Abstract
Background
Brachial–ankle pulse wave velocity (baPWV) and cardio-ankle vascular index (CAVI) are indices of arterial stiffness, and several studies have used these indices. However, there is no comprehensive review of these parameters in the prognostic significance.
Methods
The aim of this study was to review the articles exploring the prognostic significance of these parameters. Articles demonstrating independent significance after multivariate analysis on the Cox proportional hazards model were defined as “successful.” The success rate was compared using Fisher’s exact test. In addition, multivariate logistic regression analysis was performed to explore the independent determinants of the success of prognostic prediction.
Results
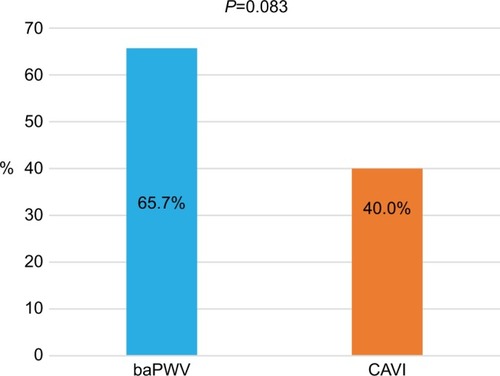
The success rate of the baPWV articles (65.7% [46/70]) tended to be higher than that of the CAVI articles (40.0% [6/15]; P=0.083). Multivariate analysis demonstrated that log (number of patients) (OR 11.20, 95% CI 2.45–51.70, P=0.002) and dialysis population (OR 0.28, 95% CI 0.08–0.94, P=0.039) were positive and negative independent determinants of the success of prognostic prediction, respectively. In addition, after redefining two studies as the absence of arteriosclerosis obliterans (ASO) exclusion, baPWV (OR 3.36, 95% CI 0.86–13.20, P=0.083) and the existence of exclusion criteria of ASO (OR 3.08, 95% CI 0.96–9.93, P=0.060) exhibited statistical tendency in the multivariate analysis.
Conclusion
This study demonstrated that the number of study participants and dialysis population were the independent determinants of the success of prognostic prediction. This study also showed the importance of exclusion criteria of ASO when using these indices. In addition, a prospective large-scale study to confirm the superiority in the prognostic prediction of these indices is warranted.
Introduction
The burden of managing atherosclerotic diseases is increasing globally as economic development continues. Pulse wave velocity (PWV) and ankle–brachial index (ABI) have long been used to quantify arteriosclerosis and atherosclerosis,Citation1,Citation2 and the clinical significance of each has been established.Citation3–Citation5 Carotid–femoral PWV (cfPWV) is a representative marker of arterial stiffness, and several meta-analyses have demonstrated its independent prognostic predictability.Citation6–Citation8 Vascular Profiler (VP; BP-203RPE, VP-1000, and VP-2000 series, Japanese product name “form”) and VaSera (VS; VS-1000, VS-1500, VS-2000, and VS-3000 series) were first sold in Japan at the end of 1999Citation9,Citation10 and in the first half of 2002,Citation11,Citation12 respectively, which were new devices that can simultaneously measure brachial–ankle PWV (baPWV) and ABI. The specifications of VS changed to measure cardio-ankle vascular index (CAVI) and ABI in the first half of 2004, and it was continued to be sold.Citation13,Citation14 Several English-language articles about both devices have been published. The first article discussing the prognostic predictability of the baPWV was published in 2005,Citation15 whereas the first article reporting that of the CAVI was published in 2009.Citation16 The number of articles detailing the prognostic predictability of baPWV rapidly increased after 2012, nearing 40 at the end of 2014.Citation17 Moreover, three meta-analyses and one rapid communication article using the data derived from one meta-analysis were also published.Citation18–Citation21 As information accumulated, the baPWV threshold of 18 m/s was set as “high risk,”Citation3,Citation22,Citation23 whereas that of 14 m/s was set as “middle risk”Citation22 in the related guidelines. Five articles reported the prognostic significance of baPWV and CAVI in the same population.Citation24–Citation28 However, no studies have comprehensively discussed the differences in prognostic predictability among those indices.Citation29 Therefore, this study aimed to identify articles that researched the prognostic predictability of both indices and compare the success rate wholly and in each category. Moreover, this review also aimed to explore the independent predictors of the success of prognostic prediction.
Methods
Identifying and defining articles
The concept and measurement method of baPWV and CAVI are available elsewhere.Citation10,Citation14,Citation22 The articles identified in this study were written in English (at least in the abstract) and indexed to PubMed or released publicly on the Internet. Each was obtained by the end of April 2018. shows the selection process of the objective studies. The PubMed search was performed using the related keywords such as “pulse wave velocity,” “brachial–ankle pulse wave velocity,” “cardio-ankle vascular index,” “arterial stiffness,” and “ankle–brachial index.” Longitudinal studies that discussed the prognostic predictability of both indices were identified. End points included all-cause mortality (ACM), cerebrovascular–cardiovascular mortality (CCVM), cerebrovascular–cardiovascular events (CCVE), ischemic heart disease (IHD), major adverse cardiac events, and heart failure. When the other end points such as peripheral arterial disease (PAD) were included, they were explained additionally (–). Studies of functional prognosis such as a decline in cognitive function, kidney function, or activities of daily living were not included. Three meta-analyses and one rapid communication article detailing prognostic predictability of baPWV were excluded.Citation18–Citation21 Longitudinal studies that did not include baPWV or CAVI as a prognostic variable were also excluded.Citation30–Citation37
Figure 1 A flowchart of identifying prognostic studies of baPWV and CAVI articles.
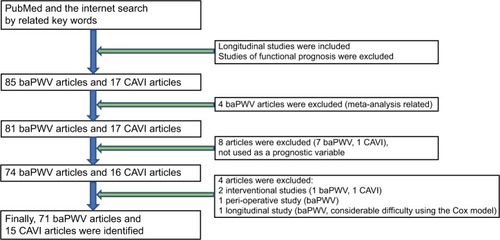
Table 1 A summary of the prognostic predictability of all examined baPWV and CAVI articles
Table 3 Details of the articles in which the prognostic predictability of baPWV and CAVI was analyzed in the same cohort
Moreover, among the interventional studies in which those indices were measured, those that did not research their prognostic significance were also excluded because of the discrepancy in the research purpose.Citation38,Citation39 One study reporting perioperative adverse events was also excluded.Citation40 Furthermore, one study that demonstrated the significance of baPWV using a Kaplan–Meier analysis (log-rank test, P<0.0001) was excluded because of considerable difficulty in adopting the Cox proportional hazards model, as the Kaplan–Meier curves apparently showed nonproportional changes in the event rates.Citation41 Finally, a total of 71 baPWV articles and 15 CAVI articles were identified. The identified studies were categorized according to patient characteristics and the presence or absence of the clarified exclusion criteria of lower extremity (LE)-arteriosclerosis obliterans (ASO)/PAD. Any criteria such as “other vascular diseases” were not defined as the exclusion criteria of LE-ASO/PAD in this study. The studies demonstrating independent prognostic predictability of those indices on a multivariate Cox proportional hazards model or multivariate logistic regression model were defined as “successful.” The studies showing significance on only Kaplan–Meier analysis (log-rank test) and/or not demonstrating statistical significance on a multivariate Cox proportional hazards model were defined as “failed.” Comparisons between baPWV and CAVI were performed in all included articles, in the presence or absence of the clarified exclusion criteria of LE-ASO/PAD, in the population of dialysis (hemodialysis and peritoneal dialysis) or other than dialysis, and in the articles discussing both indices in a same cohort. However, one article studying both baPWV and CAVI in the same patient cohort did not describe the prognostic significance of baPWV as a primary end point. As such, that study was excluded from the statistical analysis as a baPWV article because the independent prognostic significance of baPWV for the primary end point was not clarified.Citation28 Moreover, because of the relatively ample number of baPWV articles, the studies with or without the clarified exclusion criteria of LE-ASO/PAD only among baPWV articles were compared to confirm the effect on success rate. Furthermore, multivariate logistic regression analysis was performed to explore the independent factors of the success of prognostic prediction.
Statistical analyses
Statistical analyses were performed using EZR (EZR on R commander version 1.33, September 1, 2016).Citation42 All comparisons between groups were performed using Fisher’s exact test. However, a statistical analysis was not performed among the five articles that simultaneously studied baPWV and CAVI because of the too small sample and of the heterogeneity in the condition.Citation24–Citation28 Moreover, logistic regression analysis was performed to explore the independent determinants of the success of prognostic prediction (success =1, failure =0). The following covariates were analyzed in the univariate analysis: baPWV or CAVI (baPWV =1, CAVI =0), presence of the clarified exclusion criteria of LE-ASO/PAD (yes =1, no =0), dialysis population (yes =1, no =0), follow-up period (years), age (years), male gender (%) in the study cohort, and log-transformed number of patients (log NoP). The number of patients was log transformed because of skewed distribution. In this analysis, the mean values of the patients’ age and follow-up years were primarily used, and if not available, median values were used. The value of the mean/median patient age was missing in two studies.Citation43,Citation44 The proportion of gender was also missing in one study.Citation44 Nevertheless, the analysis was performed without these missing data. The covariates whose P-value was ≤0.2 in the univariate analysis were entered into the multivariate model. Furthermore, reanalysis was performed by redefining two studies as the absence of LE-ASO/PAD exclusion,Citation27,Citation45 because these studies were considered to insufficiently exclude LE-ASO/PAD patients (symptomatic PAD only). P-values of ≤0.05 were considered statistically significant, whereas P-values of 0.05<P≤0.10 were considered to have a statistical tendency.
