Abstract
Purpose
This systematic review aims to evaluate the published literature regarding totally laparoscopic aortobifemoral bypass (LABF) surgery in the treatment of aortoiliac occlusive disease (AIOD) or abdominal aortic aneurysms (AAA), compared with open aortobifemoral bypass surgery.
Materials and methods
A systematic review of the medical literature between 1990 and 2016 was performed, searching the medical databases Cochrane Library, OVID Medline, Embase and PubMed. Studies concerning totally LABF with or without control group and containing more than 10 patients were included in the analysis. Operative and aortic cross-clamping times, blood loss, rate of conversion to open surgery, mortality and morbidity within the first 30 postoperative days, hospital stay and primary and secondary patency of the graft were extracted and compared with open surgery when possible.
Results
Sixty-six studies were deemed eligible for inclusion in this review, 16 of them matched the inclusion criteria for quantitative synthesis. The patient material consisted of 588 patients undergoing totally LABF, 22 due to AAA, and the remaining 566 for AIOD. Five comparative studies regarding AIOD compared 211 totally LABF procedures with 246 open procedures. Only one study concerning AAA was eligible for inclusion, and this study did not provide a comparison against an open group. The operating and aortic cross-clamping times were shorter in the open group. Conversion rates ranged from 0% to 27%. There was no statistically significant difference in mortality between the two groups (p=0.64). Hospital stays ranged from 4.0 to 12.1 and 5.0 to 12.8 days in the laparoscopic group and open group, respectively. Most of the studies provided low levels of evidence, mainly due to lack of blinding, randomization and correction of bias.
Conclusion
Totally laparoscopic aortoiliac surgery seems to be a feasible technique with unaffected mortality and trend toward benefits in hospital stay and possibly also in complication rates. The literature published this far is sparse and with inconsistent results. More randomized controlled trials are required before this method can be widely implemented.
Introduction
The first laparoscopy-assisted aortobifemoral bypass was performed in 1993.Citation1 Since the performance of the first totally laparoscopic aortobifemoral bypass (LABF) by the same surgeon in 1996,Citation2 there has been a slow adoption of the technique and few new studies have been performed. Today, 20 years later, open surgery is still considered the standard approach for this procedure but has been lately challenged by the increasingly popular endovascular techniques. However, the endovascular approach shows patency results that seem to be inferior and re-interventions are often required.Citation3 Although several studies have shown encouraging results for laparoscopic surgery compared with open surgery,Citation4–Citation6 only one relatively small randomized controlled trial (RCT) has been published to date.Citation5 Oslo University Hospital is now performing a RCT comparing totally LABF to open aortobifemoral bypass (OABF).
Our review considers patients with severe aortoiliac occlusive disease (AIOD) and/or abdominal aortic aneurysm (AAA) in need of aortobifemoral bypass. Rouhani et al reviewed the perioperative outcomes following laparoscopic AAA repair in 2014,Citation7 whereas the last systematic review concerning both AIOD and AAA was published in 2008 by Cau et al.Citation8 The aim of the present study is to evaluate the level of evidence concerning laparoscopic aortobifemoral surgery compared with the open approach.
Materials and methods
Protocol and registration
The review protocol was published at PROSPERO on January 15, 2015, and is publically available, ID number CRD4 2015016012.
Eligibility criteria
This study is a systemic review and a critical appraisal of the published literature from medical databases, from 1990 to 2016. The inclusion and exclusion criteria are given in .
Table 1 Inclusion and exclusion criteria applied in the evaluation of the eligibility of the articles
Information sources and search strategy
Cochrane, PubMed/Medline and Embase were searched using the following keywords/MESH-terms/all fields: Laparoscop*AND surgery AND aort* including different MESH-terms and synonyms combined by the Boolean variable OR. The full search-strategy is included as a Supplementary material.
The complete search was conducted in January 2015, together with information specialist Hilde Iren Flaatten, Medical University Library, University of Oslo. Before completion of the manuscript, we performed a second literature search with the same search strategy in May 2016 to include new publications from the recent year.
Study selection
All articles were evaluated for inclusion by two researchers independently (IH and AHK). In case of disagreement, the two researchers discussed the publication based on the inclusion/exclusion criteria previously described. The articles found were at first screened based on title, followed by an assessment of the abstracts of the non-excluded studies. Finally, the full texts of the remaining publications were reviewed, and articles matching all the inclusion criteria were selected for data extraction. This process was repeated for the publications added after the final literature search was performed.
Data collection and data items
Data were abstracted by one author (IH), and two authors reviewed the final results (IH, AHK). The authors of the different publications were not contacted for additional information regarding methods or results.
We had further exclusion criteria concerning extraction of data from the different articles. As there are few comparative studies published to date, articles lacking a control group were included in the quantitative synthesis. Data were not obtained from studies that included <10 patients. Publications presenting clinical research without original patient data were not included in the quantitative analysis; hence, all systematic reviews were excluded from –. In cases of data published several times, only the latest or largest patient series were considered. This may apply for double publications of the same results, early and mid-time results or subpopulations. All studies containing non-verified double publication of data were included.
