Abstract
Objectives
The aims of this study were to assess the prevalence of diagnosed atrial fibrillation (AF), the drug use in patients with AF in terms of antithrombotic (AT) strategies used and the compliance with treatment, and to describe the characteristics of patients affected by AF in relation to treatment.
Methods
The data collected were provided from databases of general practitioners (GPs) of the Local Health Unit of Bologna in Italy. From January 1, 2009, to December 31, 2012, all subjects aged ≥18 years followed by the 44 GPs enrolled in the study were evaluated, and the subjects with a diagnosis of AF were included in the analysis.
Results
From 2009 to 2012, we identified 1,413 patients with a diagnosis of AF (2.09% of 67,517 patients of the 44 GPs). A total of 1,413 patients with a diagnosis of AF (2.09% of 67,517 patients of the 44 GPs) were enrolled in the study. During the study, 14% of the enrolled patients did not receive any prescription of ATs, 30% and 39.56% were treated only with antiplatelet (AP) agents and oral anticoagulants (OACs), respectively, and 16.28% of the patients received prescriptions for both an OAC and an AP agent; of the patients receiving prescriptions for both, only 4.17% received these therapies at the same time. Among the OAC users, the percentage of patients still on treatment with the index drug during the last 3 months of observation was 76.9%.
Conclusion
Our findings emphasize that in an Italian real-world setting, the burden of AF in general population from a public health point of view underscores the need for improvement in utilization of appropriate ATs in patients with known AF.
Introduction
Atrial fibrillation (AF) is the most common type of cardiac arrhythmia, occurring in 1–2% of the general population worldwide; the prevalence of AF increases steeply with age, from <0.5% at 40–50 years to 5–15% at 80 years.Citation1,Citation2 Men are more often affected than women.Citation3,Citation4 In all, >6 million Europeans suffer from this arrhythmia, and its prevalence is estimated to double in the next 50 years as the population ages.Citation1
AF is often associated with increased rates of death, stroke and other thromboembolic events; hospitalization; and degraded quality of life.Citation5 Because the success of therapy depends on the individual patient’s underlying level of risk, an accurate stratification of patients’ level of risk is needed to select the appropriate therapeutic strategy.Citation6 Current national and international practice guidelines for the optimal management of patients with AF recommend careful consideration of individual factors and baseline comorbidities when choosing the most appropriate antithrombotic (AT) agent.Citation7–Citation9 Consistently, numerous risk stratification schemes have been developed to predict the level of risk profile in patients and to manage patients accordingly.Citation10
Oral anticoagulants (OACs), also called vitamin K antagonists (VKAs), are an effective primary preventive intervention for patients with AF at a moderate and high risk of stroke.Citation1,Citation11 Nevertheless, these agents are associated with a number of limitations, including, when not adequately controlled, a risk of bleeding.
Antiplatelet (AP) agents have been widely used for stroke prophylaxis in patients with AF, particularly in patients with nonvalvular AF who are considered at a low risk of stroke or in patients in whom OAC therapy is contraindicated.Citation5
A number of studies have demonstrated that maintaining the intensity of anticoagulation is crucial to achieving effective stroke prevention and for avoiding bleeding complications.Citation12,Citation13 Some studies have examined OACs utilization in a “real-life” setting through administrative claims databases and have reported that their use is suboptimal.Citation14–Citation16
In view of these findings, AF management represents a considerable cost burden on health care systems, and strategies to improve the entire process of AF care should be suggested based on knowledge obtained from real-world scenarios.
The aims of this retrospective cohort study were to assess the prevalence of AF diagnoses, the drug usage in patients with AF in terms of the AT strategies used and the compliance with treatment and to describe the characteristics of patients affected by AF in relation to treatment.
