Abstract
Objective
The objective of this study is to investigate the association of body mass index (BMI) with arterial stiffness assessed by cardioankle vascular index (CAVI).
Subjects and methods
A retrospective cross-sectional study was conducted in 23,257 healthy Japanese subjects (12,729 men and 10,528 women, aged 47.1 ± 12.5 years, BMI 22.9 ± 3.4 kg/m2) who underwent health screening between 2004 and 2006 in Japan. Exclusion criteria were current medication use and a past history of cardiovascular disease, hypertension, stroke, diabetes, and nephritis.
Results
Male subjects showed significantly higher BMI, CAVI, and triglycerides and lower high-density lipoprotein (HDL)-cholesterol compared with female subjects. Next, the subjects were divided into tertiles of BMI: lower, middle, and upper, in a gender-specific manner. After adjusting for confounders including age, systolic blood pressure, and HDL-cholesterol identified by multiple regression analysis, the mean CAVI decreased progressively as BMI tertile increased in both genders. Furthermore, a negative inverse relationship between BMI and adjusted CAVI was observed throughout the BMI distribution. Multivariate logistic regression model for contributors of high CAVI (≥90th percentile) identified obesity (odds ratios (95% confidence interval): 0.804 (0.720–0.899)], older age [15.6 (14.0–17.4)], male gender [2.26 (2.03–2.51)], hypertension [2.28 (2.06–2.54)], impaired fasting glucose [1.17 (1.01–1.37)], and low HDL-cholesterol [0.843 (0.669–1.06)] as independent factors.
Conclusion
We demonstrated an inverse relationship between CAVI and BMI in healthy Japanese subjects, suggesting that systemic accumulation of adipose tissue per se may lead to a linear decrease of arterial stiffness in nonobese and obese subjects without metabolic disorders.
Introduction
Overweight and obesity are defined as abnormal or excessive fat accumulation that may impair healthCitation1 and have been reported to be associated with glucose in tolerance, dyslipidemia, and hypertension, thus increasing cardiovascular risks.Citation2,Citation3 Furthermore, cardiovascular disease (CVD) is the leading cause of death worldwide.Citation4 On the other hand, underweight is also associated with increased all-cause mortality compared to normal weight after adjustment for covariates.Citation5–Citation8 It is an obvious fact that body fat distribution influences morbidity and mortality. Thus, healthy ranges for percentage body fat (%BF) should be considered in the management of intensive therapeutic approaches for obesity.Citation9–Citation11 The most commonly used surrogate marker of %BF is body mass index (BMI), which is calculated from a person’s height and weight. BMI is reliable and provides a fair indication of body fat level but is not a perfect system for measuring body fat.Citation12–Citation14 A BMI <18.5 kg/m2 is defined as underweight and a BMI >25 kg/m2 as overweight. Actually, numerous studies have documented a U- or J-shaped association between BMI and mortality and an association of increased mortality rate with relatively low or high BMI.Citation15,Citation16 In Japan, the ideal body weight that is associated with the lowest mortality corresponds to a BMI of 22 kg/m2 in both men and women.Citation17 Arterial stiffness is a significant surrogate marker of subclinical atherosclerosis, and increased arterial stiffness is independently associated with an increased risk of major adverse cardiovascular events (MACEs).Citation18,Citation19
Recently, a novel arterial stiffness diagnostic parameter called cardioankle vascular index (CAVI) has been developed in Japan, which allows quantification of the stiffness parameter beta independent of blood pressure (BP).Citation20–Citation22 This stiffness parameter has adequate reproducibility for clinical useCitation23–Citation27 and is associated with a number of risk factors and severity of CVD.Citation28–Citation33 CAVI has also been reported to be an independent predictor of MACE.Citation34,Citation35 Moreover, an increase in the number of risk factors for metabolic syndrome correlates positively with increased CAVI, probably due to insulin resistance.Citation36 Weight gain most likely contributes to the risk of increase in arterial stiffness. Nevertheless, the relationship between BMI and arterial stiffness has not been fully elucidated.
The aim of this cross-sectional study was to investigate whether BMI is associated independently with arterial stiffness assessed by CAVI after adjustment for covariates in healthy Japanese subjects. Additionally, gender difference in the relationship between BMI and CAVI was also examined.
