Abstract
While pulse wave velocity (PWV) correlates with blood pressure (BP), its extent differs between patients, and some cases of high PWV in normotensives are present. Moreover, PWV frequently remains high in hypertensive patients despite adequate BP control. The factors associated with such phenomena are yet to be elucidated. Here, we investigated the factors associated with brachial–ankle PWV (baPWV) in 107 patients whose systolic BP was under 140 mmHg at their latest baPWV measurement. There were 64 controlled hypertensives and 43 normotensives. Multivariate regression analysis identified age, hypertension, body mass index (BMI), systolic BP, and heart rate (HR) as independent factors for baPWV. Next, we divided the subjects into groups according to their age (in 5-year increments) and calculated the mean and standard deviation (SD) of the baPWV for each group. For each age group, we defined patients with a baPWV above the mean + SD baPWV for the group as the high-baPWV cohort. Multivariate logistic regression analysis revealed that BMI, hypertension, and smoking were independent determinants of a high-baPWV subject. This represents the first study to report the existence of the hypertensive state itself as one of the independent predictors of high baPWV in normotensive and well-treated hypertensive patients. This finding implies that the hypertensive state itself possibly worsens arterial stiffness independently from aging in spite of adequate BP maintenance. To prevent the early progression of arterial stiffness, the application of an appropriate intervention during the early stages of hypertension is important and the continuation of an appropriate BP treatment is suggested.
Introduction
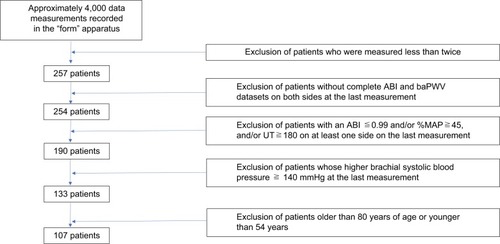
Brachial–ankle pulse wave velocity (baPWV) is an index of arterial stiffness that shows prognostic predictability independently from conventional atherosclerotic risk factors.Citation1,Citation2 In Western countries, evidence is mounting to indicate that aortic PWV represents a useful prognostic marker for arterial stiffness.Citation3,Citation4 The baPWV shows a strong correlation with aortic PWV,Citation5–Citation7 and a significant number of studies have demonstrated the prognostic significance of baPWV over recent years.Citation8–Citation10 Hypertension is the strongest risk factor for cardiovascular diseases, and adequate blood pressure (BP) control is essential in the prevention of such diseases.Citation2 PWV generally depends upon BP, but its extent is known to differ between patients. Depending on certain conditions, PWV sometimes displays independence from changes in BP.Citation5 Furthermore, even when BP is well controlled, there are cases of reduced PWV and frequent cases of PWV remaining high without improvement (). It is possible that this condition indicates a residual risk.Citation8,Citation9 However, factors associated with these phenomena have not been fully elucidated. Therefore, in the present study, we investigated the potential association between baPWV and a variety of factors in outpatients attending our clinic, both with and without hypertension, and in whom systolic BP was controlled to less than 140 mmHg.
Figure 1 Trend graphs of two typical blood pressure-controlled patients with or without improved baPWV.
Abbreviations: baPWV, brachial–ankle pulse wave velocity; BP, blood pressure; H, high; ST, standard.
Methods
Subjects
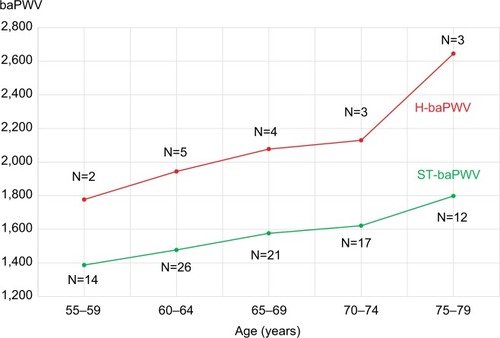
We recruited outpatients attending the Sawayama Clinic (Kurashiki city, Okayama, Japan) who had undergone simultaneous baPWV/ankle–brachial index (ABI) measurements at least three times before the end of October 2014 and who had bilateral baPWV values at the latest opportunity. depicts the patient selection process. The condition of baPWV/ABI measured at least three times was stipulated to ensure that we selected patients whose BP was continuously controlled over a definite period through hospital attendance. We did not include patients if data arising from unilateral baPWV, and/or ABI, were lacking in the latest opportunity. Moreover, we excluded patients who had an ABI ≤0.99, a percent mean arterial pressure (%MAP) of the ankle pulse waveform ≥45%, or an upstroke time (UT) ≥180 ms, at least unilaterally in the last examination; this was done to exclude possible cases of arteriosclerosis obliterans (ASO) and the underestimation of baPWV.Citation1,Citation11–Citation13 Furthermore, we excluded data from patients in whom systolic BP was >140 mmHg in their most recent test, as these patients could not be BP controls.Citation2 We excluded patients <54 or >80 of age due to the small numbers of such patients (n=14 and n=12, respectively). Finally, 107 patients, between 55 and 79 years of age, were included for analysis. Although four of these patients had a diastolic BP >90 mmHg, we did not exclude them. This was because diastolic BP showed no significant correlation with baPWV in this cohort, and we believed that these patients would have no significant influence on our statistical analysis. The data were obtained from the records of the Sawayama Clinic and were fully anonymized before analysis by the authors. The Sawayama Clinic permitted waiver of informed consent from subjects because of the retrospective study design and the fact that de-identified data were being accessed. The authors agreed with the study protocol, and the study was ethically conducted in accordance with the principles of the Declaration of Helsinki.