Methods
Data sources
This study collected data from databases of 44 general practitioners (GPs) of the Local Health Unit (LHU) of Bologna in Italy. The structure of this database has been described in detail elsewhere.Citation17,Citation18
Briefly, the database included different sections as follows: 1) patient data, such as gender and date of birth; 2) prescription records with information on the drugs dispensed by the retail pharmacies in the territory; 3) hospital data, the discharge diagnosis codes classified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM); 4) prescription records for diagnostic tests and 5) the exemptions database, records for exemptions, which includes the exemption code (identifying the disease for which the exemption was granted). All drugs prescribed were classified according to the codes of International Anatomic Therapeutic Chemical (ATC) Classification System. In compliance with privacy laws, the patients’ identification codes were encrypted. The sections were linked by an encrypted unique identification code according to the Italian law for confidentiality data. No identifiers linking individuals to the data were provided to the researchers, and the authors were never involved in collecting the patient data from patients at any point. The anonymous data file was routinely used by the regional health authorities for epidemiological and administrative purposes. Informed consent was not required for using encrypted retrospective information. This study was notified to the local ethics committee of each participating LHU according to the Italian law regarding the conduct of observational analysis, and the ethics committee of LHU approved the study.Citation19
Study population
From January 1, 2009, to December 31, 2012, the patient files of all subjects aged ≥18 years cared by the 44 GPs enrolled in the study were analyzed, and the subjects with a diagnosis of AF (supported by electrocardiographic findings or the diagnosis recorded on a hospital discharge summary) were included in the analysis.
The index date was defined as the date of the first qualifying AF diagnosis, and all patients enrolled were followed for 1 year after the enrollment date. According to their first prescription of ATs during the enrollment period, the patients were stratified into the following four main categories: 1) monotherapy with OACs (warfarin or acenocumarol); 2) monotherapy with APs (acetylsalicylic acid or clopidogrel); 3) prescriptions of both an OAC agent and an AP agent and 4) without therapy.
The CHA2DS2-VASc scoreCitation1 (where points are attributed to the presence of known risk factors: congestive heart failure or left ventricular systolic dysfunction, hypertension history, vascular disease, age ≥75 years, diabetes mellitus, prior stroke/transient ischemic attack [TIA] or thromboembolism and gender category) was calculated, and the patients were stratified in various risk levels; a score of ≥2 indicated a risk for thromboembolism requiring anticoagulation. The scores considered in this study ranged from 0 to 5+. Because the risk of bleeding is also an important concern,Citation9 the HAS-BLED (hypertension, abnormal renal and liver function, stroke, bleeding, labile international normalized ratio [INR], elderly [age >65 years], drugs [other AP agents or nonsteroidal anti-inflammatory drugs {NSAIDs}] or alcohol history) score was calculated to evaluate an individual patient’s risk for bleeding.Citation1 An HAS-BLED score of ≥3 is associated with a high bleeding risk. The HAS-BLED score was categorized as 0 through 5+ in this study. Because in our database information on labile INR and alcohol use was not available for all patients according to a previous analysis,Citation20 we calculated a modified HAS-BLED score with a maximum score of 8 instead of 9. The CHA2DS2-VASc and HAS-BLED scores were calculated only for patients for whom gender data were available.
When available, the number of INR tests in the period after the index date was assessed. The following covariates were assessed for each patient at the index date: 1) demographic variables; 2) risk factors for stroke, such as previous stroke/TIA/hemorrhagic stroke (ICD-9-CM codes: 430–436, 438, 442), valve disease (ICD-9-CM codes: 394, 424.0), diabetes (ICD-9-CM code: 250), peripheral vascular disease (ICD-9-CM codes: 433.1, 440.2, 443.9), hypertension (ICD-9-CM codes: 401–404), heart failure (ICD-9-CM code: 428) and coagulation defects (ICD-9-CM codes: 286, 287); 3) other disease, such as peptic ulcer (ICD-9-CM codes: 531–534); hemorrhage/bleeding (ICD-9-CM codes: 456.0, 531.0, 531.2, 531.4, 531.6, 532.0, 532.2, 532.4, 532.6, 533.0, 533.2, 533.4, 533.6, 534.0, 534.2, 534.6, 569.3, 578.0, 578.9, 596.7, 599.7, 626.5, 626.6, 626.9, 627.0, 627.1, 623.8, 626.2, 784.7, 786.3, 459.0, 719.1, 423.0, 379.2, 852.2); chronic bronchitis (ICD-9-CM code: 491), in particular obstructive chronic bronchitis (ICD-9-CM code: 491.2); asthma (ICD-9-CM code: 493); gastroesophageal reflux (ICD-9-CM code: 530.81); disorders of thyroid gland (ICD-9-CM codes: 240–246); dementia (ICD-9-CM code: 290); other cerebral degenerations (ICD-9-CM code: 331); sleep apnea (ICD-9-CM codes: 780.51, 780.53, 780.57) and bone fractures (ICD-9-CM codes: 805, 806, 808, 820, 824, 812.0–812.5, 813.4, 813.5, 807.0, 807.1); 4) test prescription and resource usage related to AF management, such as cardiologic visits, echocardiograms (ECGs) and ECG with Holter and mechanical heart valves prior to the index date and 5) all prescriptions due to the use of beta blocker (b-blocker) agents (ATC code: C07), statins (ATC code: C10AA), organic nitrates (ATC code: C01DA), antidiabetic drugs (ATC codes: A10A, A10B), anti-inflammatory and anti-rheumatic agents and non-steroids (ATC code: M01A), macrolides (ATC code: J01FA) and proton pump inhibitors (ATC code: A02BC) 6 months before the data index.
