Abstract
Objectives
The aim of the study was to assess all-cause mortality and cardiovascular (CV) events in patients after a period of 12 months of treatment with dual antiplatelet therapy (DAPT) after hospitalization for acute myocardial infarction (AMI) in a real-world setting. Health care costs for the management of patients post-AMI was also assessed.
Methods
A retrospective analysis using data from the administrative databases of six local health units (LHUs) was performed. All beneficiaries of these LHUs hospitalized with AMI between January 01, 2010, and December 31, 2011, and exposed to a treatment period with DAPT up to 12 months after AMI discharge were included. All-cause mortality, CV hospitalizations, and health care costs occurring during the 36-month follow-up period from end of treatment with DAPT were considered. For the cost analysis, only patients still alive at the end of the follow-up period were included.
Results
A total of 2,721 patients were included (mean ± SD age 63.6±17.3 years, 67.8% males). About 17% and 18% of all patients had CV events and died during the follow-up period, respectively. The annual mean cost per patient was €3,523.27. During the follow-up period, 63 patients had a second AMI event; for whom, the mean health care cost per patient was €19,570.70.
Conclusion
In a real-world setting in Italy, considering a 36-month follow-up period, all-cause mortality, CV events, and related health care cost of patients hospitalized with an AMI undergoing a 12-month treatment period with DAPT remained relevant. This study suggests that increased efforts aimed at the prevention of recurrent AMI are warranted, as well as an accurate risk stratification in order to improve long-term outcome.
Introduction
Acute coronary syndrome (ACS) is still one of the most common cardiac diseases, with substantial morbidity and mortality.Citation1 The clinical spectrum of ACS includes unstable angina, non-ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction. Worldwide each year more than 7 million people experience acute myocardial infarction (AMI), in which 1-year mortality rates are now 10%, but vary with patient characteristics.Citation2–Citation4
Current guidelines for the management of ACS recommend both a pharmacological approach and a mechanical reperfusion with percutaneous coronary intervention (PCI).Citation5–Citation7
Antiplatelet agents are the mainstay therapy for all clinical settings of ACS.Citation8 Given that platelet-rich thrombi are a common feature of all forms of ACS, antiplatelet therapies are indicated both in the acute phase of ACS and in the postacute phase to reduce the risk of reinfarction.
In particular, dual antiplatelet therapy (DAPT) has become the standard of care for patients with AMI, and new antiplatelet agents have become available.Citation9
European guidelines currently recommend treatment with the initiation of DAPT with acetylsalicylic acid and an irreversible thienopyridine P2Y12 inhibitor (clopidogrel or prasugrel) or reversibly binding (ticagrelor) to reduce the risk of acute ischemic complications and recurrent athero-thrombotic events for up to 1 year after ACS.Citation5
Notably, despite progress in evidence-based treatments and improved outcomes, preventive care post-ACS remains suboptimal, thus resulting in worse outcomes and higher health care costs.Citation10 Among patients who survive an AMI, 20% suffer a second cardiovascular (CV) event in the first year and approximately 50% of major coronary events occur in those with a previous hospital discharge diagnosis of AMI.Citation11 Within the first year after AMI, CV rehospitalizations are common.Citation12–Citation14 Although the total all-cause rehospitalizations cannot be prevented, readmissions within a short time can be reduced with a proper prevention and they can be considered as a marker for low-quality care and efficiency.Citation15 Several studies have reported 30-day rehospitalization rates and predictors of composite events (such as major adverse cardiac events) among patients surviving hospitalization for AMI;Citation16–Citation19 nevertheless, few studies have evaluated the residual risk of recurrent events after treatment with DAPT, including both all-cause mortality rate and potential predictors of death. In addition, there are few contemporary data that describe the economic impact among patients surviving an AMI after treatment with DAPT. Health care costs related to disease morbidity are most closely associated to the prevention and management of disease directly. Additionally, in a rapidly aging society, the number of AMI patients with higher severity is likely to increase, which can lead to an increase in medical expenditures related to hospitalization.
