Abstract
Objective
Vasopressor agents are often prescribed in septic shock. However, their effects remain controversial. We conducted a systematic review and Bayesian network meta-analysis to compare the effects among different types of vasopressor agents.
Data sources
We searched for relevant studies in PubMed, Embase, and the Cochrane Library databases from database inception until December 2014.
Study selection
Randomized controlled trials in adults with septic shock that evaluated different vasopressor agents were selected.
Data extraction
Two authors independently selected studies and extracted data on study characteristics, methods, and outcomes.
Data synthesis
Twenty-one trials (n=3,819) met inclusion criteria, which compared eleven vasopressor agents or vasopressor combinations (norepinephrine [NE], dopamine [DA], vasopressin [VP], epinephrine [EN], terlipressin [TP], phenylephrine [PE], TP+NE, TP + dobutamine [DB], NE+DB, NE+EN, and NE + dopexamine [DX]). Except for the superiority of NE over DA, the mortality of patients treated with any vasopressor agent or vasopressor combination was not significantly different. Compared to DA, NE was found to be associated with decreased cardiac adverse events, heart rate (standardized mean difference [SMD]: −2.10; 95% confidence interval [CI]: −3.95, −0.25; P=0.03), and cardiac index (SMD: −0.73; 95% CI: −1.14, −0.03; P=0.004) and increased systemic vascular resistance index (SVRI) (SMD: 1.03; 95% CI: 0.61, 1.45; P<0.0001). This Bayesian meta-analysis revealed a possible rank of probability of mortality among the eleven vasopressor agents or vasopressor combinations; from lowest to highest, they are NE+DB, EN, TP, NE+EN, TP+NE, VP, TP+DB, NE, PE, NE+DX, and DA.
Conclusion
In terms of survival, NE may be superior to DA. Otherwise, there is insufficient evidence to suggest that any other vasopressor agent or vasopressor combination is superior to another. When compared to DA, NE is associated with decreased heart rate, cardiac index, and cardiovascular adverse events, as well as increased SVRI. The effects of vasopressor agents or vasopressor combinations on mortality in patients with septic shock require further investigation.
Introduction
Septic shock is a life-threatening condition and severe sepsis accounts for 20% of all admissions to intensive care units.Citation1 Severe sepsis approximates 750,000 cases annually in the USA and has a mortality rate averaging 28%.Citation2 For initial resuscitation, intravenous fluids are recommended as the first-line therapy. However, vasopressor agents are also critical to achieve and maintain adequate blood pressure and tissue perfusion, and hence, should be used early.Citation3 Sakr et alCitation4 reported that the most frequently used vasopressor agent during septic shock was norepinephrine (NE, 80.2%), followed by dopamine (DA, 35.4%), and epinephrine (EN, 23.3%) alone or in combination. Although NE is recommended as the fist-line agent for treating hypotension in volume-resuscitated hyperdynamic septic shock,Citation5 the second-line vasopressor remains controversial. Previous studies have reported that NE may have significant superiority over DA in terms of survival.Citation5–Citation8 However, compared with other vasopressors, such as EN, vasopressin (VP), terlipressin (TP), and phenylephrine (PE), the outcomes on the use of NE were not different. Morelli et alCitation9 reported that there was no difference in terms of cardiopulmonary performance, global oxygen transport, and regional hemodynamics when PE was administered instead of NE in the initial hemodynamic support of septic shock. Russell et alCitation10 revealed that low-dose VP did not improve survival rates in contrast with NE in septic shock patients treated with catecholamine vasopressors. Additionally, EN was recommended as an additional agent to NE to maintain adequate blood pressure.Citation5 Recently in a single-center randomized controlled trial (RCT), NE supplemented by dobutamine (DB) was compared to NE supplemented by EN in the treatment of septic shock patients.Citation11 However, the effectiveness of other vasopressor agents or vasopressor combinations as compared to others is limited. Whether the use of any vasopressor agents or vasopressor combinations in patients with septic shock translates to a survival advantage remains unclear. Meta-analyses of vasopressor agents have been limited by considering only two or three categories of vasopressor agents, not including indirect and direct comparisons, and omission of recent RCTs. Therefore, we performed a network meta-analysis (NMA) considering direct and indirect comparisons of vasopressor agents and vasopressor combinations in reducing overall mortality for septic shock patients.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA Statement) guidelines were used to perform this meta-analysis.Citation12
Information sources and eligibility criteria
A search of the PubMed (US National Library of Medicine, Bethesda, MD, USA) and Cochrane Library databases and Embase from database inception to December 2014 was performed. The eligibility criteria were as follows: the study design must be randomized controlled, the study must report mortality outcome, and the study must evaluate adult patients at least 18 years of age.