Compliance with therapy among OAC users
Persistence to therapy in terms of the percentage of patients still on treatment with the index drug during the last 3 months of observation was also assessed. Patients were excluded if they had a procedure of electrical cardioversion (ICD-9-CM procedure code: 99.6). An interruption of treatment was defined as the absence of prescriptions in the last 3 months of the observation period. This method is validated and has been used in previous studies.Citation21,Citation22
Statistical analysis
Standard descriptive statistical methods were used to analyze the patient’s demographics and clinical status, to evaluate the proportion of treated patients in each drug category and to calculate the cohort of patients still on treatment with the index drug. In cases where data were not issuable for data privacy – results referred to less than four patients, as potentially reconductable to single individuals “Codice in materia di protezione dei dati personali [Code for protection of personal data]”Citation38 – they have been reported as NI (not issuable). Statistical analyses were performed using Stata software version (StataCorp LP, College Station, TX, USA).
Results
From 2009 to 2012, we identified 1,413 patients with a diagnosis of AF (2.09% of 67,517 patients of the 44 GPs). The numbers of patients identified during the 4 years of data screening were 365 and 354 in 2009 and 2010, respectively, and 346 and 348 in 2011 and 2012, respectively; of these patients, 49.9% were males. The frequency of AF increased with age, with a significant majority of cases observed in the elderly population. A total of 934 patients (66.1%) had at least one cardiologic visit in the year prior to the index. During the 6 months before the index date, 33.2% patients had at least one prescription for b-blockers, while 27.3% and 20% patients had at least one prescription for proton pump inhibitors and statins, respectively. The baseline characteristics of the patients, stratified according to the treatment assignment, are described in .
Table 1 Clinical and demographic characteristics stratified by treatment strategy assignment
At the time of the analysis, 559 patients (39.56% of all patients with AF) were treated with OACs, 424 patients (30% of all patients with AF) received AP agents and 200 patients (14% of all patients with AF) were without any prescription for ATs. Prescriptions for both an OAC and AP agent were given to 16.28% of patients; of these patients, only 4.17% were given an OAC plus an AP agent at the same time. The distribution of the study population stratified by treatment strategy assignment 1 year after the index date is shown in .
Table 2 Distribution of the study population stratified by treatment strategy assignment 1 year after the index date
In the entire study population, the most frequent CHA2DS2-VASc scores were 4, 3 and 5+, occurring in 31.6%, 26.1% and 18% of patients, respectively (). The distribution of ATs use according to stroke risk categories is reported in . We evaluated the HAS-BLED score; the results showed that a low proportion of patients had a high and a low HAS-BLED score, with the majority of patients having a moderate bleeding risk score (). The given combinations between the treatment options for each patient and the HAS-BLED scores are summarized in . Data regarding INR tests were available in 64.6% of all patients treated with OACs. Among the OAC users, the percentage of patients still on treatment with the index drug during the last 3 months of observation was 76.9%.
Figure 1 Stratification of treatment strategy assignment per risk category according to CHA2DS2-VASc score.
