-like peptide 1–based therapies for type 2 diabetes: a focus on exenatideClin Diabetes2005235662
- BakrisGLFonsecaVASharmaKWrightEMRenal sodium-glucose transport: role in diabetes mellitus and potential clinical implicationsKidney Int2009751272127719357717
- FerranniniESodium-glucose transporter-2 inhibition as an antidiabetic therapyNephrol Dial Transplant2010252041204320466683
- DeFronzoRAHompeschMKasichayanulaSCharacterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetesDiabetes Care2013363169317623735727
- StumvollMChintalapudiUPerrielloGWelleSGutierrezOGerichJUptake and release of glucose by the human kidney. Postabsorptive rates and responses to epinephrineJ Clin Invest199596252825337593645
- MeyerCStumvollMNadkarniVDostouJMitrakouAGerichJAbnormal renal and hepatic glucose metabolism in type 2 diabetes mellitusJ Clin Invest19981026196249691098
- FoxCSCoadySSorliePDIncreasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart StudyCirculation20071151544155017353438
- CoreshJSelvinEStevensLAPrevalence of chronic kidney disease in the United StatesJAMA20072982038204717986697
- FoleyRNCollinsAJEnd-stage renal disease in the United States: an update from the United States Renal Data SystemJ Am Soc Nephrol2007182644264817656472
- OhkuboYKishikawaHArakiEIntensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year studyDiabetes Res Clin Pract1995281031177587918
- No authors listedEffect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) GroupLancet1998a3528548659742977
- No authors listedIntensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) GroupLancet1998b3528378539742976
- GaedePLund-AndersenHParvingHHPedersenOEffect of a multifactorial intervention on mortality in type 2 diabetesN Engl J Med200835858059118256393
- American Diabetes AssociationApproaches to glycemic treatment. Sec 7. In Standards of medical care in diabetes – 2015Diabetes Care201538Suppl 1S41S4825537707
- GarberAJAbrahamsonMJBarzilayJIAmerican Association of Clinical Endocrinologists’ comprehensive diabetes management algorithm 2013 consensus statement – executive summaryEndocr Pract20131953655723816937
- NathanDMBuseJBDavidsonMBAmerican Diabetes AssociationEuropean Association for Study of DiabetesMedical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of DiabetesDiabetes Care20093219320318945920
- KnowlerWCBarrett-ConnorEFowlerSEDiabetes Prevention Program Research GroupReduction in the incidence of type 2 diabetes with lifestyle intervention or metforminN Engl J Med200234639340311832527
- CheungBMOngKLChernySSShamPCTsoAWLamKSDiabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006Am J Med200912244345319375554
- SchmittdielJAUratsuCSKarterAJWhy don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensificationJ Gen Intern Med20082358859418317847
- VallonVPlattKACunardRSGLT2 mediates glucose reabsorption in the early proximal tubuleJ Am Soc Nephrol20112210411220616166
- ListJFWhaleyJMGlucose dynamics and mechanistic implications of SGLT2 inhibitors in animals and humansKidney Int201179S20S27
- GerichJERole of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implicationsDiabet Med20102713614220546255
- BolinderJLjunggrenOKullbergJEffects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metforminJ Clin Endocrinol Metab2012971020103122238392
- BaileyCJSGLT2 inhibitors: glucuretic treatment for type 2 diabetesBr J Diabetes Vasc Dis201010193199
- Abdul-GhaniMANortonLDefronzoRARole of sodium-glucose cotransporter 2 (SGLT 2) inhibitors in the treatment of type 2 diabetesEndocr Rev20113251553121606218
- ChaoECHenryRRSGLT2 inhibition – a novel strategy for diabetes treatmentNat Rev Drug Discov2010955155920508640
- FerranniniERamosSJSalsaliATangWListJFDapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trialDiabetes Care2010332217222420566676
- BaileyCJGrossJLPietersABastienAListJFEffect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trialLancet20103752223223320609968
- NauckMADel PratoSMeierJJDapagliflozin versus glipizide as add-on therapy in patients with type 2 diabetes who have inadequate glycemic control with metformin: a randomized, 52-week, double-blind, active-controlled noninferiority trialDiabetes Care2011342015202221816980
- StrojekKYoonKHHrubaVElzeMLangkildeAMParikhSEffect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomized, 24-week, double-blind, placebo-controlled trialDiabetes Obes Metab20111392893821672123
- RosenstockJVicoMWeiLSalsaliAListJFEffects of dapagliflozin, an SGLT2 inhibitor, on HbA1c, body weight, and hypoglycemia risk in patients with type 2 diabetes inadequately controlled on pioglitazone monotherapyDiabetes Care2012351473147822446170