Search strategy
We used text words and medical subject heading (MeSH) terms with Boolean strategy. The cross-searching was done based on the following three categories: 1) vasopressors related (“vasopressor” or “vasoactive drug” or “catecholamine” or “pressor agent”); 2) different vasopressors (“norepinephrine” or “dopamine” or “epinephrine” or “adrenaline” or “isuprel” or “aleudrin” or “vasopressin” or “terlipressin” or “phenylephrine” or “dopexamine”); 3) disease (“sepsis” or “infection” or “septic shock” or “shock” or “systemic inflammatory response syndrome” or “SIRS”). The search was limited to the “English” language and “human” subjects. Further search by reviewing conference proceedings and the references of review articles was performed manually if necessary.
Study selection
Two independent investigators (FZ and ZM) performed the study selection. Differences between the two investigators were resolved by consensus or adjudicated by a third investigator (XZ). Agreement between the two reviewers on study inclusion was excellent (k=1). Studies on adult patients with septic shock that evaluated the mortality rates of different vasopressor agents or vasopressor combinations were selected.
Data extraction
Two investigators independently extracted raw data using a standard form for each study. The form included year of publication, the study type, number of patients, patient characteristics, and details of the outcomes. The main outcome was 28-day mortality. We used the mortality rate from the only undetermined time point or the nearest time point when mortality was reported at only an undetermined time point or several time points, respectively. In addition, we also assessed cardiac adverse events and hemodynamic and metabolic parameters.
Quality assessment
We assessed the quality of each study selected for this meta-analysis by using the Jadad score, which includes the following criteria: randomization, concealment of treatment allocation, clinician blinding, baseline balance between groups, and the description of withdrawals and dropouts.Citation13
Statistical analysis
A meta-analysis was performed to calculate direct estimates of treatment effect for each pair of vasopressor agents or vasopressor combinations. According to heterogeneity of treatment effect across trials using the I2-statistics,Citation14 a fixed-effect model (P≥0.1) or random-effects model (P<0.1) was used. Results in terms of odds ratio (OR) for dichotomous outcomes or standardized mean difference (SMD) for continuous data were expressed with mean and 95% confidence intervals (CIs). The direct meta-analysis was done using Review Manager, version 5.1.2 (RevMan; The Cochrane Collaboration, Oxford, UK).
Using a Bayesian framework, we performed random-effects NMAs for each vasopressor agent or vasopressor combination. NMA is a recent emerging approach used to evaluate the effect size of all possible pairwise comparisons even if they are not compared head-to-head.Citation15 Results such as ORs are expressed with 95% CIs. These CIs from NMAs are the Bayesian analogs of the 95% CIs.Citation15 The models had 80,000 iterations, while a burn-in of 40,000 and a thin of 10 were used.Citation16 Vague priors were used.Citation16 All convergence on the basis of Brooks–Gelman–Rubin plots was assessed.Citation16 Cumulative probability plot (cumulative probability vs rank curve) is presented. Using R-project 3.1.1, the Z-test was conducted to assess for inconsistency of triangular loops.Citation17 Area under the cumulative probability curve represents the rank of probability. The analysis for the NMA was performed using WinBUGS1.4.3 (Medical Research Council Biostatistics Unit; www.mrc-bsu.cam.ac.uk/software/bugs/) and R-project 3.1.1 (http://cran.r-project.org/). Publication bias was tested by funnel plots whenever possible.
