Abstract
Denosumab is a breakthrough biological drug approved by the Food and Drug Administration and European Medicines Agency for the treatment of osteoporosis in 2010. It is a fully human monoclonal antireceptor activator of nuclear factor kappa-B ligand antibody, which inhibits the activity of osteoclasts, resulting in an antiresorptive effect with a significant increase in bone mineral density. The FREEDOM (Fracture Reduction Evaluation of Denosumab in Osteoporosis every 6 Months) trial, comparing denosumab with no treatment in 7868 women with postmenopausal osteoporosis, showed an important reduction of fracture risk at hip, vertebral, and nonvertebral sites in the treated group, while no statistically significant difference in the incidence of adverse events was detected between denosumab and placebo groups. The specific action of denosumab directed against a key regulator of osteoclasts makes it a valuable tool in preventing the occurrence of skeletal events caused by bone destruction in patients with advanced malignancies. The drug was approved for postmenopausal osteoporosis in women at increased risk of fracture and for the treatment of bone loss associated with androgen deprivation therapy in men with prostate cancer.
Introduction
The aim of osteoporosis treatment is to reduce as far as possible the risk of bone fracture. Osteoporosis, the most common metabolic bone disease, is characterized by low bone mineral density (BMD) and microarchitectural deterioration of bone tissue with a consequent increase in the susceptibility to fragility fractures. It has become an increasingly important public health problem due to the rapidly aging population. Currently, every third postmenopausal woman and every fifth man older than 50 years suffer from osteoporosis.Citation1
It should be important to identify the possible pathological mechanisms underlying bone fragility, especially in populations at risk such as the elderly and postmenopausal women. Bone strength, ie, resistance to fracture, depends not only on bone mass, but also on its spatial distribution and the intrinsic properties of the materials that constitute the bone.Citation1,Citation2
Data from the National Osteoporosis Risk Assessment study revealed that only 6.4% of postmenopausal women with an osteoporotic fracture had T-score (the standard deviation difference between the patient’s BMD and the mean BMD of a female young adult reference population) of less than −2.5 (World Health Organization definition of osteoporosis) in the year preceding the fracture.Citation3,Citation4
More than one-half (52%) of the women with fractures were osteopenic (T-score −2.5 to −1)Citation3,Citation4 and, similarly, the increase in BMD achieved through the treatments for osteoporosis seemed to account for only part of the reduction of fracture risk observed.Citation4,Citation5
Knowledge of the molecular bases of bone metabolism would be essential to formulate drugs that act not only on BMD but also on bone quality, especially in order to reduce fracture risk. Moreover, as described below, prescription of the therapy for osteoporosis, which must be specific to the individual patient, should be the result of the evaluation of multiple factors, such as age, sex, severity of osteoporosis, bone turnover markers (bone formation or resorption), patient compliance, allergies to medications, and contraindications or side effects of drugs.
Behind the choice of the most appropriate therapy, is the concept of bone as a dynamic tissue, which has the ability to adapt its shape and size in response to mechanical loads through modeling process, and to be constantly renewed by remodeling phenomenon.Citation1,Citation6 Remodeling process allows the skeleton to maintain mechanical integrity through constant osteoclastic resorption of damaged bone followed by osteoblast-mediated deposition and mineralization of new matrix.
Antiosteoporosis drugs can be classified on the basis of their action on bone remodeling.Citation7 Antiresorptive drugs (such as bisphosphonates, raloxifene – a selective estrogen receptor modulator, and denosumab) decrease bone remodeling and reduce fractures by preserving skeletal microarchitecture and moderately increasing bone mass.Citation1 Anabolic drugs, such as teriparatide or parathyroid hormone (PTH) 1–84, on the other hand, reduce fractures by enhancing remodeling. In addition to increasing BMD, they appear to repair bone microarchitecture and improve bone geometry.Citation1 Strontium ranelate, available for osteoporosis in Europe, decouples the two processes, inhibiting bone resorption and stimulating bone formation.Citation1 The evidence for this suggested mechanism of action of strontium ranelate has been largely acquired from in vitro and animal studies, where doses 30 times higher than those appropriate for men were used.Citation8 However, bone anabolic effect has not been demonstrated in animals treated with doses of strontium ranelate comparable to the marketed dose,Citation9 nor in human paired bone biopsies by clinical studies.Citation1
A large body of scientific evidence derives from randomized controlled trials concerning the treatment of postmenopausal osteoporosis. Three different aminobisphosphonates (alendronate, risedronate, and zoledronate), teriparatide, strontium ranelate, and hormone replacement therapy – which is no longer recommended for the prevention or treatment of osteoporosis – were shown to be effective against both vertebral and nonvertebral fractures. Evidence of efficacy against vertebral fractures is available for ibandronate (an aminobisphosphonate), raloxifene, and PTH 1–84.Citation1,Citation10 shows the site of action and effect on BMD and bone turnover of the most commonly used antiosteoporosis drugs.
Table 1 Osteoporosis therapies in useCitation1
In women with osteoporosis, each 1% improvement in spine BMD (measured by dual X-ray absorptiometry) is expected to reduce vertebral fracture risk by about 4%. However, randomized trials of antiresorptive agents show that 1%–6% improvements in spine BMD reduce vertebral fracture risk by 35%–50%. Less than 20% of the decreased spine fracture risk produced by alendronate or raloxifene can be explained by improvement in spine BMD. The discrepancy is even greater during the first year or two of treatment when 1%–4% improvements in BMD are associated with 65%–68% decreases in spine fracture risk. Bisphosphonates continue to increase BMD but the reduction in fracture risk wanes to 20%–45%. Dual X-ray absorptiometry underestimates the change in bone density of spinal trabecular bone, which might explain part of the discrepancy between expected and observed reductions in spine fracture risk. Even more accurate measurements of BMD would not explain the rapid onset and later waning of effect despite gradually increasing BMD.Citation11
The effect of drugs on nonspine fracture risk is more complex and cannot be predicted from changes in dual X-ray absorptiometry BMD. Long-term use (>10 years) of estrogen, for example, has been associated with >50% reduction in risk of hip and wrist fracture, which could not be explained by improvements in BMD, and increased section modulus versus nonusers with a net increase in predicted femoral neck strength despite losing about 0.4% per year in femoral neck BMD.Citation12 PTH reduces spine fracture risk and this effect is more completely explained by improvement in spine BMD. This suggests that sustaining increased BMD produced by PTH may maintain long-term reduction in fracture risk.
The choice of the most appropriate therapy for individual patients should be based on the level of turnover rate indicated by biochemical markers, therefore preferring an anticatabolic drug in the case of high bone turnover postmenopausal woman and an anabolic or decoupling drug in an old patient with low turnover indices or a very low spinal and/or hip BMD. Importantly, patients’ compliance with medical therapy should be considered when choosing drugs with a certain frequency of administration.Citation1
Alendronate, risedronate, and ibandronate were marketed with administration schedules that increasingly simplified oral therapy from once daily to weekly and then to monthly. A third-generation bisphosphonate, zoledronate, is provided in the form of a brief intravenous infusion administered yearly. The therapeutic plan for PTH involves daily subcutaneous administration performed at the same time for a maximum period of 24 consecutive months overall. Denosumab, the latest one on the market, requires a subcutaneous injection every 6 months.