This study aims to assess all-cause mortality and CV events in patients after 12 months of treatment with DAPT after hospitalization for AMI in a unselected Italian population under clinical practice setting. Health care direct costs (in terms of pharmaceutical and hospitalization costs) for the management of patients’ post-AMI will be assessed as well.
Methods
Data sources
This study was based on data from the administrative databases of six Italian local health units (LHUs), geographically distributed. In particular, the following databases were used: the Health-Assisted Subjects’ Database, containing patients’ demographic data; Outpatients and Inpatients Pharmaceutical Drugs Database, providing information for each medication prescription, such as the ATC (Anatomical Therapeutic Chemical) code of the drug purchased, the number of packages, the number of units per package, the dosages, the unit cost per package, and the prescription date; Hospital Discharge Database, which includes all hospitalization data with the discharge diagnosis codes classified according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). This administrative database is complete and includes validated data, and it has been used in previous real-world studies.Citation20,Citation21
The patient code in each database permitted electronic linkage between all databases. Informed consent is not required by the LHU ethics committee for using the encrypted retrospective information, according to Italian regulations. This study was notified to the local ethics committee in each participating LHU according to the Italian law,Citation22 regarding the conduct of observational analysis, and the LHU Ethics Committees approved the study.
Study design and cohort definition
This observational retrospective cohort analysis included all beneficiaries of each LHUs hospitalized with a primary diagnosis of AMI (ICD-9-CM code: 410) between January 1, 2010, and December 31, 2011 (enrollment period). The date of AMI discharge was identified as the index date (ID), which represents the enrollment day of each individual patient, who was then followed for 36 months from ID (follow-up period). Data on baseline characteristics, including demographics, risk factors, and medical history, were investigated for 12 months prior to ID (characterization period). Only cohort of patients hospitalized with a primary diagnosis of AMI during the enrollment period and exposed to a period of treatment with DAPT after AMI discharge of 12 months [acetylsalicylic acid (ATC code: B01AC06)+P2Y12 adenosine diphosphate receptor inhibitors (ATC codes: B01AC04, B01AC05, B01AC22, B01AC24)] was considered for the first and second objectives in the analysis. All-cause mortality and CV hospitalizations occurring from the end of treatment with DAPT to the subsequent 36-month follow-up period were considered.
From the analysis we excluded all patients diagnosed with cancer (ICD-9-CM code: 14X-20X) or anemia (ICD-9-CM codes: 281, 283, 284, 285) at AMI discharge (ID) and patients with a follow-up duration of less than 3 years. In addition, we excluded LHUs of Frosinone and Grosseto because data on deaths were not available and patients were transferred to another LHU during the follow-up period.
Study variables
Data on baseline characteristics, including demographics (age and gender) and medical history, were collected during the characterization period; previous CV hospitalizations were identified by ICD-9-CM codes: 410–414; myocaridal infarction (MI) at ID with PCI [procedure codes (primary or secondary discharge reasons): 00.66, 36.0x or absence of 36.04] or MI of other anterior wall (ICD-9-CM codes: 410.0 or 410.1) or MI at ID with coronary angiography [ICD-9-CM codes (primary or secondary discharge reasons): 8855, 8856, 8857] or coronary stent implantation [with drug-eluting stents (DES)] (procedure code: 0055) were also evaluated. The presence of chronic kidney disease was also identified by ICD-9-CM code: 585 (primary or secondary discharge reasons) during the characterization period.
Hospitalizations for AMI and all-cause mortality occurring from the end of treatment with DAPT to the subsequent 36-month follow-up period were considered.
A patient was defined in treatment with antidiabetic, antihypertensive, or agent for heart disease if he had at least two prescriptions of oral hypoglycemic drugs and/or insulin (ATC code: A10), antihypertensive drugs (ATC codes: C02, C03, C08), or cardiac drugs (ATC code: C01), respectively, during the follow-up period. A patient was defined as treated with statins (ATC code: C10AA, C10BA02), beta-blocking agents (ATC code: C07), or angiotensin-converting enzyme (ACE)-inhibitors/angiotensin II receptor antagonists (AAIIs) (ATC code: C09) if he had at least two prescriptions of such drugs during the follow-up period. Hospitalizations with cancer diagnosis and blood transfusion [ICD-9-CM code (primary or secondary discharge reasons): 9.90] required during the follow-up period were also considered.