Results
Study selection
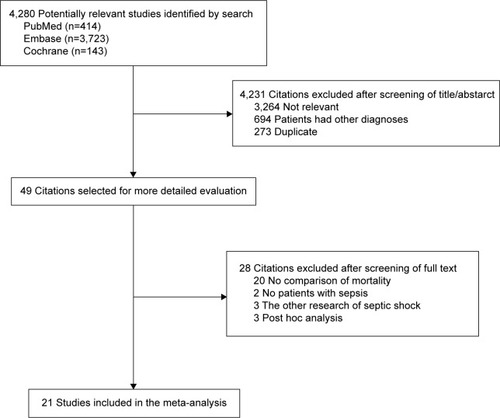
There were 4,280 potentially relevant studies, and 49 articles were retrieved for detailed assessment. Twenty-eight articles were excluded because there were no mortality comparisons (n=20), no sepsis patients (n=2), other septic shock investigations (n=3), and post hoc analyses (n=3). Twenty-one studies were included in this meta-analysis ().Citation9–Citation11,Citation18–Citation35 To evaluate hemodynamic outcomes, we extracted heart rate (HR), mean arterial pressure (MAP), systemic vascular resistance index (SVRI), cardiac index, and mortality data from studies by Russell et alCitation10 and Gordon et al.Citation30
Study characteristics
Fourteen single-centerCitation9,Citation11,Citation18–Citation24,Citation26,Citation29,Citation31,Citation32,Citation34 and seven multicenter studiesCitation10,Citation25,Citation27,Citation28,Citation30,Citation33,Citation35 were identified. The characteristics and inclusion criteria of the selected RCTs are summarized in . These articles were reported between 1993 and 2012, and a total of 3,819 patients were included in this study. Inclusion criteria were not the same for all trials; however, all patients met the diagnosis of severe sepsis or septic shock ().Citation36 Mean age ranged from 18 years to 70 years, and the proportion of male patients ranged from 46% to 77.3%. The mean Acute Physiology and Chronic Health Evaluation II (APACHE II) score was 23.8.
Table 1 Characteristics of the included randomized trials
All studies evaluated the vasopressor effects in patients with septic shock by using a primary outcome such as survival, hemodynamics, or APACHE II score (). Vasopressor agents include NE,Citation9,Citation10,Citation18–Citation20,Citation23,Citation25,Citation26,Citation28–Citation35 EN,Citation21,Citation22,Citation24,Citation27,Citation28 VP,Citation10,Citation25,Citation30,Citation31,Citation33 DA,Citation18–Citation20,Citation26,Citation34,Citation35 TP,Citation23,Citation31 PE,Citation9,Citation32 NE+DB,Citation11,Citation21,Citation22 NE+EN,Citation11 TP+NE,Citation9 TP+DB,Citation9 and NE + dopexamine (DX) (, ).Citation24 The mortality data from the RCT by De Backer et alCitation7,Citation35 were extracted from their meta-analysis.
Figure 2 Network of eligible comparisons for the multiple-treatment meta-analysis for mortality.
Abbreviations: DA, dopamine; DB, dobutamine; DX, dopexamine; EN, epinephrine; NE, norepinephrine; PE, phenylephrine; TP, terlipressin; VP, vasopressin.
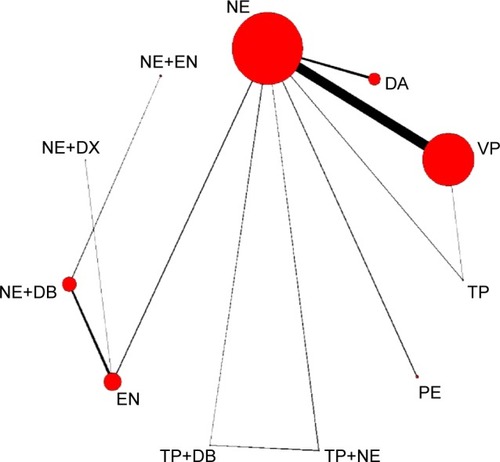
Table 2 The interventions of different vasopressors in the included randomized trials
Risk of bias within studies
Only RCTs were included in the analysis. Sequence of randomized allocation was reported in all but two studies.Citation22,Citation34 Blinding was conducted in nine studies.Citation9–Citation11,Citation20,Citation27,Citation30,Citation32,Citation33,Citation35 The mean Jadad score was 3.3.