Results
All articles
A total of 70 articles on baPWVCitation15,Citation24–Citation27,Citation43–Citation107 and 15 articles on CAVICitation16,Citation24–Citation28,Citation108–Citation116 were identified. presents a summary of these articles. The success rate of independent prognostic predictability of the baPWV articles (65.7% [46/70]) tended to be higher than that of the CAVI articles (40.0% [6/15]; P=0.083; ).
Articles clarifying the exclusion criteria of LE-ASO/PAD
presents the detailed information about the articles in this category. In this category, the success rates of baPWV and CAVI articles were 75.9% (22/29) and 57.1% (4/7), respectively (P=0.37). After excluding two studies that insufficiently excluded LE-ASO/PAD patients,Citation27,Citation45 the success rates of baPWV and CAVI articles were 81.5% (22/27) and 66.7% (4/6), respectively (P=0.58).
Table 2 Detailed information about baPWV and CAVI articles in which ASO and/or PAD was excluded from the analysis
Articles lacking or not clarifying the exclusion criteria of LE-ASO/PAD
In this category, the success rates of baPWV articles and CAVI articles were 58.5% (24/41) and 25% (2/8), respectively (P=0.12). After adding two studies that insufficiently excluded LE-ASO/PAD patientsCitation27,Citation45, the success rates of baPWV articles and CAVI articles were 55.8% (24/43) and 22.2% (2/9), respectively (P=0.14).
Population other than dialysis (hemodialysis and peritoneal dialysis)
In this category, the success rate of baPWV articles was 71.43% (41/57) which was similar to that of CAVI articles (54.5% [6/11]; P=0.30).
Studies of dialysis population only
In this category, the success rate of baPWV articles was 38.5% (5/13) which was similar to that of CAVI articles (0% [0/4]; P=0.26).
Studies comparing baPWV and CAVI in the same cohort
presents the detailed information of the five articles in this category. Among the baPWV articles, the result was one success, two studies with statistical significance in the log-rank test, one failure, and one without a clarified result of the primary end point. Among the CAVI articles, the result was two successes and three failures. In the study that presented the success of baPWV, CAVI showed a statistical tendency in the Kaplan–Meier analysis (log-rank test, P=0.06). However, the trend disappeared after the adjustment for age, gender, and diabetes on the multivariate Cox proportional hazards model (P=0.49).Citation25 The two studies that showed a statistical significance of baPWV in the Kaplan–Meier analysis (log-rank test) did not reveal significance for CAVI.Citation24,Citation27 In the study that demonstrated the success of CAVI and failure of baPWV, CAVI was analyzed with respect to the presence or absence of improvement for ≥6 months (persistently impaired CAVI). However, the baPWV’s raw value at the second occasion of the measurement was analyzed.Citation26 In a study in which the baPWV result was defined as “not clarified,” the prognostic significance of baPWV in the multivariate Cox proportional hazards model analysis on the primary end point was not described. However, the prognostic significance of CAVI (not baPWV) on the secondary end point of nonfatal stroke was presented.Citation28
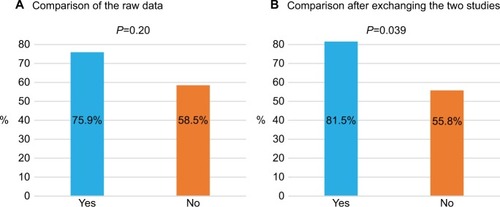
Comparison of baPWV articles according to the presence or absence of the clarified exclusion criteria of LE-ASO/PAD
The success rate of the articles in the presence of these criteria (75.9% [22/29]) was similar to that in their absence (58.5% [24/41]; P=0.20; ). However, after redefining two studies as the absence of LE-ASO/PAD exclusion,Citation27,Citation45 the success rate of the articles in the presence of these criteria (81.5% [22/27]) was significantly higher than that of the articles in the absence (55.8% [24/43]; P=0.039; ).
Figure 3 The success rate of baPWV articles according to the presence of exclusion criteria of LE-ASO/PAD. (A) Comparison of the raw data. (B) Comparison after exchanging the two studies.
Multivariate logistic regression analysis to identify the independent determinants for the success of prognostic prediction
presents this result. In the univariate analysis, log NoP (P=0.0006) and dialysis population (P=0.005) were significantly associated with the success of prognostic prediction, whereas baPWV and exclusion of LE-ASO/PAD showed a statistical tendency (P=0.071, P=0.076, respectively). In the multivariate analysis, log NoP (OR 11.20, 95% CI 2.45–51.70, P=0.002) and dialysis population (OR 0.28, 95% CI 0.08–0.94, P=0.039) were identified as the independent determinants of the success of prognostic prediction.
Table 4 Logistic regression analysis exploring the independent determinants of the success of prognostic prediction
summarizes the result after redefining two studies as the absence of LE-ASO/PAD exclusion.Citation27,Citation45 In the univariate analysis, exclusion of LE-ASO/PAD (P=0.01), dialysis population (P=0.005), and log NoP (P=0.0006) were significantly associated with the success of prognostic prediction, whereas baPWV showed statistical tendency (P=0.071). In the multivariate analysis, log NoP and dialysis population were the statistically significant factors (for log NoP: OR 9.04, 95% CI 1.90–43.00, P=0.006; for dialysis population: OR 0.27, 95% CI 0.07–0.96, P=0.043). However, baPWV and the exclusion of LE-ASO/PAD showed statistical tendency in the success of prognostic prediction (for baPWV: OR 3.36, 95% CI 0.86–13.20, P=0.083; for the exclusion of LE-ASO/PAD: OR 3.08, 95% CI 0.96–9.93, P=0.060).
Table 5 Logistic regression analysis exploring the independent determinants of the success of prognostic prediction after exchanging the studies excluding patients with only symptomatic PAD
Discussion
Overview
To the best of our knowledge, this study is the first to comprehensively review the prognostic predictability of baPWV and CAVI. The current number of English articles using the indices of VP and VS is approximately 1,800 and 550, respectively.Citation117 The ratio of articles studying the prognostic significance of these parameters did not differ significantly (baPWV 70/1,800; CAVI 15/550, P=0.24). There were five articles that simultaneously studied prognostic significance of baPWV and CAVI in a same patient population. The success rate of baPWV articles tended to be higher than that of CAVI articles (65.7% vs 40.0%, P=0.083). Dialysis population and log NoP were the independent determinants for the success in the multivariate logistic regression analysis (). Moreover, after redefining two studies as the absence of exclusion of LE-ASO/PAD,Citation27,Citation45 the success rate in the presence of these criteria was significantly higher than that in the absence of these criteria among the baPWV articles only (81.5% vs 55.8%, P=0.039). Furthermore, multivariate logistic analysis showed that baPWV and exclusion of LE-ASO/PAD had a statistical trend on the success of prognostic prediction (P=0.083, P=0.060, respectively). The multivariate analysis also showed that the effects of dialysis population and log NoP were attenuated, although these parameters were still significant (P=0.043, P=0.006, respectively; ). Therefore, log NoP had the strongest power on the success of prognostic prediction among the articles investigated in this study. Actually, the most studies involving >1,000 participants were successful in the prognostic prediction.Citation47,Citation48,Citation52,Citation53,Citation55,Citation58,Citation68,Citation88,Citation93,Citation97,Citation103,Citation107,Citation109 These studies mostly used baPWV, and one study used CAVI.Citation109 However, the largest study of CAVI involving >2,000 participants failed.Citation110 Moreover, this review confirmed that the dialysis population (mostly hemodialysis) was a negative determinant of the success of prognostic prediction of the baPWV and CAVI. This is not surprising because the incidence of having false-negative LE-ASO/PAD is high even if the exclusion criteria are defined as ABI of ≤0.9 in the hemodialysis population. Age, proportion of male gender, and follow-up period in the study population had no effect on the success of baPWV and CAVI in the prognostic prediction. In general, age and gender affect the progression of arterial stiffness and thus prognosis.Citation118 However, the result of this study is plausible because this study explored the key factors for the success of prognostic prediction of baPWV and CAVI, not investigating the factors affecting arterial stiffness. This study also confirmed that more than half of the articles did not clarify the exclusion criteria of LE-ASO/PAD or did not exclude patients with LE-ASO/PAD when using baPWV and CAVI in the prognostic studies.