Moreover, osteoporosis type (postmenopausal, senile, or secondary to pathologies or to the use of drugs), potential side effects, allergies, drug-specific contraindications, and the cost of treatment should be considered.Citation1
The different drug classes: mechanisms of action
Bisphosphonates
Bisphosphonates are antiresorptive agents which act via the inhibition of osteoclasts, leading to reduced bone turnover, increased bone mass, and improved mineralization.Citation13
Bisphosphonates are chemically stable analogues of inorganic pyrophosphate; publications of their biological effects began in 1969.Citation14 Studies on the role of inorganic pyrophosphate as the body’s natural “water softener” in the control of soft tissue and skeletal mineralization led to the need to find inhibitors of calcification that would resist hydrolysis by alkaline phosphatase.Citation14 The observation that inorganic pyrophosphate and bisphosphonates could not only retard the growth but also the dissolution of hydroxyapatite crystals prompted studies on their ability to inhibit bone resorption.Citation14 Although inorganic pyrophosphate was unable to do this, bisphosphonates turned out to be remarkably effective inhibitors of bone resorption in both in vitro and in vivo experimental systems, and eventually in humans. As more potent bisphosphonates were synthesized and studied, it became apparent that physicochemical effects were insufficient to explain their biological effects and that cellular actions must be involved. Despite many attempts, it was not until the 1990s that their biochemical actions were elucidated. Selectively taken up and adsorbed to mineral surfaces in bone, bisphosphonates are internalized by the bone-resorbing osteoclasts and interfere with specific biochemical processes.
Bisphosphonates can be classified into at least two groups with different molecular modes of action. The simpler nonnitrogen-containing bisphosphonates (such as etidronate and clodronate) can be metabolically incorporated into non-hydrolysable analogues of adenosine triphosphate, which interfere with adenosine triphosphate-dependent intracellular pathways.Citation14 The more potent nitrogen-containing bisphosphonates (including pamidronate, alendronate, risedronate, ibandronate, and zoledronate) are not metabolized in this way but inhibit key enzymes of the mevalonate/cholesterol biosynthetic pathway, such as farnesyl pyrophosphate synthase. They therefore interfere with geranylgeranylation (attachment of the lipid to regulatory proteins) and with the biosynthesis of isoprenoid compounds (notably farnesol and geranylgeraniol) that are required for posttranslational prenylation of small guanosine triphosphate-binding proteins (which are also guanosine triphosphatases), essential intracellular messengers, thus causing osteoclast inactivation. Citation13,Citation14 Loss of geranylgeranylation leads to osteoclast apoptosis,Citation15,Citation16 disruption of the actin cytoskeleton, and altered membrane trafficking.Citation13,Citation17–Citation19 This mechanism is responsible for nitrogen-containing bisphosphonate suppression of osteoclastic bone resorption and reduction of bone turnover, which leads to fracture prevention.Citation13
Because of the appearance in humans of gastrointestinal adverse events after oral administration of nitrogen-containing bisphosphonates,Citation20 the effects of oral bisphosphonates were examined in special studies in animals. Suprapharmacologic doses of alendronate administered orally to rats have been reported to induce gastric and esophageal erosions and ulcerations, as well as delay healing of indomethacin-induced gastric erosions. These effects were not attributable to changes in gastric acid secretion or prostaglandin synthesis, but are thought to be due to a topical irritant effect. Similar effects were reported with etidronate, risedronate, and tiludronate when given at pharmacologically equivalent doses.Citation13,Citation21–Citation23
Accumulation of the upstream metabolite, isopentenyl pyrophosphate, as a result of inhibition of farnesyl pyrophosphate synthase may be responsible for immunomodulatory effects on gamma delta T cells, and can also lead to production of another adenosine triphosphate metabolite called ApppI, which has intracellular actions.Citation14
Bisphosphonates are established as the treatments of choice for various diseases of excessive bone resorption, including Paget’s disease of bone, skeletal complications of malignancy, and primarily osteoporosis.
Recently, it has been suggested that in addition to inhibiting osteoclasts, bisphosphonates (specifically alendronate) may also promote osteoblast proliferation and maturation.Citation4,Citation24 The evidence base for bisphosphonates in the prevention of fracture in postmenopausal women is well established.Citation4 Treatment with alendronate 10 mg/day resulted in statistically significant reductions in vertebral, nonvertebral, hip, and wrist fractures in patients with prior osteoporotic fracture or low BMD. For those patients without osteoporotic fracture or low BMD, treatment with alendronate resulted in a significant reduction in vertebral, but not other sites, fracture.Citation4,Citation25 Similar is the antifracture efficacy of risedronate 5 mg/day, although the reduction in wrist fractures in patients with prior fracture or low BMD was not statistically significant and there was no significant benefit in patients with normal BMD.Citation4,Citation26 Treatment with a once-yearly infusion of zoledronate (5 mg) significantly reduces the risk of vertebral, nonvertebral, hip, and wrist fracture in postmenopausal women with osteoporosis.Citation4,Citation27 In contrast, ibandronate in women with postmenopausal osteoporosis has shown a significant reduction in vertebral fracture only.Citation4,Citation28
Bisphosphonates improve trabecular microarchitecture; however, they have a relatively small effect on cortical bone. Trabecular microarchitecture is improved (greater bone volume, greater trabecular thickness, decreased trabecular spacing) after 2–3 years of alendronate treatment compared with placebo,Citation29 or after 1 year of treatment with risedronate.Citation30
In regards to the optimal treatment period, it should be considered that both alendronate and zoledronate bind strongly to the bone matrix and become internalized within bone; therefore, suppression of bone resorption continues even after treatment ends. There have been recent concerns that long-term suppression of bone remodeling and increased mineralization may result in detrimental changes to bone quality and accumulation of damage.Citation4,Citation31
Postmenopausal osteoporosis is a chronic disease requiring long-term management. While most antiosteoporotic treatments have been tested in 3–5-year studies, it should be crucial to assess the long-term safety and efficacy of these agents.Citation32
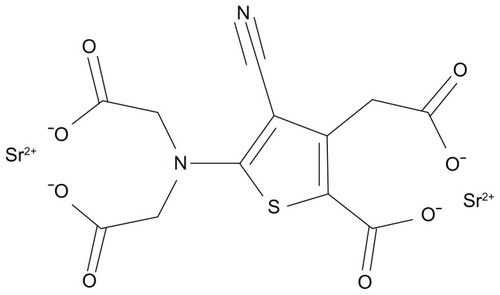
Strontium ranelate
Strontium ranelate is a divalent strontium salt comprised of two molecules of stable strontium and one molecule of ranelic acid ().Citation33,Citation34 It is a bone-seeking agent capable of increasing bone formation and reducing bone resorption, thereby uncoupling and rebalancing bone turnover in favor of bone formation.Citation33–Citation35
Strontium ranelate has been shown to increase bone formation in vitro, enhancing preosteoblastic cell replication and osteoblastic differentiation and decreasing abilities of osteoblasts to induce osteoclastogenesis via the calcium-sensing receptor and an increase in the osteoprotegerin (OPG)/ receptor activator of nuclear factor kappa-B (RANK) ligand (RANKL) ratio.Citation36 In human primary osteoblasts, strontium ranelate downregulated the expression of RANKL (which induces the differentiation of mature osteoclasts and increases osteoclast survival) and enhanced OPG expression (which inhibits RANKL-induced osteoclastogenesis), thus reducing osteoclastogenesis.Citation34
Strontium, like calcium, acts as an agonist at the calcium-sensing receptor, promoting replication,Citation36 differentiation,Citation36,Citation37 and survivalCitation36 of rodentCitation37,Citation38 or humanCitation36 primary osteoblasts. The drug triggers mitogenic signals, such as the activation of protein kinase C and p38 mitogen-activated protein kinase,Citation39 and enhances the expression of c-Fos and EGR-1 genes, involved in osteoblast replication.Citation37 The drug may act independently of the calcium-sensing receptor by protecting primary osteoblasts against apoptosis, thereby promoting osteoblastogenesis – partly via extracellular signal-related kinases 1/2 and Akt signaling – and prostaglandin E2 production.Citation34,Citation40
In rats,Citation8 2 years’ treatment with strontium ranelate increased bone resistance (assessed by a compression test) and trabecular and cortical bone mass (as shown by ash weight and areal BMD in the vertebra and femur), with an improvement in bone microarchitecure.Citation8,Citation34 Similar effects were observed in women with postmenopausal osteoporosis in whom oral administration of strontium ranelate 2 g/day led to continued increases in BMD at all sites, proving efficacy against vertebral and nonvertebral fracture over 5 years, as demonstrated in the SOTI (Spinal Osteoporosis Therapeutic Intervention) trialCitation41 and in the TROPOS (Treatment of Peripheral Osteoporosis) trial,Citation42,Citation43 though many women required longer-term treatment.Citation32 No studies have been performed on strontium ranelate efficacy on men.