Table 2 Aortoiliac occlusive disease
Table 4 Summary of findings table and grading the level of evidence of the results from the comparative studiesTable Footnotea
We assessed differences in mortality, morbidity, and complications (adverse effects and adverse events [AEs], including but not restricted to, pneumonia, heart attack, paralytic ileus, sepsis, renal failure, cerebrovascular events, bleeding, infection, seroma, major vascular and ischemic events) perioperatively and the first 30 days postoperatively, between those undergoing totally LABF versus OABF. Technical outcomes included operating time, aortic cross-clamping time, blood loss, and conversion to open or hand-assisted laparoscopic surgery (HALS). Postoperative outcomes included length of hospital stay and patency rates. Outcome measures of eligible studies were extracted, tabulated, and then analyzed cumulatively using a descriptive statistical approach.
Risk of bias
All articles included in the data abstraction were evaluated using the “Risk of bias tool” and the “Quality Assessment tool for Quantitative Studies”, recommended by the Cochrane Institute. For all major outcomes, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) assessment tool was used to grade the level of evidence and describe our confidence in the result.
Statistics
Results from studies with prospective or retrospective patient series are presented as comparative tables to assess the safety of the procedure. We used Microsoft Office Excel 2010© (Microsoft, Redmond Campus, Redmond, Washington, USA) to create the tables. As the data did not allow for a meta- analysis to be performed, the results are narratively reported in the text illustrated with tables. Comparisons between the two treatment groups were performed using the Mann–Whitney U-test for continuous variables and Fisher’s exact test for categorical variables, if comparison was possible.
Results
Study selection
The initial search yielded 983 articles from the different databases. One hundred and ten full-text articles were assessed for eligibility after removal of the studies excluded based on title and abstract, together with duplicates. This resulted in 62 publications matching our inclusion/exclusion criteria, 11 of them concerning robotic surgery.
Our final search, performed on May 13, 2016, resulted in 101 additional articles published over the last year. Four of them met the inclusion criteria and were added to the review, resulting in a total of 66 articles included at last. Due to further exclusion criteria, 50 studies were left out from the quantitative analysis, including six systematic reviews,Citation7–Citation12 25 studies involving <10 patientsCitation13–Citation37 and 19 articles either mixing the results from patients suffering from AIOD and AAA, or not separating patient groups receiving tube grafts and aortounifemoral bypass from the patients receiving aortobifemoral bypass.Citation38–Citation56 Hence, 16 articles were deemed eligible for inclusion in and , see for details concerning the systematic literature search process for this study.
Figure 1 Flow chart of systematic search for literature and inclusion regarding laparoscopic aortobifemoral bypass surgery compared with open aortobifemoral bypass.
Abbreviation: RCT, randomized controlled trial.
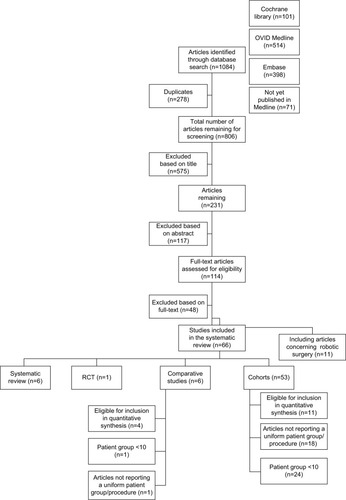
Table 3A Aortoiliac occlusive disease – operative data of included studies, LABF compared with OABF
An unsystematic search performed after the final search made us aware of two more studies. One regarded the long-term results of totally LABF,Citation6 whereas the other study by Krog et alCitation57 concerned the acute phase response after laparoscopic versus OABF surgery. They were not systematically reviewed and hence left out from the analysis.
Study characteristics
This systematic review comprises 66 articles; six systematic reviews, one RCT, six comparative studies, and 53 cohort studies. Finally, 16 studies were deemed eligible for inclusion in the quantitative synthesis, two of them concerning robotic surgeryCitation58,Citation59 and one AAA surgery.Citation60
The publication years ranged from 1997 to 2016. The last addition was a prospective comparative cohort study using propensity score matching in order to diminish bias.Citation56 The sample size ranged from 11Citation61 to 139 patientsCitation62 in the intervention group, the equivalent numbers for the open control group were 14Citation5 to 156Citation4 patients. Most patients were classified as C or D according to the Trans-Atlantic Inter-Society Consensus (TASC) classification,Citation63 with two publications also including TASC B lesions.Citation59,Citation64 Seven articles did not report the TASC classification of the included patients.Citation61,Citation65–Citation70
Peri- and postoperative outcomes
A total of 588 patients underwent totally LABF surgery, 566 for AIOD and 22 due to AAA. Of the 566 patients undergoing LABF surgery for AIOD, 211 of them were included in the five comparative studies and compared with 246 open procedures for AIOD that served as the control group. The different outcomes after LABF surgery for AIOD are reported in and .