baPWV
Main findings
The success rate of baPWV articles (65.7%) tended to be higher than that of CAVI articles (40.0%) (P=0.083). This difference may be partly caused by the number of the study population. The success rate of baPWV articles (75.9%) was similar to that of CAVI articles (57.1%) in the studies clarifying the exclusion criteria of LE-ASO/PAD. Among the 29 baPWV articles that had the patient exclusion criteria of LE-ASO/PAD, seven articles failed to prove prognostic significance of baPWV. Among the seven articles, two excluded those patients only with symptomatic PAD.Citation27,Citation45
The former study consisted of patients with multiple risk factors for cardiovascular disease (CVD), and the mean ABI in this cohort was 1.01±0.17 (SD). Therefore, patients with an ABI of ≤0.9 existed at high probability. In this study, baPWV, but not CAVI, showed statistical significance in the Kaplan–Meier analysis. Nevertheless, its significance was lost after multivariate adjustment by the Cox model including ABI as a covariate, and the cutoff ABI of 1.04 was selected as an independent predictor.Citation27 Moreover, the mean baPWV and CAVI values of both sides were used in the analysis. This condition meant that the decreased baPWV or CAVI on the side with asymptomatic PAD would lower the mean parameter. However, in reality, a patient was considered to have a high-risk prognosis.Citation5,Citation22,Citation117,Citation119 Therefore, the risk of a patient with asymptomatic PAD who was considered at equivalently high risk as a patient with symptomatic PAD was considerably underestimated by the falsely lowered baPWV or CAVI.Citation27
In the study by Lau et al,Citation45 the study cohort included patients with diabetes vintage of 15.2±7.5 years. Thus, the high probability of a falsely overestimated ABI due to arte-rial calcification in the lower limbs was considered.Citation5 The mean ABI of both sides, 1.1±0.1, was used in the analysis, and the high probability of asymptomatic LE-ASO/PAD was considered. Furthermore, the mean baPWV of both sides was also used; as such, a similar phenomenon observed in the study by Kusunose et al would be most likely.Citation27 As a result, no prognostic significance of baPWV was proven in this study.Citation45 Thus, at least when utilizing baPWV and CAVI as prognostic predictors that include the lower-limb arteries in the measuring path, these findings imply that the exclusion of symptomatic PAD is insufficient. Therefore, redefining of these two articles and the reanalysis were performed, and this change presented the statistically higher success rate in the presence of exclusion criteria of LE-ASO/PAD than that in the absence of the criteria among the baPWV articles. At the same time, baPWV and exclusion of LE-ASO/PAD showed a statistical tendency in the multivariate logistic model ().
However, within the articles that clarified the exclusion criteria using ABI (≤0.9) or an expression of LE-ASO/PAD exclusion, the other five studies did not prove an indepen-dent prognostic significance of baPWV. The cohorts of these studies were as follows: two patients with IHD,Citation26,Citation74 of the patients receiving hemodialysis,Citation80 one of the patients with chronic kidney disease stage 3–5,Citation83 and one of an outpatient population with a 78% incidence of diabetes.Citation86 Thus, these studies were conducted in population that were still very likely to include patients with LE-ASO/PAD (false-negative LE-ASO/PAD), even if the exclusion criterion was set at ABI ≤0.9. Therefore, the reason for failure in these five studies is considerably similar to that in the two studies.Citation27,Citation45 The reason why ABI and/or (false-negative) LE-ASO/PAD is a stronger indicator of prognosis is given in the following section.
Prognostic significance of ABI is much stronger than that of baPWV without sufficient exclusion of LE-ASO/PAD
In the hemodialysis cohort that did not exclude patients with LE-ASO/PAD, it was already demonstrated that a high baPWV (the top quartile of baPWV ≥23.6 m/s) lost prognostic significance after multivariate adjustment including ABI as one of the covariates using the Cox model, even though a high baPWV showed significance in the Kaplan–Meier analysis.Citation46 This is because ABI, which assesses LE-ASO/PAD as a more severe disease, is a considerably stronger prognostic indicator than baPWV. In the same study, baPWV showed independent prognostic significance after the exclusion of patients with an ABI of <0.9. Nevertheless, patients with a borderline ABI of 0.90–0.99 and patients with a high ABI of ≥1.3 also showed independent prognostic significance. Furthermore, patients with a low normal ABI of 1.00–1.09 showed a statistical tendency or a close value as a prognostic indicator (P=0.113 for ACM, P=0.086 for CCVM after adjustment).Citation46
In another study of hemodialysis patients evaluating the prognostic significance of ABI but not using baPWV,Citation120 patients with an abnormal ABI of <0.9 and those with a borderline ABI of 0.90–0.99 showed the worst prognosis. However, in the present study, those with a high ABI of ≥1.3 and even those with a low normal ABI of 1.00–1.09 showed significantly worse prognosis than those with a reference ABI of 1.10–1.29 (in those with a low normal ABI of 1.00–1.09, an HR of 1.92% and 95% CI of 1.02–3.59 for ACM and an HR of 2.82% and 95% CI of 1.22–6.54 for CCVM after multivariate adjustment using the Cox proportional hazards model). In the report published in 2003, Ono et alCitation120 mentioned that those with an ABI of 0.9–1.1 as well as those with an abnormal ABI should be carefully monitored in the hemodialysis population.
Moreover, in a study of a hemodialysis cohort that evaluated the prognostic predictability of ABI in ACM, the best cutoff ABI of 1.1 was demonstrated by a receiver operating characteristic (ROC) curve analysis (area under the ROC curve to predict mortality, 0.79; sensitivity, 0.90; specificity, 0.62).Citation121 This significance was maintained after multivariate analysis using the Cox model. In the studies that evaluated the diagnostic ability of ABI compared to imaging modalities or clinical symptoms in patients on hemodialysis, an ABI threshold of 1.01–1.10 was mainly reported.Citation122–Citation124 Ohtake et alCitation123 suggested raising the ABI cutoff to 1.1 in patients on hemodialysis. In a cohort of patients with diabetes, significant HRs and P-values in prognostic predictability (ACM and CCVM) were reportedly similar between those with an abnormal ABI of ≤0.9 and those with a borderline ABI of 0.91–0.99 (both HRs of about 2.0, significant) compared to those with normal ABI of 1.00–1.4.Citation125 Moreover, in a study of a cohort with multiple cardiovascular risk factors and a history of CVDs, those with a borderline ABI of 0.91–0.99 showed significantly higher HRs in ACM (HR 2.27, P=0.005) and CCVM (HR 3.47, P=0.003) than those with a normal ABI of 1.00–1.4.Citation126
Among the studies of patients with IHD, one report showed the independent prognostic predictability of a border-line ABI of 0.91–0.99,Citation127 whereas another study demonstrated the best cutoff ABI of 1.057 as an independent prognostic predictor.Citation128 In contrast, in the Hisayama study involving a general population, those with abnormal ABI of ≤0.9 clearly showed independent prognostic predictability in CCVE (HR 2.40, P=0.02). However, those with a borderline ABI of 0.91–0.99 did not show any difference compared to those with a normal ABI of 1.0–1.4, and the result was virtually the same even in the Kaplan–Meier analysis.Citation129 All the ABI values in the study mentioned earlier were measured using VP. The information described earlier indicated that there are frequent cases in which those with LE-ASO/PAD still exist after excluding those with an ABI of ≤0.9 and that a borderline or low normal ABI has stronger prognostic significance than baPWV depending on the cohort or at least has confounding power to weaken the prognostic significance of baPWV in the multivariate analysis. Moreover, it is also plausible that the existence of the patients with false-negative LE-ASO/PAD weakens the prognostic significance of baPWV even if ABI is not included in the multivariate model, because the prognostic risk of such a patient cannot be appropriately assessed by baPWV even if the higher baPWV is used.Citation117 Simply, in other words, the existence of the false-negative LE-ASO/PAD weakens the prognostic significance of baPWV (and also CAVI) anyway regardless of the ABI included in the multivariate model or not.
Appropriate settings when evaluating baPWV and CAVI
Therefore, to set the exclusion criteria of LE-ASO/PAD to appropriately assess baPWV as a prognostic indicator, the cutoff ABI of ≤0.9 is sometimes insufficient, or it would be necessary to increase the ABI value in such a case. This is one of the limitations when using baPWV (and also CAVI). As such, among the seven studies that failed to show the prognostic significance of baPWV,26,27,45,74,80,83,86 if the exclusion criteria of LE-ASO/PAD were defined to include the upstroke time (UT)Citation130 and/or percent mean arterial pressure (%MAP),Citation131 the baPWV success rate would be higher. This might be the same for CAVI. In contrast, several studies showed the independent prognostic significance of baPWV and CAVI without the clarified exclusion criteria of LE-ASO/PAD or without LE-ASO/PAD exclusion. For this reason, some studies might have excluded LE-ASO/PAD using the cutoff ABI of ≤0.9, but it might not be just precisely described in the articles (it is very likely in three articles of reference number of 56, 68, and 111 for some reasons). These studies might also be performed in the cohort with a low frequency of LE-ASO/PAD even if LE-ASO/PAD was not excluded. It is also plausible that the independent prognostic predictability of baPWV or CAVI was proven incidentally in the relationship of the covariates included in the multivariate model.
In reality, two baPWVCitation56,Citation68 and one CAVICitation111 studies, which were defined as not clarifying exclusion criteria of LE-ASO/PAD, were considered most likely to exclude those with LE-ASO/PAD and/or ABI of ≤0.9. It is almost certain according to the data of ABI (ABI=1.13±0.00 [standard error], the number of patients was 338),Citation56 the context of the patient exclusion criteria and the end point,Citation111 and the information of other studies of their institutions.Citation58,Citation68 Therefore, reanalysis was performed. Among the baPWV articles, the success rate of the articles in the presence of these criteria (82.8% [24/29]) was significantly higher than that of the articles in the absence of these criteria (53.7% [22/41]; P=0.020). In the multivariate logistic regression analysis (Table S1), exclusion of LE-ASO/PAD emerged as an independent predictor of the successful prognostic prediction (P=0.022). The P-value of baPWV improved (from 0.083 to 0.059).