Subjects and methods
Design
This retrospective cross-sectional study was approved by the Institutional Review Board and Ethics Committee of Sakura Hospital, School of Medicine, Toho University (no S16002). Written informed consent was obtained from the participants.
Data collection and laboratory assay methods
A total of 23,257 Japanese urban residents (12,729 men and 10,528 women) residing in major cities nationwide, who participated in the CVD and cancer screening program provided by the Japan Health Promotion Foundation between 2004 and 2006, were studied. Subjects were excluded if they were taking any medication or had a past history of heart disease, hypertension, stroke, diabetes, nephritis, or gout. Height and body weight were measured, and BMI was calculated [weight (kg) divided by square of height (m2)]. Obesity was defined as BMI ≥25 kg/m2, which is the definition for obesity in adult Japanese population according to the Examination Committee of Criteria for Obesity Disease in Japan.Citation37 Blood was collected from the antecubital vein in the morning after 12-hour fasting to determine γ-glutamyl transpeptidase (γ-GTP), fasting plasma glucose (FPG), glycosylated hemoglobin (HbA1c), total cholesterol (TC), triglycerides (TGs), high-density lipoprotein-cholesterol (HDL-C), creatinine, and uric acid. All the blood levels were measured according to standard procedures. Non-HDL-C was defined as the difference between total and HDL-cholesterol. HbA1c (%) measured by the Japan Diabetes Society (JDC) method was converted to NGSP value (%) using the following formula: HbA1c (NGSP) (%) = HbA1c (JDS) (%) + 0.4%.Citation38 Impaired fasting glucose (IFG) was defined as fasting glucose levels of 100 to 125 mg/dL.Citation39
Measurement of CAVI and BP
CAVI was measured using a VaSera VS-1000 (Fukuda Denshi Co Ltd, Tokyo, Japan) by the methods described previously.Citation20 Cuffs were applied to bilateral upper arms and ankles, with the subject lying supine and the head held in midline position. After resting for 10 minutes, the examinations were performed. To detect the brachial and ankle pulse waves with cuffs, a low cuff pressure from 30 to 50 mmHg was used to ensure minimal effect of cuff pressure on hemodynamics. Furthermore, BP was measured thereafter. Hypertension was defined as systolic BP (sBP) ≥140 mmHg and/or diastolic BP (dBP) ≥90 mmHg.Citation40 Finally, for the convenience of comparison with the pulse wave velocity (PWV), scale conversion was performed. CAVI was calculated by the following formula: CAVI = a{(2r/∆P) × ln(Ps/Pd)PWV2} + b, where Ps is sBP, Pd is dBP, ∆P is Ps − Pd, r is blood density, and a and b are constants. BP was measured from the cuff of the upper arm. PWV was obtained by dividing the vascular length by the time for which the pulse wave propagated from the aortic valve to the ankle and was measured using cuffs at the upper arms and ankles. All the measurements and calculations were performed automatically by the VaSera. Subjects with ankle–brachial indices <0.90 were excluded, because patients with severe arterial occlusive diseases may give falsely low CAVI.Citation20 The mean coefficient of variation of CAVI measured by this method is <5%, which is sufficiently small for clinical usage and indicates that CAVI has good reproducibility.Citation25
Statistical analysis
All data are expressed as mean ± standard deviation. The SPSS software (version 11.5; SPSS Inc, Chicago, IL, USA) was used for statistical processing. Student’s t-test was performed to examine gender difference in clinical variables. The relationship between CAVI and clinical variables was analyzed using multiple regression analysis. The relationship of CAVI with BMI was analyzed using analysis of variance (ANOVA) after adjusting for confounders of CAVI, together with trend analysis. Logistic regression analysis was used to identify contributors of high CAVI (≥90th percentile) and expressed as odds ratio (OR) with 95% confidence interval (CI). In all comparisons, P values <0.05 were considered statistically significant.
Results
Characteristics of male and female participants
In this study, a total of 23,257 Japanese urban residents (12,729 men and 10,528 women) aged from 20 to 74 (mean 47.1 ± 12.5) years were screened. compares the clinical characteristics of male and female participants. Compared with women, men had significantly and markedly higher BMI (23.9 ± 3.2 vs. 21.7 ± 3.3 kg/m2, P = 0.003) and CAVI (7.96 ± 1.14 vs. 7.69 ± 0.97, P < 0.001).