Measurements and variables
All variables related to BP and pulse wave examination were measured using a pulse waveform analyzer BP-203RPE II (form PWV/ABI, Nippon Colin, Komaki, Aichi, Japan). Details of the function and utility of this device have been described previously.Citation1,Citation5 Detailed explanations pertaining to %MAP and UT, derived from ankle pulse waveforms, have also been provided previously.Citation1,Citation11,Citation13 This device was also used to measure HR. For brachial BP, higher systolic BP and diastolic BP were used. Surrogate markers for arterial stiffness and lower limb atherosclerosis, higher baPWV, and lower ABI were used.Citation1 For additional surrogate markers of lower limb atherosclerosis, higher UT and %MAP were also selected. Moreover, this apparatus provided indices related to left ventricle systolic time intervals (STI), such as ejection time (ET), pre-ejection period (PEP), and ET/PEP.Citation14,Citation15 In five patients, at least one of the STI indices was not measured; thus, in terms of STI indices, data were collated from the remaining 102 patients. Most of the measurements from this device were conducted in the morning (106 out of 107). BMI was calculated as weight divided by height squared (kg/m2).
Definition of atherosclerotic risk factors
Hypertension was said to be present when BP recorded was >140/90 mmHg and/or when a patient was treated with anti-hypertensive medications. Diabetes and dyslipidemia were defined according to the current Japanese guidelines,Citation16,Citation17 including on the use of medications. Smoking was defined as having a regular smoking habit at the point when the last baPWV measurement was taken.
Statistical analysis
Continuous variables are expressed as means ± standard deviations (SDs), while nominal variables are expressed as percentage ratios (%). We compared characteristics between sexes and between patients with and without risk factors (hypertension, diabetes, dyslipidemia, or smoking), coronary arterial disease (CAD), and cerebrovascular disease (CVD). We identified indices correlating with baPWV using the Pearson correlation method and conducted multivariate regression analysis of baPWV as a dependent variable. Next, we divided patients into five groups according to their age, 55–59 years (n=16), 60–64 years (n=31), 65–69 years (n=25), 70–74 years (n=20), and 75–79 years (n=15). We then calculated the mean baPWV ± SD for each age group. We defined those with a baPWV ≤ mean + SD in each group as the standard baPWV (ST-baPWV, n=90), and those with a baPWV > mean + SD in each group as high baPWV (H-baPWV, n=17). Then, we undertook multivariate logistic regression analysis to identify independent determinants of H-baPWV. We conducted the Mann–Whitney–Wilcoxon test for continuous variables and the chi-square test for nominal variables to compare the two groups using Microsoft Excel 2016. Two multivariate analyses were also performed using EZR (EZR on R commander Version 1.33, September 1, 2016).Citation18 Multivariate analysis was based on a stepwise forward–backward procedure to determine independent factors. All the conventional risk factors (hypertension, diabetes, dyslipidemia, and smoking), and any variables for which probability (p) was identified by univariate analysis as <0.1 were also included in the model, except for indices of pulse waveforms (UT, %MAP, ET, and PEP). Statistical significance was set at p<0.05 (two tailed).