PTH
Until the advent of teriparatide (human recombinant PTH 1–34), the only available therapies for the treatment of osteoporosis worked by primarily inhibiting bone resorption (bisphosphonates, raloxifene, and estrogen), which decrease the rate of bone turnover by reducing the level of bone resorption with a subsequent reduction of bone formation activity.Citation44,Citation45
There is evidence from randomized controlled trials on the efficacy of anti-resorptives in reducing the risk of fracture, but none of these agents completely abolish fracture risk. Although they reduce fracture risk, particularly in the spine, there is no increase in bone formation or restoration of architectural bone tissue damage after treatment.Citation46 Enhancement of bone formation may be provided by anabolic therapies.
PTH, the major hormonal regulator of calcium homeostasis, is a potent stimulator of bone formation and can restore bone to an osteopenic skeleton when administered intermittently. Citation1 Osteoblasts are the primary target cells for the anabolic effects of PTH in bone tissue. Anabolic effects of PTH on bone have been demonstrated in animals and humans by numerous measurement techniques including BMD and bone histomorphometry. Recently, two-dimensional and three-dimensional assessments of cancellous bone structure have shown that PTH can reestablish lost trabecular connectivity in animals and humans by a novel mechanism in which trabeculae are first thickened and then split by longitudinal tunneling.Citation47
These results provide new insight into the positive clinical effects of PTH in osteoporosis. In recent randomized controlled clinical trials of intermittent PTH treatment, PTH decreased incidence of vertebral and nonvertebral fractures in postmenopausal women. Thus, PTH shows strong potential as therapy for osteoporosis. However, two-dimensional and three-dimensional structural analysis of advanced osteopenia in animals has shown that there is a critical limit of trabecular connectivity and bone strength below which PTH cannot completely reverse the condition. Given that PTH treatment fails to completely restore trabecular connectivity and bone strength in animals with advanced osteopenia, early treatment of osteoporosis appears important and efficacious for preventing fractures caused by decreased trabecular connectivity.Citation48
The beneficial effect of introducing a treatment with antiresorptives after a treatment course with teriparatide or PTH has been demonstrated and is supported by a good rationale. Teriparatide increases bone mass but, at the same time, the new bone is less mineralized. Treatment with antiresorptives after teriparatide prevents accelerated osteoclastic resorption of the new bone tissue built during teriparatide therapy, increases mineralization, and rapidly lowers cortical porosity; this leads to further increases in BMD. The cost of teriparatide treatment is considerably higher than that of antiresorptives. For this reason, its use is indicated for patients with severe osteoporosis; in Italy, for example, teriparatide is fully reimbursed in patients with a new vertebral or hip fracture while on chronic treatment with antiresorptives or in patients never treated with antiresorptives with three or more vertebral or hip fractures.Citation1,Citation49 Contrary to bisphosphonates, the effect of which persists for many months after drug withdrawal,Citation50 the protective action of teriparatide on BMD vanishes with time in both genders but not up to the baseline values.Citation51,Citation52
Bazedoxifene
Bazedoxifene is a novel third-generation selective estrogen receptor modulator, a molecule developed to act as estrogen receptor agonists in some tissues (eg, bone) and as estrogen receptor antagonists in others, such as breast and endometrium, in order to reduce the risk of breast and endometrial cancers that would be induced by hormone replacement therapy.Citation53,Citation54
Two large Phase III clinical trialsCitation54,Citation55 showed that bazedoxifene, as well as raloxifene, increased BMD, decreased levels of bone turnover markers, and significantly reduced the risk of new vertebral fractures in postmenopausal women compared with placebo. Although the incidence of nonvertebral fractures with bazedoxifene or raloxifene did not differ significantly from that with placebo, a post hoc analysis of a subgroup of women at higher fracture risk revealed that bazedoxifene significantly reduced the nonvertebral fracture risk relative to placebo and raloxifene. Bazedoxifene also improved the lipid profile by reducing the serum concentrations of total cholesterol and low-density lipoprotein cholesterol, with an increase in the serum level of high-density lipoprotein cholesterol. The incidences of vasodilatation (hot flushes), leg cramps, and venous thromboembolic events were significantly higher with bazedoxifene and raloxifene compared with placebo. There was no evidence of endometrial and breast stimulation with bazedoxifene. Taking advantage of the favorable effects of bazedoxifene on the breast and endometrium, the pairing of bazedoxifene with conjugated estrogens is under investigation for the treatment of menopausal symptoms and prevention of postmenopausal osteoporosis. A Phase III trial showed that combination therapy of bazedoxifene and conjugated estrogens significantly increased BMD and decreased bone turnover markers, with relief of hot flushes and improvement of vaginal atrophy.Citation54
Although bazedoxifene is a promising new therapy for patients with osteoporosis, further clinical investigations of long-term treatment with this selective estrogen receptor modulator are needed to evaluate the prevention of osteoporotic fractures, breast cancers, endometrial cancers, and cardiovascular events. When treating patients with osteoporosis, estrogens and selective estrogen receptor modulators have effects not only on bone metabolism, but also on the breast, endometrium, and lipid metabolism. Before starting treatment, a risk–benefit assessment should be performed for each patient with osteoporosis.Citation54
Denosumab
Background
The principal regulator of bone resorption is the RANKL/ RANK/OPG pathway. RANKL is a transmembrane and soluble protein that is highly expressed by osteoblasts;Citation56,Citation57 its receptor, RANK, is located on the cell membrane of osteoclasts and preosteoclasts.Citation57,Citation58 RANKL–RANK binding stimulates the formation, activity, and survival of osteoclasts, resulting in increased bone resorption.Citation59
OPG is a naturally occurring, soluble, nonsignaling “decoy receptor” for RANKL. By binding to RANKL and preventing its interaction with RANK, OPG inhibits osteoclast formation,Citation59,Citation60 activity,Citation61,Citation62 and survival,Citation63 thereby reducing bone resorption.Citation57,Citation60