Table 1 Characteristics of male and female participants
Prevalence of major cardiovascular risk factors
The prevalence of traditional cardiovascular risks in participants is shown in . The proportions of older age, obesity, and hypertension were significantly (P < 0.001) higher in men than in women, whereas the proportions of IFG and low HDL-cholesterol (defined as HDL-C <40 mg/dL) were not significantly different ().
Table 2 Prevalence of major cardiovascular risk factors
Correlation of CAVI with clinical variables analyzed by multiple regression model
Next, we examined the factors associated with CAVI. summarizes the results of a multiple regression analysis for the correlation between CAVI and clinical variables. TG was also omitted because of intraclass correlation with HDL-C, and non-HDL-C was added instead. Age was a major independent predictor of CAVI (b coefficient = 0.584, P < 0.001). Additionally, a low correlation between CAVI and gender (b = 0.149, P < 0.001), BMI (b = −0.119, P < 0.001), sBP (b = 0.139, P < 0.001), or HDL-C (b = 0.107, P < 0.001) was observed. These confounders, except gender and BMI, were adjusted in subsequent analyses of CAVI as shown in and .
Figure 1 Relationship between adjusted cardioankle vascular index and BMI in (A) male and (B) female subjects.
Abbreviations: BMI, body mass index; CAVI, cardioankle vascular index; sBP, systolic blood pressure; HDL-C, high-density lipoprotein-cholesterol.
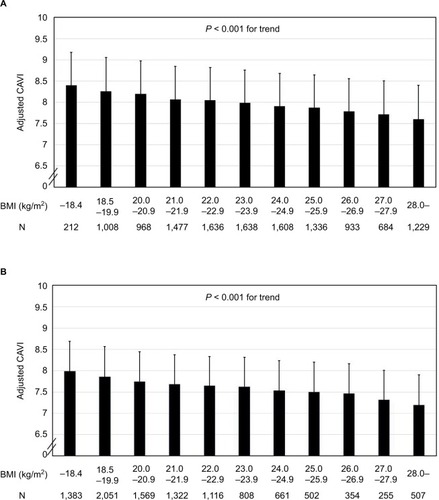
Table 3 Correlation of cardioankle vascular index with clinical variables analyzed by multiple regression model
Table 4 Characteristics of male and female participants stratified by tertile of body mass index
Characteristics of male and female participants stratified by tertiles of BMI
Participants were divided into men and women, and each gender group was stratified by BMI tertiles into the following three groups: lower (T1), middle (T2), and upper tertile (T3). Among 12,729 men, 4,181 were stratified into T1 (BMI ≤22.2 kg/m2), 4,365 into T2 (22.3–24.9 kg/m2), and 4,183 into T3 (≥25.0 kg/m2). Among 10,528 women, 3,585 were stratified into T1 (≤20.0 kg/m2), 3,462 into T2 (20.1–22.5 kg/m2), and 3,481 into T3 (≥22.6 kg/m2). compares their clinical characteristics. CAVI was adjusted for confounders identified in the multiple regression model as shown in . In both genders, sBP, dBP, γ-GTP, FPG, HbA1c, TC, TG, and non-HDL-C increased, while adjusted CAVI and HDL-C decreased progressively with increasing BMI tertile.
ORs (95% CIs) for high CAVI (≥90th percentile)
Furthermore, we examined the factors associated with high CAVI using multivariate logistic regression model with dichotomous variables (). High CAVI was defined as ≥90th percentile of CAVI (9.20 in all participants). Gender and major cardiovascular risks were entered into the model as shown in . The analysis identified the following factors to be independently associated with high CAVI: male gender (OR: 2.26, P < 0.001), older age (OR: 15.6, P < 0.001), hypertension (OR: 2.28, P < 0.001), and IFG (OR: 1.17, P = 0.0428). Interestingly, obesity correlated negatively with high CAVI (OR: 0.804, P < 0.001). Low HDL-cholesterol was not a significant independent predictor of high CAVI.