Results
shows the characteristics of all 107 patients, classified by sex, and highlighting those with ST-baPWV and those with H-baPWV. Taking all patients into account, mean age was 66±6 years, mean height was 164±8 cm, mean BMI was 22.8±2.9, mean systolic BP was 124±10 mmHg, mean baPWV was 1644±302 cm/s, and mean ABI was 1.14±0.07. Within our patient cohort, the proportion of those with hypertension was 60% (n=64), diabetes 16% (n=17), dyslipidemia 45% (n=48), smoking 37% (n=40), CAD 13% (n=14), and CVD 3% (n=3). Other heart diseases (OHD), rather than CAD, were identified in seven patients, including atrial fibrillation (n=2), ventricular tachycardia (n=1), supraventricular arrhythmia (n=1), sick sinus syndrome (n=1), hypertrophic cardiomyopathy (n=1), and mitral valve prolapse (n=1). Comparing sexes, males were significantly taller (168±5 cm vs 158±6 cm, p<0.00001) and had a significantly higher BMI (23.2±2.6 kg/m2 vs 22.0±3.1 kg/m2, p<0.05). Systolic BP was significantly higher in females (122±10 mmHg vs 126±9 mmHg, p<0.03), but there was no significant difference between sexes in terms of baPWV. The 17 patients with diabetes were male only (25% male vs 0% female, p<0.002). Smokers were mostly males (39 out of 40 smokers); the smoking ratio was also higher in males (58% vs 3%, p<0.00001). The incidence of CAD among males was higher than among females (18% vs 5%, p=0.07), whereas OHD was more common in females than among males (13% vs 3%, p=0.06).
Table 1 Patient characteristics according to sex and baPWV category
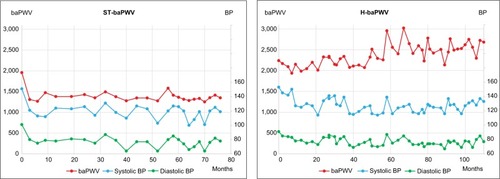
shows a comparison between patients with ST-baPWV (n=90) and H-baPWV (n=17). Age and systolic BP were not significantly different between those with ST-baPWV and those with H-baPWV (age 66±6 and 67±7; systolic BP: 123±9 mmHg and 126±9 mmHg, respectively). The baPWV was significantly higher in the H-baPWV group (1,556±206 cm/s in ST-baPWV patients and 2,112±301 cm/s in H-baPWV patients, p<0.00001). Furthermore, baPWV increased with age in both the ST-baPWV and H-baPWV groups although there was no significant difference in systolic BP among different generations (). Ratios of hypertension and smoking were not significantly different when compared between these two groups (hypertension: 56% and 82%, smoking: 34% and 53%, respectively). BMI was significantly lower in the H-baPWV group (23.1±2.8 kg/m2 and 20.8±2.5 kg/m2, p<0.002), whereas HR was significantly higher in the H-baPWV group (63±10 bpm and 68±9 bpm, p<0.04).
Figure 3 The baPWV according to age and category.
depicts our univariate analysis of factors and baPWV. There were significant correlations between baPWV and age (R=0.49, p<0.00001), BMI (R=−0.24, p<0.02), systolic BP (R=0.26, p<0.01), HR (R=0.27, p<0.01), and hypertension (R=0.32, p<0.001). However, baPWV did not correlate with diabetes, dyslipidemia, smoking, CAD, CVD, or OHD. also depicts the results arising from our multivariate regression analysis using baPWV as a continuous variable. Age (β=0.43, p<0.00001), hypertension (β=0.61, p<0.0001), systolic BP (β=0.25, p<0.001), BMI (β=−0.28, p<0.001), and HR (β=0.23, p<0.01) were identified as independent determinants of baPWV. Of these factors, patient age was the strongest determinant (t=6.00); among the other factors, hypertension had the most powerful influence (β=0.61, t=4.13).
Table 2 Univariate and multivariate regression analysis of factors and baPWV as a continuous variable
Finally, presents the results arising from our multivariate logistic regression analysis for H-baPWV as a dependent variable. Independent determinants of H-baPWV were BMI (odds ratio [OR] 0.57, 95% confidence interval [CI] 0.42–0.78, p<0.001), hypertension (OR 6.41, 95% CI 1.46–28.1, p<0.02), and smoking (OR 4.62, 95% CI 1.23–17.3, p<0.03). In addition, HR showed a tendency to represent an independent determinant, although this was not statistically significant (OR 1.06, 95% CI 0.99–1.13, p=0.055).