An increase of RANKL in proportion to OPG is associated with the development of postmenopausal osteoporosis and other skeletal disorders that include multiple myeloma, metastatic bone disease, treatment-related bone loss, rheumatoid arthritis, and Paget’s disease of bone.Citation57,Citation59,Citation64,Citation65
Development of RANKL inhibitors
The understanding of this pathway dates back to the end of the 1990s, Amgen (Amgen Inc, Thousand Oaks, CA) researchers identified in rats a gene sequence able to influence bone metabolism.Citation60,Citation66 Transgenic mice in which they induced the hepatic expression of the protein derived from that sequence resulted in a profound yet nonlethal osteopetrosis, coincident with a decrease in later stages of osteoclast differentiation.Citation60 These same effects were observed upon administration of recombinant OPG into normal mice. Recombinant OPG was shown to block osteoclast differentiation from precursor cells in vitro.Citation60 In vivo, it stopped ovariectomy-associated bone loss in rats. In vivo and in vitro data showed that OPG could act as a soluble factor in the regulation of bone mass and be of use in the treatment of osteoporosis associated with increased osteoclast activity.Citation60
The Amgen research group identified a protein, which they called “OPG ligand.”Citation67 The Snow Brand (Snow Brand Milk Products Co, Ltd, Tokyo, Japan) researchers isolated the same OPG-binding protein, and by comparing gene sequences discovered that it was identical to a previously described protein named RANKL or tumor necrosis factor-related activation-induced cytokine.Citation68 Subsequently the laboratories of Amgen analyzed osteoclast precursor cells and isolated RANK protein, which was discovered to be RANKL receptor.Citation69
While transgenic mice knockout for RANK or RANKL developed severe osteopetrosis, the overexpression of RANKL caused an increase in osteoclasts and a reduction in bone strength, and thus caused osteoporosis.Citation70
Several studies showed that pathological loss of bone mass, a typical example of postmenopausal osteoporosis, is associated with increased RANKL levels and the consequent hyperactivation of osteoclasts.Citation63 Moreover, RANKL levels in postmenopausal women are directly proportional to bone turnover markers, such as serum C-telopeptide of collagen type 1 and urinary N-telopeptide of collagen type 1 (NTX) – degradation products of collagen type 1 released into circulation during resorption of bone matrix.Citation71 Estrogen deficiency is also associated with an increment of osteoclasts and RANKL levels.Citation71 This evidence led to the development of targeted molecules specifically interacting with RANK/RANKL/ OPG pathway.
The entry of denosumab
Denosumab is a fully human monoclonal antibody of the immunoglobulin G2 isotype with a high affinity and specificity for RANKL. By binding RANKL, denosumab prevents its interaction with RANK, in much the same way as OPG, resulting in a decrease in bone resorption.
Pharmacokinetics of denosumab
The pharmacokinetics of denosumab are nonlinear with dose, similar to other fully human monoclonal antibodies. In healthy postmenopausal women given subcutaneous denosumab in varying doses, three phases were identified: (1) a prolonged absorption phase with maximum serum concentration observed at 5–21 days postdose, increasing as dose increased; (2) a prolonged phase, with serum halflife as long as 32 days with maximum dose; and (3) a rapid terminal phase when serum concentration dropped below 1000 ng/mL.Citation72
Efficacy and safety studies
The effect on bone remodeling of denosumab was assessed in a Phase I studyCitation72 by measurement of bone turnover markers, such as NTX, marker of bone resorption, and bone-specific alkaline phosphatase, a marker of bone formation. Forty-nine healthy postmenopausal women were treated with a single dose of subcutaneous denosumab 0.01, 0.03, 0.1, 0.3, 1.0, or 3.0 mg/kg or placebo, and followed for up to 6 months in all cohorts and as long as 9 months in the cohorts receiving the three highest doses.Citation57,Citation72 A reduction in NTX levels was observed that was dose-dependent, rapid (within 12 hours), profound (up to 84% decrease), sustained (for up to 6 months), and reversible with discontinuation. Reduction of bone-specific alkaline phosphatase was observed later than with NTX and was less pronounced.
The efficacy and safety of denosumab were evaluated in a Phase II randomized placebo-controlled study in postmenopausal women with low BMD, defined as lumbar spine T-score of −1.8 to −4.0 or total hip or femoral neck T-score of −1.8 to −3.5.Citation57,Citation73–Citation74 A total of 412 women were randomized to receive subcutaneous denosumab 6, 14, or 30 mg every 3 months or 14, 60, 100, or 210 mg every 6 months, open-label oral alendronate 70 mg once a week, or placebo. The primary endpoint was the percentage change in lumbar spine BMD at 12 months compared to baseline. Other endpoints included the percentage change from baseline in BMD at the total hip, femoral neck, distal one-third radius, and assessment of bone turnover with serum C-telopeptide of collagen type 1, urinary NTX, and bone-specific alkaline phosphatase. At 12 months, denosumab treatment was associated with a significant lumbar spine BMD increase of 3.0%–6.7%, depending on the dose and dosing interval, with smaller significant BMD increases observed at other skeletal sites.Citation73 BMD increases at the total hip and distal one-third radius with subcutaneous denosumab 30 mg every 3 months and 60 mg every 6 months were greater than with open-label alendronate.
Treatment with denosumab resulted in a dose-dependent, rapid, sustained, and reversible suppression of bone turnover markers.Citation57 The data at 24 months supported and extended the findings at 12 months, with continuing increases in BMD and suppression of bone turnover markers.Citation74
The study was extended for 24 months beyond the initial 24 months.Citation75 Patients originally randomized to denosumab were treated with subcutaneous denosumab 60 mg every 6 months, placebo, or placebo for 12 months followed by retreatment with subcutaneous denosumab 60 mg every 6 months for 12 months. Open-label alendronate patients discontinued alendronate therapy after 24 months and received no additional drug therapy. The original placebo group was maintained for the entire 48 months. Continuous denosumab treatment for 48 months increased BMD at the lumbar spine (9.4%–11.8% compared with baseline) and total hip (4.0%–6.1% compared with baseline), with consistent suppression of bone turnover markers for the duration of the study. Discontinuation of denosumab after 24 months of treatment was associated with a BMD decrease of 6.6% at lumbar spine and 5.3% at total hip within 12 months of discontinuation.Citation57
Retreatment with denosumab 12 months after discontinuation increased BMD to an extent similar to what was observed with initial treatment (BMD at lumbar spine increased 9.0% and at total hip increased by 3.9% compared with original baseline values).