Table 5 OR (95% CI) for high cardioankle vascular index (≥90th percentile)
Relationship of adjusted CAVI with BMI in men and women
shows the relationship of adjusted CAVI with BMI in () men and () women. In both genders, a trend test after ANOVA detected an inverse linear relationship (P < 0.001) between adjusted CAVI and BMI throughout the entire BMI distribution.
Discussion
In this cross-sectional study, gender, age, BMI, BP, and HDL-cholesterol were major independent variables associated with CAVI in 23,257 healthy Japanese subjects. After adjusting for confounders, CAVI correlated negatively with BMI in both genders. Furthermore, obesity was identified as an independent negative predictor of high CAVI (≥90th percentile), while male gender, hypertension, and IFG were found to be independent positive predictors. Consequently, the present study is the first report to demonstrate an inverse relationship between CAVI and BMI in healthy middle-aged subjects. Note that most of the participants in the present study were nonobese subjects without metabolic disorders. If the study was conducted in obese subjects with metabolic disorders, the results might have been markedly different.
Weight gain has been associated with vascular remodeling and increased cardiovascular mortality.Citation41 CAVI has been shown to be high in the abdominal obesity/metabolic syndrome and decrease by body weight reduction.Citation42 Insulin resistance, a consequence of weight gain, has been recognized as an independent predictor of vascular stiffening and other elements of diabetic vasculopathy.Citation43 Our finding of an inverse relationship between CAVI and BMI might seem inconsistent with previous reports. However, the interaction of weight gain with insulin resistance in the regulation of vascular pathophysiology involves complex mechanisms that are not fully understood. Thus, the mechanism of vascular adaptation to fat accumulation remains controversial. In fact, a negative association of obesity with vascular stiffening has been reported in children and adolescentsCitation44–Citation46 but not in older adults or the elderly.Citation47–Citation50 We therefore stratified the participants in this study by age into tertiles: lower (33.1 ± 5.0 years, n = 7,878), middle (47.1 ± 3.8 years, n = 7,577), and upper (61.0 ± 6.1 years, n = 7,802) and investigated the contribution of BMI to CAVI in each group using logistic regression analysis. We found approximately equal degree of inverse relationship between CAVI and BMI in all three tertiles (data not shown). However, these data do not imply a similar inverse relationship between CAVI and BMI in elderly subjects. While weight gain is a risk factor for CVD, an inverse relationship between BMI and CAVI was observed in the present study. An increase in number of risk factors for metabolic syndrome has been shown to correlate positively with an increase in CAVI.Citation36 Furthermore, we observed previously that weight reduction resulted in a decrease of CAVI in 47 obese (BMI: 33.3 ± 7.5 kg/m2) Japanese subjects with metabolic disorders.Citation42 In that study, change in visceral fat area alone contributed to the change in CAVI. From the previous findings, we hypothesize that systemic accumulation of adipose tissue per se leads to decreased arterial stiffness in nonobese subjects and in obese subjects without metabolic disorders, and excessive accumulation of visceral fat may induce an increase in arterial stiffness from insulin resistance. However, the mechanism and the threshold of the effect of BMI on change in arterial stiffness are not fully understood. Despite weight gain being a risk of CVD development, an obesity paradox exists in which obese patients with heart failure, hypertension, and chronic renal disease have better prognosis with lower mortality than normal weight individuals.Citation51–Citation54 For example, ~10–25% of obese individuals are metabolically healthy due to preserved insulin sensitivity.Citation55 The plausible mechanisms for this reverse epidemiology may be explained by greater metabolic reserves, less cachexia, attenuated response to renin–angiotensin–aldosterone system, increased muscular strength, implications related to cardiorespiratory fitness, and others. Furthermore, various protective cytokines and neuroendocrine profiles in obese patients may account for this phenomenon.Citation56–Citation58 Similarly, adipose tissue-derived cytokines may explain the paradox in arterial stiffness observed in the present study. Shiba et alCitation59 reported that intravitreal injection of antivascular endothelial growth factor (anti-VEGF) drugs decreased CAVI and carotid intima–media thickness, probably due to attenuation of vasa vasorum and improved kidney function. Inhibition of angiogenesis inducers such as VEGF may therefore result in a decrease in arterial stiffness. On the other hand, tenomodulin (TNMD), a putative angiogenesis inhibitor, has been shown to be highly expressed in human adipose tissue, especially in obese subjects.Citation60 Furthermore, a recent study suggests that TNMD acts as a protective factor in visceral adipose tissue to alleviate insulin resistance in obesity.Citation61 We have previously reported that improved insulin resistance may contribute to decreased CAVI in obeseCitation42 and type 2 diabetic patients.Citation62–Citation64 These reports suggest that adipose tissue may affect systemic vascular function through expression of antiangiogenic factors such as TNMD. However, whether the decrease in arterial stiffness through inhibition of angiogenesis provides favorable effects is questionable, because antiangiogenic factor may impair the development of collaterals, which is an important mechanism to compensate for obstructive artery disease.Citation65 Further elucidation of the cause–effect relationship between accumulation of adipose tissue and regulation of arterial pathophysiology is required.