Due to inconsistency in the use of mean and median between the publications, the results from the studies are reported individually in and . No summary or combining the results was possible, making the planned meta-analysis inappropriate.
Laparoscopic surgery due to AIOD without control group
Overall, the operating time ranged from 240Citation68 to 376 minutesCitation65 in the 10 cohorts concerning AIOD,Citation58,Citation59,Citation61,Citation62,Citation64–Citation68,Citation71 with aortic cross-clamping time ranging from 59Citation71 to 121 minutes ().Citation65 The perioperative blood loss ranged from 497Citation64 to 1150Citation59 mL. Between 5%Citation64 and 27%Citation61 of the procedures resulted in conversion to open surgery or HALS. The overall mortality in this group was low; a total of six patients died (1.7%). The study by Barbera et al did not report 30-day mortality.Citation61 The morbidity range was quite consistent between the studies, ranging from 16% to 18%. Three studies reported slightly higher rates of 32%,Citation62 33%Citation65 and 23.8%.Citation68 Length of hospital stay was reported by eight studiesCitation59,Citation61,Citation64–Citation68,Citation71 and ranged from 5Citation64 to 10.1Citation61 days. In terms of patency, the different studies demonstrated large variation in follow-up times. Consequently, this outcome was not included in .
Comparative studies concerning AIOD
Further information is included in . Five of the studies were comparative in nature,Citation4,Citation5,Citation69–Citation72 including one RCT.Citation5 In the laparoscopic group, the operating time ranged from a mean of 231 minutesCitation70 to a median of 273 minutes,Citation5 and the aortic cross-clamping time stretched from a median of 48 minutesCitation5 to a median of 89.5 minutes.Citation69 Both mean/median operating and clamping times were shorter for all the open procedures. Three publications found the difference in operating and cross-clamping time between the laparoscopic and open group to be statistically significant.Citation4,Citation70–Citation72 Two studies did not report p-values.Citation5,Citation69
A median blood loss of 400 mLCitation72 was reported as the lowest for the laparoscopic group, with a median of 725 mLCitation5 being the most substantial amount of hemorrhage occurring. In the open group, the blood loss ranged from 982Citation5 to 1010 mL.Citation4 One study did not report this outcome at all.Citation70 Two studies found the difference between the two groups to be statistically significant,Citation4,Citation72 two did not report p-values,Citation69,Citation70 and in one paper, the difference did not reach statistical significance.Citation5
Numbers regarding conversion rate, mortality, morbidity and length of hospital stay are reported in . The conversion rate in the laparoscopic group ranged from 2%Citation70 to 22%.Citation4 One research group was able to perform all the procedures without need for conversion.Citation5 However, this publication presented the smallest patient group, with only 14 patients in the laparoscopic group.
Table 3B Aortoiliac occlusive disease – postoperative outcomes of included studies, LABF compared with OABF
Regarding mortality, three studies in the laparoscopic groupCitation4,Citation5,Citation70 and three in the open groupCitation5,Citation69,Citation70 reported a mortality rate of zero. None of the findings were significant. In contrast, significant differences in mortality between the two groups were obtained by Kazmi et al,Citation72 reporting a p-value of 0.005 in favor of less mortality in the laparoscopic group. However, the latter study reported the total mortality at the end of the study, and not after 30 days.
We calculated the difference in mortality between the open and laparoscopic groups (). We found no significant differences in mortality between the two groups (p=0.64). For the reasons pointed out above, the study by Kazmi et alCitation72 could not be included in this calculation.
The morbidity rate displayed a wide range in both groups. One study found this difference to be statistically significant, with higher morbidity in the open group.Citation4
The shortest length of hospital stay was a median of 4 days in the laparoscopic group and 5 days following open surgery, both outcomes originating from the same study.Citation69 The longest duration of hospital stay after surgery was a mean of 12.1 days in the laparoscopic group and 12.8 days in the open group.Citation4 This difference was found to be statistically significant in all studies. One study did not report p-value for this outcome.Citation69
Not all publications described patency rates, and the studies displayed great diversity in follow-up time and the patency definition. Hence, this was left out from and .
AAA repair
Only one study concerning AAA surgery was included in the quantitative synthesisCitation60 and included 22 patients. All patients underwent laparoscopic surgery, and the study did not include a comparison with any open procedures. The rest of the studies concerning AAA were excluded from the quantitative synthesis as a consequence of either small patient series or because the results were reported together for AAA and AIOD. Originating from one study, these outcomes are not reported in –. Edoga et alCitation60 reported an operating time of 391 minutes and a clamping time of 146 minutes. Blood loss was not an outcome. Two of the 22 procedures (9%) were converted to open surgery, both of them due to difficulty in exposure of the aorta. Two patients died from myocardial infarction and multiorgan failure, respectively. They were both high-risk patients enrolled early in the trial before the introduction of a global risk assessment scoring system. Nine patients (41%) developed perioperative complications, most of them suffering from transient postoperative ileus. The average length of hospital stay was 6.2 days.
