Abstract
Pneumoscrotum is the term used to describe the presence of air within the scrotum and includes scrotal emphysema as well as pneumatocele. The etiology varies; in some cases, pneumoscrotum may be due to life-threatening disease like pneumothorax or Fournier gangrene. Despite this, pneumoscrotum is a rarely debated issue. We present two different cases of pneumoscrotum and a review of the literature. The first case report is about a 29 year old male patient affected by Duchenne syndrome who showed pneumoscrotum after cardiopulmonary resuscitation that was performed for asphyxic crisis and cardiovascular arrest. We carried out local puncture with an 18-gauge needle, and the pneumoscrotum was successfully solved. The second case report is about a 56 year old male with pneumoscrotum due to Fournier gangrene who underwent radical exeresis of all necrotic tissues and drainage. This is why most of the scrotal skin and all of the penis skin were removed; as a result, the testicles, epididymis, and cavernosa corpora were externalized. On postoperative day one, the patient was feverless and underwent hyperbaric chamber therapy. No postoperative complications occurred. Accurate evaluation of the pneumoscrotum is always needed. Despite the benign course of most of the clinically evident pneumoscrotum cases, this condition should never be underestimated.
Introduction
Pneumoscrotum is the term used to describe the presence of air within the scrotum. The incidence of pneumoscrotum is not clear, and probably the real incidence is underestimated because the condition is often not reported. Pneumoscrotum includes scrotal emphysema as well as pneumatocele. Scrotal emphysema is palpable and typically shows clinical signs such as swelling of the scrotum and palpable crepitus. Pneumatocele is not palpable because the air is present within the tunica vaginalis of the testicle.Citation1 Intrascrotal gas may not manifest as crepitus or as classic subcutaneous emphysema but more often may appear as diffuse swelling and, eventually, edema. The lack of subcutaneous emphysema in pneumoscrotum may be due to gas tracking along the transversalis fascia, which forms the innermost layer of the covering of the spermatic cord.Citation2 The etiologies vary; in some cases pneumoscrotum may be due to a life-threatening disease, such as pneumothorax or Fournier gangrene (FG). Despite this, pneumoscrotum is a rarely debated issue. We present two different cases of pneumoscrotum and a review of the literature.
Case 1 presentation
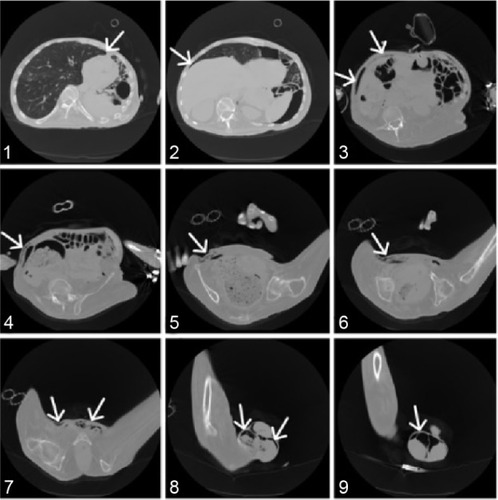
A 29 year old male affected by Duchenne syndrome with mild left systolic dysfunction and chronical respiratory distress arrived on trans-tracheostomic jet-ventilation (continuous positive airway pressure [CPAP]: inspiratory pressure [PI] 20 cm H2O; positive end-expiratory pressure [PEEP] 3 cm H2O; breathing rate [BR] 13 breaths/minute; inspiratory time [TI] 1–2 seconds) and was admitted to our emergency room for cyanosis, asphyxic crisis, and cardiovascular arrest due to the obstruction of the tracheostomic tube by necrotic tissue after home care substitution. The patient underwent cardiopulmonary resuscitation with success. After this maneuver, pneumoscrotum occurred. At the time of the clinical examination, massive subcutaneous emphysema had spread through the anterior wall of the abdomen to the scrotum, where pneumoscrotum was evident. An electrocardiogram taken after the resuscitation showed sinusal tachycardia with aspecific abnormalities of the repolarizing phase. The high resolution X-ray computed tomography scan of the chest showed a marked ectasia of the trachea, in correspondence with the endotracheal tube, with thin fluid level in the context; a basal pneumothorax on the left base with major thickness of 28 mm and a secondary 7 mm flap of apical pneumothorax on the right side were also highlighted. Apical emphysematous blebs of the left lung and scar tissue were also present. Pneumoperitoneum was evident. A flap allowed air to diffuse through the abdominal wall to the scrotum bilaterally; this resulted in pneumoscrotum (). We carried out local puncture with an 18-gauge needle, and the pneumoscrotum was successfully resolved. The patient died 2 days after the resuscitation from acute respiratory distress syndrome due to the progression of the Duchenne syndrome.