What is the clinical efficacy of our findings? We hypothesized that CAVI might be useful to exclude “malignant obesity”, which was rapidly needed to receive intensive medical interventions. Obese subjects with relatively low CAVI may reveal “benign obesity”, which means normal metabolic features despite increased adiposity, and they may be allowed a period of grace for atherogenesis. Of course, metabolically healthy overweight/obese individuals may be needed to receive permanent medical follow-up because of increased risk of adverse long-term outcomes after all.Citation66
Gender difference in CAVI has been reported previously.Citation21 Similarly, in this study, mean CAVI was higher in men (7.96 ± 1.14) than in women (7.69 ± 0.97), despite almost the same age in both groups (47.0 ± 13.0 in men and 47.1 ± 12.0 years in women). The mechanism of this gender difference in CAVI remains uncertain, although gender-related differences in body fat distribution may partly explain the phenomenon.
In 2002, brachial–ankle PWV (baPWV) was proposed to be a marker of vascular damage and was reported to be a predictive marker of CVD.Citation67 Furthermore, baPWV correlates strongly with aortic (carotid–femoral) PWV, an established index of central arterial stiffness.Citation68 However, PWV is known to depend on BP at the time of measurement. Therefore, the validity of PWV in reflecting actual arterial stiffness is controversial, and this parameter is unsuitable for evaluating the effect of antihypertensive drugs on the arterial wall. On the other hand, CAVI is independent of BP, which makes it more precise and reproducible than PWV as an index of arterial stiffness, whereas its predictive value of cardiovascular events has not been established adequately.Citation69 Additionally, a multiple logistic analysis revealed that CAVI, but not baPWV, was associated with the presence of carotid and coronary arteriosclerosis.Citation29
The limitations of this study include the lack of data on some potential confounders such as proteinuria,Citation70 alcohol consumption, menopause, and smoking status. In addition, the cross-sectional nature of this study does not allow determination of the time course for the development of vascular changes. Therefore, it was not possible to establish the exact pathophysiology linking BMI with CAVI. From these viewpoints, longitudinal cohort studies are needed to clarify the change in relationship between body composition and arterial stiffness during the development of cardiovascular risks.
Conclusion
We demonstrated an inverse linear relationship between CAVI and BMI in healthy Japanese subjects, suggesting that systemic accumulation of adipose tissue per se may lead to a proportionate decrease in arterial stiffness in nonobese subjects and obese subjects without metabolic disorders.