Methodological quality
Of the 16 studies included in the quantitative synthesis, only one of them was randomized.Citation5 One publication attempted to correct for bias, making use of a propensity score matching system.Citation73 As this article reported the results together for aortobifemoral bypass and other procedures applying tube graft, it was not eligible for inclusion in the quantitative analysis.
After evaluating the quality of the individual articles using Risk of bias tool recommended by the Cochrane Institute, only the RCT was rated as “strong”,Citation5 two as “moderate”Citation65,Citation68 and the rest as “weak”. The systematic reviews were evaluated similarly and also displayed variable quality. Three studies were assessed to be of low methodological quality,Citation8,Citation9,Citation11 two of moderate qualityCitation7,Citation10 and one of high quality, with a satisfactory methodological chapter.Citation12
The GRADE approach was applied to assess our confidence in the results (). The quality of evidence was low for all outcomes, largely due to study design and weak effect estimates.
Discussion
In this review, we have seen that totally LABF for AIOD seems to achieve satisfactory results compared with OABF, with shorter hospital stay, longer operating and clamping times and perhaps less peri- and postoperative complications in the laparoscopic group. The overall research conducted so far provides a low level of evidence and is clearly focused on AIOD surgery. Hence, no conclusions could be drawn regarding AAA surgery.
An international consensus for the management of peripheral disease was updated in 2007,Citation74 recommending aortobifemoral bypass as the procedure of choice for most patients with severe (TASC C or D) AIOD. Despite several studies demonstrating the feasibility of totally laparoscopic aortic surgery,Citation38,Citation42,Citation47,Citation55,Citation61,Citation65,Citation68 the widespread use of this technique has remained relatively low. A rapid development of endovascular methods has led to few centers adopting the procedure.
This review demonstrates that the quality of the research and evidence is low, with great diversity between the studies and their way of reporting results. Heterogeneity of the studies and selection of the patients made comparison difficult. Nevertheless, it seems quite evident that laparoscopic surgery for AIOD is related to longer operating and clamping times, with three of the comparative studies showing p-values <0.05 for this result. Similarly, significant differences were obtained by four studies in favor of shorter hospital stay in the laparoscopic group, leading us to believe that laparoscopic surgery might result in a shorter postoperative course. This may have an impact on decision making and health economy.Citation70,Citation75
The results regarding intraoperative blood loss and postoperative morbidity were less conclusive, but there is a tendency toward less postoperative complications in the laparoscopic group. Morbidity was defined differently by the research groups and made comparison unfortunate. However, significantly shorter hospital stay in the laparoscopic group can be a result of fewer intra- and postoperative complications, and possibly less intraoperative blood loss in the laparoscopic group, as both these outcomes are indirect measures of intraoperative problems encountered.Citation75–Citation77 The two studies that did report p-values for differences in morbidityCitation4,Citation72 had the largest patient groups of all the studies. Kazmi et alCitation72 reported results over a period of 6 years and included a thorough analysis of the complications faced. From these results, it seems possible that less morbidity comes at the expense of longer operating and clamping times.
Overall, most studies provide evidence that laparoscopic surgery for AIOD is comparable with open surgery in terms of survival and safety of the procedure. This is in great contrast to the only study reporting negative results so far. The latest study by Ricco et alCitation73 suggests that the laparoscopic approach significantly increases the risk of AE compared with open surgery. However, the study combines the results of aortobifemoral bypass surgery for AAA and AIOD and hence was not included in the quantitative synthesis. Combined results from the two patient groups must be interpreted cautiously. In the study by Edoga at al,Citation60 the operating and clamping time was notably longer than all the laparoscopic surgeries performed for AIOD. A complication rate of 41% was reported. Conclusions cannot be drawn on the basis of one study alone. Nevertheless, it seems that laparoscopic surgery for AAA involves longer operating and clamping times,Citation8,Citation78 thus, perhaps, resulting in more complications than surgery performed for AIOD. Similar observations have been made after comparing open surgery for AAA and AIOD, with increased risk of death in the AAA group.Citation79
Ricco’s cohort studyCitation73 attempts to reduce the recruitment bias by using propensity score matching, a method originally introduced by Rosenbaum and Rubin.Citation80 This approach is meant to limit selection bias by predicting the likelihood that a patient with given characteristics will receive a specific treatment. In this particular study, 50 patients from the laparoscopy group were matched with 50 patients from the laparotomy group and showed similar scores. Both the propensity score matched group and the overall series found significantly higher risk of AE after undergoing LABF compared with OABF. Although this study could not be included in our final analysis, it still brings a few new and noteworthy points into the discussion. The publication is interesting for more than one reason.