Effect of different vasopressor agents on mortality
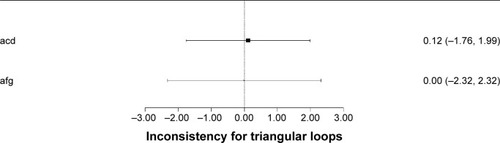
Mortality in these 21 trials was 50.1% (1,915/3,819). When compared to NE, DA was associated with increased mortality (OR: 1.24, 95% CI: 1.01, 1.53). However, there was no significant difference in mortality in direct or indirect comparisons between other different vasopressor agents and vasopressor combinations (P>0.05) (). For the probability of mortality, the possible rank from low to high was NE+DB (area under the curve [AUC]: 0.2648), EN (AUC: 0.3473), TP (AUC: 0.379), NE+EN (AUC: 0.3943), TP+NE (AUC: 0.3967), VP (AUC: 0.4212), TP+DB (AUC: 0.5423), NE (AUC: 0.5752), PE (AUC: 0.6796), NE+DX (AUC: 0.7279), and DA (AUC: 0.7718) ( and ). The tests of inconsistency for the two triangular closed loops were not significant (). This meant that direct and indirect estimates had similar effects in the closed loop.Citation15,Citation17
Figure 3 Mortality of different vasopressors in direct comparison and network meta-analysis in terms of mortality.
Abbreviations: CI, confidence interval; DA, dopamine; DB, dobutamine; DX, dopexamine; EN, epinephrine; NE, norepinephrine; NMA, network meta-analysis; OR, odds ratio; PE, phenylephrine; TP, terlipressin; VP, vasopressin.
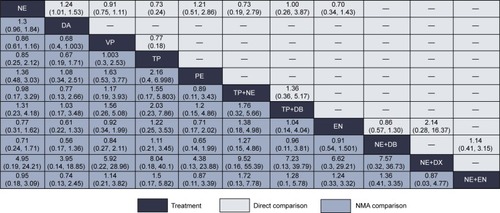
Figure 4 Ranking for mortality.
Abbreviations: DA, dopamine; DB, dobutamine; DX, dopexamine; EN, epinephrine; NE, norepinephrine; PE, phenylephrine; TP, terlipressin; VP, vasopressin.
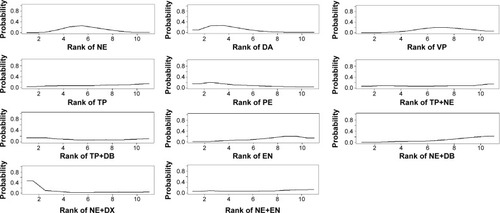
Figure 5 The cumulative probability plot.
Abbreviations: DA, dopamine; DB, dobutamine; DX, dopexamine; EN, epinephrine; NE, norepinephrine; PE, phenylephrine; TP, terlipressin; VP, vasopressin.
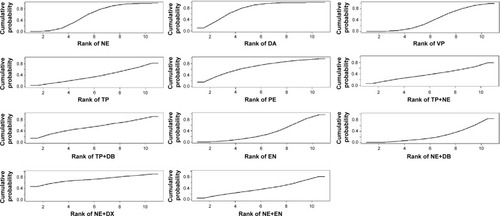
Figure 6 Inconsistency for triangular loops.
Effect of different vasopressor agents on cardiac adverse events
Included studies compared NE vs DA, NE vs VP, NE vs TP, NE vs PE, TP+NE vs TP+DB, and TP+DB vs EN directly. We performed direct meta-analysis of cardiac adverse events, which mainly consisted of arrhythmias and tachycardia. NE decreased cardiac adverse events significantly compared to DA (). No significant difference in cardiac adverse events was found between other vasopressor agents and vasopressor combinations.
Table 3 Direct comparison of different vasopressors on cardiac adverse events
Effect of different vasopressors on hemodynamic and metabolic parameters
Thirteen studies reported that there were significant differences in the effect on hemodynamics,Citation10,Citation11,Citation18,Citation20,Citation22–Citation26,Citation29–Citation32 and eleven studies reported that there were significant differences on metabolic parameters or organ function between vasopressor agents and vasopressor combinations ().Citation11,Citation18–Citation22,Citation24–Citation26,Citation29,Citation31,Citation33
Four trials with complete data compared the treatment of NE and DA.Citation18–Citation20,Citation26 The results revealed that NE decreased HR (SMD: −2.10; 95% CI: −3.95, −0.25; P=0.03) and cardiac index (SMD: −0.73; 95% CI: −1.14, −0.03; P=0.004) and increased SVRI (SMD: 1.03; 95% CI: 0.61, 1.45; P<0.0001), but there was no significant difference on MAP, oxygen delivery (DO2), oxygen consumption (VO2), and lactate. In contrast, as compared to NE, VP significantly decreased HR (SMD: 0.21; 95% CI: 0.07, 0.34; P=0.003).