Author contributions
Kohji Shirai contributed to concept/design. Daiji Nagayama contributed to data analysis and interpretation. Ichiro Tatsuno contributed to critical revision of article. Haruki Imamura, Yuta Sato, Takashi Yamaguchi, Noriko Ban, Hidetoshi Kawana, Masahiro Ohira, and Atsuhito Saiki contributed to data interpretation. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We are grateful to Dr. Kenji Suzuki, Japan Health Promotion Foundation, for making enormous contribution in this study, and we gratefully acknowledge the investigators, their coinvestigators, study coordinators, and the patients who participated in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization [webpage on the Internet]Obesity and Overweight: Fact Sheet N0 3112012 Updated June 2016. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/index.htmlAccessed June 1, 2016
- YusufSHawkenSOunpuuSINTERHEART Study InvestigatorsObesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control studyLancet200536694971640164916271645
- BrittonKAMassaroJMMurabitoJMKregerBEHoffmannUFoxCSBody fat distribution, incident cardiovascular disease, cancer, and all-cause mortalityJ Am Coll Cardiol2013621092192523850922
- GBD Mortality Causes of Death CollaboratorsGlobal, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013Lancet2015385996311717125530442
- FlegalKMGraubardBIWilliamsonDFGailMHExcess deaths associated with underweight, overweight, and obesityJAMA2005293151861186715840860
- JeeSHSullJWParkJBody-mass index and mortality in Korean men and womenN Engl J Med2006355877978716926276
- RohLBraunJChioleroASwiss National Cohort Study GroupMortality risk associated with underweight: a census-linked cohort of 31,578 individuals with up to 32 years of follow-upBMC Public Health20141614371
- BucholzEMKrumholzHAKrumholzHMUnderweight, markers of cachexia, and mortality in acute myocardial infarction: a prospective cohort study of elderly medicare beneficiariesPLoS Med2016134e100199827093615
- GallagherDHeymsfieldSBHeoMJebbSAMurgatroydPRSakamotoYHealthy percentage body fat ranges: an approach for developing guidelines based on body mass indexAm J Clin Nutr200072369470110966886
- McCarthyHDColeTJFryTJebbSAPrenticeAMBody fat reference curves for childrenInt J Obes2006304598602
- Gómez-AmbrosiJSilvaCGalofréJCBody mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposityInt J Obes2012362286294
- JacksonASStanforthPRGagnonJThe effect of sex, age and race on estimating percentage body fat from body mass index: the heritage family studyInt J Obes Relat Metab Disord200226678979612037649
- GallagherDVisserMSepulvedaDPiersonRNHarrisTHeymsfieldSBHow useful is body mass index for comparison of body fatness across age, sex, and ethnic groups?Am J Epidemiol19961432282398561156
- RanasingheCGamagePKatulandaPAndraweeraNThilakarathneSTharangaPRelationship between Body Mass Index (BMI) and body fat percentage, estimated by bioelectrical impedance, in a group of Sri Lankan adults: a cross sectional studyBMC Public Health2013313797
- WhitlockGLewingtonSSherlikerPBody-mass index and cause-specific mortality in 900000 adults: collaborative analyses of 57 prospective studiesLancet200937396691083109619299006
- ZhengWMcLerranDFRollandBAssociation between body-mass index and risk of death in more than 1 million AsiansN Engl J Med2011364871972921345101
- TokunagaKMatsuzawaYKotaniKIdeal body weight estimated from the body mass index with the lowest morbidityInt J Obes199115115
- YamashinaATomiyamaHAraiTBrachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular riskHypertens Res200326861562214567500
- ImanishiRSetoSTodaGHigh brachial-ankle pulse wave velocity is an independent predictor of the presence of coronary artery disease in menHypertens Res2004272717815005269
- ShiraiKUtinoJOtsukaKTakataMA novel blood pressure-independent arterial wall stiffness parameter; cardioankle vascular index (CAVI)J Atheroscler Thromb200613210110716733298
- ShiraiKHirutaNSongMCardio-ankle vascular index (CAVI) as a novel indicator of arterial stiffness: theory, evidence and perspectivesJ Atheroscler Thromb2011181192493821628839
- ShiraiKSaikiANagayamaDTatsunoIShimizuKTakahashiMThe role of monitoring arterial stiffness with cardio-ankle vascular index in the control of lifestyle-related diseasesPulse (Basel)20153211813326587461