Case 2 presentation
A 56 year old male patient was referred to the emergency room of our hospital with a fever (39°C), scrotal swelling, necrotic areas of the scrotum, and penis skin swelling from necrosis. During a clinical exam, it was discovered that an irreducible, bilateral, tension pneumoscrotum associated with edema of the scrotum and the penis had developed. The patient did not report pain. The patient was also affected by severe diabetes mellitus with poor medical control due to the patient’s low compliance. Cultural specimens of blood, urine, and dermal surfaces were collected, and the blood was analyzed. The leucocyte count was 14.29×103/mm3; 87% of the leukocytes were neutrophils and 2.9% were basophils. The concentration of hemoglobin was 8.9 g/dL, and the concentration of glucose was 247 mg/dL. Sodium was 134 mEq/L. Serum creatinine was 2.24 mg/dL with an estimated glomerular filtration rate of 32.36 mL/min. Inflammation markers were collected, too. The erythrocyte sedimentation rate was 120 mm/h. The concentration of pseudocolinesterase was 4,187 units/L, and the concentration of procalcitonine was 13.79 ng/mL. The C-reactive protein concentration was 30.23 mg/dL. The cultural specimen of urine was negative. The specimen of the dermal surface was positive for Staphylococcus warneri. The diagnosis of FG was done, and 6 hours later the patient underwent surgical toilet with antibiotic therapy including trimethoprim–sulfamethoxazole, meropenem, tigecycline, and an antimycotic prophylaxis with micafungin (). We performed radical debriding of all necrotic tissues and drained the pus. For this purpose, the most of scrotal skin and all of the penis skin were removed; this procedure externalized the testicles, epididymis, and cavernosa corpora (). A second procedure within 48 hours was not necessary because of the adequacy of the initial debridement. On the first postoperative day, the fever disappeared, and the patient was transferred to another hospital in order to undergo hyperbaric chamber therapy. No postoperative complications occurred. After 1 month, the patient was in good health without progression of necrotic areas or signs of local or systemic infection. As of this writing, the patient is undergoing reconstructive surgery of the scrotum wall. Written informed consent was obtained from this patient for the publication of this case report and the accompanying images.
Discussion
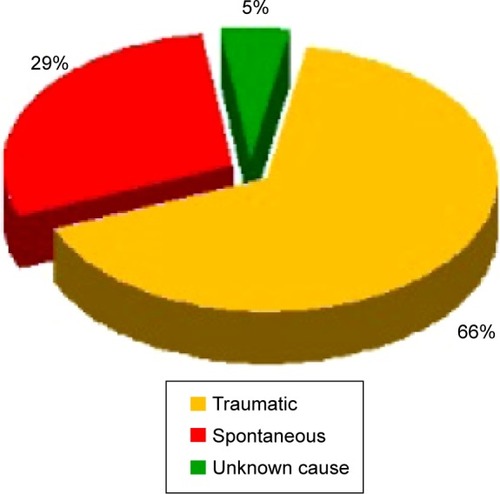
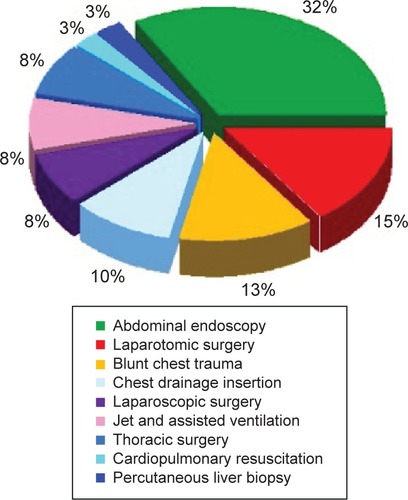
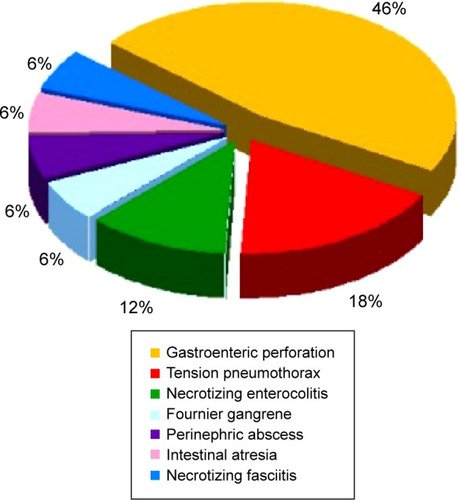
The most common causes of pneumoscrotum include traumatic factors, such as thoracic trauma, and iatrogenic factors, such as the colonic perforation after endoscopic polypectomy. Pneumoscrotum is also due to spontaneous causes including spontaneous pneumothorax, perforation of hollow abdominal organs, and gas-producing bacterial infections.Citation2 Three physiopathological mechanisms may explain pneumoscrotum. One is that the infection could be caused by gas-producing bacteria, which cause the diffusion of air through the subcutaneous tissues (eg, FG) or the direct access of the air to the scrotum. Another mechanism could include the presence of an air layer in the abdominal hollow; this air could spread by diffusion through the fascial planes or across different peritoneal defects into the scrotum. An embryological defect of the processus vaginalis is present in 15%–30% of the male adults and in 60% of the infants. This anatomy is generally the result of visceral perforations either in a case of spontaneous perforation due to infections or in a case of iatrogenic perforation. Colonic perforation secondary to operative colonoscopy is uncommon, and its reported incidence range is 0.073%–2.14%.Citation3,Citation4 