Compared to the NE+DB combination, EN did not show a significant difference in HR, MAP, cardiac index, pulmonary MAP, DO2, VO2, and lactate (). However, the NE+EN combination was more effective than the NE+DB combination in reversing the abnormalities of cardiovascular parameters, and the NE+EN group had significantly higher MAP, HR, CVP, cardiac index, SVRI, ejection fraction, left ventricular end diastolic volume, DO2, lactate, and urine output.Citation11
Table 4 Direct comparison of different vasopressors on hemodynamic and metabolic parameters
Discussion
Twenty-one trials that included 3,819 patients and that compared different vasopressor agents or vasopressor combinations in septic shock were identified and included in this systematic review and NMA of RCTs. The trials’ mean Jadad score was 3.3, which means that they were of high quality. The main results showed that except for the superiority of NE over DA in direct comparison, the mortality of patients treated with any other vasopressor agent or vasopressor combination was not significantly different. NE was also associated with decreased cardiac adverse events, HR, and cardiac index, as well as increased SVRI, as compared to DA.
Our meta-analysis revealed a possible rank of probability of mortality among the eleven vasopressor agents or vasopressor combination; from low to high, they are NE+DB, EN, TP, NE+EN, TP+NE, VP, TP+DB, NE, PE, NE+DX, and DA. However, variations in each RCT’s inclusion criteria may have influenced the probability of mortality. Thus, this ranking should be interpreted with caution.
Our NMA evaluated the vasopressor agents or vasopressor combinations from both direct and indirect comparisons. This approach differs from traditional head-to-head meta-analysis. Some traditional meta-analyses of RCTs have compared only two or three vasopressor agents, such as NE, DA, and VP.Citation10,Citation35 However, other types of comparisons have never been performed. This NMA compared any vasopressor agent or vasopressor combination to others and revealed a possible rank of probability of mortality.Citation15
Three factors support the internal validity of our analysis. First, a rigorous and extensive literature search was conducted, and the number of selected studies was more than any in previous meta-analyses focusing on vasopressor agents and vasopressor combinations for the treatment of septic shock. Second, the selected trials are considered high-quality studies, with a mean Jadad score of 3.3 points. Third, tests of inconsistency for triangular loops were not significant; in other words, the direct and indirect estimates had similar effects. This finding supports that our NMA has adequate homogeneity, which translates to more confidence in support of the results.
Vasopressor therapy is recommended by every major clinical practice guideline when fluid resuscitation fails to maintain adequate blood pressure and organ perfusion. However, different vasopressor agents and vasopressor combinations increase blood pressure through different mechanisms, leading to heterogeneity of physiological effects.Citation37 NE is the first-line vasopressor agent used to treat septic shock (grade 1B)Citation5 and is associated with lower mortality compared to DA.Citation6,Citation7 Although the typical order for the addition of vasopressor agents is NE, epinephrine, VP, DA, and PE,Citation38 the supporting evidence for this order is limited except for the superiority of NE over DA in terms of mortality.Citation6,Citation7 NE supplemented with EN is the second choice in treating septic shock (grade 2B).Citation5 In this meta-analysis, only one study reported NE+EN vs NE+DB.Citation11 The rank of probability of mortality revealed that NE+EN had lower risk than NE. VP is neither recommended nor suggested (grade UG) but can be added to NE with the intent of either raising MAP or decreasing NE dosage.Citation5,Citation38 PE, which is used to stimulate purely α-1 receptors, is recommended when cardiac output is known to be high and the target blood pressure is not achieved (grade 1C).Citation5 No significant difference between PE and other vasopressor agents or vasopressor combinations was found. Similar results were also found in the comparison between other vasopressor agents or vasopressor combinations. Recently, a trial compared the vasopressor effects of NE+DB and NE+EN on the cardiovascular support of patients with septic shock.Citation11 To better evaluate any mortality benefit from the initial vasopressor used, we also compared vasopressor combinations of NE+DB, TP+NE, TP+DB, NE+EN, and NE+DX. The results showed that the vasopressor combination NE+DB had the lowest probability of mortality, and this finding may be supported by the rapid normalization of both gastric–arterial difference (PCO2 gap) and gastric intramu-cosal pH.Citation22 No other vasopressor combination is superior to another in both direct and indirect comparisons.