On the one hand, higher probability for AE in the laparoscopic group has not previously been reported. However, the study has composite endpoints, grouping together different AEs such as death, postoperative hemorrhage, myocardial infarction, stroke, postoperative respiratory failure and problems related to the prosthesis and anastomosis. A similar method was applied by Kazmi et al.Citation72 Employing composite endpoints in the analysis is a way of generating significant results in smaller patient series but may pose interpretation difficulties, as an increased risk for the individual events may be related to each other and impose very different clinical importance. In contrast to Ricco’s publication,Citation73 Kazmi et alCitation72 found significantly less morbidity in the laparoscopic group even by means of a composite endpoint, an outcome more similar to previous publications.
On the other hand, propensity score matching has been criticized and errors are often made when applying this method in statistical analysis.Citation81 Without knowing the full implication this might have, it is worth mentioning that medical complications were balanced out between LABF and OABF in this particular study. This might imply that the risk of AE following LABF is closely linked to surgical technique, particularly completion of the anastomosis. The complexity of the procedure is indicated by a considerable learning curve,Citation68 which is overcome after ~25–30 procedures.Citation62 Lately, robots have been used in an attempt to shorten the operating time by assisting in the creation of the anastomosis. So far, it seems to be a viable technique,Citation50 which may enhance the surgical procedure.Citation9,Citation59 There is a distinct need for further research concerning robotic laparoscopic surgery.
Limitations
This systematic review has several limitations, mostly due to poor quality of the individual studies and great diversity in terms of procedure type and reporting manners. A meta-analysis could not be performed and the results could not be summarized, as there was no uniformity in the way they were described. Few publications reported standard deviations as part of their analysis, and even less studies made use of p-values when comparing with other groups. Consequently, range became the most objective measurement of reporting the results. Unfortunately, this is substantially less reliable than performing a meta-analysis. Some of the publications seem to report repeated patient material. Nevertheless, all the mentioned studies were included, as this assumption could not be verified. What impact this has on the results can hardly be quantified.
In addition to the problems encountered above, numerous studies reported diverse patient and procedure groups, and the larger part of the studies were excluded from the quantitative synthesis for this reason. These studies carry a significant risk of bias, assuming operating and clamping times are considerably longer for AAA than AIOD,Citation8,Citation78 and vary between the procedure types. Most of Stadler’s publicationsCitation45,Citation46,Citation48,Citation51,Citation52 were affected by this decision and could not be included despite a large patient material in most of the studies. This was one of the main reasons why most of the studies concerning AAA surgery could not be included.
Most studies were observational, and the description of the characteristics of the consecutive patients in the cohorts was inadequate in most of them. We must assume a considerable selection bias, as none of the studies describe attempts to correct confounders existing in the different groups. The only randomized study was closed prematurely at 28 patients,Citation5 when an ethical committee eventually found it unethical to randomize patients originally referred for laparoscopic surgery. As a consequence of weak study designs and low methodological quality resulting from the limitations described above, the research conducted this far provides evidence of low quality. This is emphasized by the quality assessment of both the individual studies (Risk of bias tool) and the outcome results from all the studies grouped together (GRADE). When assessing the latter, the GRADE approach was applied. Although this grading system is widely acceptedCitation82,Citation83 and recommended by the Cochrane Institute, the weak effect estimates and reporting manners provided by all the studies included in this review made full utilization of the method difficult.
Conclusion
The laparoscopic aortoiliac surgery is still sparsely employed despite promising results for AIOD. No research comparing totally laparoscopic surgery for AAA with open surgery, without combining results from AIOD, has been conducted to date. It seems reasonable to claim that LABF can be performed safely, with shorter hospital stay, less intraoperative hemorrhage, and possibly less peri- and postoperative complications and morbidity compared to open surgery. Open surgery delivers shorter operating and aortic cross-clamping times. The mortality rate appears unaffected by surgical approach. However, few centers and surgeons are performing this procedure. The published literature to date is of weak quality and the level of evidence is low. There is a need for further research.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
All expenses for this review were covered fully by the University of Oslo. We extend a very special thanks to late Prof Jørgen J Jørgensen for all the inspiration, guidance and support. We also thank medical librarian Hilde Iren Flaatten at the University of Oslo for her contribution with the literature search and Dr. Truls Erik B Johansen at the Department of Urology, Oslo University Hospital, for helpful advice and critical revision.
Supplementary material
Complete search strategy
Disclosure
The authors report no conflicts of interest in this work.