Table 3 Multivariate logistic regression analysis of H-baPWV determinants
Discussion
To the best of our knowledge, this is the first study to demonstrate that the hypertensive state itself is a determinant of high baPWV in patients with adequately controlled BP. A phenomenon that correlates baPWV with systolic BP is consistent with its properties despite the fact that the systolic BP of our study subjects was <140 mmHg. Nevertheless, multivariate regression analysis showed that systolic BP influenced only approximately 70 cm/s of baPWV for every SD increase in systolic BP. On the other hand, the hypertensive state itself emerged as an independent determinant that could increase baPWV to 184 cm/s despite the adequate achievement of an antihypertensive condition. This influence is the equivalent of aging by 9 years (184.1 ÷ 19.8=9.3). Furthermore, those in a hypertensive state were predicted to develop H-baPWV by an OR of six. These results imply that the hypertensive state itself is a candidate predictor for H-baPWV. In contrast, there was no difference in baPWV for those with or without diabetes and dyslipidemia. These results, particularly the fact that baPWV was not associated with diabetes mellitus, are contradictory to the results of a recent Mendelian randomization study, which indicated the causal role of diabetes on baPWV.Citation19 For this reason, we consider that the rate of diabetes was relatively low in our subjects (16%). Moreover, our institute is a cardiology clinic that focuses particularly upon primary prevention. Consequently, there may be differences in terms of our patient characteristics as compared with those attending other institutes or departments, such as general medicine, diabetic clinics, or a foundation hospital. Our finding that baPWV had no association with dyslipidemia is plausible for several reasons, including the findings of a recent Mendelian randomization study that has evaluated triglyceride as a causative factor.Citation20–Citation22 Dyslipidemia is a factor that mainly affects the formation of intimal hyperplasia and plaque formation. On the other hand, baPWV is a factor that mainly reflects the stiffness or function of an aortic wall.Citation5–Citation7 Furthermore, statins are mainly used to treat low-density lipo-protein cholesterol, and several studies have demonstrated differences in baPWV improvement, which relate to different types of statins. This suggests variance in pleiotropy, including antioxidative effects.Citation23–Citation25 For these reasons, dyslipidemia did not associate strongly with baPWV.
BMI was identified as a negative independent determinant of baPWV as a continuous variable and H-baPWV. A similar report has been published for a health check-up population in which the reference value of baPWV in each gender was calculated. Furthermore, it showed that BMI was independently associated with baPWV in a negative manner.Citation21 Generally, lean individuals possibly have lesser volume of circulating blood and have arteries of smaller caliber (higher PWV), especially if BPs are similar. Our result would not contradict this logic. However, the influence of BMI in our study was approximately threefold higher than that of the health check-up population (β=−0.09 in males, β=−0.08 in females).Citation21 There are several different factors between our study subjects and the health check-up population. Those are mean age (~20 years), mean baPWV (~400 cm/s), and independent determinants identified by multivariate analysis.Citation21 Mechanisms related to body composition such as sarcopenia could also have influenced baPWV. Ochi et al investigated the relationship between baPWV and sarcopenia in a cohort of middle-aged and elderly patients. They showed that the ratio of thigh muscle cross-sectional area to body weight correlated in a negative independent manner with baPWV.Citation26 There have also been continuous reports of the “obesity paradox” over recent years.Citation27–Citation30 Especially, we noted striking evidence which showed simply, “the leaner they are, the earlier they decease,” in a Japanese elderly cohort (aged 65~79) of the Japan Collaborative Cohort study.Citation27 A synchronized phenomenon of 1) weight reduction mainly due to muscle mass reduction, 2) aortic stiffness progression, and 3) the trajectory of prognostic disadvantage from the aspect of baPWV in middle-aged and elderly patients may be consistent. Another study reported regional differences in PWVs in terms of correlation with BMI.Citation31 Further studies are now needed to clarify these mechanisms.
In the present study, smoking emerged as an independent factor for H-baPWV although baPWV did not differ significantly between those with or without smoking. Furthermore, some studies have shown inconsistent results in terms of the influence of smoking upon baPWV.Citation21,Citation32–Citation37 According to these reports, smoking acted acutely to increase baPWV as a whole. Nevertheless, in terms of long-term effects, smoking might have possible interactions with a variety of other factors, including exercise habits, total amount of smoking, smoking duration, and genetic factors.Citation36,Citation37 These interactions may, thus, exert influences upon baPWV.