The third possible mechanism is the air spreading from the lungs due to pneumothorax, pneumomediastinum, or thoracic traumas. In the case of pneumothorax, the air disseminates through Camper’s fascia and Scarpa’s fascia up to the scrotum via a connective tissue across the abdominal segments. The superficial and deep fascial planes of the Camper’s and Scarpa’s fascia are distinct in the abdomen but fuse at the corona of the penis, where they form the Colles fascia; even in the testicles, they blend together and generate the Dartos’ fascia. Pneumomediastinum, too, may cause air to spread through periesophageal and periaortic fascial planes and then to the diaphragmatic hiatus, where air is allowed direct access into the perinephric space and can cause pneumoretroperitoneum. The air can diffuse through the inguinal canal and along the spermatic fascia to the scrotum. Lastly, the sternocostal margin of the diaphragm may allow the diffusion of an air layer to the abdominal hollow and pelvis through direct communication. The first case of pneumoscrotum was described in 1912 after a nephrostomy.Citation5 Until now, few cases have been reported to be caused by pathological, traumatic, or iatrogenic processes. A systematic bibliographic research from January 1972 until December 2013 was conducted in PubMed and Scopus. Two authors (GC, FB) independently performed online bibliographic searches in order to identify titles and abstracts of interest. Full texts of relevant articles were further assessed for inclusion in this study. In this way we included 58 articles. To our knowledge, 59 cases of pneumoscrotum were described (). Traumatic and iatrogenic causes accounted for 66% of all pneumoscrotum cases (39 cases out of 58 total). Spontaneous causes accounted for 29% (17 of 58), and the reasons for the remaining 5% (3 of 58) of the reviewed cases are unknown (). By themselves, the endoscopic colonic procedures and the abdominal endo scopy accounted for 32% (13 of 39) of all the reported cases of pneumoscrotum caused by iatrogenic complications. Laparotomic surgery accounted for 15% (6/39), and blunt chest trauma accounts for 13% (5/39) of all of the traumatic or iatrogenic cases. Chest drainage insertion affected 10% (4/39) of these cases, while thoracic surgery, laparoscopic surgery, and assisted or jet ventilation each account for 8% (3/39). Only one case of pneumoscrotum secondary to percutaneous liver biopsy was reported, which amounted to 3% in our series (). The first case that we described is the second case of pneumoscrotum secondary to cardiopulmonary resuscitation reported in literature. In our case, the pneumothorax caused by the chest compression resulted in air diffusing via a flap through the abdominal wall to the scrotum bilaterally, as shown by the arrows in . High quality chest compression has been emphasized to improve the survival of patients with cardiac arrest, and various skeletal injuries were reported. Rib fractures and sternal fractures were the most common skeletal injuries; rib fractures account for 13%–97% of these injuries, and sternal fractures for 1%–43%.Citation6–Citation8 Vertebral fractures have been seen less frequently. Pulmonary complications such as hemothorax, pneumothorax, and pneumomediastinum are infrequent but also possible. In this case, a conservative approach was carried out, and the pneumoscrotum was finally resolved. Spontaneous pneumoscrotum is reported less often in literature than is traumatic pneumoscrotum. In our series, 17 cases due to spontaneous causes were described. Of these, 46% (8/17) were due to gastroenteric perforation. Newborns presented a high incidence of pneumoscrotum due to gastric and bowel perforation. The causes were various: congestion of the