References
- DionYMKatkhoudaNRouleauCAucoinALaparoscopy-assisted aortobifemoral bypassSurg Laparosc Endosc1993354254298261276
- DionYMGraciaCRDemalsyJCLaparoscopic aortic surgeryJ Vasc Surg1996233539
- TimaranCHPraultTLStevensSLFreemanMBGoldmanMHIliac artery stenting versus surgical reconstruction for TASC (TransAtlantic Inter-Society Consensus) type B and type C iliac lesionsJ Vasc Surg200338227227812891108
- BrulsSQuaniersJTrommePLavigneJPVan DammeHDefraigneJOComparison of laparoscopic and open aortobifemoral bypass in the treatment of aortoiliac disease. Results of a contemporary series (2003–2009)Acta Chir Belg20121121515822442910
- TiekJRemyPSabbeTLaparoscopic versus open approach for aortobifemoral bypass for severe aortoiliac occlusive disease – a multicentre randomised controlled trialEur J Vasc Endovasc Surg201243671171522386382
- LecotFSabbeTHouthoofdSDaenensKFourneauILong-term results of totally laparoscopic aortobifemoral bypassEur J Vasc Endovasc Surg201652558158727346447
- RouhaniMJThaparAMaruthappuMMunsterABDaviesAHShalhoubJSystematic review of perioperative outcomes following laparoscopic abdominal aortic aneurysm repairVascular201523552555325425618
- CauJRiccoJBCorpatauxJMLaparoscopic aortic surgery: techniques and resultsJ Vasc Surg2008486 Suppl37S44S discussion 45S18945578
- AntoniouGARigaCVMayerEKCheshireNJBicknellCDClinical applications of robotic technology in vascular and endovascular surgeryJ Vasc Surg201153249349920801611
- EconomopoulosKPMartinouEHakimianSAn overview of laparoscopic techniques in abdominal aortic aneurysm repairJ Vasc Surg201358251252023890444
- LinJCThe role of robotic surgical system in the management of vascular diseaseAnn Vasc Surg201327797698323849652
- NioDDiksJBemelmanWAWisselinkWLegemateDALaparoscopic vascular surgery: a systematic reviewEur J Vasc Endovasc Surg200733326327117127084
- DionYMGraciaCRA new technique for laparoscopic aortobifemoral grafting in occlusive aortoiliac diseaseJ Vasc Surg19972646856929357472
- SaidSMallJPeterFMullerJMLaparoscopic aortofemoral bypass grafting: human cadaveric and initial clinical experiencesJ Vasc Surg199929463964810194491
- AlimiYSHartungOOrsoniPJuhanCAbdominal aortic laparoscopic surgery: retroperitoneal or transperitoneal approach?Eur J Vasc Endovasc Surg2000191212610706830
- AlimiYSHartungOValerioNJuhanCLaparoscopic aortoiliac surgery for aneurysm and occlusive disease: when should a minilaparotomy be performed?J Vasc Surg200133346947511241114
- WisselinkWCuestaMAGraciaCRauwerdaJARobot-assisted laparoscopic aortobifemoral bypass for aortoiliac occlusive disease: a report of two casesJ Vasc Surg20023651079108212422124
- DionYMThaveauFFearnSJCurrent modifications to totally laparoscopic “apron technique”J Vasc Surg200338240340612891131
- CoggiaMJaverliatIDi CentaITotal laparoscopic infrarenal aortic aneurysm repair: preliminary resultsJ Vasc Surg200440344845415337872
- DesgrangesPBourriezAJaverliatIRobotically assisted aortofemoral bypass grafting: lessons learned from our initial experienceEur J Vasc Endovasc Surg200427550751115079774
- MercierOCoggiaMJaverliatIDi CentaIColacchioGGoeau-BrissonniereOTotal laparoscopic repeat aortic surgeryJ Vasc Surg200440482282515472615
- CoggiaMDi CentaIJaverliatIAlfonsiPKitzisMGoeau- BrissonniereOATotal laparoscopic abdominal aortic aneurysms repairJ Cardiovasc Surg (Torino)2005464407414
- NioDDiksJLinsenMARobot-assisted laparoscopic aortobifemoral bypass for aortoiliac occlusive disease: early clinical experienceEur J Vasc Endovasc Surg200529658659015878533
- RuurdaJPDraaismaWAvan HillegersbergRRobot-assisted endoscopic surgery: a four-year single-center experienceDig Surg200522531332016192731
- Di CentaICoggiaMJaverliatITotal laparoscopic suprarenal aortic coral reef removalJ Vasc Surg200644119419716828444
- KazmiSSSundhagenJOFlorenesTLKroeseAJJorgensenJJLaparoscopic aortic surgeryTidsskr Nor Laegeforen2007127111518152017551557
- CoggiaMCerceauPDiCentaIJaverliatIColacchioGGoeau- BrissonniereOTotal laparoscopic juxtarenal abdominal aortic aneurysm repairJ Vasc Surg2008481374218486423
- DebingEDe BrabandereKVanhulleAVan Den BrandePFrom retro-peritoneoscopic lumbar sympathectomy to total laparoscopic abdominal aorta surgery: how to learnJ Cardiovasc Surg (Torino)2008494511517
- Di CentaICoggiaMCochennecFAlfonsiPJaverliatIGoeau-BrissonniereOLaparoscopic abdominal aortic aneurysm repair in octogenariansJ Vasc Surg20094951135113919307083