Cost analysis
The average annual health care costs per patient, based on the total resource consumption, were assessed from the end of treatment with DAPT to the subsequent 36-month follow-up period. Only patients still alive at the end of the follow-up period were analyzed. The total resource consumption was defined as the sum of all prescribed treatments and hospital admission. Both the overall and the CV-related annualized health care resource costs were estimated. Hospitalizations inherent to CV were identified by ICD-9-CM codes: 410, 411, 413, 433, 434, 435, 436; while the treatments of interest were antithrombotic agents (ATC code: B01) and CV (ATC code: C). Cost analysis was conducted with the perspective of the Italian National Health Service (NHS). The costs are reported in Euros (€). Drug costs were evaluated using the Italian NHS purchase price. Hospitalization costs were determined using the diagnosis-related group (DRG) tariff.
Statistical analysis
Continuous variables are given as means with standard deviations (mean±SD), whereas categorical variables are shown as percentages and absolute numbers.
Cumulative incidence of CV death, composite CV endpoint, and incidence of AMI were examined using the Kaplan–Meier approach. For the composite CV endpoint, the following ICD-9-CM codes were considered: 410 (AMI), 411 (other acute and subacute forms of ischemic heart disease), 413 (angina pectoris), 433 (occlusion and stenosis of precerebral arteries), 434 (occlusion of cerebral arteries), 435 (transient cerebral ischemia), and 436 (acute, but ill-defined, cerebrovascular disease). In addition, the events that occurred within 30 days were excluded. A generalized regression model was performed to identify the associations between total health care costs (in terms of drugs and hos-pitalizations) during the follow-up period and demographic characteristics; other guidelines recommended post-AMI therapies (including beta-blocking agents, ACE inhibitors/AAIIs, and statin), AMI front/front-lateral at ID, previous hospitalizations for CV disorders, previous hospitalizations for heart failure, hospitalizations for neoplasia and blood transfusion, and antidiabetic, antihypertensive, or cardiac therapy required during the follow-up period. All analyses were performed with Stata software version 12.1 (StataCorp LP, College Station, TX, USA).
Results
The details of the study’s inclusion and exclusion criteria are shown in . A total of 2,721 patients met the inclusion criteria and were considered for the analysis (). Of these patients, 67.8% were males. The mean (SD) patient age at ID was 63.6 years (±17.3). Baseline demographic and clinical characteristics and procedural characteristics are summarized in . An anterior/anterolateral AMI was found in 27.6% of patients. Coronary angiography and PCI were performed in 60.8% and 67.5% of patients, respectively (). No patients treated with DAPT underwent DES at baseline. Less than 10% of patients (n=267) had been previously hospitalized for CV disorders ().
Figure 1 Sequential sample selection of subjects.
Abbreviations: AMI, acute myocardial infarction; DAPT, dual antiplatelet therapy; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; LHU, local health units.
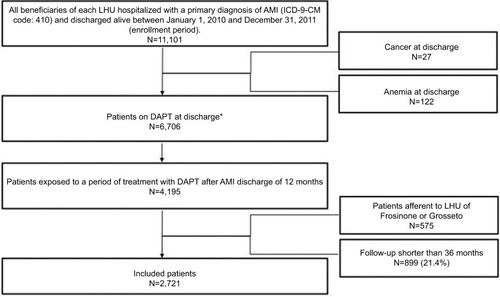
Table 1 Demographic and clinical characteristics of included patients
Patients’ characteristics and health care resource utilization during the follow-up period are shown in . Among the enrolled patients at follow-up, 56.4% had a diagnosis of systemic arterial hypertension, 45.0% heart disease, 27.0% diabetes, 7.7% cancer, and 6.7% required blood transfusion. Statins, ACE inhibitors, and beta-blocking agents were used in 91.3%, 83.5%, and 81.9% of patients, respectively.