bowel wall secondary to aspyhxia or septicemia, trauma coincident with delivery, excessive gastric acidity, direct or indirect mechanical injury from gavage tubes or resuscitation maneuver, congenital mural defects of the gastroenteric tract, meconium stasis, rupture of a diverticulum, and coincident central nervous system abnormalities (). Although speculation concerning the precise etiology of these perforations is intriguing, it is of far less importance than early recognition of the condition and early and appropriate treatment. Tension pneumothorax accounted for 18% (3/17) of all cases of reported spontaneous pneumoscrotum. Tension pneumothorax preferably affects young adults; the incidence of pneumothorax is 0.16% among the entire perinatal population. Therefore, it is worth considering that spontaneous pneumoscrotum is more common among newborns, among whom the incidence of gastrointestinal infection presenting as necrotizing enterocolitis accounted for 12% (2/17) of the spontaneous pneumoscrotum cases in the literature. Necrotizing enterocolitis is the most common gastrointestinal emergency and is the reason for 1%–8% of neonatal intensive care unit admissions; the mortality rate for this condition is between 20% and 40%.Citation9 The most consistent risk factors are prematurity, enteral feeding, hypoxia, and bacterial colonization.Citation10
Table 1 The 59 reported cases of pneumoscrotum from the literature search
Other rare conditions that may occur with pneumoscrotum are the perinephric abscess, the complication of intestinal atresia, and the rare necrotizing fasciitis; each of these represented 6% of the spontaneous pneumoscrotum cases in our review because there was only one case of each described in our literature search. In our bibliographic research, we found only case reports because no other types of studies on spontaneous pneumoscrotum were available. Furthermore, there are no standardized methods to quantify the grades of the pneumoscrotum cases that are reported. We feel that pneumoscrotum is an underestimated issue; nevertheless, it is often a clinical sign of a life-threatening disease. FG was described in 6% (1/17) of the reported spontaneous pneumoscrotum cases. However, FG is a rare condition; it has an incidence of 1.6 cases per 100,000 males per year (<0.02% of hospitals admissions). The mean age of patients with FG is 50.9 years with a major difference in incidence between males and females (male: female ratio for FG is 10:1).Citation11,Citation12 The mortality rate varies from 0% to 88% and depends on the severity of FG at the time of diagnosis. A diagnosis of FG is clinical, but blood analysis and radiological examinations may be helpful in establishing the severity and in identifying the extent of the necrotic process. In our second case, pneumoscrotum was a sequela of the bacterial infection. The management of FG was consistent with the diagnostic and therapeutic strategies reported in recent literature.Citation11,Citation12 Prompt diagnosis and an aggressive surgical debridement with hyperbaric oxygen therapy and broad-spectrum antibiotic combinations guarantee the best outcome.
Conclusion
In cases of pneumoscrotum, correct evaluation is needed. Some conditions such as torsion, neoplasms, epididymitis and orchitis, hydrocele, spermatocele, hematocele, hernia, and urine extravasation must be considered. Despite the benign course of most of the clinically evident pneumoscrotum cases, this condition should never be underestimated. A careful medical history that considers any thoracic or abdominal trauma or surgery, history of spontaneous pneumothorax, and recent endoscopic procedures is strongly suggested. Surgical puncture can be considered only if a correct diagnosis has been made.