Abbreviations: OAC, oral anticoagulant; AP, antiplatelet.
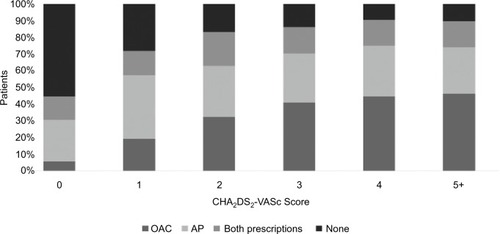
Figure 2 Stratification of treatment strategy assignment per bleeding risk category according to the HAS-BLED score.
Abbreviations: HAS-BLED, hypertension, abnormal renal and liver function, stroke, bleeding, labile INR, elderly (age >65 years), drugs (other AP agents or NSAIDs) or alcohol history; OAC, oral anticoagulant; AP, antiplatelet; INR, international normalized ratio; NSAID, nonsteroidal anti-inflammatory drug.
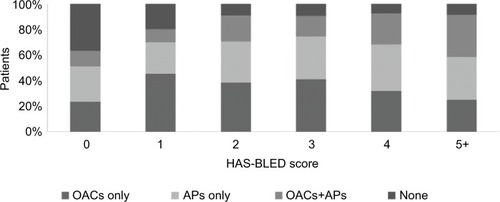
Table 3 Distribution of stroke risk and bleeding risk of patients according to the CHA2DS2-VASc and HAS-BLED scores, respectively
Discussion
AF is the most common sustained arrhythmia in Italy.Citation17,Citation18 We studied, retrospectively, a population of 1,413 patients with AF cared by 44 GPs. The AF prevalence varies considerably between countries, although this variance might partially be a function of the differences in the methods of data collection and the demographic characteristics of the populations investigated.Citation23,Citation24 In previous studies, the prevalence and incidence were higher in men than woman,Citation23 whereas in our study, the opposite trend was observed. In our study, the prevalence of AF was 2.09%; this value is in accordance with what was reported previously in a retrospective Italian study (on patients being cared for by 233 GPs, homogeneously distributed across Italy), in which the prevalence of AF was estimated to be of 1.85%.Citation18
The profile of comorbidities at baseline was in agreement with previous analyses and showed that hypertension was the most prevalent condition associated with AF patients.Citation18,Citation25
Our study shows that a considerable proportion of AF patients did not receive any prescription of ATs. Moreover, our finding shows that 55.8% of all patients enrolled were treated with OACs (39.56% were prescribed an OAC and 16.2% had both prescriptions during the observation period); the OAC use rate was lower than expected compared with the Euro Heart Survey (where, among 2,706 patients enrolled, ~64% patients received OAC due to AF)Citation26 or European countries.Citation27,Citation28 Our underutilization of OAC is in accordance with data observed in other two Italian studies. The survey conducted by Mazzaglia et alCitation18 from 2001 to 2004 showed that in patients with AF, the use of OACs and AP agents was 26.6% and 30.7%, respectively, and 5.5% of patients had both prescriptions. In the recent study, ISAF,Citation17 in which a diagnosis of AF was confirmed in 2.04% of all the patients screened, only 46% of the entire population received OACs, 37.5% were taking AP agents and 16.5% had no AT treatment at all. Taken together, these data indicate that despite the growth in the awareness of the benefits of anticoagulation as a treatment for AF, the underuse of OAC remains evident. In 2007, the ARNO Cardiovascular Observatory documented a percentage of OACs prescription of 42.7% in patients with a primary diagnosis of AF and 37.7% in patients with a secondary diagnosis of AF from hospital discharge records in the first month of follow-up post-discharge.Citation29
In the present study, we calculated the levels of stroke and bleeding risks according to risk stratification schemes. Although, HAS-BLED score is now recommended in European guidelineCitation1,Citation30 to estimate major bleeding risk in anticoagulated AF patients, physicians rarely take into consideration HAS-BLED in prescribing the therapy. This could be explained by the fact that many risk factors for stroke are also risk factors for bleeding. A substantial percentage of patients were associated with moderate and high scores; based on this risk profile, although AT therapy is highly recommended in AF patients with a CHA2DS2-VASc score of >2, we report underuse of AT therapies. OACs appear to be underused, even in patients with a high risk of stroke who might benefit from such medication. A recent review reported underuse of OAC in high-risk patients.Citation13 In addition, the AntiThrombotic Agents in Atrial Fibrillation (ATA-AF) study, performed in 2012, showed that a considerable underuse of OAC was observed in eligible high-risk patients, in whom the prescription rate was only 56%.Citation25
It is unclear why AF patients are untreated and guidelines are not followed in clinical practice. A recent Italian studyCitation31 analyzed the levels of knowledge and information on AF in the Italian population and the level of AF risk awareness by GPs and AF patients. The results showed that only one-third of Italians know that AF is perceived as a severe disease. In addition, Gensini et alCitation31 showed an underuse of the scores for thromboembolic and hemorrhagic risk stratification recommended by the current guidelines and a frequent use of AP agents rather than OAC therapy.