CAVI
Main findings
The success rate tended to be lower in studies of CAVI than in those of baPWV (40% vs 65.7%, P=0.083). Moreover, all four studies of a hemodialysis cohort failed to show prognostic significance.Citation24,Citation25,Citation108,Citation116 In three of the four studies, LE-ASO/PAD was not excluded.Citation24,Citation106,Citation114 The prognostic significance of CAVI was also definitely weakened by uncertainty or absence of the exclusion criteria of LE-ASO/PAD. The relatively small number of the participants in the hemodialysis studies might also affect the outcome. However, among the studies clarifying the exclusion criteria of LE-ASO/PAD, the success rate was 57.1% (4/7), which was lower than that for studies of baPWV (75.9%), although this was not statistically significant. Moreover, four of the six studies that showed the independent prognostic significance of CAVI implied that the statistical power was not very strong from the aspect of P-values despite the studied cohorts not being very small (P=0.039 for 1,003 patients; P=0.029 for 300 patients; P=0.049 or<0.05 for 626 patients; P=0.04 for 400 patients).Citation109,Citation111–Citation113 Furthermore, the largest study of CAVI involving 2,106 Caucasian participants with metabolic syndromes failed. In this study, there were no clarified criteria of LE-ASO/PAD. Nevertheless, the subjects were middle aged (54±6 years), and those with the previous history of CVDs were excluded. Thus, the prevalence of LE-ASO/PAD was considered low in this cohort. In the present study, CAVI showed statistical significance in the Kaplan–Meier analysis and the univariate Cox model. However, in the multivariate analysis, this significance was lost, and age and gender were selected as the independent prognostic predictors.Citation110 These phenomena are similar to that of the hemodialysis study by Kato et al.Citation25 In Kato’s study, the statistical tendency of CAVI was lost after the adjustment of age, gender, and diabetes in the multivariate Cox proportional hazards model.
Therefore, considering the whole information described earlier, the prognostic power of CAVI may be weaker than that of baPWV. The possible reasons are described in the following section.
Factors possibly affecting prognostic predictability of CAVI
CAVI is a product of PWV adjusted by blood pressure, and its concept is derived from the stiffness parameter β.Citation14 In adopting the concept of the stiffness parameter β on heart–ankle PWV (haPWV), the equation is as follows: β= CAVI = 2ρ·PP−1· Ln(SBP/DBP)· haPWV,Citation2 where ρ is the blood density, PP is the pulse pressure, and Ln is a natural logarithm.Citation14 As a result of this method, CAVI is considered less dependent on blood pressure than baPWV or independent from blood pressure.Citation14,Citation132 However, the appropriateness of using only brachial blood pressure as the representative of the haPWV measuring path, as well as the independence of blood pressure, has been controversial.Citation132–Citation141 A few authors in these studies clearly denied the blood pressure independence of CAVI.Citation135,Citation138,Citation139 To calculate haPWV, the pulse transit times between the brachial–ankle and the heart–brachial are required. The equation of haPWV is as follows: haPWV = Lha/Tha = Lha/(Tba + Thb), where Lha is the length between the heart and the ankle, Tha is the pulse transit time between the heart and the ankle, Tba is the pulse transit time between the brachium and the ankle, and Thb is the pulse transit time between the heart and the brachium.Citation14 However, measuring Tha or Thb is virtually impossible. Therefore, it is substituted with the time interval between the onset of the second heart sound and that of the dicrotic notch (DN) on the brachial pulse wave form (Thb ≒ T¢hb = TII–DN). Nevertheless, one study reported that this method using volume plethysmography could induce a 50% reduction in CAVI.Citation142 The timings of the second sound and the DN themselves could be falsely determined depending on the patient’s condition, especially in cases of valvular heart diseases. Furthermore, the blood density ρ is considered constant in the VS device, but this is not always constant in vivo. Kato et alCitation25 pointed out the change in blood density of patients on hemodialysis.Citation143 Moreover, we must recognize the risk of using the brachial blood pressure of the upper extremity (UE)-ASO in those on hemodialysis. Patients on hemodialysis reportedly have falsely elevated ABI to a certain extent because of UE-ASO on the contralateral side of the hemodialysis access, and its frequency was reportedly about 10% in the Japanese hemodialysis patients.Citation117,Citation144 In all four hemodialysis cohort studies that failed to show the prognostic significance of CAVI, no difference in CAVI was found between those with and without the primary end point (before adjustment). This might be caused by the absence of exclusion criteria of LE-ASO/PAD in three of the studies. Nevertheless, a decreased brachial blood pressure due to UE-ASO and error in the pulse transit time (T¢hb and Tba) might have partly affected the results. We must also recognize that a false measurement of ABI and baPWV in the cases of UE-ASO in patients on hemodialysis would affect the prognostic predictability of baPWV.Citation117
With respect to blood pressure and ABI measurement, we must recognize that there are a few minor differences between VP and VS. VP synchronizes the timing of SBP determination to make it simultaneous. In contrast, a blood pressure measurement using VS is basically performed through the sequential method (from the right side to the left side). Thus, for determining SBPs in the arms and ankles, the difference in measurement time is considered more likely to occur with VS than with VP. In the statement document of the American Heart Association published in 2012 regarding the measurement and interpretation of ABI, two studies reported that the left ABI measured using the Doppler method was significantly lower (0.03) than the right ABI.Citation5 In a meta-analysis of the risks of inter-arm blood pressure differences, a significantly increased relative risk of inter-arm difference (ie, difference in SBP ≥10 mmHg) was demonstrated in the sequential method compared to the simultaneous method.Citation145 The difference in the risk of the inter-arm blood pressure difference mentioned earlier may affect the individual ABI and the prevalence of LE-ASO/PAD (it could also change the excluded patients) and may affect the brachial blood pressure to be used in the CAVI equation. Furthermore, as a fundamental issue, we may have to ensure that the blood pressure measured by the oscillometric method is used in the CAVI equation of VS. Blood pressures measured by the oscillometric method are reportedly lower than those measured by the invasive method (internal arterial pressure).Citation146–Citation148 This implies that, even if it is theoretically correct to use the brachial blood pressure as a representative value of the systemic arteries in the CAVI equation, because it is an oscillometric method anyway, a discrepancy inevitably exists regardless of the device used. It should also be recognized that the invasive method is not always perfect.
Difference between CAVI and baPWV
Various factors that would affect the prognostic significance of CAVI were discussed earlier. The correlation between baPWV and haPWV, which is a parameter in the CAVI equation, is reportedly very high in healthy male individuals of the general population (r=0.92 for baPWV and haPWV in the right side, n=135; mean, 59 years old).Citation149 In contrast, the blood pressure dependence of CAVI is reportedly weaker than that of baPWV.Citation14,Citation132 Moreover, several studies have shown superior associations with other atherosclerotic parameters of CAVI to that of baPWV.Citation150,Citation151 However, we may have to recognize that the characteristics of PWV, which is considered to natively possess prognostic significance,Citation6–Citation8,Citation18–Citation21 might be affected by various factors in the measurement and the equation of CAVI as pointed out earlier. Furthermore, we suppose that CAVI is superior to baPWV as an index of arterial wall stiffness. Nevertheless, we may also have to recognize that the superiority for quantifying arterial wall stiffness itself is a different issue from superiority as a prognostic predictor. We may also have to recognize a study that showed the superiority of baPWV to CAVI in terms of reproducibility in the Caucasian population, although the statistical difference was not described.Citation152
Perspective
Necessity of more prognostic studies of CAVI
Three meta-analyses of the prognostic significance of baPWV have already been published,Citation18–Citation21 and the cutoff baPWV of 18 m/s is largely consistent.Citation3,Citation21,Citation22 No published meta-analysis has examined the prognostic significance of CAVI probably due to the shortage of reports. Thus, further studies are required. The large-scale CAVI-J study that aims to validate the prognostic significance of CAVI is currently in progress, and its results are pending.Citation153 A few large longitudinal studies in Western countries are also in progress. According to the MARK study in Spain, CAVI was significantly and positively associated with an index of physical functional quality of life (standardized physical component: the higher, the better), ABI was also significantly and positively associated (both after multivariate adjustment), and baPWV was not correlated.Citation154 Moreover, baPWV and CAVI showed similar correlations with carotid atherosclerosis indices.Citation155 This result is similar to that of the Japanese hemodialysis study.Citation143 In the comparison of cfPWV and CAVI according to the Advanced Approach to Arterial Stiffness study of 18 European countries, age–gender adjustment of cfPWV but not CAVI was higher in the patients with metabolic syndrome than those without.Citation141,Citation156 A similar result was also reported in Japan. In the present study, baPWV but not CAVI was significantly higher in the patients with meta-bolic syndromes than those without among the middle-aged health checkup population.Citation157 It will be interesting to note whether the same difference in study results as that obtained in the Japanese cohorts is demonstrated.Citation136,Citation154,Citation156
Necessity of rigorous patient exclusion criteria
When using baPWV and CAVI, especially in a study cohort consisting of patients with severe conditions, the patient exclusion criteria should be more rigorous; at least, LE-ASO/PAD definition of ABI ≤0.9 should be used. Arrhythmia and aortic valve disease should be used as well.Citation117 In addition, UE-ASO should be considered in patients receiving hemo-dialysis.Citation117,Citation144 Especially, regarding the exclusion criteria of LE-ASO/PAD in the study of prognostic significance, as the first step, we can set the best ABI cutoff by ROC curve analysis in the prognostic prediction. The analysis of baPWV and CAVI can be permitted only in patients with an ABI that exceeds the best cutoff. When using a simple cutoff such as ABI ≤0.9 or ABI ≤0.99, the heart rate-adjusted UTCitation130 and %MAPCitation86,Citation131 should also be included in the criteria.Citation158 Moreover, the use of a higher baPWV and CAVI on either side is favorable.Citation22,Citation119 Especially, when using the mean or designated side of those indices, the masked LE-ASO/PAD must be thoroughly excluded.