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in either drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
- FirmanRHeiselmanDLloydTMardesichPPneumoscrotumAnn Emerg Med1993228135313568333643
- KlimachOEDefriendDJFosterDNPneumoscrotum following endoscopic sphincterotomySurg Endosc1990442302312291167
- GhaziAGrossmanMComplications of colonoscopy and polypectomyThe Surgical Clinics of North America19826258898966981859
- LoAYBeatonHLSelective management of colonoscopic perforationsJ Am Coll Surg199417933333378069431
- KeyesELTwo cases of pneumo-scrotum following nephrectomyAm J Urol1912846871
- LostoridisEGkagkalidisKVarsamisNPneumoscrotum as complication of blunt thoracic trauma: a case reportCase Rep Surg2013201339286923401836
- KhanRANarasimhanKLSpontaneous intestinal perforationAnn Ital Chir201283543743923064306
- BoumansDvan ZantenRASchotBWA man with painless scrotal swelling. Scrotal emphysema (pneumoscrotum)Neth J Med201270419419822641630
- WilsonCGreenABaderSGrafDPneumoscrotum as the presenting symptom of pneumothorax and pneumoperitoneum after jet ventilationAnesthesiology2012117240822430121
- NetschCBachTGrossAJPneumoscrotum as a consequence of long-term ventilationUrologe A2012512242244 German22269991
- HillTWMillsLDButtsCJPneumoscrotum after jejunal perforation: a case reportJ Emerg Med201242327928219201137
- CakmakEKoyuncuAYilmazAIatrogenic pneumoscrotum after colonoscopyTurk J Gastroenterol201122444344421948583
- SilákJNemecLOndrákMSefrRPneumoscrotum: uncommon sign in duodenal perforation (a case review)Rozhl Chir2011904237239 Czech [with English abstract]21755907
- KhanYAAkhtarJPneumoscrotum: a rare presentation of gastric perforation in a neonateAPSP J Case Rep2010121522953258
- PatelCBarnacleAMPneumoscrotum: a complication of pneumatosis intestinalisPediatr Radiol201141112920526593
- SuJTHsiaJYHuSYTsanYTLinTCWangLMPneumoscrotum after blunt chest traumaUrology2011771757620347122
- ToroAPulvirentiEDi CarloIPneumoscrotum due to perforated peptic ulcer previously sutured by laparoscopyJ Laparoendosc Adv Surg Tech A201020435936120156121
- AkdoganMOnalIKKurtMPneumoscrotum associated with nontherapeutic lower gastrointestinal endoscopyEndoscopy201042Suppl 2E7E820066607
- HeinerJDSkeinsECDevitaDLitnerJSScrotal swelling after penetrating chest traumaWest J Emerg Med200910429720046255
- De’AthHDPerforation of a sigmoid diverticulum presenting with a pneumoscrotum and surgical emphysemaBMJ Case Rep20082008bcr0820080834
- SimaioforidisVKontosSFokitisILefakisGKoritsiadisSSubcutaneous emphysema of the scrotum (pneumoscrotum) due to traumatic pneumothorax: a case reportCases J20081129318976497
- Di Capua SacotoC1Bahilo MateuPRamírez BackhausMGimeno ArgenteVPontones MorenoJLJiménez CruzJFPneumoscrotum secondary to bilateral tension pneumothoraxActas Urol Esp2008327756758 Spanish [with English abstract]18788495
- DasDTappouniRHoughtonRRenal colic associated with pneumoscrotumBr J Radiol2007809601025102718065649
- SinghSThakurMPneumoscrotum after colonoscopyCan J Gastroenterol200822441141318414718
- YangBJiangSXFanZLPneumoscrotum induced by spontaneous colon perforation: a case report and review of the literatureZhonghua Nan Ke Xue2007138744745 Chinese [with English abstract]17918718
- GraeplerFLauerUMHorgerMSLadurnerRGregorMPneumoscrotum after colonoscopic polypectomyEndoscopy200739Suppl 1E9017440870
- CaseyRGAl-DousariSMurphyDPowerREChest drain insertion may result in the acute scrotumScand J Urol Nephrol2006401787916452062
- FuKISanoYKatoSPneumoscrotum: a rare manifestation of perforation associated with therapeutic colonoscopyWorld J Gastroenterol200511325061506316124067
- Martínez-OrdazJLSuárez-RomeroMAMonter-CarreolaGABlanco-BenavidesRPneumoscrotum after colon surgeryGac Med Mex20051412155156 Spanish [with English abstract]15892464
- MazraanyWKohliHGabrielAMachadoGRBojalianMOReevesMEMassive pneumoscrotum following open gastrostomyContemp Surg200460219221