Table 2 Health care resource utilization (in terms of hospitalizations and drugs) during the follow-up period
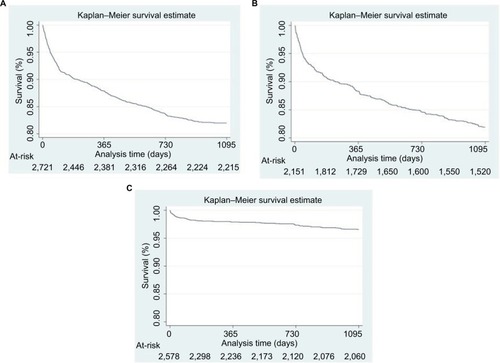
Of the 2,721 patients with AMI and after a 12-month treatment period with DAPT, 489 patients (18% of all patients) died within 36 months of follow-up (n=330 for the first year, n=114 and n=45 during the second and third years of follow-up, respectively). shows the Kaplan–Meier curve of incidence of risk of death. The survival function calculated for all-cause mortality was 0.88 at 12 months (95% CI 0.87–0.89), 0.84 at 24 months (95% CI 0.82–0.85), and 0.82 at 36 months (95% CI 0.80–0.83) (). Considering overall CV hospitalizations, about 17% of patients had this type of event within 36 months of follow-up; survival function was 0.88 at 12 months (95% CI 0.87–0.90), 0.85 at 24 months (95% CI 0.83–0.86), and 0.82 at 36 months (95% CI 0.80–0.84) (). Focusing on AMI hospitalizations only during the follow-up period, survival function was 0.98 at 12 months (95% CI 0.97–0.98), 0.97 at 24 months (95% CI 0.97–0.98), and 0.97 at 36 months (95% CI 0.96–0.97) ().
Figure 2 The Kaplan–Meier curve of incidence of risk of death.
Abbreviations: AMI, acute myocardial infarction; DAPT, dual antiplatelet therapy; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; LHU, local health unit; MI, myocardial infarction.
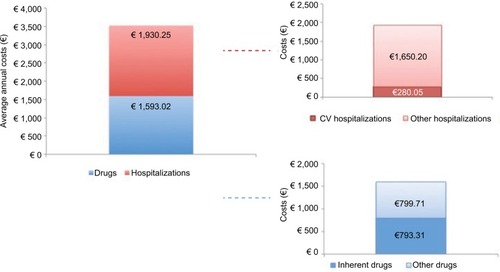
To account for all health care costs that occurred during the 36-month follow-up period, only patients still alive at the end of the follow-up period were analyzed (N=2,594). The annual average cost per patient was €3,523.27, in which €1,593.02 was for drug treatments (particularly €793.31 for therapies related to AMI such as antithrombotic agents, ATC B01 and cardiovascular, ATC C) and €1,930.25 for hospitalizations (particularly, €280.05 in relation to CV hospitalizations and €102.87 in relation to AMI hospitalizations; ).
Figure 3 The annual average cost per patient post-acute myocardial infarction after 12 months of dual antiplatelet therapy during the follow-up period.
Abbreviations: ATC, Anatomical Therapeutic Chemical; CV, cardiovascular; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification.
During the 36-month follow-up period, 63 patients had (at least) a second AMI event. The average cost of health care per patient during the 3-year follow-up period was €19,570.70 (of which €3,584.01 and €15,986.68 were attributable to drug treatments and hospitalization, respectively) (). The annual average cost per patient for these was €6,523.57, of which €1,194.67 was for drugs (particularly, €669.64 for therapies related to AMI: antithrombotic agents, ATC code: B01 and cardiovascular, ATC code: C) and €5,328.89 for hospitalizations (particularly, €3,084.14 in relation to CV hospitalizations and €2,646.31 in relation to AMI hospitalizations) ().
Figure 4 Average annual costs among patients with a second acute myocardial infarction event during the follow-up period.
Abbreviations: ATC, Anatomical Therapeutic Chemical; CV, cardiovascular; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification.