- JabbourSHardyESuggJEParikhSDapagliflozin as add-on therapy to sitagliptin with or without metformin: a randomized, double-blind, placebo-controlled studyDiabetes201261A275
- WildingJPHWooVSolerNGDapagliflozin 006 Study GroupLong-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulinAnn Intern Med2012b15640541522431673
- HenryRRMurrayAVMarmolejoMHHennickenDPtaszynskaAListJFDapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trialInt J Clin Pract20126644645622413962
- KohanDEFiorettoPTangWListJFLong-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic controlKidney Int20148596297124067431
- Farxiga® (dapagliflozin). 2014Full Prescribing InformationPrinceton NJ, USABristol-Myers SquibbWilmington, DE, USAAstraZeneca2014
- WildingJPWooVRohwedderKSuggJParikhSDapagliflozin 006 Study GroupDapagliflozin in patients with type 2 diabetes receiving high doses of insulin: efficacy and safety over two yearsDiabetes Obes Metab20141612413623911013
- BaileyCJGrossJLHennickenDIqbalNMansfieldTAListJFDapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trialBMC Med2013114323425012
- BolinderJLjunggrenOJohanssonLDapagliflozin maintains glycaemic control while reducing weight and body fat mass over 2 years in patients with type 2 diabetes mellitus inadequately controlled on metforminDiabetes Obes Metab20141615916923906445
- Lambers HeerspinkHJde ZeeuwDWieLLeslieBListJDapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetesDiabetes Obes Metab20131585386223668478
- PtaszynskaAChalamandarisASuggJEJohnssonKMParikhSListJLEffect of dapagliflozin on renal functionDiabetes201261A283
- JohnssonKMPtaszynskaASchmitzBSuggJParikhSJListJFVulvovaginitis and balanitis in patients with diabetes treated with dapagliflozinJ Diabetes Complications2013b2747948423806570
- JohnssonKMPtaszynskaASchmitzBSuggJParikhSJListJFUrinary tract infections in patients with diabetes treated with dapagliflozinJ Diabetes Complications2013a2747347823849632
- StenlofKCefaluWTKimKAEfficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exerciseDiabetes Obes Metab20131537238223279307
- CefaluWTLeiterLAYoonKHEfficacy and safety of canagliflozin versus glimepiride in patients with type 2 diabetes inadequately controlled with metformin (CANTATA-SU): 52 week results from a randomised, double-blind, phase 3 non-inferiority trialLancet201338294195023850055
- WildingJPMathieuCVercruysseFCanagliflozin (CANA), a sodium glucose co-transporter 2 inhibitor, improves glycemic control and reduces body weight in subjects with type 2 diabetes (T2D) inadequately controlled with metformin (MET) and sulfonylurea (SU)Diabetes2012a61A262
- SchernthanerGGrossJLRosenstockJCanagliflozin compared with sitagliptin for patients with type 2 diabetes who do not have adequate glycemic control with metformin plus sulfonylurea: a 52-week randomized trialDiabetes Care2013362508251523564919
- YaleJFBakrisGCariouBEfficacy and safety of canagliflozin in subjects with type 2 diabetes and chronic kidney diseaseDiabetes Obes Metab20131546347323464594
- RosenstockJPolodoriDZhaoYCanagliflozin, an inhibitor of sodium glucose co-transporter 2, improves glycaemic control, lowers body weight, and improves beta cell function in subjects with type 2 diabetes on background metforminDiabetologia2010b53S351
- WrightEMLooDDHirayamaBABiology of human sodium glucose transportersPhysiol Rev20119173379421527736
- PolidoriDShaSMudaliarSCanagliflozin lowers postprandial glucose and insulin by delaying intestinal glucose absorption in addition to increasing urinary glucose excretion: results of a randomized, placebo-controlled studyDiabetes Care2013362154216123412078
- US Food Drug AdministrationEndocrinologic and Metabolic Drugs Advisory Committee1102013 Available from: http://www.fda.gov/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/EndocrinologicandMetabolicDrugsAdvisoryCommittee/ucm331504.htmAccessed July 16, 2014
- SinclairABodeBHarrisSEfficacy and safety of canagliflozin compared with placebo in older patients with type 2 diabetes mellitus: a pooled analysis of clinical studiesBMC Endocr Disord2014143724742013
- Invokana® (canagliflozin)Full Prescribing InformationTitusville, NJ, USAJanssen Pharmaceuticals2013
- FerranniniESemanLSeewaldt-BeckerEHantelSPinnettiSWoerleHJA Phase IIb, randomized, placebo-controlled study of the SGLT2 inhibitor empagliflozin in patients with type 2 diabetesDiabetes Obes Metab2013a1572172823398530
- RosenstockJSemanLJJelaskaAEfficacy and safety of empagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, as add-on to metformin in type 2 diabetes with mild hyperglycaemiaDiabetes Obes Metab2013151154116023906374
- KovacsCSSeshiahVSwallowREMPA-REG PIO™ trial investigatorsEmpagliflozin improves glycaemic and weight control as add-on therapy to pioglitazone or pioglitazone plus metformin in patients with type 2 diabetes: a 24-week, randomized, placebo-controlled trialDiabetes Obes Metab20141614715823906415