- MatsuiYKarioKIshikawaJEguchiKHoshideSShimadaKReproducibility of arterial stiffness indices (pulse wave velocity and augmentation index) simultaneously assessed by automated pulse wave analysis and their associated risk factors in essential hypertensive patientsHypertens Res2004271185185715824467
- YambeTYoshizawaMSaijoYBrachio-ankle pulse wave velocity and cardio-ankle vascular index (CAVI)Biomed Pharmacother200458suppl 1959814992790
- KubozonoTMiyataMUeyamaKClinical significance and reproducibility of new arterial distensibility indexCirc J2007711899417186984
- NakamuraKTomaruTYamamuraSMiyashitaYShiraiKNoikeHCardio-ankle vascular index is a candidate predictor of coronary atherosclerosisCirc J200872459860418362432
- NoikeHNakamuraKSugiyamaYChanges in cardio-ankle vascular index in smoking cessationJ Atheroscler Thromb201017551752520215706
- NakamuraKIidukaTTakahashiMAssociation between cardio-ankle vascular index and serum cystatin C levels in patients with cardiovascular risk factorJ Atheroscler Thromb200916437137919672028
- IzuharaMShiojiKKadotaYRelationship of cardiovascular index to carotid and coronary arteriosclerosisCirc J200872111762176718802315
- MiyoshiTDoiMHirohataSCardio-ankle vascular index is independently associated with the severity of coronary atherosclerosis and left ventricular function in patients with ischemic heart diseaseJ Atheroscler Thromb201017324925820103976
- HorinakaSYabeAYagiHComparison of atherosclerotic indicators between cardio ankle vascular index and brachial ankle pulse wave velocityAngiology200960446847619015165
- YingchoncharoenTLimpijankitTJongjirasiriSLaothamatasJYamwongSSritaraPArterial stiffness contributes to coronary artery disease risk prediction beyond the traditional risk score (RAMA-EGAT score)Heart Asia201241778223585778
- SuzukiJKurosuTKonTTomaruTImpact of cardiovascular risk factors on progression of arteriosclerosis in younger patients: evaluation by carotid duplex ultrasonography and cardio-ankle vascular index (CAVI)J Atheroscler Thromb201421655456224521982
- SatoYNagayamaDSaikiACardio-ankle vascular index is independently associated with future cardiovascular events in outpatients with metabolic disordersJ Atheroscler Thromb201623559660526632164
- Satoh-AsaharaNKotaniKYamakageHJapan Obesity and Metabolic Syndrome Study (JOMS) GroupCardio-ankle vascular index predicts for the incidence of cardiovascular events in obese patients: a multicenter prospective cohort study (Japan Obesity and Metabolic Syndrome Study: JOMS)Atherosclerosis2015242246146826295798
- SatohNShimatsuAKatoYEvaluation of the cardio-ankle vascular index, a new indicator of arterial stiffness independent of blood pressure, in obesity and metabolic syndromeHypertens Res200831101921193019015600
- Examination Committee of Criteria for ‘Obesity Disease’ in Japan, Japan Society for the Study of ObesityNew criteria for ‘obesity disease’ in JapanCirc J2002661198799212419927
- The Committee of Japan Diabetes Society on the Diagnostic Criteria of Diabetes MellitusSeinoYNanjoKReport of the Committee on the classification and diagnostic criteria of diabetes mellitusJ Diabetes Soc201053450467
- GenuthSAlbertiKGBennettPExpert Committee on the Diagnosis and Classification of Diabetes MellitusFollow-up report on the diagnosis of diabetes mellitusDiabetes Care2003263160316714578255
- CarreteroOAOparilSEssential hypertension. Part I: definition and etiologyCirculation2000101332933510645931
- Martínez-MartínezEMianaMJurado-LópezRThe potential role of leptin in the vascular remodeling associated with obesityInt J Obes (Lond)201438121565157224583853
- NagayamaDEndoKOhiraMEffects of body weight reduction on cardio-ankle vascular index (CAVI)Obes Res Clin Pract201372139145
- JiaGSowersJREndothelial dysfunction potentially interacts with impaired glucose metabolism to increase cardiovascular riskHypertension20146461192119325225204
- LurbeETorroIGarcia-VicentCAlvarezJFernández-FornosoJARedonJBlood pressure and obesity exert independent influences on pulse wave velocity in youthHypertension201260255055522733475
- DangardtFOsikaWVolkmannRGanLMFribergPObese children show increased intimal wall thickness and decreased pulse wave velocityClin Physiol Funct Imaging200828528729318476996