Adopting the concept of stiffness parameter β and other methods of blood pressure adjustment
The concept of stiffness β and CAVICitation14 can be applied to other devices that measure PWV and blood pressure if we neglect the “a” and “b” constants, which are used to convert the slope and the coordinate of the CAVI equation in VS. We can also use a general constant for the blood density ρ. In fact, a few studies have adopted this idea using VP.Citation159 However, this is not exactly the same as the CAVI measured by VS. Nevertheless, a baPWV-derived CAVI, the brachial–ankle vascular index, is comparable to the baPWV, and this conversion is quite easy to make. Therefore, a reanalysis comparing both indices in the previously published studies would be interesting. If necessary, haPWV can also be measured by changing the VP settings.Citation149 Regarding CAVI, Spronck et alCitation138 suggested a novel method of adjusting blood pressure. Steppan et alCitation135 also suggested “arterial stiffness index,” which is the product of PWV divided by PP (PWV/PP), as an effective method to adjust the influence of blood pressure on PWV. One study indicated a strong linear relationship between baPWV and the sum of four-limb PP.Citation160 Applying those concepts to these devices would also be easy.
Necessity of prospective large-scale study
Finally, this study discussed the independent prognostic predictability of baPWV and CAVI after adjustment by the multivariate Cox proportional hazards model. The more important ability is the additive predictive value on conventional risk factors (reclassification improvement in risk stratification), which was demonstrated in a few studies of baPWV and CAVI.Citation47,Citation111 This was also demonstrated in the latest meta-analysis of baPWV using individual participant data.Citation20 Further studies are expected to confirm the superior index including this factor. Furthermore, no study to date directly compared prognostic predictability of baPWV and cfPWV in a same study population. Therefore, a prospective large-scale study is warranted to simultaneously investigate baPWV, CAVI, cfPWV, and other arterial stiffness indices in the prognostic significance.
Limitations
There are several limitations to the interpretation of the results. First, because the number of articles was insufficient, the multivariate logistic analysis showed only the statistical tendency for the significance of baPWV after redefining the studies. Moreover, the analysis also demonstrated the most powerful effect of the number of the participants in each study. This implies that the success of the prognostic prediction strongly relies upon the quality of the study itself. However, it should be recognized that the statistical tendency for baPWV and exclusion criteria of LE-ASO/PAD emerged in the number of currently available articles. The results also imply that the reproducibility of baPWV as a prognostic predictor is superior to that of CAVI in the various clinical conditions. Moreover, the fact that baPWV already showed results similar to those for cfPWV in the meta-analyses would be consistent with the results of this study as a whole. Furthermore, we should recognize that only 40% of the studies proved the prognostic significance of CAVI. Second, publication bias was not considered in this study. As such, denying the existence of unpublished studies that could affect the statistical results is difficult. Nevertheless, the ratio of articles that clarified the exclusion criteria of LE-ASO/PAD was similar in the baPWV and CAVI studies. The success rates of the baPWV and CAVI studies declined in the absence of clarified exclusion criteria of LE-ASO/PAD. Moreover, the ratio of the articles studying the prognostic significance of these parameters did not differ significantly (baPWV 70/1,800; CAVI 15/550). Therefore, the prognostic studies of baPWV and CAVI were published without strong bias. Third, this study did not consider other criteria of the patient exclusion such as arrhythmia and aortic valve diseases. However, the description and the definition of the patient exclusion criteria are diverse among each study and sometimes uncertain. Thus, it was impossible to quantitatively include these factors in the statistical analysis. Nevertheless, the major limitation when using baPWV and CAVI is the presence of LE-ASO/PAD. Therefore, this factor was representatively included in the analysis. Fourth, this study did not consider the difference of covariates entered into the Cox multivariate model in each study. It is possible that the success or failure of prognostic prediction of baPWV and CAVI are induced by missing covariates or inappropriate adjustment. However, most articles researched in this study were peer reviewed. Therefore, the incidence of the inappropriate multivariate analysis would be low. Fifth, this study considered seven parameters potentially included in the multivariate logistic analysis. There might be other important factors that should have been included. Nevertheless, the number of the successful studies in the prognostic prediction was 52. Therefore, it was difficult to increase the number of parameters anyway. Finally, PubMed was the only database used in this study. However, PubMed is a widely used database worldwide, so most of the English-written articles related to the theme of this study are included.
Conclusion
This study demonstrated that the number of study participants and dialysis population were the independent determinants of the successful prognostic prediction in the baPWV and CAVI articles. This study also showed that baPWV tended to be superior to CAVI in the prognostic prediction. Moreover, the exclusion criteria of LE-ASO/PAD also affected the prognostic predictive success of both indices. Therefore, for the appropriate use of these indices, thorough LE-ASO/PAD exclusion is essential. In addition, a large-scale prospective study to simultaneously research the prognostic significance of these indices is warranted.
Acknowledgments
The author appreciates the researchers and participants of the preceding studies.
Supplementary material
Table S1 Logistic regression analysis after redefining three studies (five studies in total)
Disclosure
Dai Ato is a former employee of Fukuda Colin (formerly Omron Colin, Nippon Colin) Co., Ltd. Fukuda Colin is a distributor of VP (form PWV/ABI, BP-203RPE series). Dai Ato wrote this article as an academic activity based on the guaranteed right of freedom in academia for the Japanese (Article 23) and on the supreme law provided in Article 98 of the Constitution of Japan. Dai Ato reports no other conflicts of interest in this work.
References
- BramwellJCHillAVVelocity of transmission of the pulse-wave: and elasticity of arteriesLancet19221995149891892
- YaoSTHobbsJTIrvineWTAnkle pressure measurement in arterial disease of the lower extremitiesBr J Surg19685511859860
- VlachopoulosCXaplanterisPAboyansVThe role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation: Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) SocietyAtherosclerosis2015241250753226117398
- TownsendRRWilkinsonIBSchiffrinELRecommendations for Improving and Standardizing Vascular Research on Arterial Stiffness: A Scientific Statement From the American Heart AssociationHypertension201566369872226160955
- AboyansVCriquiMHAbrahamPMeasurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart AssociationCirculation2012126242890290923159553
- VlachopoulosCAznaouridisKStefanadisCPrediction of cardiovas-cular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysisJ Am Coll Cardiol2010551318132720338492
- Ben-ShlomoYSpearsMBoustredCAortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjectsJ Am Coll Cardiol201463763664624239664
- ZhongQHuMJCuiYJCarotid-Femoral Pulse Wave Velocity in the Prediction of Cardiovascular Events and Mortality: An Updated Systematic Review and Meta-AnalysisAngiology201869761762929172654
- SuzukiEKashiwagiANishioYIncreased arterial wall stiffness limits flow volume in the lower extremities in type 2 diabetic patientsDiabetes Care200124122107211411723092
- YamashinaATomiyamaHTakedaKValidity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurementHypertens Res200225335936412135313
- YambeTKovalevYAMilyaginaIAA Japanese-Russian collaborative study on aging and atherosclerosisBiomed Pharmacother200458Suppl 1S91S9415754844
- OrlovaIKuz’minaAEBarinovaIVIarovaiaEBAgeevFTAssessment of major artery stiffness: new perspectives of noninvasive diagnosis of coronary atherosclerosisTer Arkh2009814813
- YambeTYoshizawaMSaijoYBrachio-ankle pulse wave velocity and cardio-ankle vascular index (CAVI)Biomed Pharmacother200458Suppl 1S95S9815754845
- ShiraiKUtinoJOtsukaKTakataMA novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI)J Atheroscler Thromb200613210110716733298
- TomiyamaHKojiYYambeMBrachial -- ankle pulse wave velocity is a simple and independent predictor of prognosis in patients with acute coronary syndromeCirc J200569781582215988107
