Abstract
Purpose
This study was conducted to investigate the relationships between arterial stiffness, frailty and fall-related injuries among community-dwelling older adults.
Materials and Methods
A cross-sectional study of a random sample of older adults aged 60 years and older was conducted. Main study parameters: arterial stiffness was measured by the determining the cardio-ankle vascular index (CAVI); Frailty status was defined using a 7-item frailty screening scale, developed in Russia. This questionnaire included question about falls and fall-related injuries. Orthostatic test and anthropometric tests were done. Medical history (comorbidity, medications), the Osteoporosis Self-assessment Tool (OST), nutritional, physical, cognitive and functional status were evaluated.
Results
The study population included 163 people aged 60–89 years. The average predicted value of CAVI in women aged 60–69 was 9.13 ± 0.13, in men, 9.49 ± 0.05; in women aged 70–79, it was 9.49 ± 0.16, in men, 9.73 ±0.11; in women aged 80 and older it was 10.04 ±0.18, in men, 10.24 ±0.10 units. The CAVI above the predicted value was associated with fall-related injuries even after adjustment for age, sex, use of β-blockers (BBs), history of stroke, and region of residence with the odds ratio 3.52 (95% CI: 1.03 −12.04).
Conclusion
Our study revealed an independent association between arterial stiffness and fall-related injuries in older adults over 60 years. The findings suggest that clinicians, especially geriatricians, should pay attention to arterial stiffness of patients with fall-related injuries. Similarly, the patients with CAVI above age-predicted value should be evaluated for risk of falls for prevention of fall-related injuries.
Graphical abstract

Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Fall-related injuries are a main cause of morbidity and disability in older adults.Citation1 The greatest number of fatal falls occurs among people over 65-years-old. Almost a third of community-dwelling older adults over 65-years-old and half of them over 80-years-old fall at least once per year.Citation1 Every second patient who reported a fall incident would fall again. Commonly, older patients do not inform their doctor about fall events, considering them as inevitable and regular companions of old age - especially if falls did not lead to fractures.
The pathogenesis of falls is often multifactorial and the cause is not always easily identifiable. Factors, which are associated with falls in older adults include: frailty, reduced efficacy of postural responses, cardiovascular diseases (CVD), chronicle lung diseases, diabetes mellitus, obesity, sensory impairment, low muscle strength, polypharmacy, depression, fear of falling, cognitive decline, environmental factors (poor lighting, slippery or uneven surfaces, problems with bad shoes, etc.), and others.Citation2,Citation3
Arterial stiffness was proposed as a new factor of falls in older adults,Citation4 however the association between arterial stiffness and fall-related injuries is still not clear.
There are several non-invasive methods to assess the arterial wall structure and function. Due to the large number of studies, measurement of pulse wave velocity (PWV) was a widely accepted as a “gold standard” of the assessment of arterial stiffness.Citation5,Citation6 However, PWV is not a direct measure of stiffness, but a measure of the speed of the pressure pulse. Thus, measurement of PWV has several limitations. Foremost, PWV value depends highly on blood pressure value at the time of measurement. Moreover, it does not reliably represent the true length of the arterial segment in obese patients and in older adults with more tortuous arteries.Citation5 A cardio-ankle vascular index (CAVI) was developed as an alternative test for more direct measure of stiffness, and independent from blood pressure and used hypotensive therapy.Citation5 The additional advantage of CAVI over other procedures for measuring arterial stiffness is its relative simplicity and low cost.Citation6,Citation7
This study was conducted to investigate the relationships between arterial stiffness assessed by CAVI and fall-related injuries among community-dwelling older adults.
Materials and Methods
Design of Study
This cross-sectional study was conducted on a random sample of community-dwelling older adults aged 60 years and older. We recruited 100 patients from Bashkortostan and 63 patients from St. Petersburg. The exclusion criteria were as follows: persistent atrial fibrillation, any limb amputation, previously diagnosed critical aortic stenosis or severe aortic valve insufficiency.
Written informed consent was obtained from all participants. We confirm that this study was conducted in accordance with the Declaration of Helsinki. The local ethics committee of The North-Western State Medical University named after I. I. Mechnikov approved this research for Postgraduate Studies.
Main Study Parameters
Cardio-Ankle Vascular Index
CAVI was measured using the Vascular Screening System VaSera VS-1500 (Fukuda Denshi Co Ltd, Tokyo, Japan) as per the manufacturer’s recommendations. CAVI requires placement of ECG electrodes on both wrists, a microphone for phonocardiography on the sternum, and four BP cuffs wrapped around the four limbs. The upper arm and ankle pulse waves, as well as blood pressure are measured. CAVI is disregarded if the ankle–brachial index is less than 0.9Citation6,Citation8
In a previous study, we obtained equations for calculating the predicted CAVI for older people in Bashkortostan and then confirmed this result during an external validation in the population from St. Petersburg Citation9. These equations were used in current study as follows:
CAVI above the predicted value in accordance with the proposed formula was considered as a high CAVI.