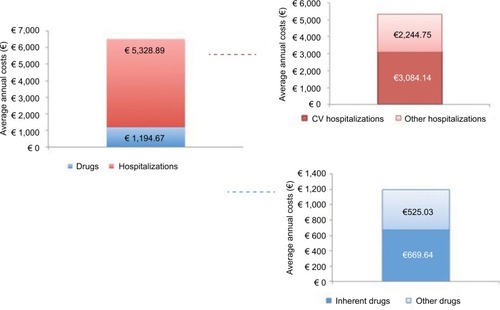
Table 3 Mean costs (€) during the 3-year follow-up period
The generalized regression model showed that a statistically significant increase in overall cost was caused by previous cardiovascular hospitalizations (+€6,098, P<0.01); previous heart failure hospitalizations (+€18,772, P<0.05); exposure to antidiabetic (+€6,275, P<0.001), antihypertensive (+€4,094, P<0.001), and cardiac (+€1,728, P=0.001) therapy (compared with no exposure); presence of hospitalizations for neoplasia (+€22,941, P<0.001); and request for blood transfusion (+€9,331, P<0.01) ().
Table 4 The overall annual direct cost (€) for treating patient post-AMI after 12 months of DAPT and still alive at the end of the follow-up period, Generalized Linear Model
Discussion
The results of this observational study suggest that among Italian patients who survived their hospitalization for an AMI and after a 12-month treatment period with DAPT, about 17% of all patients had CV events within 36 months and about 18% in the overall cohort died during the years under study. Over the past decades, medical advancements in the management of patients with AMI led to improved survival and increased life expectancy. In this regard, the incidence of AMI has declined in Western countries and 1-year post-AMI survival rates have improved, leading to growth of the stable post-MI patient population.Citation23 This trend has been matched by a growing need to better manage patients’ postdischarge and chronic care after an AMI.
In line with previous studies, our results in the real-life setting showed that patients with AMI had an average age above 63 years and were predominantly male. Patients who underwent coronary angiography and PCI at the time of admission for AMI were more than half of all enrolled patients. In addition, we identified many demographic and clinical factors associated with an increased death during the 3 years after hospital discharge for AMI and after a 12-month treatment period with DAPT. Indeed, we observed that male patients and patients who were hospitalized for cancer and patients who required a blood transfusion during the follow-up period were significantly associated with an increased risk of mortality during the 3-year post-AMI from the end of treatment with DAPT.
Pivotal studies led to guidelines recommending DAPT for up to 12 months post-ACS.Citation24 However, the optimal duration of DAPT in post-AMI patients remains uncertain yet.Citation25 Indeed, despite improved secondary prevention efforts, several prior studies have shown that stable patients with a history of prior AMI are at high risk of major adverse CV events.Citation15,Citation25,Citation26 In other words, after AMI, patients may have a persistent state that predisposes them to benefit more from DAPT.
Recently, results of randomized clinical trials have evaluated the potential benefits of long-term DAPT.Citation27,Citation28 These data suggested that prolonged DAPT may reduce major adverse cardiac events in a population considered at high risk of anti-thrombotic events with prior history of AMI.Citation15,Citation25,Citation29–Citation34 This is crucial in the context where the reduction of hospital readmissions is a health priority to improve the quality of patient care and lower health care burden.Citation15,Citation35,Citation36 It should be highlighted that high rates of hospital readmissions indicate potentially poor health care quality or inadequate management of post-discharge care. This represents a significant burden to both patients and the health care system by imposing a significant burden in terms of morbidity and mortality and generating major public health service costs.
This retrospective analysis also underscores that over a 36-month follow-up period, health care costs (in particular hospitalization costs), especially for those patients with at least a second AMI, are relevant in the real-life setting. Few data regarding long-term CV outcomes post-AMI and related health care cost of patients are currently available. Kern et al have shown that the high risk of AMI survivors who have been event free for ≥1 year remained at substantial risk of CV events and had increased health care costs for up to 5 years post-AMI.Citation37 An Italian real-world study, performed in 2008, showed that direct health care costs were at least 50% higher in patients with a recurrent ACS compared with patients without recurrent ACS.Citation38 In particular, Roggeri et alCitation38 showed that, in an Italian health care setting, the average yearly costs per patient alive at the end of the follow-up period and in treatment with DAPT were €20,554 in the group of patients with recurrent ACS and €13,303 in the group of patients without recurrent ACS, respectively.