When the analysis was conducted, there were no data available about novel oral anticoagulants (NOACs); nevertheless, recently published studies show that adoption of NOACs might have a positive effect on the undertreatment of AF.Citation32–Citation34
In the current study, among the patients treated with OACs, >75% of all OACs users were still on treatment during the last months of the follow-up period. A number of studies have reported that noncompliance with anticoagulation therapy could have a significant clinical effect by increasing the thromboembolic and stroke risk, which could lead to prolonged hospital admissions and residential care and could play an important role in increasing the consumption of health care resources and in worsening morbidity and mortality.Citation35,Citation36 During OAC therapy, the frequent performing of coagulation tests reminds the patient of the importance of such treatment, and the rate of discontinuation could be indicated by abnormal INR results. In our analysis, a percentage of OAC patient records did not contain information on the INR, and we could not establish if INR tests were not performed or if the INR values were not reported in our database. Although the monitoring requirements of OACs are generally thought of as a negative factor discouraging OAC use, regular monitoring measures of patients’ compliance and the interface with expert health care providers might improve compliance to treatment.Citation37 The lack of information on the INR monitoring in the administrative database points toward the need for a greater effort in formation/communication with GPs.
Our analysis has several limitations inherent to any observational study. First, the analyses were performed using the databases of one LHU; although GPs in Bologna have a well-managed collaborative audit project that could lead to actual health care benefits for users and great improvement in health care quality, the findings of this study must be interpreted with caution, and further larger studies are required to confirm these results. A second limitation is the relatively small sample size of patients with a confirmed diagnosis of AF. A third limitation of this study is that the reasons for noncompliance with treatment in the patients are not retrievable from the dataset. For this reason, we cannot exclude that the occurrence of important contraindications or the use of concomitant treatment with potentially interacting medication might also explain the treatment discontinuation. In addition, no important clinical information was available to us. Finally, the OAC daily dose is extremely variable, because it is dependent on patient-related factors; therefore, the precision of the method used to calculate the percentage of patients still on treatment with the index drug during the observation period is likely to be limited.
Conclusion
Our study emphasizes that in an Italian real-world setting, the burden of AF in general population from a public health point of view underscores the need for improvement in utilization of appropriate ATs in patients with known AF.
The present findings suggest that a proportion of patients do not receive or discontinue therapy for AF management. Considering these findings, other studies are needed to identify the reason why AF treatment is not optimal and the relevance of the implementation of educational interventions aimed at improving the clinical management of patients with AF.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The GP group consisted of Emanuela Aldrovandi, Paolo Amorati, Luigi Bagnoli, Antonio Balduzzi, Giulio Bandi, Salvatore Bauleo, Antonino Cammarata, Roberto Cau, Lucia Cecchini, Enrico Delfini, Cecilia Deni, Giancarlo Furlò, Fabio Gentili, Angela Inì, Marco Maccaferri, Carla Marzo, Angelo Masi, Annunzio Matrà, Gaito PieroMazzetti, Giampiero Mazzoni, Federico Montanari, Dante Monti, Mara Mori, Massimo Oggianu, Maria Palasciano, Marcello Paolo, Laura Pittigliani, Stefano Quadrelli, Stefano Rubini, Marcello Salera, Sandra Santi, Alberto Serio, Matteo Siena, Elisabetta Simoncini, Luigi Simoni, Pietro Speziali, Luigi Spinnato, Cesare Tosetti, Pietro Velonà, Andrea Verri, Domenico Zisa, Donato Zocchi and Giuseppe Zoccoli.