Bone turnover marker levels increased with discontinuation of denosumab and decreased with retreatment. Discontinuation of alendronate at 24 months resulted in a modest decrease in BMD at lumbar spine by 48 months, with a greater decrease in BMD at total hip and distal one-third radius; bone turnover marker levels increased, but remained below baseline at 48 months. The initial 4-year study was extended an additional 4 years to evaluate the efficacy and safety of denosumab with up to 8 years of continuous exposure. A preliminary interim analysis after 2 years of the extension study (total of 6 years of denosumab therapy), with all patients switched to open-label denosumab at a dose of 60 mg subcutaneously every 6 months, showed that BMD at lumbar spine increased 13.3% compared with baseline, with sustained reductions in serum C-telopeptide of collagen type 1 and bone-specific alkaline phosphatase.Citation75 No patient developed neutralizing antibodies to denosumab.Citation57
FREEDOM (Fracture Reduction Evaluation of Denosumab in Osteoporosis every 6 Months) was a large 3-year Phase III clinical trial in 7868 postmenopausal women with osteoporosis who were randomized to receive either subcutaneous denosumab 60 mg (n = 3902) or placebo (n = 3906) every 6 months.Citation76 The primary efficacy endpoint was new vertebral fractures at 36 months, with secondary endpoints that included time to first hip and non-vertebral fractures. Study subjects, between the ages of 60 and 90 years, had a baseline T-score at lumbar spine or total hip between −2.5 and −4.0, with approximately 23% having at least one prevalent vertebral fracture at time of entry into the study. Treatment with denosumab was associated with a statistically significant 68% reduction in the risk of new vertebral fractures compared with placebo (2.3% denosumab versus 7.2% placebo, P < 0.0001), 40% reduction in the risk of hip fractures (0.7% denosumab versus 1.2% placebo, P = 0.036), and 20% reduction in the risk of nonvertebral fractures (6.5% denosumab versus 8.0% placebo, P = 0.011).Citation57,Citation76 There was no increase in the risk of cancer, infection, cardiovascular disease, delayed fracture healing, or hypocalcemia, and there were no cases of osteonecrosis of the jaw and no adverse reactions to the injection of denosumab.
DEFEND (Denosumab Fortifies Bone Density) was a Phase III trial evaluating the efficacy and safety of denosumab in 332 postmenopausal women with low bone mass (osteopenia). Postmenopausal women with lumbar spine T-scores between −1.0 and −2.5 were randomized to receive subcutaneous denosumab 60 mg every 6 months or placebo. Citation77 The primary efficacy endpoint was percentage change from baseline in lumbar spine BMD measured by dual X-ray absorptiometry at 24 months compared to placebo. Denosumab significantly increased BMD at lumbar spine compared with placebo at 24 months (denosumab 6.5% versus placebo −0.6%, P < 0.0001), as well as at total hip, distal one-third radius, and total body (P < 0.0001 for each compared with placebo), with a significant decrease in bone turnover markers compared with placebo. The safety profile was similar to placebo, except for a slightly higher incidence of cellulitis and exanthema. Eczema was reported in 3.0% of denosumab-treated patients compared with 1.7% in the placebo group (P < 0.001); cellulitis as a serious adverse event was more common with denosumab (0.3%) than placebo (<0.1%).
DECIDE (Determining Efficacy: Comparison of Initiating Denosumab Versus Alendronate) was a 1-year Phase III double-blind, double-dummy noninferiority trial in 1189 postmenopausal women with lumbar spine or total hip T-score of −2.0 or less who were randomized to receive subcutaneous denosumab 60 mg every 6 months plus weekly oral placebo or oral alendronate 70 mg weekly plus placebo subcutaneous injections every 6 months.Citation78 The primary endpoint was percentage change from baseline of total hip BMD at 12 months in subjects treated with denosumab compared with alendronate. At 12 months, there was a significantly greater BMD increase with denosumab compared with alendronate at total hip (denosumab 3.5% versus alendronate 2.6%, P < 0.0001) and all other measured skeletal sites, with treatment difference 0.6% at femoral neck, 1.0% at trochanter, 1.1% at lumbar spine, and 0.6% at distal one-third radius (P < 0.0002 for all sites). There was a statistically significant greater reduction in bone turnover markers with denosumab compared with alendronate.
STAND (Study of Transitioning from Alendronate to Denosumab) was a 1-year Phase III double-blind, active-controlled, double-dummy study in 504 postmenopausal women being treated with alendronate, with lumbar spine or total hip T-score between −2.0 and −4.0.Citation79 Subjects were randomized to receive subcutaneous denosumab 60 mg every 6 months or continuing oral alendronate 70 mg weekly. The primary endpoint was percentage change in BMD at total hip at 12 months for denosumab compared to alendronate. At 12 months, there was a statistically significant greater increase in BMD with denosumab compared with continuing alendronate at total hip (denosumab 1.90%, alendronate 1.05%, P < 0.0001), lumbar spine, and distal one-third radius. Discontinuing denosumab (at a dose of 210 mg) after 24 months resulted in a decrease in BMD in the following year comparable to the gains in BMD with 24 months of therapy.Citation75 Denosumab has a declining residual effect over 1 year, a period called offset time.Citation80
provides a summary of the principal randomized controlled trials conducted with denosumab.
Table 2 Phase III clinical trials of denosumab for the treatment of postmenopausal osteoporosis or osteopeniaCitation58
Clinical applications of denosumab
Denosumab has been approved for treatment of postmenopausal osteoporosis, as the data of clinical trials showed antifracture efficacy of denosumab to be at least as good as current therapeutic agents in the treatment of postmenopausal osteoporosis and is associated with excellent tolerability. It may be particularly important for patients with gastrointestinal contraindications or side effects with oral bis phosphonates and for patients with malabsorption.Citation57 The long dosing interval of 6 months is likely to be attractive to patients who have difficulty with the more frequent and sometimes bothersome requirements for oral bisphosphonate therapy. The subcutaneous route of administration expands the potential locations for drug administration to any physician’s office, as compared with intravenous bisphosphonates, which are typically given at an infusion center or office with staff trained in infusion therapy.Citation57
The clinical significance of the observation of statistically significant differences in some individual adverse events (eg, sore throat, rash) and serious adverse events (eg, cellulitis, infections requiring hospitalization) is unclear, but has raised concern regarding possible adverse effects on the immune system. RANKL inhibition might increase the risk of infection or malignancy, since RANKL, RANK, and/or OPG are expressed in activated T and B lymphocytes, dendritic cells, and CD4/CD8 thymocytes,Citation81,Citation82 and RANKL and RANK knockout mice have a deficiency of splenic B cells and fail to develop lymph nodes.Citation83,Citation84 However, inhibition of RANKL in adult humans has not been shown to adversely affect measured parameters of immune function.Citation57
No evidence of adverse clinical consequences due to bone turnover suppression, eg, increased fracture risk or impaired fracture healing, were observed with denosumab.Citation57 Iliac crest bone biopsy data has shown normal bone quality with significant decreases in bone turnover parameters in denosumab-treated patients,Citation85,Citation86 consistent with the observed effects on bone turnover markers. All placebo-treated patients were found to have double label, while 36% of patients treated with denosumab had no detectable tetracycline label and 25% had only a single label.