Despite the advances in medical care following AMI, readmission risk has not declined. Given the potential impact on patients’ quality of life and health care costs, comprehensive strategies in care of patients with AMI including an optimization of risk stratification as well as novel therapeutic strategies are needed to prevent both the frequency and the adverse impact of future hospitalizations in the post-AMI period.
Our cohort of patients reflected real clinical practice, and the results must be interpreted taking into account limitations related to the observational nature of the study, based on data collected through administrative databases. Because the information concerning the severity of the pathology or the information related to the exact cause of death and rehospitalization were not available from the data set given their administrative scope, the results and conclusions of this study are limited to the analyzed population.
Conclusions
In a real-world setting in Italy, considering a 36-month follow-up period, all-cause mortality, CV events, and related health care cost (in particular hospitalizations costs) in patients hospitalized with the diagnosis of AMI undergoing a 12-month treatment period with DAPT remained relevant. This study suggests that increased efforts aimed at the prevention of recurrent AMI are warranted, as well as an accurate risk stratification in order to improve long-term outcome.
Acknowledgments
Manuscript development was supported by unconditional funding from AstraZeneca.
The Local Health Unit (LHU) study group included Samanta Sonzogni, Rossana Piccinelli, and Marco Gambera (LHU Bergamo, Bergamo, Italy), Isabella Ruggeri (LHU Milano 2, Milan, Italy), Giovanna Riccioni (LHU Roma 1, Rome, Italy), and Fabrizio Quarta (LHU Lecce, Lecce, Italy).
Disclosure
L Degli Esposti, V Perrone, C Veronesi, and S Buda are employees of Clicon s.r.l. Health, Economics & Outcomes Research. The authors report no other conflicts of interest in this work.
References
- WallentinLKristensenSDAndersonJLHow can we optimize the processes of care for acute coronary syndromes to improve outcomes?Am Heart J2014168562263125440789
- WhiteHDChewDPAcute myocardial infarctionLancet2008372963857058418707987
- SmolinaKWrightFLRaynerMGoldacreMJDeterminants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database studyBMJ2012344d8059d805922279113
- PedersenFButrymovichVKelbækHShort- and long-term cause of death in patients treated with primary PCI for STEMIJ Am Coll Cardiol201464202101210825457398
- StegPGJamesSKAtarDBadanoLPLundqvistCBAuthors/Task Force MembersESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology ESCEur Heart J201233202569261922922416
- HammCWBassandJPAgewallSESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology ESCEur Heart J201132232999305421873419
- AmsterdamEAWengerNKBrindisRG2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice GuidelinesCirculation2014130252354239425249586
- BriegerDAntithrombotic strategies to reduce adverse clinical outcomes in patients with acute coronary syndromeAm J Cardiol201211081200120622840845
- ClarkMGBeaversCOsborneJManaging the acute coronary syndrome patient: Evidence based recommendations for anti-platelet therapyHeart Lung201544214114925592204
- PiepoliMFCorràUDendalePChallenges in secondary prevention after acute myocardial infarction: A call for actionEur J Prev Cardiol201623181994200627600690
- JernbergTHasvoldPHenrikssonMHjelmHThuressonMJanzonMCardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspectiveEur Heart J201536191163117025586123
- ShoreSSmolderenKGKennedyKFHealth status outcomes in patients with acute myocardial infarction after rehospitalizationCirc Cardiovasc Qual Outcomes20169677778427780850
- HannaEBChenAYRoeMTWiviottSDFoxCSSaucedoJFCharacteristics and in-hospital outcomes of patients with non-ST-segment elevation myocardial infarction and chronic kidney disease undergoing percutaneous coronary interventionJACC Cardiovasc Interv2011491002100821939940
- RoeMTWhiteJAKaulPRegional patterns of use of a medical management strategy for patients with non-ST-segment elevation acute coronary syndromes: insights from the EARLY ACS TrialCirc Cardiovasc Qual Outcomes20125220521322373905