Frailty
Frailty was diagnosed using a 7-item frailty screening scale, developed in Russia.Citation10 The assessment of frailty based on the 7-item frailty screening scale used the following 7 criteria:
- Weight loss was defined as unintentionally losing 5 kg of weight in the past 6 months (Weight loss).
- Experience any limitations in everyday life due to decreased vision or hearing (Hearing or vision loss)
- Falls or self-reported fall-related injuries during last year
- Feeling depressed, sad or anxiety in recent weeks (Mood decline)
- Problems with memory, understanding, orientation, or ability to plan (Cognitive decline)
- Urinary Incontinence
- Difficulty moving around your home or outdoors (Walking up to 100 m/climb 1 flight of stairs) (Mobility)
Participants were considered frail if five or more of the above criteria were present.Citation10,Citation11
Orthostatic Hypotension
Systolic (SBP) and diastolic blood pressure (DBP) was measured in clinic according to the European Society of Hypertension guidelines using validated equipment that meets certification criteria.Citation12 Orthostatic test included measurement of heart rate, SBP and DBP in the sitting position, the supine position, and at 1, 2 and 3 minutes after the transition to a vertical position. Orthostatic hypotension was diagnosed with a decrease in SBP ≥ 20 mm and/or a decrease in diastolic pressure ≥ 10 mm within 3 minutes after moving to a vertical position (standing position) from the supine position.Citation13
Covariates
Anthropometric Tests
Anthropometric measurements were conducted, including height, weight, waist circumference. Body mass index (BMI) was calculated as the weight (in kilograms) divided by the square of the height (in meters) (BMI = Kg/M2).
Comorbidity
Details of past and current medical problems, information on arterial hypertension, coronary artery diseases, myocardial infarction, peripheral artery disease, stroke, chronic obstructive pulmonary disease (COPD), asthma, diabetes mellitus, cancer, osteoarthritis and rheumatoid arthritis, anemia, osteoporosis were collected based on anamnesis or information in the medical records.
Pharmacotherapy
Data of pharmacotherapy were collected based on information in the medical records or according to the survey of participants.
Risk of Osteoporosis and Low Bone Mineral Density
The Osteoporosis Self-assessment Tool (OST) index [0,2*[weigh ((kilograms) – age (years))] was used for detection participants at the risk of osteoporosis and low bone mineral density. The cut-off value for OST was <2.Citation11
Cognitive Function
The Mini-Mental State Examination (MMSE) was used to determine cognitive impairment. The cut-off score was 24.
Nutritional Status
Nutritional status was evaluated using the Mini Nutritional Assessment (MNA) questionnaire. An MNA score < 23.5 was interpreted as malnutrition or at risk of malnutrition.
Physical Function
A balance test and gait speed were used to assess physical function.Citation1
Statistical Analysis
Means (± standard deviation [SD]) or median (interquartile range [IQR]) were calculated for the continues data. Differences among the participants with different value of CAVI, frailty status and falls injuries were compared using the Mann–Whitney U-test for continuous variables or the chi-square test for categorical variables.
Multivariate analysis (simple and multiple logistic and linear regression) was used to evaluate the association between the CAVI, falls injuries and frailty. The variables were first checked for multicollinearity.
All statistical calculations were performed using SPSS 20.0 (IBM, Armonk, NY, USA), MedCalc 11.5.00 (MedCalc Software, Oostende). The level of significance adopted was p<0.05
Results
Full data was collected for 163 people aged 60–89 years. The mean age of the participants was 70.9 ±6.5 years. In total, 40% (n=66) were women. The average predicted value of CAVI in women aged 60–69 was 9.13±0.13, in men, 9.49 ±0.05; in women aged 70–79 it was 9.49 ±0.16, in men, 9.73 ±0.11; in women aged 80 and older it was 10.04 ±0.18, in men, 10.24 ±0.10 .
The CAVI above the predicted value was detected in 47.8% (n=78) participants (). Participants with a higher value of CAVI reported more fall-related injuries in the previous year (, ). Specifically, for women, but not for men, high CAVI was associated with lower BMI and low waist circumference (). Association between lower BMI and high CAVI remained significant even after adjustment for age, stroke and nutritional status with β −3.130 (95% CI: −4.960 - −1.300). Association between waist circumference and high CAVI remained significant after adjustment for age and stroke, but lost significance after adjustment for nutritional status. There were no differences between the participants with different CAVI value in age, prevalence of other chronic diseases and drug use (p > 0.05 for all variables).
Table 1 Health Characteristics of Study Population with Different CAVI
Figure 1 Flowchart of data collection.
Abbreviations: High CAVI, cardio-ankle vascular index above predicted value; Low CAVI, cardio-ankle vascular index lower or equal predicted value.
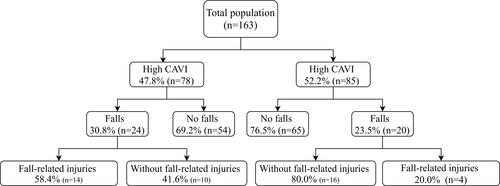
We assessed baseline characteristics of participants with and without fall-related injuries. The prevalence of falls during last year was 27% (n=44) and 40.9% (n=18) of them were accompanied by fall-related injuries. High CAVI was associated only with fall-related injuries, but not with total cases of falls during last year (). Baseline characteristics of participants with and without fall-related injuries are described in . Weight loss, depression and use of β-blockers (BBs) were more prevalent in participants with fall-related injuries.