- CharakidaMJonesAFalaschettiEChildhood obesity and vascular phenotypes: a population studyJ Am Coll Cardiol201260252643265023177297
- Sutton-TyrrellKNewmanASimonsickEMAortic stiffness is associated with visceral adiposity in older adults enrolled in the study of health, aging, and body compositionHypertension200138342943311566917
- WildmanRPMackeyRHBostomAThompsonTSutton-TyrrellKMeasures of obesity are associated with vascular stiffness in young and older adultsHypertension200342446847312953016
- RiderOJTayalUFrancisJMThe effect of obesity and weight loss on aortic pulse wave velocity as assessed by magnetic resonance imagingObesity (Silver Spring)201018122311231620360756
- ZebekakisPENawrotTThijsLObesity is associated with increased arterial stiffness from adolescence until old ageJ Hypertens200523101839184616148607
- MorseSAGulatiRReisinEThe obesity paradox and cardiovascular diseaseCurr Hypertens Rep201012212012620424935
- CicoiraMMaggioniAPLatiniRBody mass index, prognosis, and mode of death in chronic heart failure: results from the Valsartan Heart Failure TrialEur J Heart Fail20069439740217166768
- FonarowGCSrikanthanPCostanzoMRCintronGBLopatinMADHERE Scientific Advisory Committee and InvestigatorsAn obesity paradox in acute heart failure: analysis of body mass index and inhospital mortality for 108,927 patients in the Acute Decompensated Heart Failure National RegistryAm Heart J200715317481
- WuAHEagleKAMontgomeryDGKline-RogersEHuYCAaronsonKDRelation of body mass index to mortality after development of heart failure due to acute coronary syndromeAm J Cardiol2009103121736174019539085
- BlüherMThe distinction of metabolically ‘healthy’ from ‘unhealthy’ obese individualsCurr Opin Lipidol2010211384319915462
- LavieCJMilaniRVVenturaHOObesity and cardiovascular disease: risk factor, paradox, and impact of weight lossJ Am Coll Cardiol200953211925193219460605
- AnkerSNegassaACoatsAJPrognostic importance of weight loss in chronic heart failure and the effect of treatment with angiotensin-converting enzyme inhibitors: an observational studyLancet200336193631077108312672310
- Kalantar-ZadehKBlockGHorwichTFonarowGCReverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failureJ Am Coll Cardiol20044381439144415093881
- ShibaTTakahashiMYoshidaITaniguchiHMatsumotoTHoriYArteriosclerotic changes after intravitreal injections of anti-vascular endothelial growth factor drugs in patients with exudative age-related macular degenerationOphthalmologica2016235422523227082736
- SaikiAOlssonMJernåsMTenomodulin is highly expressed in adipose tissue, increased in obesity, and down-regulated during diet-induced weight lossJ Clin Endocrinol Metab200994103987399419602561
- Senol-CosarOFlachRJDiStefanoMTenomodulin promotes human adipocyte differentiation and beneficial visceral adipose tissue expansionNat Commun201616710686
- NagayamaDSaikiAEndoKImprovement of cardio-ankle vascular index by glimepiride in type 2 diabetic patientsInt J Clin Pract201064131796180120946343
- NagayamaDOhiraMSaikiAShiraiKTatsunoISarpogrelate hydrochloride decreases cardio-ankle vascular index accompanied by increased serum lipoprotein lipase mass in type 2 diabetic patientsInt Heart J201455433734124898600
- OhiraMYamaguchiTSaikiAPioglitazone improves the cardio-ankle vascular index in patients with type 2 diabetes mellitus treated with metforminDiabetes Metab Syndr Obes2014177313319
- PeregDLishnerMBevacizumab treatment for cancer patients with cardiovascular disease: a double edged sword?Eur Heart J200829192325232618762551
- KramerCKZinmanBRetnakaranRAre metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysisAnn Intern Med20131591175876924297192
- KimHJNamJSParkJSUsefulness of brachial-ankle pulse wave velocity as a predictive marker of multiple coronary artery occlusive disease in Korean type 2 diabetes patientsDiabetes Res Clin Pract2009851303419398141
- SugawaraJHayashiKYokoiTBrachial-ankle pulse wave velocity: an index of central arterial stiffness?J Hum Hypertens200519540140615729378
- WenWLuoRTangXAge related progression of arterial stiffness and its elevated positive association with blood pressure in healthy peopleAtherosclerosis2015238114715225485738
- KuoCFSeeLCLuoSFGout: an independent risk factor for all-cause and cardiovascular mortalityRheumatology (Oxford)201049114114619933595