For cardiac adverse events and hemodynamic and metabolic parameters, we conducted only direct comparisons because the small number of studies failed to form an effective network analysis loop. Our direct meta-analysis revealed that cardiac adverse events, HR, and cardiac index were decreased and SVRI was increased on treatment with NE compared to the results of treatment with DA. These results support the notion that NE may have stronger α-receptor effects, resulting in a greater increase in SVRI and blood pressure as compared to DA.Citation4,Citation39 Even though some studies favored NE as the more effective vasopressor agent to maintain adequate MAP during septic shock, no significant difference in terms of effect on MAP between these two vasopressor agents has ever been detected.Citation20,Citation40 Overall, NE is probably more effective than DA in hemodynamic support for septic shock patients.
A previous trial reported that VP might increase SVRI and decrease cardiac index compared to baseline, while NE did not.Citation25 Meta-analysis that included two trials failed to find any significant difference in cardiac adverse events as well as hemodynamic and metabolic parameters between NE and VP.
Statistically, with 80% power and two-sided alpha level of 0.04, to detect a 15% relative difference in 28-day mortality rate, at least 765 subjects in each group were needed.Citation35 In the present meta-analysis, only “NE vs VP” (n=1,799) and “NE vs DA” (n=1,408) comparisons had potentially adequate sample size.
Limitations
Our analysis has many limitations. First, only English language articles were included in this study, which may have affected the findings due to selection bias. Second, although 21 trials were included in this study, the actual sample size population in specific comparisons was small, and the risk of false attribution of positive effect from pooling small trials is well known. Moreover, differences in each RCT’s inclusion criteria may have influenced the probability of mortality. Additionally, publication bias analysis could not be conducted. Hence, we do not think that these results constitute a reason to change clinical practice, but rather, they support the need for further investigations.
Conclusion
In terms of survival, NE may be superior to DA. Otherwise, there is insufficient evidence to suggest that any other vasopressor agent or vasopressor combination is superior to another. When compared to DA, NE is associated with decreased cardiac adverse events, HR, and cardiac index, as well as increased SVRI. The effects of vasopressor agents or vasopressor combinations on patients with septic shock require further investigation by larger-scale RCTs.
Disclosure
The authors report no conflicts of interest in this work.
References
- LevyMMDellingerRPTownsendSRThe surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsisCrit Care Med201038236737420035219
- AngusDCLinde-ZwirbleWTLidickerJClermontGCarcilloJPinskyMREpidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of careCrit Care Med20012971303131011445675
- BeckVChateauDBrysonGLCooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research GroupTiming of vasopressor initiation and mortality in septic shock: a cohort studyCrit Care2014183R9724887489
- SakrYReinhartKVincentJLDoes dopamine administration in shock influence outcome? Results of the sepsis occurrence in acutely ill patients (SOAP) studyCrit Care Med200634358959716505643
- DellingerRPLevyMMRhodesASurviving Sepsis Campaign Guidelines Committee including The Pediatric SubgroupSurviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012Crit Care Med201341258063723353941
- VasuTSCavallazziRHiraniAKaplanGLeibyBMarikPENorepinephrine or dopamine for septic shock: systematic review of randomized clinical trialsJ Intensive Care Med201227317217821436167
- De BackerDAldecoaCNjimiHVincentJLDopamine versus norepinephrine in the treatment of septic shock: a meta-analysis*Crit Care Med201240372573022036860
- BartelBNorepinephrine vs dopamine: new recommendations for initial vasopressor selection in septic shockS D Med201467520020124851468
- MorelliAErtmerCRehbergSPhenylephrine versus norepinephrine for initial hemodynamic support of patients with septic shock: a randomized, controlled trialCrit Care2008126R14319017409
- RussellJAWalleyKRSingerJVASST InvestigatorsVasopressin versus norepinephrine infusion in patients with septic shockN Engl J Med2008358987788718305265