The clinical significance of the absence of tetracycline label in denosumab-treated patients is uncertain. While denosumab appears to be an excellent option as the primary treatment of postmenopausal osteoporosis, it is most likely to be used in patients with a contraindication to oral bisphosphonates, gastrointestinal intolerance, malabsorption, or poor response to therapy.Citation57
A validated Markov microsimulation model was used to estimate the cost (€2009) per quality-adjusted life year gained of a 3-year denosumab treatment compared with no treatment.Citation80 The model was populated with cost and epidemiological data for Belgium from a health-care perspective and the base–case population was defined from the FREEDOM trial.Citation80 This study suggests, on the basis of currently available data, that denosumab is cost-effective compared with no treatment for postmenopausal Belgian women with low bone mass and who are similar to patients included in the FREEDOM trial. In addition, denosumab was found to be cost-effective at the commonly accepted threshold of €30,000 per quality-adjusted life year gained in a population currently reimbursed in Europe with T-score −2.5 or less or prevalent vertebral fracture, aged 60 years and above.Citation80
As well as in postmenopausal osteoporosis, denosumab has been examined in rheumatoid arthritis, multiple myeloma, breast cancer, prostate cancer, and other solid tumors.Citation87
Androgen deprivation therapy is the cornerstone treatment for metastatic prostate cancer. The profound hypogonadal state is associated with metabolic changes including decreased BMD and an increased risk of fracture.Citation87
In postmenopausal women, a single administration of denosumab resulted in rapid (within 12 hours), marked (80%), and sustained (6 months) suppression of osteoclast activity.Citation71 In patients with multiple myeloma or bone metastasis from breast or prostate cancer, denosumab was well tolerated and achieved rapid and sustained suppression of osteoclast activity,Citation88,Citation89 and has proven efficacy in fracture prevention in men on initial androgen deprivation therapy.
Denosumab was superior to zoledronate in treatment of bone metastatic disease in castration resistant prostate cancer, the one setting in which a bisphosphonate is approved for prostate cancer.Citation87 Ongoing Phase III studies will address other important unmet medical needs including metastasis prevention.Citation87
In patients receiving methotrexate for erosive rheumatoid arthritis, denosumab provided protection against erosion, not only preventing bone loss but increasing hand BMD as measured by dual X-ray absorptiometry.Citation90
Safety information on denosumab
Data is summarized in and available in the leaflet information of denosumab.
Table 3 Safety information on denosumab
Denosumab and osteonecrosis of the jaw (ONJ)
The FREEDOM trial reported no cases of ONJ in either denosumab or placebo group.Citation76 As ONJ and atypical femoral subtrochanteric fracture associated with long-term bisphosphonate use are rare, there might be an advantage (albeit small, given the rarity of these events) to the use of denosumab. Moreover, since bisphosphonates are cleared by the kidney and contraindicated in patients with renal insufficiency, denosumab (which is cleared by non-renal metabolism) may prove to be a safe drug in these patients, although studies that directly address this issue need to be done.Citation91
All denosumab randomized controlled trials published to date include a dosing interval longer than 3 months and a cumulative dose of not more than 210 mg per 6 months.Citation92,Citation93 None of these studies report any cases of ONJ. On the contrary, preliminary results of two randomized controlled trials studying denosumab for the treatment of bone metastases in cancer patients include a monthly dosing interval and a dose of 120 mg per month.Citation94,Citation95 Denosumab-related ONJ could be a dose-related adverse effect.Citation93
ONJ has been reported to be a much more common event in patients receiving bisphosphonates for the treatment and prevention of cancer-related skeletal events (mainly intravenously) rather than in those patients receiving bisphosphonates (mainly orally) for nonmalignancy indications.Citation96,Citation97
Similar to bisphosphonate-related ONJ pharmacosurveillance and reporting history,Citation98 broad introduction of denosumab into clinical practice would allow for the recognition of denosumab-related ONJ adverse effect. Common plausible mechanisms for the etiopathogenesis of both denosumab- and bisphosphonate-related ONJ would encompass defective osteoclast differentiation, function, survival, and “fatigue.”Citation99 When compared to bisphosphonates, denosumab exhibits the advantage of short clearance time. Thus, more feasible treatment and earlier healing of denosumab-related ONJ when compared to bisphosphonate-related ONJ could be anticipated.Citation93
Denosumab and atypical fractures
Research from the first 3 years of an open-label extension of the pivotal Phase III FREEDOM trial, presented at the American College of Rheumatology 2011 Annual Meeting, showed that long-term use of the antiresorptive agent denosumab in postmenopausal women with osteoporosis continues to increase bone density and reduce markers of bone turnover, with no increased risk for the atypical fractures seen with long-term use of bisphosphonates.Citation100
Further clinical investigations of long-term treatment with denosumab are needed to evaluate the possible occurrence of atypical fractures.
Conclusion
Denosumab is a promising emerging drug for the prevention and treatment of postmenopausal osteoporosis. Human monoclonal antibody to RANK, denosumab 60 mg given subcutaneously every six months has shown to increase BMD and reduce bone turnover and fracture risk in all the fragile sites. It is simple to administer and well tolerated, with a safety profile generally similar to placebo, except for a slightly higher incidence of cellulitis and exanthema.
Approved by the Food and Drug Administration and European Medicines Agency for the treatment of postmenopausal osteoporosis in women at high risk of fracture and for the bone loss associated with androgen deprivation therapy in men with prostate cancer, denosumab may be particularly useful in clinical practice for the treatment of patients who have failed or are intolerant to other available osteoporosis therapy, eg, patients with gastrointestinal contraindications, side effects with oral bisphosphonates, or malabsorption.
Denosumab has also shown promising skeletal effects in the treatment of cancer and rheumatoid arthritis.
Disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. No writing assistance was utilized in the production of this manuscript.