Disclosure
The authors have no conflicts of interest to disclose. The opinions expressed in this article do not necessarily reflect the views of the authors’ institutions.
References
- CammAJLipGYDe CaterinaR2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm AssociationEur Heart J201233212719719
- ChughSSHavmoellerRNarayananKWorldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 StudyCirculation2014129883784724345399
- GoASHylekEMPhillipsKAPrevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and risk factors in Atrial Fibrillation (ATRIA) StudyJAMA2001285182370237511343485
- FeinbergWMBlackshearJLLaupacisAKronmalRHartRGPrevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implicationsArch Intern Med199515554694737864703
- CammAJKirchhofPLipGYGuidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC)Europace201012101360142020876603
- PriscoDCenciCSilvestriEEmmiGBarniniTTamburiniCThe risk stratification in atrial fibrillationIntern Emerg Med20127suppl 3S233S24023073863
- RavieleADisertoriMAlboniP webpage on the InternetLinee guida AIAC per la gestione e il trattamento della fibrillazione atriale. Aggiornamento 2013G Ital Cardiol2013 Available from: http://www.giornaledicardiologia.it/articoli.php?archivio=yes&vol_id=1234&id=13660Accessed April 27, 2017
- FusterVRydenLECannomDS2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm SocietyJ Am Coll Cardiol20115711e101e19821392637
- CurtisABPractice implications of the atrial fibrillation guidelinesAm J Cardiol2013111111660167023507710
- WasmerKEckardtLManagement of atrial fibrillation around the world: a comparison of current ACCF/AHA/HRS, CCS, and ESC guidelinesEuropace201113101368137421712281
- AndersonJLHalperinJLAlbertNMManagement of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on Practice GuidelinesJ Am Coll Cardiol201361181935194423558044
- HylekEMGoASChangYEffect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillationN Engl J Med2003349111019102612968085
- OgilvieIMNewtonNWelnerSACowellWLipGYUnderuse of oral anticoagulants in atrial fibrillation: a systematic reviewAm J Med20101237638.e4645.e420609686
- FerroDLoffredoLPolimeniLVioliFUnderuse of oral anticoagulants in patients with nonvalvular atrial fibrillation in ItalyIntern Emerg Med200721242817551680
- MonteSMacchiaAPellegriniFAntithrombotic treatment is strongly underused despite reducing overall mortality among high-risk elderly patients hospitalized with atrial fibrillationEur Heart J200627182217222316935869
- WilkeTGrothAPfannkucheMReal life anticoagulation treatment of patients with atrial fibrillation in Germany: extent and causes of anticoagulant under-useJ Thromb Thrombolysis20154019710725218507
- MazzagliaGFilippiAAlacquaMA national survey of the management of atrial fibrillation with antithrombotic drugs in Italian primary careThromb Haemost2010103596897520216987
- Zoni-BerissoMFilippiALandolinaMFrequency, patient characteristics, treatment strategies, and resource usage of atrial fibrillation (from the Italian Survey of Atrial Fibrillation Management [ISAF] study)Am J Cardiol2013111570571123273528
- Italian Medicine Agency (AIFA)Guideline for the Classification and Conduction of the Observational Studies on Medicines2017 Available from: https://www.agenziafarmaco.gov.it/ricclin/sites/default/files/files_wysiwyg/files/CIRCULARS/Circular%2031st%20May%202010.pdfAccessed April 27, 2017
- ShahMAvgil TsadokMJackeviciusCAWarfarin use and the risk for stroke and bleeding in patients with atrial fibrillation undergoing dialysisCirculation2014129111196120324452752
- Degli EspostiLSangiorgiDPerroneVAdherence and resource use among patients treated with biologic drugs: findings from BEETLE studyClinicoecon Outcomes Res2014640140725258545
- GerthWCCompliance and persistence with newer antihypertensive agentsCurr Hypertens Rep20024642443312419170