- Di CentaICoggiaMCochennecFJaverliatIAlfonsiPGoeau-BrissonniereOTotal laparoscopic repair of abdominal aortic aneurysm with short proximal necksAnn Vasc Surg2009231434819135910
- LeeTKimHHHanHSMinSKHaJKimSJEarly experiences of laparoscopic aortofemoral bypass in Korea-report from a single centerAnn Vasc Dis200921343923555354
- LinJCKaulSARogersCGSuccessful total robotic-assisted aortobifemoral bypass for treatment of complicated aortoiliac occlusive diseaseVasc Endovascular Surg201145434034421527465
- FukuiSAlbertiVMalliosASouryPGigouFEarly and mid-term results of total laparoscopic bypass for aortoiliac occlusive lesionsJ Cardiovasc Surg (Torino)2012532235239
- LinJCKaulSABhandariAPetersonELPeabodyJOMenonMRobotic-assisted aortic surgery with and without minilaparotomy for complicated occlusive disease and aneurysmJ Vasc Surg2012551162221917403
- GuoLRGuYQQiLXTotally laparoscopic bypass surgery for aortoiliac occlusive disease in ChinaChin Med J2013126163069307223981614
- QiLGuYGuoLAnalysis of operation-related complications of totally laparoscopic aortoiliac surgeryChin Med J201412771218122124709169
- HowardAQBennettPCAhmadIChoksySAMackenzieSIBack-houseCMIntroduction of laparoscopic abdominal aortic aneurysm repairBr J Surg2015102436837425689292
- CoggiaMJaverliatIDi CentaITotal laparoscopic bypass for aortoiliac occlusive lesions: 93-case experienceJ Vasc Surg200440589990615557903
- KolvenbachRSchwierzEWasilljewSMiloudAPuerschelAPinterLTotal laparoscopically and robotically assisted aortic aneurysm surgery: a critical evaluationJ Vasc Surg200439477177615071439
- CoggiaMJaverliatIDi CentaITotal laparoscopic versus conventional abdominal aortic aneurysm repair: a case-control studyJ Vasc Surg2005425906910 discussion 91116275445
- LinJCKolvenbachRSchwierzEWassiljewSTotal laparoscopic aortofemoral bypass as a routine procedure for the treatment of aortoiliac occlusive diseaseVascular2005132808315996361
- CauJRiccoJBMarchandCTotal laparoscopic aortic repair for occlusive and aneurysmal disease: first 95 casesEur J Vasc Endovasc Surg200631656757416414294
- DoonerJLeeSGriswoldWKuechlerPLaparoscopic aortic reconstruction: early experienceAm J Surg2006191569169516647362
- KolvenbachRTotal laparoscopic aortic aneurysm surgeryActa Chir Belg20061061363916612910
- StadlerPMatousPVitasekPSpacekMRobot-assisted aortoiliac reconstruction: a review of 30 casesJ Vasc Surg200644591591917098518
- StadlerPSebestaPVitasekPMatousPEl SammanKA modified technique of transperitoneal direct approach for totally laparoscopic aortoiliac surgeryEur J Vasc Endovasc Surg200632326626916567115
- Di CentaICoggiaMCerceauPTotal laparoscopic aortobifemoral bypass: short- and middle-term resultsAnn Vasc Surg200822222723218346577
- StadlerPDvoracekLVitasekPMatousPIs robotic surgery appropriate for vascular procedures? Report of 100 aortoiliac casesEur J Vasc Endovasc Surg200836440140418722141
- CoscasRCoggiaMDi CentaIJaverliatICochennecFGoeau-BrissonniereOLaparoscopic aortic surgery in obese patientsAnn Vasc Surg200923671772119875006
- StadlerPRole of the robot in totally laparoscopic aortic repair for occlusive and aneurysmal diseaseActa Chir Belg2009109330030519943583
- StadlerPDvoracekLVitasekPMatousPRobotic vascular surgery, 150 casesInt J Med Robot20106439439820652874
- StadlerPDvoracekLVitasekPMatouAiPThe application of robotic surgery in vascular medicineInnovations (Phila)20127424725323123990
- JaverliatICapdevilaCBeauchetADi CentaIGoeau-BrissonniereOCoggiaMResults of laparoscopic surgery for abdominal aortic aneurysms in patients with standard surgical risk and anatomic criteria compatible with EVARAnn Vasc Surg201327441241723406789
- CoscasRMaumiasTCapdevilaCJaverliatIGoeau-BrissonniereOCoggiaMMini-invasive treatment of abdominal aortic aneurysms: current roles of endovascular, laparoscopic, and open techniquesAnn Vasc Surg201428112313124200131
- GhammadKDupuisAAmondLTotal laparoscopic bypass is safe and effective for aortoiliac occlusive diseaseJ Vasc Surg201561369870225720928
- RiccoJBCauJBiancariFOutcome after open and laparoscopic aortic surgery in matched cohorts using propensity score matchingEur J Vasc Endovasc Surg201652217918827102201
- KrogAHSahbaMPettersenEMComparison of the acute-phase response after laparoscopic versus open aortobifemoral bypass surgery: a substudy of a randomized controlled trialVasc Health Risk Manag20161237137827713633