- YamamotoNYamanakaGIshikawaMCardio-ankle vascular index as a predictor of cognitive impairment in community-dwelling elderly people: four-year follow-upDement Geriatr Cogn Disord200928215315819696483
- AtoDTakamiTBrachial-Ankle Pulse Wave Velocity, Mortality, and Cardiovascular EventsJ Cardiovasc Disord2015211009
- VlachopoulosCAznaouridisKTerentes-PrintziosDIoakeimidisNStefanadisCPrediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysisHypertension201260255656222733468
- TomiyamaHMatsumotoCShiinaKYamashinaABrachial-Ankle PWV: Current Status and Future Directions as a Useful Marker in the Management of Cardiovascular Disease and/or Cardiovascular Risk FactorsJ Atheroscler Thromb201623212814626558401
- OhkumaTNinomiyaTTomiyamaHBrachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-AnalysisHypertension20176961045105228438905
- OhkumaTTomiyamaHNinomiyaTProposed Cutoff Value of Brachial-Ankle Pulse Wave Velocity for the Management of HypertensionCirc J201781101540154228835589
- YamashinaAKarioKKoharaKGuidelines for noninvasive vascular function test (JCS)2013 Available from: http://www.j-circ.or.jp/guideline/pdf/JCS2013_yamashina_h.pdfAccessed October 5, 2018
- ShimamotoKAndoKFujitaTJapanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Committee for Guidelines for the Management of HypertensionHypertens Res201437425339024705419
- KatoATakitaTFuruhashiMKumagaiHHishidaAA small reduction in the ankle-brachial index is associated with increased mortality in patients on chronic hemodialysisNephron Clin Pract20101141c29c3719816041
- KatoATakitaTFuruhashiMMaruyamaYMiyajimaHKumagaiHBrachial-ankle pulse wave velocity and the cardio-ankle vascular index as a predictor of cardiovascular outcomes in patients on regular hemodialysisTher Apher Dial201216323224122607566
- OtsukaKFukudaSShimadaKSerial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery diseaseHypertens Res201437111014102025007768
- KusunoseKSatoMYamadaHPrognostic Implications of Non-Invasive Vascular Function Tests in High-Risk Atherosclerosis PatientsCirc J20168041034104026936237
- GohbaraMIwahashiNSanoYClinical Impact of the Cardio-Ankle Vascular Index for Predicting Cardiovascular Events After Acute Coronary SyndromeCirc J20168061420142627116899
- KusunoseKYamadaHNoninvasive Vascular Function Tests - Long Journey for Predicting Cardiovascular EventsCirc J20168061321132227151336
- ShimizuTYoshihisaAKannoYRelationship of hyperuricemia with mortality in heart failure patients with preserved ejection fractionAm J Physiol Heart Circ Physiol20153097H1123H112926297226
- LinCYLeuJGFangYWTsaiMHAssociation of interleg difference of ankle brachial index with overall and cardiovascular mortality in chronic hemodialysis patientsRen Fail2015371889525350835
- TokitsuTYamamotoEHirataYClinical significance of pulse pressure in patients with heart failure with preserved left ventricular ejection fractionEur J Heart Fail201618111353136127197000
- SuzukiHInoueTDogiMKikutaTTakenakaTOkadaHRole of Pulse Wave Velocity in Patients with Chronic Kidney Disease Stages 3-5 on Long-Term Follow-UpPulse201521–4110
- HuangJCChenSCSuHMChangJMHwangSJChenHCPerformance of the Framingham risk score in patients receiving hemodialysisNephrology201318751051523647978
- OhtakeTIshiokaKHondaKImpact of coronary artery calcification in hemodialysis patients: Risk factors and associations with prognosisHemodial Int201014221822520345389
- MiuraTMinamisawaMUekiYImpressive predictive value of ankle-brachial index for very long-term outcomes in patients with cardiovascular disease: IMPACT-ABI studyPLoS One2017126e017760928617815
- MinamisawaMMiuraTMotokiHGeriatric Nutritional Risk Index Predicts Cardiovascular Events in Patients at Risk for Heart FailureCirc J20188261614162229212959
- IimoriSMoriYAkitaWEffects of sevelamer hydrochloride on mortality, lipid abnormality and arterial stiffness in hemodialyzed patients: a propensity-matched observational studyClin Exp Nephrol201216693093722581064
- YoshihisaASuzukiSYamakiTImpact of adaptive servo-ventilation on cardiovascular function and prognosis in heart failure patients with preserved left ventricular ejection fraction and sleep-disordered breathingEur J Heart Fail201315554355023250911
- SugimotoTYamamotoKTakizawaKAssessment of pulse wave velocity as a marker of post-operative cardiovascular risk in off-pump coronary artery bypass grafting patientsKyobu Geka201063753153520662230
- IchikawaKSakuragiSNishiharaTInfluence of arterial stiffness on cardiovascular outcome in patients without high blood pressureHeart2018104431832328814492
- KandaYInvestigation of the freely available easy-to-use software ‘EZR’ for medical statisticsBone Marrow Transplant201348345245823208313
- YoshidaMMitaTYamamotoRCombination of the Framingham risk score and carotid intima-media thickness improves the prediction of cardiovascular events in patients with type 2 diabetesDiabetes Care201235117818022028278
- TokitsuTYamamotoEHirataYClinical significance of pulse pressure in patients with coronary artery diseaseInt J Cardiol201519029930125935616
- LauKKWongYKChanYHPrognostic implications of surrogate markers of atherosclerosis in low to intermediate risk patients with type 2 diabetesCardiovasc Diabetol201211110122900680
- KitaharaTOnoKTsuchidaAImpact of brachial-ankle pulse wave velocity and ankle-brachial blood pressure index on mortality in hemodialysis patientsAm J Kidney Dis200546468869616183424
- NinomiyaTKojimaIDoiYBrachial-ankle pulse wave velocity predicts the development of cardiovascular disease in a general Japanese population: the Hisayama StudyJ Hypertens201331347748323615210
- MaedaYInoguchiTEtohEBrachial-ankle pulse wave velocity predicts all-cause mortality and cardiovascular events in patients with diabetes: the Kyushu Prevention Study of AtherosclerosisDiabetes Care20143782383239024898302
- KuroiwaYMiyanoINishinagaMAssociation between level of brachial-ankle pulse wave velocity and onset of activities of daily living impairment in community-dwelling older individualsGeriatr Gerontol Int201515784084725406937
- SeoHJKiYJHanMAChoiDHRyuSWBrachial-ankle pulse wave velocity and mean platelet volume as predictive values after percutaneous coronary intervention for long-term clinical outcomes in Korea: A comparable and additive studyPlatelets201526766567125383727
- ChangLHLinHDKwokCFThe combination of the ankle brachial index and brachial ankle pulse wave velocity exhibits a superior association with outcomes in diabetic patientsIntern Med201453212425243125365999
- ShengCSLiYLiLHBrachial-ankle pulse wave velocity as a predictor of mortality in elderly ChineseHypertension20146451124113025259749
- KatakamiNOsonoiTTakaharaMClinical utility of brachial-ankle pulse wave velocity in the prediction of cardiovascular events in diabetic patientsCardiovasc Diabetol201413112825186287
- KiYJChoiDHLeeYMLimLSongHKohYYPredictive value of brachial-ankle pulse wave velocity for long-term clinical outcomes after percutaneous coronary intervention in a Korean cohortInt J Cardiol2014175355455925015023
- KimJSongTJSongDBrachial-ankle pulse wave velocity is a strong predictor for mortality in patients with acute strokeHypertension201464224024624821942
- KawaiTOhishiMOnishiMPrognostic impact of regional arterial stiffness in hypertensive patientsHeart Vessels201530333834624566589
- NagaiKShibataSAkishitaMEfficacy of combined use of three non-invasive atherosclerosis tests to predict vascular events in the elderly; carotid intima-media thickness, flow-mediated dilation of brachial artery and pulse wave velocityAtherosclerosis2013231236537024267253
- TakashimaNTurinTCMatsuiKThe relationship of brachial-ankle pulse wave velocity to future cardiovascular disease events in the general Japanese population: the Takashima StudyJ Hum Hypertens201428532332724172293
- YoonHEShinDIKimSJBrachial-ankle pulse wave velocity predicts decline in renal function and cardiovascular events in early stages of chronic kidney diseaseInt J Med Sci201310111430143624046514
- IshisoneTKoedaYTanakaFSatoKNaganoMNakamuraMComparison of utility of arterial stiffness parameters for predicting cardiovascular events in the general populationInt Heart J201354316016523774240
- KawaiTOhishiMOnishiMCut-off value of brachial-ankle pulse wave velocity to predict cardiovascular disease in hypertensive patients: a cohort studyJ Atheroscler Thromb201320439140023268984
- HanJYChoiDHChoiSWPredictive value of brachial-ankle pulse wave velocity for cardiovascular eventsAm J Med Sci20133462929723085673
- MunakataMKonnoSMiuraYYoshinagaKJ-TOPP Study GroupPrognostic significance of the brachial-ankle pulse wave velocity in patients with essential hypertension: final results of the J-TOPP studyHypertens Res201235883984222534520
- ChenSCChangJMLiuWCBrachial-ankle pulse wave velocity and rate of renal function decline and mortality in chronic kidney diseaseClin J Am Soc Nephrol20116472473221454721