We found, moreover, that HR was an independent factor for baPWV as a continuous variable and tended to be a determinant of H-baPWV. Compared to subjects in previous studies, who also showed an association between HR and baPWV,Citation38,Citation39 our subjects were older. This phenomenon might possibly be related to sympathetic nerve activity.Citation40–Citation42
We first demonstrated that the hypertensive state itself represents an independent factor for both baPWV and H-baPWV, especially among patients without hypertension and patients with appropriately treated hypertension. This result may represent a potential countermeasure for a future “heart failure (HF) pandemic.”Citation43,Citation44 The baPWV has already been proved to be a predictor of all-cause mortality and cardiovascular events, even after adjustment for conventional atherosclerotic risk factors.Citation8–Citation10 Moreover, using baPWV with a cutoff of 1,750 cm/s, recurrent HF in those with normal BP and the onset of HF can be efficiently predicted.Citation45,Citation46 Knowledge of baPWV also enhances our ability to diagnose heart failure with preserved ejection fraction (HFpEF) in patients with acute dyspnea.Citation47 Cong et al reported that the diagnostic accuracy for HFpEF significantly improved after adding baPWV to the diagnostic criteria of the 2007 ESC consensus statement (net reclassification improvement 0.127, p=0.02).Citation47 Collectively, these data suggest that baPWV has the diagnostic ability to predict patients with a high risk of HF and has adjunctive value to diagnose HFpEF. Moreover, this examination can simultaneously measure indices for left ventricle (LV) function; ET/PEP can accurately predict a reduced ejection fraction and LV dyssynchrony.Citation15,Citation48 Furthermore, ET/PEP can efficiently identify abnormal LV–aorta coupling in stable patients with HF.Citation49 Thus, this measurement device could efficiently support the evaluation or prediction of a decline in LV function and HF. Furthermore, it has been reported that baPWVCitation50–Citation53 and aortic stiffnessCitation54,Citation55 are independent predictors of the onset of hypertension. With regard to the Japanese population only, a cutoff value of approximately 14 m/s was shown to significantly raise the OR and the hazard ratio.Citation50–Citation52 One reason for the baPWV cut-off value at 14 m/s is that this represents “middle-risk”; this cutoff is recommended for lifestyle modifications in the guidelines for “vascular function tests” published by the Japanese Circulation Society.Citation1,Citation51 Therefore, it is implied that baPWV is able to stratify normotensive patients at higher risk of the onset of hypertension. Needless to say, genetic factors are also considered as one of the causes of hypertension.Citation2 Yet, the mechanism involved is not understood because the onset of hypertension is also strongly affected by a combination of acquired and environmental factors.Citation2 Thus, to predict the onset of hypertension, the use of baPWV testing is both simple and economical,Citation1,Citation5 and could be a more realistic measure than those available at present. Once hypertension develops, a natural consequence is for arterial stiffness to progress synergistically. The extent of the accumulating damage upon the vessels would depend upon the duration for which hypertension was untreated and the internal pressure of the arteries. As a result, even if hypertension is controlled for a certain period after its onset, it follows that the baPWV of such patients gets higher than it does in patients whose BP is maintained at normal levels.Citation56 The baPWV also shows individual differences, even in the pediatric population.Citation21,Citation57–Citation60 Tomiyama et al described reference values for baPWV in healthy Japanese adults without atherosclerotic risk factors.Citation21 The explanatory power of the relevant quadratic regression curve was limited (male R2=0.16, female R2=0.37, both p<0.01). This indicates that there are clear individual differences in baPWV, even within populations without any atherosclerotic risk factors. Taking this information together, the wider application of a simple baPWV measurement could be a very practical method over the next few decades. Because this measurement can stratify the high risks of hypertension and HF in Japan. Furthermore, baPWV is an independent predictor for all-cause mortality and cardiovascular events.Citation1,Citation2,Citation8–Citation10 We should also consider that, even in young normotensive subjects, if baPWV is higher than the normal range (> mean + SD) according to their ages, then there is a higher risk of developing hypertension earlier. In addition, the subject should receive advice pertaining to lifestyle modifications.
Limitations