- MahmoudKAmmarANorepinephrine supplemented with dobutamine or epinephrine for the cardiovascular support of patients with septic shockIndian J Crit Care Med2012162758022988361
- MoherDLiberatiATetzlaffJAltmanDGPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementInt J Surg20108533634120171303
- JadadARMooreRACarrollDAssessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials19961711128721797
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in meta-analysesBMJ2003327741455756012958120
- MillsEJIoannidisJPThorlundKSchunemannHJPuhanMAGuyattGHHow to use an article reporting a multiple treatment comparison meta-analysisJAMA2012308121246125323011714
- RochwergBAlhazzaniWSindiAFluids in Sepsis and Septic Shock GroupFluid resuscitation in sepsis: a systematic review and network meta-analysisAnn Intern Med2014161534735525047428
- ZhangCYanJSunFLiuQGuoYZengXDifferentiation and handling of homogeneity in network meta-analysisChin J Evid Based Med2014147884888
- MarikPEMohedinMThe contrasting effects of dopamine and norepinephrine on systemic and splanchnic oxygen utilization in hyperdynamic sepsisJAMA199427217135413577933396
- RuokonenETakalaJKariASaxenHMertsolaJHansenEJRegional blood flow and oxygen transport in septic shockCrit Care Med1993219129613038370292
- MartinCPapazianLPerrinGSauxPGouinFNorepinephrine or dopamine for the treatment of hyperdynamic septic shock?Chest19931036182618318404107
- LevyBBollaertPECharpentierCComparison of norepinephrine and dobutamine to epinephrine for hemodynamics, lactate metabolism, and gastric tonometric variables in septic shock: a prospective, randomized studyIntensive Care Med19972332822879083230
- SeguinPBellissantELe TulzoYEffects of epinephrine compared with the combination of dobutamine and norepinephrine on gastric perfusion in septic shockClin Pharmacol Ther200271538138812011824
- AlbaneseJLeoneMDelmasAMartinCTerlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized studyCrit Care Med20053391897190216148457
- SeguinPLaviolleBGuinetPMorelIMalledantYBellissantEDopexamine and norepinephrine versus epinephrine on gastric perfusion in patients with septic shock: a randomized study [NCT00134212]Crit Care2006101R3216507156
- LauzierFLevyBLamarrePLesurOVasopressin or norepinephrine in early hyperdynamic septic shock: a randomized clinical trialIntensive Care Med200632111782178917019548
- MathurSDhunnaRChakrabortyAComparison of norepinephrine and dopamine in the management of septic shock using impedance cardiographyIndian J Crit Care Med2007114186191
- AnnaneDVignonPRenaultACATS Study GroupNorepinephrine plus dobutamine versus epinephrine alone for management of septic shock: a randomised trialLancet2007370958867668417720019
- MyburghJAHigginsAJovanovskaALipmanJRamakrishnanNSantamariaJA comparison of epinephrine and norepinephrine in critically ill patientsIntensive Care Med200834122226223418654759
- MorelliAErtmerCLangeMEffects of short-term simultaneous infusion of dobutamine and terlipressin in patients with septic shock: the DOBUPRESS studyBr J Anaesth2008100449450318308741
- GordonACWangNWalleyKRAshbyDRussellJAThe cardiopulmonary effects of vasopressin compared with norepinephrine in septic shockChest2012142359360522518026
- MorelliAErtmerCRehbergSContinuous terlipressin versus vasopressin infusion in septic shock (TERLIVAP): a randomized, controlled pilot studyCrit Care2009134R13019664253
- JainGSinghDKComparison of phenylephrine and norepinephrine in the management of dopamine-resistant septic shockIndian J Crit Care Med2010141293420606906
- GordonACRussellJAWalleyKRThe effects of vasopressin on acute kidney injury in septic shockIntensive Care Med2010361839119841897
- PatelGPGraheJSSperryMEfficacy and safety of dopamine versus norepinephrine in the management of septic shockShock201033437538019851126
- De BackerDBistonPDevriendtJSOAP II InvestigatorsComparison of dopamine and norepinephrine in the treatment of shockN Engl J Med2010362977978920200382
- BoneRCBalkRACerraFBACCP/SCCM Consensus Conference CommitteeDefinitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care MedicineChest19921016164416551303622
- HollenbergSMInotrope and vasopressor therapy of septic shockCrit Care Clin200925478180219892253
- ArellanoDLHannemanSKVasopressor weaning in patients with septic shockCrit Care Nurs Clin North Am201426341342525169693
- BraccoDPharmacologic support of the failing circulation: practice, education, evidence, and future directionsCrit Care Med200634389089216505669
- ReinhartKSakkaSGMeier-HellmannAHaemodynamic management of a patient with septic shockEur J Anaesthesiol200017161710758438