- ChenHYTisminetzkyMLapaneKLDecade-long trends in 30-day rehospitalization rates after acute myocardial infarctionJ Am Heart Assoc2015411e00229126534862
- RanasingheIWangYDharmarajanKHsiehAFBernheimSMKrumholzHMReadmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort studyPLoS Med2014119e100173725268126
- DunlaySMWestonSAKillianJMBellMRJaffeASRogerVLThirty-day rehospitalizations after acute myocardial infarction: a cohort studyAnn Intern Med201215711122751756
- DharmarajanKHsiehAFLinZDiagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumoniaJAMA2013309435523340637
- ArnoldSVSmolderenKGKennedyKFRisk factors for rehospitalization for acute coronary syndromes and unplanned revascularization following acute myocardial infarctionJ Am Heart Assoc201542e001352e00135225666368
- OnderGMarengoniARussoPAdvanced age and medication prescription: more years, less medications? A nationwide report from the Italian medicines agencyJ Am Med Dir Assoc201617216817226441359
- Degli EspostiLSangiorgiDBudaSDegli EspostiEScaglioneFTherapy discontinuation or substitution in patients with cardiovascular disease, switching among different products of the same off-patent active substance: a ‘real-world’ retrospective cohort studyBMJ Open2016611e012003
- Italian Medicines Agency (AIFA, Agenzia Italiana del Farmaco)Guideline for the classification and conduction of the observational studies on medicines2010 Available from: https://www.agenziafarmaco.gov.it/ricclin/sites/default/files/files_wysiwyg/files/CIRCULARS/Circular%2031st%20May%202010.pdfhttps://www.agenziafarmaco.gov.it/ricclin/sites/default/files/files_wysiwyg/files/CIRCULARS/Circular%2031st%20May%202010.pdfAccessed August 6, 2018
- Cardiovascular disease in Europe 2016: an epidemiological updateEur Heart J201637423182318327856561
- RoffiMPatronoCColletJP2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESCEur Heart J201637326731526320110
- BarillàFPellicciaFBorziMOptimal duration of dual anti-platelet therapy after percutaneous coronary intervention: 2016 consensus position of the Italian Society of CardiologyJ Cardiovasc Med201718119
- BhattDLHulotJSMoliternoDJHarringtonRAAntiplatelet and anticoagulation therapy for acute coronary syndromesCirc Res2014114121929194324902976
- BonacaMPBhattDLBraunwaldEDesign and rationale for the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin-Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trialAm Heart J2014167443744424655690
- WallentinLCommentary on the OPTIDUAL trial results: how to optimise prolonged dual antiplatelet treatment and independent randomised clinical trialsEur Heart J2016374ehv499
- BittlJABaberUBradleySMWijeysunderaDNDuration of dual antiplatelet therapy: a systematic review for the 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery diseaseJ Am Coll Cardiol201668101116113927036919
- CohenMLong-term outcomes in high-risk patients with non-ST-segment elevation myocardial infarctionJ Thromb Thrombolysis201641346447426001907
- MauriLKereiakesDJYehRWTwelve or 30 months of dual antiplatelet therapy after drug-eluting stentsN Engl J Med2014371232155216625399658
- LeeCWAhnJMParkDWOptimal duration of dual antiplatelet therapy after drug-eluting stent implantation: a randomized, controlled trialCirculation2014129330431224097439
- HelftGStegPGLe FeuvreCStopping or continuing clopidogrel 12 months after drug-eluting stent placement: the OPTIDUAL random-ized trialEur Heart J20157ehv481
- ColletJPSilvainJBarthélémyODual-antiplatelet treatment beyond 1 year after drug-eluting stent implantation (ARCTIC-Interruption): a randomised trialLancet201438499541577158525037988
- AxonRNWilliamsMVHospital readmission as an accountability measureJAMA2011305550421285430
- McIlvennanCKEapenZJAllenLAHospital readmissions reduction programCirculation2015131201796180325986448
- KernDMMellströmCHuntPRLong-term cardiovascular risk and costs for myocardial infarction survivors in a US commercially insured populationCurr Med Res Opin201632470371126709864
- RoggeriAGnaviRDalmassoMResource consumption and healthcare costs of acute coronary syndrome: a retrospective observational administrative database analysisCrit Pathw Cardiol201312420420924240551