References
- CavalliLBrandiMLAge- and gender-related macro and microarchitecture changes in bone structure and implications for treatmentInt J Clin Rheumatol201163359369
- BouxseinMLDeterminant of skeletal fragilityBest Pract Res Clin Rheumatol200519689791116301186
- SirisESChenYTAbbottTABone mineral density thresholds for pharmacological intervention to prevent fracturesArch Intern Med2004164101108111215159268
- GallacherSJDixonTImpact of treatments for postmenopausal osteoporosis (bisphosphonates, parathyroid hormone, strontium ranelate, and denosumab) on bone quality: a systematic reviewCalcif Tissue Int201087646948420872215
- ChenPMillerPDReckerRIncreases in BMD correlate with improvements in bone microarchitecture with teriparatide treatment in postmenopausal women with osteoporosisJ Bone Miner Res20072281173118017451369
- BrandiMLMicroarchitecture, the key to bone qualityRheumatology (Oxford)200948Suppl 4iv3iv819783591
- RiggsBLParfittAMDrugs used to treat osteoporosis: the critical need for a uniform nomenclature based on their action on bone remodelingJ Bone Miner Res200520217718415647810
- AmmannPShenVRobinBMaurasYBonjourJPRizzoliRStrontium ranelate improves bone resistance by increasing bone mass and improving architecture in intact female ratsJ Bone Miner Res200419122012202015537445
- FuchsRKAllenMRCondonKWStrontium ranelate does not stimulate bone formation in ovariectomized ratsOsteoporos Int20081991331134118385919
- PietschmannPRaunerMSiposWKerschan-SchindlKOsteoporosis: an age-related and gender-specific disease – a mini-reviewGerontology200955131218948685
- CummingsSRHow drugs decrease fracture risk: lessons from trialsJ Musculoskelet Neuronal Interact20022319820015758432
- BeckTJStoneKLOreskovicTLEffects of current and discontinued estrogen replacement therapy on hip structural geometry: the study of osteoporotic fracturesJ Bone Miner Res200116112103211011697807
- ReszkaAARodanGABisphosphonates mechanism of actionCurr Osteoporos Rep200312455216036064
- RussellRGBisphosphonates: the first 40 yearsBone201149121921555003
- CoxonFPHelfrichMHVan’t HofRProtein geranylgeranylation is required for osteoclast formation, function, and survival: inhibition by bisphosphonates and GGTI-298J Bone Miner Res20001581467147610934645
- ReszkaAAHalasy-NagyJMMasarachiaPJRodanGABisphosphonates act directly on the osteoclast to induce caspase cleavage of mst1 kinase during apoptosis. A link between inhibition of the mevalonate pathway and regulation of an apoptosis-promoting kinaseJ Biol Chem199927449349673497310574973
- Halasy-NagyJMRodanGAReszkaAAInhibition of bone resorption by alendronate and risedronate does not require osteoclast apoptosisBone200129655355911728926
- RogersHLMarshallDRogersMJEffects of bisphosphonates on osteoclasts in vitro, studies by scanning electron microscopyBone200230343S
- AlakangasASelanderKMulariMAlendronate disturbs vesicular trafficking in osteoclastsCalcif Tissue Int2002701404711907706
- de GroenPCLubbeDFHirschLJEsophagitis associated with the use of alendronateN Engl J Med199633514101610218793925
- BlankMAEmsBLGibsonGWNonclinical model for assessing gastric effects of bisphosphonatesDig Dis Sci19974222812889052507
- ElliottSNMcKnightWDaviesNMAlendronate induces gastric injury and delays ulcer healing in rodentsLife Sci199862177919444970
- PeterCPKindtMVMajkaJAComparative study of potential for bisphosphonates to damage gastric mucosa of ratsDig Dis Sci1998435100910159590415
- XiongYYangHJFengJShiZLWuLDEffects of alendronate on the proliferation and osteogenic differentiation of MG-63 cellsJ Int Med Res200937240741619383235
- WellsGACranneyAPetersonJAlendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal womenCochrane Database Syst Rev20081CD00115518253985
- WellsGACranneyAPetersonJRisedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal womenCochrane Database Syst Rev20081CD00452318254053
- BlackDMDelmasPDEastellRHORIZON Pivotal Fracture TrialOnce-yearly zoledronic acid for treatment of postmenopausal osteoporosisN Engl J Med2007356181809182217476007
- ChesnutCHIIISkagAChristiansenCOral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE)Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosisJ Bone Miner Res20041981241124915231010
- ReckerRMasarachiaPSantoraATrabecular bone microarchitecture after alendronate treatment of osteoporotic womenCurr Med Res Opin200521218519415801989
- DufresneTEChmielewskiPAManhartMDJohnsonTDBorahBRisedronate preserves bone architecture in early postmenopausal women in 1 year as measured by three-dimensional microcomputed tomographyCalcif Tissue Int200373542343212964065
- SeemanETo stop or not to stop, that is the questionOsteoporos Int200920218719519096746
- ReginsterJYBruyèreOSawickiALong-term treatment of postmenopausal osteoporosis with strontium ranelate: results at 8 yearsBone20094561059106419679207
- European Medicines AgencyProtelos: scientific discussion Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000560/human_med_000999.jsp&jsenabled=trueAccessed October 12, 2009
- DeeksEDDhillonSStrontium ranelate: a review of its use in the treatment of postmenopausal osteoporosisDrugs201070673375920394457
- MariePJAmmannPBoivinGReyCMechanisms of action and therapeutic potential of strontium in boneCalcif Tissue Int200169312112911683526
- BrennanTCRybchynMSGreenWAtwaSConigraveADMasonRSOsteoblasts play key roles in the mechanisms of action of strontium ranelateBr J Pharmacol200915771291130019563530
- ZhuLLZaidiSPengYInduction of a program gene expression during osteoblast differentiation with strontium ranelateBiochem Biophys Res Commun2007355230731117300752
- ChattopadhyayNQuinnSJKiforOYeCBrownEMThe calcium-sensing receptor (CaR) is involved in strontium ranelate-induced osteoblast proliferationBiochem Pharmacol200774343844717531955
- CaverzasioJStrontium ranelate promotes osteoblastic cell replication through at least two different mechanismsBone20084261131113618378206
- FromiguèOHayEBarbaraACalcium sensing receptor-dependent and receptor-independent activation of osteoblast replication and survival by strontium ranelateJ Cell Mol Med2009138B2189219920141614
- MeunierPJRouxCSeemanEThe effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosisN Eng J Med20043505459468
- ReginsterJYSeemanEDe VernejoulMCStrontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) studyJ Clin Endocrinol Metab20059052816282215728210
- ReginsterJYFelsenbergDBoonenSEffects of long term strontium ranelate treatment on the risk of nonvertebral and vertebral fractures in postmenopausal osteoporosis: results of a 5-year randomized, placebo-controlled trialAtrthritis Rheum200858616871695
- DelmasPDTreatment of postmenopausal osteoporosisLancet200235993222018202612076571
- ReckerRRMarinFIsh-ShalomSComparative effects of teriparatide and strontium ranelate on bone biopsies and biochemical markers of bone turnover in postmenopausal women with osteoporosisJ Bone Miner Res20092481358136819338452
- RiggsBLParfittAMDrugs used to treat osteoporosis: the critical need of a uniform nomenclature based on their action on bone remodelingJ Bone Miner Res200520217718415647810
- ReckerRRBareSPSmithSYCancellous and cortical bone architecture and turnover at the iliac crest of postmenopausal osteoporotic women treated with parathyroid hormone 1–84Bone200944111311918983947
- MiyakoshiNEffects of parathyroid hormone on cancellous bone mass and structure in osteoporosisCurr Pharm Des200410212615262715320749
- AdamiSBrandiMLCanonicoPLMinisolaGMinisolaSTarantinoUAppropriate use of anabolic treatment for severe osteoporosisClin Cases Miner Bone Metab20107211412222460015
- BoneHGHoskingDDevogelaerJPTen years’ experience with alendronate for osteoporosis in postmenopausal womenN Engl J Med2004350121189119915028823