- InoueTOgawaTIshidaHAndoYNittaKAortic arch calcification evaluated on chest X-ray is a strong independent predictor of cardiovascular events in chronic hemodialysis patientsHeart Vessels201227213514221416116
- OrlovaIKuz’minaAEMasenkoVPIarovaiaEBAgeevFTEffect of arterial stiffness on development of cardiovascular complications in ischemic heart diseaseKardiologiia200949121117
- NakamuraMYamashitaTYajimaJBrachial-ankle pulse wave velocity as a risk stratification index for the short-term prognosis of type 2 diabetic patients with coronary artery diseaseHypertens Res201033101018102420703233
- TurinTCKitaYRumanaNBrachial-ankle pulse wave velocity predicts all-cause mortality in the general population: findings from the Takashima study, JapanHypertens Res201033992292520555327
- MiyanoINishinagaMTakataJAssociation between brachial-ankle pulse wave velocity and 3-year mortality in community-dwelling older adultsHypertens Res201033767868220431594
- MeguroTNagatomoYNagaeAElevated arterial stiffness evaluated by brachial-ankle pulse wave velocity is deleterious for the prognosis of patients with heart failureCirc J200973467368019246812
- MatsuokaOOtsukaKMurakamiSArterial stiffness independently predicts cardiovascular events in an elderly community -- Longitudinal Investigation for the Longevity and Aging in Hok-kaido County (LILAC) studyBiomed Pharmacother200559Suppl 1S40S4416275505
- WangXDangAPrognostic Value of Brachial-Ankle Pulse Wave Velocity in Patients With Takayasu Arteritis With Drug-Eluting Stent ImplantationArthritis Care Res201567811501157
- ChenSCLeeWHHsuPCAssociation of Brachial-Ankle Pulse Wave Velocity With Cardiovascular Events in Atrial FibrillationAm J Hypertens201629334835626271108
- ParkKHHanSJKimHSImpact of Framingham risk score, flow-mediated dilation, pulse wave velocity, and biomarkers for cardiovascular events in stable anginaJ Korean Med Sci201429101391139725368493
- KuwaharaMHasumiSMandaiSRate of ankle-brachial index decline predicts cardiovascular mortality in hemodialysis patientsTher Apher Dial2014181918
- OrlovaIANuralievEYYarovayaEBAgeevFTPrognostic value of changes in arterial stiffness in men with coronary artery diseaseVasc Health Risk Manag201061015102121127698
- TanakaMIshiiHAoyamaTAnkle brachial pressure index but not brachial-ankle pulse wave velocity is a strong predictor of systemic atherosclerotic morbidity and mortality in patients on maintenance hemodialysisAtherosclerosis2011219264364722018643
- AmemiyaNOgawaTOtsukaKAndoYNittaKComparison of serum albumin, serum C-reactive protein, and pulse wave velocity as predictors of the 4-year mortality of chronic hemodialysis patientsJ Atheroscler Thromb201118121071107921921415
- ChenSCChangJMTsaiJCA new systolic parameter defined as the ratio of brachial pre-ejection period to brachial ejection time predicts overall and cardiovascular mortality in hemodialysis patientsHypertens Res201033549249820203683
- MorimotoSYurugiTAotaYPrognostic significance of ankle-brachial index, brachial-ankle pulse wave velocity, flow-mediated dilation, and nitroglycerin-mediated dilation in end-stage renal diseaseAm J Nephrol2009301556319204388
- NagataYMiuraSSuematsuYAssociation between major adverse cardiovascular events and brachial-ankle pulse wave velocity and a difference in blood pressure between arms after percutaneous coronary interventionExp Clin Cardiol2014
- LeeHSKimHLKimHIncremental Prognostic Value of Brachial-Ankle Pulse Wave Velocity to Single-Photon Emission Computed Tomography in Patients with Suspected Coronary Artery DiseaseJ Atheroscler Thromb201522101040105026235347
- ChenSCChangJMTsaiJCA systolic parameter defined as the ratio of brachial pre-ejection period to brachial ejection time predicts cardiovascular events in patients with chronic kidney diseaseCirc J201074102206221020736503
- WeiSYHuangJCChenSCChangJMChenHCUnequal Arterial Stiffness With Overall and Cardiovascular Mortality in Patients Receiving HemodialysisAm J Med Sci2016351218719326897274
- IinoRYokoyamaNKonnoKNaitoKIsshikiTImpact of combined assessment of coronary artery calcium score, carotid artery plaque score, and brachial-ankle pulse wave velocity for early coronary revascularization in patients with suspected coronary artery diseaseInt Heart J201253315415922790682
- LiYHLinSYSheuWHLeeITRelationship between percentage of mean arterial pressure at the ankle and mortality in participants with normal ankle-brachial index: an observational studyBMJ Open201663e010540
- SugamataWNakamuraTUematsuMThe combined assessment of flow-mediated dilation of the brachial artery and brachial-ankle pulse wave velocity improves the prediction of future coronary events in patients with chronic coronary artery diseaseJ Cardiol201464317918424556367
- SongYXuBXuRIndependent and Joint Effect of Brachial-Ankle Pulse Wave Velocity and Blood Pressure Control on Incident Stroke in Hypertensive AdultsNovelty and SignificanceHypertension2016681465327217412
- IkuraKHanaiKOkaSBrachial-ankle pulse wave velocity, but not ankle-brachial index, predicts all-cause mortality in patients with diabetes after lower extremity amputationJ Diabetes Investig201782250253
- KawaiTOhishiMTakeyaYAdiponectin single nucleotide polymorphism is a genetic risk factor for stroke through high pulse wave pressure: a cohort studyJ Atheroscler Thromb201320215216023047599
- ChenSCChangJMTsaiYCAssociation of interleg BP difference with overall and cardiovascular mortality in hemodialysisClin J Am Soc Nephrol20127101646165322859748
- MimuraTTakenakaTKannoYMoriwakiKOkadaHSuzukiHVascular compliance is secured under angiotensin inhibition in non-diabetic chronic kidney diseasesJ Hum Hypertens2008221384717653243
- AhnKTJeongJOJinSABrachial-ankle PWV for predicting clinical outcomes in patients with acute strokeBlood Press201726420421028142262
- KimEJChoiMJLeeJHExtracellular Fluid/Intracellular Fluid Volume Ratio as a Novel Risk Indicator for All-Cause Mortality and Cardiovascular Disease in Hemodialysis PatientsPLoS One2017121e017027228099511
- TabataNSuetaDYamashitaTRelationship between asymp-tomatic intra-cranial lesions and brachial-ankle pulse wave velocity in coronary artery disease patients without strokeHypertens Res201740439239827881850
- SajiNMurotaniKShimizuHIncreased pulse wave velocity in patients with acute lacunar infarction doubled the risk of future ischemic strokeHypertens Res201740437137527853164
- UekiYMiuraTMinamisawaMThe usefulness of brachial-ankle pulse wave velocity in predicting long-term cardiovascular events in younger patientsHeart Vessels201732666066727822742
- AisuHSaitoMInabaSAssociation of worsening arterial stiffness with incident heart failure in asymptomatic patients with cardiovascular risk factorsHypertens Res201740217318027581536
- KuoTHYangDCLinWHCompliance Index, a Marker of Peripheral Arterial Stiffness, may Predict Renal Function Decline in Patients with Chronic Kidney DiseaseInt J Med Sci201512753053726180508
- KajimotoTSawamuraMSHayashiRDOyaTHiraoRAKouharaHHigh efficient and cost-effective screening method for diabetic cardiovascular riskDiabetol Metab Syndr2014615124713330
- WooJSKimWJangHHKimJBKimWSKimKSEffect of platelet reactivity, endothelial function, and inflammatory status on outcomes in patients with stable angina pectoris on clopidogrel therapyAm J Cardiol2014113578679224388620
- ParkHWKangMGKimKPrognostic value of brachial-ankle pulse wave velocity in patients with non-ST-elevation myocardial infarctionCoron Artery Dis201728864264828692482
- LuYCLyuPZhuHYBrachial-ankle pulse wave velocity compared with mean arterial pressure and pulse pressure in risk stratification in a Chinese populationJ Hypertens201836352853629045343
- TokitsuTYamamotoEOikeFClinical significance of brachial-ankle pulse-wave velocity in patients with heart failure with preserved left ventricular ejection fractionJ Hypertens201836356056829084082
- HwangICJinKNKimHLAdditional prognostic value of brachial-ankle pulse wave velocity to coronary computed tomography angiography in patients with suspected coronary artery diseaseAtherosclerosis201826812713729216483
- WangLLLuoQZhuBXZhouFFBrachial-Ankle Pulse Wave Velocity Could Be a Predictor of Mortality in Patients on Peritoneal DialysisPerit Dial Int201838321521929386306
- TaniguchiYKitamuraAShinozakiTTrajectories of arterial stiffness and all-cause mortality among community-dwelling older JapaneseGeriatr Gerontol Int20181871108111329608041
- YamaguchiSGohdaTGotohHFactors associated with cardiovascular death and events in patients with end stage renal diseaseNihon Jinzo Gakkai Shi201355215916623631303
- SatoYNagayamaDSaikiACardio-Ankle Vascular Index is Independently Associated with Future Cardiovascular Events in Outpatients with Metabolic DisordersJ Atheroscler Thromb201623559660526632164
- LaucevičiusARyliškytėLBalsytėJAssociation of cardio-ankle vascular index with cardiovascular risk factors and cardiovascular events in metabolic syndrome patientsMedicina201551315215828705477