There are several limitations of this study that should be considered when interpreting our conclusions. First, our study design was retrospective and cross-sectional in design, although there was an element of longitudinal design. As such, our results do not prove causation. Nevertheless, we can consider that one causative factor is the so-called “vicious cycle” in that a delay, or the neglect of hypertensive treatment, could exacerbate aortic stiffness, and that progressive aortic stiffness itself would further exacerbate hypertension. Second, we did not consider any information relating to blood samples and medication. We must consider that it is likely that there would be residual confounding factors present in class effects, the quantity of prescribed medications, and also in the combination of medications. Third, we did not consider renal function or estimated glomerular filtration rate (eGFR). It is not the case that chronic kidney disease, or end-stage renal failure alone can predict a poorer prognosis.Citation2,Citation61 Nevertheless, recent Mendelian randomization studies have, at least, cast doubt on the causative relationship between cardiovascular prognosis and eGFR or cystatin C. Specifically, causative factors related to eGFR and CADCitation62 and on the association between serum cystatin C and cardiovascular eventsCitation63 are evaluated. In other words, these studies potentially suggest that the surrogate indices of renal function, such as eGFR and serum cystatin C, are only mediating factors of prognosis. Further, those indices have no causality with regard to atherosclerotic events.Citation62,Citation63 Therefore, it might be inappropriate to undertake statistical analysis upon eGFR and cystatin C as independent determinants for baPWV, because we hypothesize that baPWV is a prognostic predictor. Fourth, we excluded some patients as possible ASO patients using not only borderline ABI (≤0.99) but also by using high %MAP (≥45) and UT (≥180).Citation1,Citation11,Citation13 Thus, there is a possibility that we may have excluded pseudo-positive ASO. On the other hand, there was a high correlation between %MAP and UT (R>0.8, p<0.00001). Thus, even if ABI is normal (≥1.0), ASO is likely, especially in those with UT and %MAP close to the exclusion criteria (i.e. 40<%MAP<45 and 170<UT<180). Therefore, although we used ASO exclusion criteria in our investigation, the possibility of underestimating baPWV is undeniable, due to pseudo-negative ASO. Fifth, our study design did not include any indices related to home BP. It was impossible to consider relationships relating to masked hypertension, morning BP, nocturnal BP, or obstructive sleep apnea. The current Japanese guidelines for hypertension prioritize home BP rather than clinic BP.Citation2 Nevertheless, we analyzed only patients whose clinic systolic BP was 123±9 (103–139) mmHg, including hypertensives, after attending our clinic on at least three occasions. It would be reasonable to suppose that antihypertensive treatment was administered in hypertensives at least several days before we measured baPWV. It is also appropriate to consider that H-baPWV arises from the influence of the hypertensive state itself. Sixth, we did not measure aortic calcification; therefore, this influence may have been masked in our analysis.Citation64 Finally, our analysis only involved outpatients attending a clinic located in a suburban area of a provincial city in Japan, and featured a relatively small number of subjects. A prospective study on a larger scale is now required to confirm our findings.
Conclusion
We demonstrated that the hypertensive state itself is an independent determinant of high baPWV in outpatients with atherosclerotic risk factors and in whom systolic BP is controlled to <140 mmHg. These results suggest the importance of treating hypertension from an early stage to control potential effects upon arterial stiffness.
Disclosure
Dai Ato wrote this article as an academic activity based on the guaranteed right of freedom in academy for the Japanese (Article 23), and on the supreme law provided in Article 98 of the Constitution of Japan. Dai Ato is a former employee of Fukuda Colin (formerly Omron Colin, Nippon Colin) Co., Ltd. Fukuda Colin is one of the distributors of the PWV/ABI device (BP-203RPE series). and reports. Dai Ato reports no other conflicts of interest in this work. Toshitami Sawayama reports no conflicts of interest in this work.
References
- YamashinaAKarioKKoharaK[Guidelines for noninvasive vascular function test] (JCS2013) Available from: http://www.j-circ.or.jp/guideline/pdf/JCS2013_yamashina_h.pdfAccessed September 20, 2017 Japanese
- ShimamotoKAndoKFujitaTJapanese Society of Hypertension Committee for Guidelines for the Management of HypertensionThe Japanese Society of Hypertension Committee for Guidelines for the Management of HypertensionHypertens Res201437425339024705419
- VlachopoulosCAznaouridisKStefanadisCPrediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysisJ Am Coll Cardiol201055131318132720338492
- Ben-ShlomoYSpearsMBoustredCAortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjectsJ Am Coll Cardiol201463763664624239664