- FinkelsteinJSWylandJJLederBZEffects of teriparatide retreatment in osteoporotic men and womenJ Clin Endocrinol Metab20099472495250119401368
- EastellRNickelsenTMarinFSequential treatment of severe postmenopausal osteoporosis after teriparatide: final results of the randomized, controlled European study of Forsteo (EUROFORS)J Bone Miner Res200924472673619049337
- KawateHTakayanagiREfficacy and safety of bazedoxifene for postmenopausal osteoporosisClin Interv Aging2011615116021753870
- SilvermanSLChristiansenCGenantHKEfficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo- and active-controlled clinical trialJ Bone Miner Res200823121923193418665787
- MillerPDChinesAAChristiansenCEffects of bazedoxifene on BMD and bone turnover in postmenopausal women: 2-yr results of a randomized, double-blind, placebo-, and active-controlled studyJ Bone Miner Res200823452553518072873
- Collin-OsdobyPRegulation of vascular calcification by osteoclast regulatory factors RANKL and osteoprotegerinCirc Res200495111046105715564564
- LewieckiEMTreatment of osteoporosis with denosumabMaturitas201066218218620236778
- HsuHLaceyDLDunstanCRTumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligandProc Natl Acad Sci U S A19999673540354510097072
- LaceyDLTimmsETanHLOsteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activationCell19989321651769568710
- SimonetWSLaceyDLDunstanCROsteoprotegerin: a novel secreted protein involved in the regulation of bone densityCell19978923093199108485
- BurgessTLQianYKaufmanSThe ligand for osteoprotegerin (OPGL) directly activates mature osteoclastsJ Cell Biol1999145352753810225954
- MosekildeLSogaardCHDanielsenCCTorringOThe anabolic effects of human parathyroid hormone (hPTH) on rat vertebral body mass are also reflected in the quality of bone, assessed by biomechanical testing: a comparison study between hPTH-1–34 and hPTH-1–84Endocrinology199112914214282055197
- LaceyDLTanHLLuJOsteoprotegerin ligand modulates murine osteoclast survival in vitro and in vivoAm J Pathol2000157243544810934148
- HofbauerLCSchoppetMClinical implications of the osteoprotegerin/RANKL/RANK system for bone and vascular diseasesJAMA2004292449049515280347
- BoyleWJSimonetWSLaceyDLOsteoclast differentiation and activationNature2003423693733734212748652
- YasudaHShimaNNakagawaNIdentity of osteoclastogenesis inhibitory factor (OCIF) and osteoprotegerin (OPG): a mechanism by which OPG/OCIF inhibits osteoclastogenesis in vitroEndocrinology19981393132913379492069
- KhoslaSMinireview: the OPG/RANKL/RANK systemEndocrinology2001142125050505511713196
- YasudaHShimaNNakagawaNOsteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKLProc Natl Acad Sci U S A1998957359736029520411
- AndersonDMMaraskovskyEBillingsleyWLA homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell functionNature199739066561751799367155
- MizunoAKannoTHoshiMTransgenic mice overexpressing soluble osteoclast differentiation factor (sODF) exhibit severe osteoporosisJ Bone Miner Metab200220633734412434161
- Eghbali-FatourechiGKhoslaSSanyalABoyleWJLaceyDLRiggsBLRole of RANK ligand in mediating increased bone resorption in early postmenopausal womenJ Clin Invest200311181221123012697741
- BekkerPJHollowayDLRasmussenASA single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal womenJ Bone Miner Res20041971059106615176987
- McClungMRLewieckiEMCohenSBDenosumab in postmenopausal women with low bone mineral densityN Engl J Med2006354882183116495394
- LewieckiEMMillerPDMcClungMRTwo-year treatment with denosumab (AMG 162) in a randomized phase 2 study of postmenopausal women with low BMDJ Bone Miner Res200722121832184117708711
- MillerPDBologneseMALewieckiEMEffect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trialBone200843222222918539106
- CummingsSRSan MartinJMcClungMRDenosumab for prevention of fractures in postmenopausal women with osteoporosisN Engl J Med2009361875676519671655
- BoneHGBologneseMAYuenCKEffects of denosumab on bone mineral density and bone turnover in postmenopausal womenJ Clin Endocrinol Metab20089362149215718381571
- BrownJPPrinceRLDealCComparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trialJ Bone Miner Res200924115316118767928
- KendlerDLRouxCBenhamouCLEffects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapyJ Bone Miner Res2010251728119594293
- HiligsmannMReginsterJYPotential cost-effectiveness of denosumab for the treatment of postmenopausal osteoporotic womenBone2010471344020303422
- ClowesJARiggsBLKhoslaSThe role of the immune system in the pathophysiology of osteoporosisImmunol Rev200520820722716313351
- XingLSchwarzEMBoyceBFOsteoclast precursors, RANKL/ RANK, and immunologyImmunol Rev2005208192916313338
- DougallWCGlaccumMCharrierKRANK is essential for osteoclast and lymph node developmentGenes Dev199913182412242410500098
- KongYYYoshidaHSarosiIOPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesisNature199939767173153239950424
- ReidIRBenhamouCLBologneseMEffects of denosumab on bone histology and histomorphometry: the FREEDOM and STAND studies [abstract]J Bone Miner Res200924Suppl 1S9
- United States Food and Drug Administration, Amgen IncBriefing information for the August 13, 2009 meeting of the Reproductive Health Drugs Advisory Committee2009 Available from: http://www.fda.gov/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ReproductiveHealth-DrugsAdvisoryCommittee/ucm176584.htmAccessed October 30, 2009
- LeeRJSaylorPLSmithMRTreatment and prevention of bone complication from prostate cancerBone2011481889520621630
- BodyJJFaconTColemanREA study of the biological receptor activator of nuclear factor-kappaB ligand inhibitor, denosumab, in patients with multiple myeloma or bone metastases from breast cancerClin Cancer Res20061241221122816489077
- LiptonAStegerGGFigueroaJRandomized active-controlled phase II study of denosumab efficacy and safety in patients with breast cancer-related bone metastasesJ Clin Oncol200725284431443717785705
- DeodharADoreRKMandelDDenosumab-mediated increase in hand bone mineral density associated with decreased progression of bone erosion in rheumatoid arthritis patientsArthritis Care Res (Hoboken)201062456957420391513
- KhoslaSIncreasing options for the treatment of osteoporosisN Engl J Med2009361881882019671654
- AnastasilakisADToulisKAGoulisDGEfficacy and safety of denosumab in postmenopausal women with osteopenia or osteoporosis: a systematic review and a meta-analysisHorm Metab Res2009411072172919536731
- KyrgidisAToulisKADenosumab-related osteonecrosis of the jawsOsteoporos Int201122136937020306021
- HenryDvon MoosRVadhan-RajSA double-blind, randomized study of denosumab versus zoledronic acid for the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myelomaEur J Cancer Suppl20097312
- StopeckABodyJJFujiwaraYDenosumab versus zoledronic acid for the treatment of breast cancer patients with bone metastases: results of a randomized phase 3 studyEur J Cancer Suppl20097323
- HessLMJeterJMBenham-HutchinsMAlbertsDSFactors associated with osteonecrosis of the jaw among bisphosphonate usersAm J Med2008121647548318501224
- KyrgidisAVahtsevanosKOsteonecrosis of the jaw in patients receiving oral bisphosphonatesOsteoporos Int201021353553619862464
- EdwardsBJGounderMMcKoyJMPharmacovigilance and reporting oversight in US FDA fast-track process: bisphosphonates and osteonecrosis of the jawLancet Oncol20089121166117219038763
- KyrgidisAVahtsevanosK“Fatigue” having a role in the pathogenesis of osteonecrosis of the jawsClin Oral Investig2009134479480
- GordonDDenosumab increases bone density, no atypical fracture riskMedscape Medical News [website on the Internet]11102011 Available from: http://www.medscape.com/viewarticle/753389Accessed January 17, 2012
- ReszkaAARodanGABisphosphonate mechanism of actionCurr Rheumatol Rep200351657412590887