- Satoh-AsaharaNKotaniKYamakageHCardio-ankle vascular index predicts for the incidence of cardiovascular events in obese patients: a multicenter prospective cohort study (Japan Obesity and Metabolic Syndrome Study: JOMS)Atherosclerosis2015242246146826295798
- ChungSLYangCCChenCCHsuYCLeiMHCoronary Artery Calcium Score Compared with Cardio-Ankle Vascular Index in the Prediction of Cardiovascular Events in Asymptomatic Patients with Type 2 DiabetesJ Atheroscler Thromb201522121255126526269147
- KubotaYMaebuchiDTakeiMCardio-Ankle Vascular Index is a predictor of cardiovascular eventsArtery Res2011539196
- YoshihisaATakiguchiMShimizuTCardiovascular function and prognosis of patients with heart failure coexistent with chronic obstructive pulmonary diseaseJ Cardiol201464425626424674751
- SawaiAYasudaYSuzukiSImpact of non-invasive cardiovascular screening programs as a predictor of cardiovascular events among asymptomatic chronic kidney disease patientsClin Exp Nephrol201620341642426403282
- HaradaMTsukadaWTsukadaOHashimotoKKamijoYThe Optimal Cut-off Value of Ankle Brachial Index for Screening Cardiovascular Disease Risk in Hemodialysis PatientsShinshu Med J2016643135146
- AtoDPitfalls in the ankle-brachial index and brachial-ankle pulse wave velocityVasc Health Risk Manag201814416229662315
- CicconeMMBilianouEBalbariniATask force on: ‘Early markers of atherosclerosis: influence of age and sex’J Cardiovasc Med20131410757766
- MunakataMBrachial-ankle pulse wave velocity in the measurement of arterial stiffness: recent evidence and clinical applicationsCurr Hypertens Rev2014101495725392144
- OnoKTsuchidaAKawaiHAnkle-brachial blood pressure index predicts all-cause and cardiovascular mortality in hemodialysis patientsJ Am Soc Nephrol20031461591159812761260
- OtaniYOtsuboSKimataNEffects of the ankle-brachial blood pressure index and skin perfusion pressure on mortality in hemodialysis patientsIntern Med201352212417242124190145
- OgataHKumata-MaetaCShishidoKDetection of peripheral artery disease by duplex ultrasonography among hemodialysis patientsClin J Am Soc Nephrol20105122199220620798256
- OhtakeTOkaMIkeeRImpact of lower limbs’ arterial calcification on the prevalence and severity of PAD in patients on hemodialysisJ Vasc Surg201153367668321211928
- TsuyukiKKohnoKEbineKUsefulness of Exercise-Ankle Brachial Pressure Index Test and Its Diagnostic Criteria in Patients on Maintenance HemodialysisJ Japanese College Angiol20155522125
- NatsuakiCInoguchiTMaedaYAssociation of borderline ankle-brachial index with mortality and the incidence of peripheral artery disease in diabetic patientsAtherosclerosis2014234236036524732575
- TanakaSKanekoHKanoHThe predictive value of the borderline ankle-brachial index for long-term clinical outcomes: An observational cohort studyAtherosclerosis2016250697627182960
- LeeSHChoiSHKimEKBorderline ankle-brachial index is associated with poor short-term clinical outcome after coronary artery interventionAtherosclerosis201624918619027124651
- KimHLSeoJBChungWYZoJHKimMAKimSHPrognostic value of the ankle-brachial index in patients undergoing drug-eluting stent implantationJ Atheroscler Thromb2015221273725168846
- KojimaINinomiyaTHataJA low ankle brachial index is associated with an increased risk of cardiovascular disease: the Hisayama studyJ Atheroscler Thromb201421996697324727729
- ShengCSLiYHuangQFKangYYLiFKWangJGPulse Waves in the Lower Extremities as a Diagnostic Tool of Peripheral Arterial Disease and Predictor of Mortality in Elderly ChineseHypertension201667352753426781275
- HashimotoTIchihashiSIwakoshiSKichikawaKCombination of pulse volume recording (PVR) parameters and ankle-brachial index (ABI) improves diagnostic accuracy for peripheral arterial disease compared with ABI aloneHypertens Res201639643043426911230
- ShiraiKSongMSuzukiJContradictory effects of β1- and α1- adrenergic receptor blockers on cardio-ankle vascular stiffness index (CAVI)--CAVI independent of blood pressureJ Atheroscler Thromb2011181495521071883
- TomiyamaHYamashinaACentral blood pressure--a possible latent factor affecting CAVIJ Atheroscler Thromb2011188720 author reply 721–72221532238
- ShiraiKTakahashiMAuthor’s Reply to: Central Blood Pressure: A Possible Latent Factor Affecting CAVIJ Atheroscler Thromb2011188721722
- SteppanJSikkaGHoriDSeeking a blood pressure-independent measure of vascular propertiesHypertens Res2016391273826490088
- MalihaGTownsendRRA study of the VaSera arterial stiffness device in US patientsJ Clin Hypertens2017197661668
- LimJPearmanMEParkWAlkatanMMachinDRTanakaHImpact of blood pressure perturbations on arterial stiffnessAm J Physiol Regul Integr Comp Physiol201530912R1540R154526468262
- SpronckBAvolioAPTanIButlinMReesinkKDDelhaasTArterial stiffness index beta and cardio-ankle vascular index inherently depend on blood pressure but can be readily correctedJ Hypertens20173519810427906838
- SegersPA lesson in vigilance: pressure dependency of a presumed pressure-independent index of arterial stiffnessJ Hypertens2017351333527902626
- ShiraiKShimizuKTakataMSuzukiKIndependency of the cardio-ankle vascular index from blood pressure at the time of measurementJ Hypertens20173571521152328426443
- GrilloASalviPCardio-ankle vascular index and carotid-femoral pulse wave velocity: limits and strengthsJ Hypertens201836475976429489613
- ObataYMizogamiMSinghSEjection time: influence of hemodynamics and site of measurement in the arterial treeHypertens Res201740981181828356575
- UeyamaKMiyataMKubozonoTNoninvasive indices of arterial stiffness in hemodialysis patientsHypertens Res200932871672019521417
- TakizawaCItoMIwasaMClinical significance of ABI by measuring bilateral arms in hemodialysis patientsJapanese Association of Cardiovascular Intervention and Therapeutic (1884-0027)5Suppl.I73620135 Japanese
- VerberkWJKesselsAGThienTBlood pressure measurement method and inter-arm differences: a meta-analysisAm J Hypertens201124111201120821776035
- Van BergenFHWeatherheadDSTreloarAEDobkinABBuckleyJJComparison of indirect and direct methods of measuring arterial blood pressureCirculation195410448149013209734
- GourdeauMMartinRLamarcheYTétreaultLOscillometry and direct blood pressure: a comparative clinical study during deliberate hypotensionCan Anaesth Soc J1986333 Pt 13003073719430
- RibezzoSSpinaEdi BartolomeoSSansonGNoninvasive techniques for blood pressure measurement are not a reliable alternative to direct measurement: a randomized crossover trial in ICUScientific World J20142014353628
- TsushimaMKyotaniSNakanoSDiagnosis of early stages of atherosis and sclerosis of carotid artery and risk factors. The pulse wave velocity(PWV), ankle-brachial index(ABI), and the intima-media complex thickness(IMT) in inhabitantsJJCDP200237117124 Japanese
- TakakiAOgawaHWakeyamaTCardio-ankle vascular index is superior to brachial-ankle pulse wave velocity as an index of arterial stiffnessHypertens Res20083171347135518957805
- IchiharaAYamashitaNTakemitsuTCardio-ankle vascular index and ankle pulse wave velocity as a marker of arterial fibrosis in kidney failure treated by hemodialysisAm J Kidney Dis200852594795518760518
- EndesSCaviezelSDratvaJReproducibility of oscillometrically measured arterial stiffness indices: Results of the SAPALDIA 3 cohort studyScand J Clin Lab Invest201575217017625594797
- MiyoshiTItoHHorinakaSShiraiKHigakiJOrimioHProtocol for Evaluating the Cardio-Ankle Vascular Index to Predict Cardiovascular Events in Japan: A Prospective Multicenter Cohort StudyPulse20174Suppl 1111628275590
- García-OrtizLRecio-RodríguezJIMora-SimónSVascular structure and function and their relationship with health-related quality of life in the MARK studyBMC Cardiovasc Disord2016169527177028
- Gomez-SanchezLGarcia-OrtizLPatino-AlonsoMCThe Association Between the Cardio-ankle Vascular Index and Other Parameters of Vascular Structure and Function in Caucasian Adults: MARK StudyJ Atheroscler Thromb201522990191125994828
- TopouchianJLabatCGautierSEffects of metabolic syndrome on arterial function in different age groups: the Advanced Approach to Arterial Stiffness studyJ Hypertens201836482483329324585
- FukuiTAbeYYasudaTYoshitakaSComparison of the Measurements of Brachial-Ankle Pulse Wave Velocity (baPWV) and Cardio-ankle Vascular Index (CAVI) as an Examination for Aortic StiffnessNingen Dock2008237076 Japanese
- AtoDSawayamaTFactors associated with high brachial-ankle pulse wave velocity in non-hypertensive and appropriately treated hypertensive patients with atherosclerotic risk factorsVasc Health Risk Manag20171338339229066906
- KimTLeeCSLeeSDImpacts of comorbidities on the association between arterial stiffness and obstructive sleep apnea in the elderlyRespiration201589430431125790940
- ZhengYLiZShuHLiuMChenZHuangJRelationship between sum of the four limbs’ pulse pressure and brachial-ankle pulse wave velocity and atherosclerosis risk factors in Chinese adultsBiomed Res Int20152015434516725695080