- YamashinaATomiyamaHTakedaKValidity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurementHypertens Res200225335936412135313
- SugawaraJHayashiKTanakaHArterial path length estimation on brachial-ankle pulse wave velocity: validity of height-based formulasJ Hypertens201432488188924609216
- SugawaraJTanakaHBrachial-ankle pulse wave velocity: myths, misconceptions, and realitiesPulse (Basel)20153210611326587459
- VlachopoulosCAznaouridisKTerentes-PrintziosDIoakeimidisNStefanadisCPrediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysisHypertension201260255656222733468
- OhkumaTNinomiyaTTomiyamaHCollaborative Group for J-BAVEL (Japan Brachial-Ankle Pulse Wave Velocity Individual Participant Data Meta-Analysis of Prospective Studies)Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysisHypertension20176961045105228438905
- AtoDTakamiTBrachial-ankle pulse wave velocity, mortality, and cardiovascular eventsJ Cardiovasc Disord2015211009
- HashimotoTIchihashiSIwakoshiSKichikawaKCombination of pulse volume recording (PVR) parameters and ankle-brachial index (ABI) improves diagnostic accuracy for peripheral arterial disease compared with ABI aloneHypertens Res201639643043426911230
- YokoyamaHShojiTKimotoEPulse wave velocity in lower-limb arteries among diabetic patients with peripheral arterial diseaseJ Atheroscler Thromb200310425325814566089
- SawayamaTUp-stroke Time Prolongation as Potential Early Diagnostic Marker of Peripheral Artery Disease – A Longitudinal StudyJapanese J Clin Physiol20164627985 Article in Japanese
- SawayamaTOchiaiMMarumotoSMatsuuraTNikiIInfluence of amyl nitrite inhalation on the systolic time intervals in normal subjects and in patients with ischemic heart diseaseCirculation19694033273355810889
- ShimizuMFujiiHYamawakeNNishizakiMPrognostic Value of Systolic Time Interval Analysis on Pulse Wave Examination for Poor Left Ventricular Contraction and DyssynchronyJapanese J Clin Physiol20164628794 Article in Japanese
- The Japan Diabetes SocietyEvidence-based Practice Guideline for the Treatment for Diabetes in Japan 2013 Available from: http://www.jds.or.jp/modules/en/index.php?content_id=44Accessed September 20, 2017
- Japan Atherosclerosis SocietyJapan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2012(June 20, 2012) Available from: http://www.j-athero.org/en/publications/guideline2012.htmlAccessed September 20, 2017
- KandaYInvestigation of the freely available easy-to-use software “EZR” for medical statisticsBone Marrow Transplant201348345245823208313
- XuMHuangYXieLDiabetes and risk of arterial stiffness: a mendelian randomization analysisDiabetes20166561731174026953161
- YaoWMZhangHFZhuZYGenetically elevated levels of circulating triglycerides and brachial-ankle pulse wave velocity in a Chinese populationJ Hum Hypertens201327426527022648266
- TomiyamaHYamashinaAAraiTInfluences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement—a survey of 12517 subjectsAtherosclerosis2003166230330912535743
- LiuZBurgessSWangZAssociations of triglyceride levels with longevity and frailty: a Mendelian randomization analysisSci Rep201774157928134330
- IchiharaAHayashiMKouraYTadaYKaneshiroYSarutaTLong-term effects of statins on arterial pressure and stiffness of hypertensivesJ Hum Hypertens200519210310915361892
- HongoMKumazakiSIzawaALow-dose rosuvastatin improves arterial stiffness in high-risk Japanese patients with dyslipidemia in a primary prevention groupCirc J201175112660266721857142
- ToyamaKSugiyamaSOkaHCombination treatment of rosuvastatin or atorvastatin, with regular exercise improves arterial wall stiffness in patients with coronary artery diseasePLoS One201277e4136922829944
- OchiMKoharaKTabaraYArterial stiffness is associated with low thigh muscle mass in middle-aged to elderly menAtherosclerosis2010212132733220554280
- TamakoshiAYatsuyaHLinYJACC Study GroupBMI and all-cause mortality among Japanese older adults: findings from the Japan collaborative cohort studyObesity (Silver Spring)201018236236919543206
- Berrington de GonzalezAHartgePCerhanJRBody-mass index and mortality among 1.46 million white adultsN Engl J Med2010363232211221921121834
- TobiasDKPanAJacksonCLBody-mass index and mortality among adults with incident type 2 diabetesN Engl J Med2014370323324424428469
- FlegalKMKitBKOrpanaHGraubardBIAssociation of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysisJAMA20133091718223280227
- ChooJShinCBarinas-MitchellERegional pulse wave velocities and their cardiovascular risk factors among healthy middle-aged men: a cross-sectional population-based studyBMC Cardiovasc Disord201414524410766
- KimJWParkCGHongSJAcute and chronic effects of cigarette smoking on arterial stiffnessBlood Press2005142808516036484
- TomiyamaHHashimotoHTanakaHContinuous smoking and progression of arterial stiffening: a prospective studyJ Am Coll Cardiol201055181979198720430271
- KubozonoTMiyataMUeyamaKAcute and chronic effects of smoking on arterial stiffnessCirc J201175369870221187657