- HeeringaJvan der KuipDAHofmanAPrevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam studyEur Heart J200627894995316527828
- LeviMHobbsFDJacobsonAKImproving antithrombotic management in patients with atrial fibrillation: current status and perspectivesSemin Thromb Hemost200935652754219787556
- Di PasqualeGMathieuGMaggioniAPCurrent presentation and management of 7148 patients with atrial fibrillation in cardiology and internal medicine hospital centers: the ATA AF studyInt J Cardiol201316762895290322884698
- NieuwlaatRCapucciALipGYAntithrombotic treatment in real-life atrial fibrillation patients: a report from the Euro Heart Survey on atrial fibrillationEur Heart J200627243018302616731536
- MurphyNFSimpsonCRJhundPSA national survey of the prevalence, incidence, primary care burden and treatment of atrial fibrillation in ScotlandHeart200793560661217277353
- FribergLHammarNRinghMPetterssonHRosenqvistMStroke prophylaxis in atrial fibrillation: who gets it and who does not? Report from the Stockholm Cohort-study on Atrial Fibrillation (SCAF-study)Eur Heart J200627161954196416847008
- Osservatorio ARNO cardiovascolare [webpage on the Internet]La prevenzione secondaria dopo un evento di sindrome coronarica acuta2017 Available from: http://www.cineca.it/it/pubblicazione/osservatorio-arno-cardiovascolare-la-prevenzione-secondaria-dopo-un-evento-di-sindromeAccessed May 11, 2017
- CammAJPintoFJHankeyGJAndreottiFHobbsFDRWriting Committee of the Action for Stroke Prevention AllianceNon-vitamin K antagonist oral anticoagulants and atrial fibrillation guidelines in practice: barriers to and strategies for optimal implementationEuropace20151771007101726116685
- GensiniGFDi PasqualeGVaccaroCMIndagine Censis sulla conoscenza in Italia della fibrillazione atriale a livello dei cittadini, dei medici di medicina generale e dei pazienti. [A Censis survey on atrial fibrillation awareness in the general population and among general practitioners and affected patients in Italy]G Ital Cardiol Rome20141513743 Italian24503733
- KirleyKRaoGBauerVMasiCThe role of NOACs in atrial fibrillation management: a qualitative studyJ Atrial Fibrillation2016911416
- De CaterinaRRendaGSangiuoloRSteering Committee del Registro Europeo PREFER in AF (vedi Appendice 1)La gestione del rischio tromboembolico nei pazienti con fibrillazione atriale in Italia: dati al basale del Registro Europeo PREFER in AF. [Management of thromboembolic risk in patients with atrial fibrillation in Italy: baseline data from the PREFER in AF European Registry]G Ital Cardiol Rome201415299109 Italian24625849
- ForslundTWettermarkBHjemdahlPComparison of treatment persistence with different oral anticoagulants in patients with atrial fibrillationEur J Clin Pharmacol201672332933826613954
- BrownTMSiuKWalkerDPladevall-VilaMSanderSMordinMDevelopment of a conceptual model of adherence to oral anticoagulants to reduce risk of stroke in patients with atrial fibrillationJ Manag Care Pharm201218535136222663168
- ChenSYWuNGulsethMOne-year adherence to warfarin treatment for venous thromboembolism in high-risk patients and its association with long-term risk of recurrent eventsJ Manag Care Pharm201319429130123627575
- HessPLMirroMJDienerHCAddressing barriers to optimal oral anticoagulation use and persistence among patients with atrial fibrillation: Proceedings, Washington, DC, December 3-4, 2012Am Heart J20141683239.e1247.e125173533
- Gruppo Di Lavoro Artiocolo 29 per la protezione dei datiParere 05/2014 sulle tecniche di anonimizzazione, adottato il 10 aprile 2014 [Working Group Article 29 for protection of data. Opinion 05/2014 on the anonymization techniques, Adopted on 10 April 2014] Available from http://ec.europa.eu/justice/data-protection/article-29/documentation/opinion-recommendation/files/2014/wp216_it.pdfAccessed June 14, 2017 Italian