- NovotnyTDvorakMStaffaRThe learning curve of robot-assisted laparoscopic aortofemoral bypass grafting for aortoiliac occlusive diseaseJ Vasc Surg201153241442021093201
- JongkindVDiksJYeungKKCuestaMAWisselinkWMid-term results of robot-assisted laparoscopic surgery for aortoiliac occlusive diseaseVascular20111911721489920
- EdogaJKJamesKVResnikoffMAsgarianKSinghDRomanelliJLaparoscopic aortic aneurysm resectionJ Endovasc Surg1998543353449867324
- BarberaLMummeAMetinSZumtobelVKemenMOperative results and outcome of twenty-four totally laparoscopic vascular procedures for aortoiliac occlusive diseaseJ Vasc Surg19982811361429685140
- FourneauILerutPSabbeTHouthoofdSDaenensKNevelsteenAThe learning curve of totally laparoscopic aortobifemoral bypass for occlusive disease. How many cases and how safe?Eur J Vasc Endovasc Surg200835672372918294873
- NorgrenLHiattWRDormandyJANehlerMRHarrisKAFowkesFGRInter-society consensus for the management of peripheral arterial disease (TASC II)J Vasc Surg2007451 SupplS5S6717223489
- DionYMGriselliFDouvilleYLangisPEarly and mid-term results of totally laparoscopic surgery for aortoiliac disease: lessons learnedSurg Laparosc Endosc Percutan Tech200414632833415599296
- DionYMGraciaCREstakhriMTotally laparoscopic aortobifemoral bypass: a review of 10 patientsSurg Laparosc Endosc1998831651709649037
- DionYMCardonAHartungOGraciaCRLaparoscopic aortoiliac surgery: present status and future perspectivesSurg Technol Int1999820120712451531
- GraciaCRDionYMTechnological advances in laparoscopic aortoocclusive surgerySemin Laparosc Surg19996316417410528066
- RemyPDeprezAFD’HontCLavigneJPMassinHTotal laparoscopic aortobifemoral bypassEur J Vasc Endovasc Surg2005291222715570267
- OlindeAJMcNeilJWSamAHebertSAFrushaJDTotally laparoscopic aortobifemoral bypass: a review of 22 casesJ Vasc Surg2005421273416012448
- RouersAMeurisseNLavigneJPPotential benefits of laparoscopic aortobifemoral bypass surgeryActa Chir Belg2005105661061516438070
- FourneauIMarienIRemyPConversion during laparoscopic aortobifemoral bypass: a failure?Eur J Vasc Endovasc Surg201039223924519892572
- KazmiSSJorgensenJJSundhagenJOA comparative cohort study of totally laparoscopic and open aortobifemoral bypass for the treatment of advanced atherosclerosisVasc Health Risk Manag20151154154726425098
- RiccoJBCauJBiancariFOutcome after open and laparoscopic aortic surgery in matched cohorts using propensity score matchingEur J Vasc Endovasc Surg201652217918827102201
- NorgrenLHiattWRDormandyJANehlerMRHarrisKAFowkesFGInter-society consensus for the management of peripheral arterial disease (TASC II)J Vasc Surg2007331S1S75
- KhanNAQuanHBugarJMLemaireJBBrantRGhaliWAAssociation of postoperative complications with hospital costs and length of stay in a tertiary care centerJ Gen Intern Med200621217718016606377
- BowerWFJinLUnderwoodMJLamYHLaiPBPeri-operative blood transfusion increases length of hospital stay and number of postoperative complications in non-cardiac surgical patientsHong Kong Med J201016211612020354245
- ZandBFrumovitzMJofreMFRisk factors for prolonged hospitalization after gynecologic laparoscopic surgeryGynecol Oncol2012126342843122668880
- de VriesSOHuninkMGResults of aortic bifurcation grafts for aortoiliac occlusive disease: a meta-analysisJ Vasc Surg19972645585699357455
- JaakkolaPHippelainenMOksalaIInfrarenalaortofemoral bypass surgery: risk factors and mortality in 330 patients with abdominal aortic aneurysm or aortoiliac occlusive diseaseAnn Chir Gynaecol199685128358739930
- RosenbaumPRRubinDBThe central role of the propensity score in observational studies for causal effectsBiometrika19837014155
- AustinPCA critical appraisal of propensity-score matching in the medical literature between 1996 and 2003Stat Med200827122037204918038446
- KunzRBurnandBSchunemannHJGrading of Recommendations, Assessment, Development and Evaluation (GRADE) Working GroupDas GRADE-System. Ein internationaler Ansatz zur Vereinheitlichung der Graduierung von Evidenz und Empfehlungen in Leitlinien. [The GRADE System. An international approach to standardize the graduation of evidence and recommendations in guidelines]Internist (Berl)2008496673680 German18461295
- BrozekJLAklEACompalatiEGrading quality of evidence and strength of recommendations in clinical practice guidelines part 3 of 3. The GRADE approach to developing recommendationsAllergy201166558859521241318