- Golpe GómezRMateos ColinoADocasar BertoloLMiguélez VaraCSpontaneous pneumomediastinum associated with anxiety stateAn Med Interna2002197378379 Spanish12224151
- KonoMMizunoTKobayashiTScrotal emphysema: a case reportHinyokika Kiyo20024813739 Japanese [with English abstract]11868384
- KohCCSheuJCIntestinal atresia presenting as bilateral scrotal pneumatocele: A case reportJ Pediatr Surg2002371E211782011
- SyEDLiuCSHuangSMShanYSCecal perforation presenting as abdominal-wall necrotizing fasciitisPediatr Surg Int2001172–321521711315293
- AslanYSarihanHDinçHGedikYAksoyADereciSGastric perforation presenting as bilateral scrotal pneumatocelesTurk J Pediatr199941226727110770669
- KatkhoudaNCamposGMMavorETrusslerAKhalilMStoppaRLaparoscopic extraperitoneal inguinal hernia repair. A safe approach based on the understanding of rectus sheath anatomySurg Endosc199913121243124610594277
- TrübelHHuthRKrämerWSudden pneumoscrotum in a ventilated infant. Sudden pneumoscrotum as clinical sign of a tension pneumothorax in an infant with tracheal stenosisEur J Pediatr199815786896909727857
- RaudatCWKatrisFWoodhallDPneumoscrotum: an unusual complication of pulmonary resectionJ Am Osteopath Assoc19969663623638690624
- StavemKHøivikBPneumoscrotum after air leak from tension pneumothoraxTidsskr Nor Laegeforen19961161012141215 Norwegian [with English abstract]8658391
- Di VitaGFrazzettaMCorteseEDamianoAComplications of the laparoscopic accessG Chir199617123136 Italian [with English abstract]
- TanSMNgFCRavintharanTLimPHChngHCLaparoscopic varicocelectomy: technique and resultsBr J Urol19957545235287788264
- WakabayashiYBushWHJrPneumoscrotum after blunt chest traumaJ Emerg Med19941256036057989685
- HeimbachDHofmockelGWirthMFrohmüllerHPneumoscrotum. Case report and review of the literatureUrologe A1993326503506 German [with English abstract]8284864
- HaselRAroraSKHickeyDRIntraoperative complications of laparoscopic cholecystectomyCan J Anaesth1993405 Pt 14594648513527
- WatsonHSKlugoRCCoffieldKSPneumoscrotum: report of two cases and review of mechanisms of its developmentUrology19924065175211466104
- CoppesMJRoukemaJABaxNMScrotal pneumatocele: a rare phenomenonJ Pediatr Surg19912612142814291765931
- MillmondSHGoldmanSMPneumoscrotum after spontaneous pneumothorax with air leakJ Urol19911456127112722033709
- MenziesDNobleJGDentCMCoxPJPneumoscrotum – an unusual complication of cardiopulmonary resuscitationBr J Urol19916744404412032090
- KlimachOEDefriendDJFosterDNPneumoscrotum following endoscopic sphincterotomySurg Endosc1990442302312291167
- GarciaCMarkowitzRIPneumoperitoneum and pneumoscrotum caused by gastric perforationAm J Perinatol19874175773790220
- ZikrillaevZZikrillaevMZAcute pneumoscrotum after kidney surgeryUrol Nefrol (Mosk)1985464 Russian4049597
- RedmanJFPahlsWLPneumoscrotum following tracheal intubationJ Urol19851336105610573999211
- HumphreysFHewetsonKADellipianiAWMassive subcutaneous emphysema following colonoscopyEndoscopy19841641601616468340
- AndreaniTBuffetCSubcutaneous abdominal emphysema and pneumoscrotum after endoscopic resection of rectal polypsGastroenterol Clin Biol198484387 French6735047
- BrayJFPneumoscrotum with testicular delineation-a new sign of pneumoperitoneumBr J Radiol1982556598678687139243
- FishmanEKGoldmanSMPneumoscrotum after colonoscopyUrology19811821711727269022
- EngelhardDOrnoyADeckelbaumRJPneumoscrotum complicating percutaneous liver biopsyGastroenterology19818023903927450429
- ChristensonPJO’ConnellKJAlbertPKnuffTEPneumoscrotum after diagnostic peritonoscopyUrology198016178796446794
- ArcherGJPneumoscrotum complicating pneumothorax and surgical emphysemaBr J Urol19744633434843727
- WilliamsRDSimmonsRLCitrobacter perinephric abscess presenting as pneumoscrotum in transplant recipientUrology1974344784804595716
- CastellanosRRegePREvansATPneumoscrotum: a case report and review of the literatureJ Urol197311022252264722618
- DenckerHPneumoscrotum as an early sign of anastomic leakage after anterior resection of the colonSurg Gynecol Obstet1972134610055032386