- FukuiTMaruyamaMYamauchiKAbeYYoshitakaSYasudaTTen-year longitudinal study on brachial-ankle pulse wave velocity (baPWV) in middle-aged Japanese males - analysis of relationship with clustering of atherosclerosis risk factorsNingen Dock International201527075
- ParkWMiyachiMTanakaHDoes aerobic exercise mitigate the effects of cigarette smoking on arterial stiffness?J Clin Hypertens (Greenwich)201416964064425135246
- JiYGeJZhuZWangFJiangJCaoHRelationship between C242T polymorphism and arterial stiffness in an apparently healthy populationJ Hum Hypertens201630848849226467818
- SuHMLeeKTChuCSEffects of heart rate on brachial-ankle pulse wave velocity and ankle-brachial pressure index in patients without significant organic heart diseaseAngiology2007581677417351160
- SonodaHTakaseHDohiYKimuraGFactors associated with brachial-ankle pulse wave velocity in the general populationJ Hum Hypertens2012261270170522089729
- SugawaraJKomineHHayashiKEffect of systemic nitric oxide synthase inhibition on arterial stiffness in humansHypertens Res200730541141517587753
- SwierblewskaEHeringDKaraTAn independent relationship between muscle sympathetic nerve activity and pulse wave velocity in normal humansJ Hypertens201028597998420408258
- TomiyamaHHashimotoHTanakaHbaPWV/cfPWV Collaboration GroupSynergistic relationship between changes in the pulse wave velocity and changes in the heart rate in middle-aged Japanese adults: a prospective studyJ Hypertens201028468769420051904
- ShimokawaHMiuraMNochiokaKSakataYHeart failure as a general pandemic in AsiaEur J Heart Fail201517988489226222508
- KonishiMIshidaJSpringerJHeart failure epidemiology and novel treatments in Japan: facts and numbersESC Heart Fail20163314515127840692
- MeguroTNagatomoYNagaeAElevated arterial stiffness evaluated by brachial-ankle pulse wave velocity is deleterious for the prognosis of patients with heart failureCirc J200973467368019246812
- AisuHSaitoMInabaSAssociation of worsening arterial stiffness with incident heart failure in asymptomatic patients with cardiovascular risk factorsHypertens Res201740217318027581536
- CongTJiangSWangKZhongLWuJSuDPredictive value of brachial-ankle artery pulse wave velocity to heart failure with preserved ejection fraction in hospitalised patients with acute dyspnoeaPak J Med Sci201531351652126150835
- ChenSCChangJMLiuWCSignificant correlation between ratio of brachial pre-ejection period to ejection time and left ventricular ejection fraction and mass index in patients with chronic kidney diseaseNephrol Dial Transplant20112661895190220935012
- ChengHMYuWCSungSHWangKLChuangSYChenCHUsefulness of systolic time intervals in the identification of abnormal ventriculo-arterial coupling in stable heart failure patientsEur J Heart Fail200810121192120019004668
- TakaseHDohiYToriyamaTBrachial-ankle pulse wave velocity predicts increase in blood pressure and onset of hypertensionAm J Hypertens201124666767321331056
- TomiyamaHMatsumotoCYamadaJPredictors of progression from prehypertension to hypertension in Japanese menAm J Hypertens200922663063619265783
- SatohHSaijoYKishiRTsutsuiHBrachial-ankle pulse wave velocity is an independent predictor of incident hypertension in Japanese normotensive male subjectsEnviron Health Prev Med201116421722321431793
- ZhengXJinCLiuYArterial stiffness as a predictor of clinical hypertensionJ Clin Hypertens (Greenwich)201517858259125917107
- LiaoDArnettDKTyrolerHAArterial stiffness and the development of hypertension. The ARIC studyHypertension199934220120610454441
- NajjarSSScuteriAShettyVPulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of AgingJ Am Coll Cardiol200851141377138318387440
- DobaNTokudaYTomiyamaHGoldsteinNEKushiroTHinoharaSChanges in ankle brachial pulse wave velocity during a five-year follow-up period in older Japanese adults: sub-analysis results of the health research volunteer study in JapanIntern Med2013521212723291670
- NiboshiAHamaokaKSakataKInoueFCharacteristics of brachial- ankle pulse wave velocity in Japanese childrenEur J Pediatr2006165962562916636815
- ShiotaniAMotoyamaMMatsudaTMiyanishiTBrachial-ankle pulse wave velocity in Japanese university studentsIntern Med200544769670116093589
- WatanabeYMasakiHYunokiYAnkle-brachial index, toe-brachial index, and pulse volume recording in healthy young adultsAnn Vasc Dis20158322723526421072
- LiSChenWSrinivasanSRBerensonGSChildhood blood pressure as a predictor of arterial stiffness in young adults: the Bogalusa heart studyHypertension200443354154614744922
- Nihon Jinzo GakkaiSpecial issue: Evidence-based practice guideline for the treatment of CKDNihon Jinzo Gakkai Shi2013555585860 Article in Japanese23980478
- CharoenPNitschDEngmannJUCLEB ConsortiumMendelian Randomisation study of the influence of eGFR on coronary heart diseaseSci Rep201662851427338949
- van der LaanSWFallTSoumaréACystatin C and cardiovascular disease: a Mendelian randomization studyJ Am Coll Cardiol201668993494527561768
- NakamuraUIwaseMNoharaSKanaiHIchikawaKIidaMUsefulness of brachial-ankle pulse wave velocity measurement: correlation with abdominal aortic calcificationHypertens Res200326216316712627877