- HaringHUMerkerLSeewaldt-BeckerEEMPA-REG METSU Trial InvestigatorsEmpagliflozin as add-on to metformin plus sulfonylurea in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trialDiabetes Care2013363396340423963895
- WoerleHJFerranniniEBerkASafety and efficacy of empagliflozin as monotherapy or add-on to metformin in a 78-week open-label extension study in patients with type 2 diabetesDiabetes201261LB13
- FonsecaVAFerranniniEWildingJPActive- and placebo-controlled dose-finding study to assess the efficacy, safety, and tolerability of multiple doses of ipragliflozin in patients with type 2 diabetes mellitusJ Diabetes Complications20132726827323276620
- WildingJPFerranniniEFonsecaVAWilpshaarWDhanjalPHouzerAEfficacy and safety of ipragliflozin in patients with type 2 diabetes inadequately controlled on metformin: a dose-finding studyDiabetes Obes Metab2013a1540340923163880
- FerranniniEVeltkampSASmuldersRAKadokuraTRenal glucose handling: impact of chronic kidney disease and sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetesDiabetes Care2013b361260126523359360
- SeinoYSasakiTFukatsuASamukawaYSakaiSWatanabeTLuseogliflozin (TS-071), a selective SGLT2 inhibitor, improves glycemic control and lowers body weight in Japanese patients with type 2 diabetes mellitusDiabetes201261A266
- KadowakiTIkedaSTakanoYTofogliflozin, a novel and selective SGLT2 inhibitor improves glycemic control and lowers body weight in patients with type 2 diabetes mellitus inadequately controlled on stable metformin or diet and excercise aloneDiabetes201261A22
- MandemaJSweeneyKTerraSSahasrabudheVModel-based meta-analysis of the HbA1c lowering effect of PF-04971729, a sodium glucose co-transporter-2 inhibitor (SGLT2i), in comparison with other SGLT2i and anti-diabetic agents (ADA)Diabetes201261A260
- ZambrowiczBFreimanJBrownPMLX4211, a dual SGLT1/SGLT2 inhibitor, improved glycemic control in patients with type 2 diabetes in a randomized, placebo-controlled trialClin Pharmacol Ther20129215816922739142
- OvertonHAFyfeMCReynetCGPR119, a novel G protein-coupled receptor target for the treatment of type 2 diabetes and obesityBr J Pharmacol2008153S76S8118037923
- GlaxoSmithKlineA study in type 2 diabetics of single and multiple doses of orally administered GSK1292263 to investigate the safety, tolerability, pharmacokinetics and pharmacodynamics Available from: http://clinicaltrials.gov/ct2/show/NCT01119846?term=gsk1292263&rank=1Accessed July 16, 2014
- CymaBay Therapeutics IncStudy to evaluate the efficacy, safety, tolerability, and pharmacokinetics of MBX-2982 administered daily for 4 weeks as monotherapy in patients with type 2 diabetes Available from: http://clinicaltrials.gov/ct2/show/NCT01035879?term=mbx2982&rank=1Accessed July 16, 2014
- KatzLBGambaleJJRothenbergPLEffects of JNJ-38431055, a novel GPR119 receptor agonist, in randomized, double-blind, placebo-controlled studies in subjects with type 2 diabetesDiabetes Obes Metab20121470971622340428
- KebedeMAAlquierTLatourMGPoitoutVLipid receptors and islet function: therapeutic implications?Diabetes Obes Metab200911102019817784
- BurantCFViswanathanPMarcinakJTAK-875 versus placebo or glimepiride in type 2 diabetes mellitus: a phase 2, randomised, double-blind, placebo-controlled trialLancet20123791403141122374408
- CooperMSStewartPM11Beta-hydroxysteroid dehydrogenase type 1 and its role in the hypothalamus-pituitary-adrenal axis, metabolic syndrome, and inflammationJ Clin Endocrinol Metab2009944645465419837912
- RosenstockJBanarerSFonsecaVAINCB13739-202 Principal InvestigatorsThe 11-beta-hydroxysteroid dehydrogenase type 1 inhibitor INCB13739 improves hyperglycemia in patients with type 2 diabetes inadequately controlled by metformin monotherapyDiabetes Care2010a331516152220413513
- InzucchiSEBergenstalRMBuseJBAmerican Diabetes Association (ADA)European Association for the Study of Diabetes (EASD)Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association and the European Association for the Study of DiabetesDiabetes Care2012351364137922517736
- InzucchiSEBergenstalRMBuseJBManagement of hyperglycemia in type 2 diabetes 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of DiabetesDiabetes Care20153814014925538310
- BlondeLCurrent antihyperglycemic treatment strategies for patients with type 2 diabetes mellitusCleve Clin J Med200976Suppl 5S4S1119952303
- ZangenehFKudvaYCBasuAInsulin sensitizersMayo Clin Proc20037847147912683699
- Welchol® (colesevelam HCl)Full Prescribing InformationParsippany, NJ, USADaiichi Sankyo, Inc2010
- Cycloset® (bromocriptine mesylate)Full Prescribing InformationTiverton, RIVeroScience, LLC2010