Table 2 Health Characteristics of Study Population with and without Fall-Related Injuries in Anamnesis
Table 3 Association Between High CAVI and Fall-Related Injuries in Study Population
The asssociation with high CAVI and fall-related injuries remained significant even after adjustment for age, sex, taking BBs, stroke, and region of residence with odds ratio 3.52 (95% CI: 1.03–12.04) ().
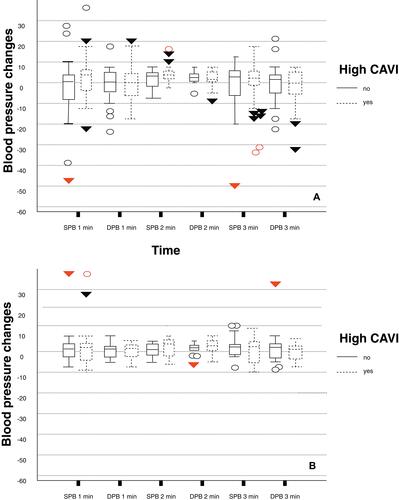
Orthostatic hypotension was revealed in 4.9% (n=8) participants in the study, but it was not associated with high CAVI or fall-related injuries (–). However, women with high CAVI had a more pronounced decline in SBP in minute 2 when performing the orthostatic test compared with those with low CAVI (A). This observation was not applicable to men (B). The association between high CAVI and a pronounced decline in SBP in minute 2 in women was significant and also after adjustment for age, stroke, nutritional status, and drugs that were used for the pharmacologic management of hypertension with β 2.684 (95% CI: 0.359–5.009). Nonetheless, changes of SBP in 2 minutes was not directly link with falls or fall-related injuries.
Figure 2 Association between arterial stiffness and changes of blood pressure during orthostatic test performing in women (A) and men (B).
Although we found a strong association between high CAVI and fall-related injuries, there was no link between arterial stiffness and the high risk of osteoporosis or proposed cut-off value of OST < 2 (–). However, we detected a negligible negative correlation between OST score and CAVI value with Pearson correlation coefficient – 0.25 (p<0.05).
Discussion
Main Findings
Our study revealed significant association between high arterial stiffness evaluated by CAVI and fall-related injuries in community-dwelling older adults 60 years and older. This difference remained significant even after adjustments for age, sex, stroke in anamnesis, and region of residence.
Possible Interconnection Between CAVI and Fall-Related Injuries in Older Adults
Falls can be described in terms of three phases:Citation14
The first phase is an initiating event that displaces the body’s centre of mass outside its base of support. Initiating events involve extrinsic factors such as environmental hazards; intrinsic factors such as unstable joints, muscle weakness, and unreliable postural reflexes; and physical activities in progress at the time of the fall.Citation14
The second phase of a fall due to the failure of systems, responsible for the upright posture maintenance, to detect and correct this displacement at the right moment to avoid a fall. This failure is usually due to factors which are specific to the given individual, e.g., loss of sensory function, impaired central processing, and muscle weakness.
The third phase is an impact of the body to the collision with surfaces – e.g., the floor or ground, which results in the transmission of forces to body tissue and organs Citation14 The potential for injury is a function of the magnitude and direction of the forces and the susceptibility of tissues and organs to damage.Citation14
High arterial stiffness may affect all three phases of falls. Unlike in our study, previous studies detected an association between high arterial stiffness, sarcopenia, and frailty that influence the first phase of fallsCitation1,Citation2,Citation14. Xue et al showed that high CAVI score was associated with phenotype model of frailty even when adjusting for multiple factors such as age, BMI, autonomy in daily living, haemoglobin, albumin, renal function, hs-CRP, and low-density lipoprotein, however, the reason for this association is unclear.Citation2 A possible explanation of this association can be linked to arterial hemodynamic dysfunction due to atherosclerosis which leads to muscle blood flow decreases and may have a predictive effect on reduction in muscle mass, grip strength, and walking speed, which can cause frailty, disability, and falls.Citation16 The phenotype model’s criteria such as weakness and low physical function describe age-related loss of muscle mass and strength, known as sarcopenia. Thus, sarcopenia is a central biological substrate of phenotype frailty model.Citation17 Several previous researches had also found artery stiffness and subclinical vascular dysfunction, even without the presence of CVD-associated sarcopenia.Citation16,Citation18,Citation19
Arterial stiffness is now accepted as one of cardiovascular risk factors.Citation20 The Rockwood cumulative deficit Frailty Index, that was used in The Framingham Heart Study, includes questions about the presence of CVD (hypertension, stroke, myocardial infarction, angina, and heart failure), arthritis comorbidity and diabetes, that associate with arterial stiffness on their own.Citation9,Citation15,Citation21-Citation24 Consequently, it explain an association between the Rockwood cumulative deficit Frailty Index and arterial stiffness.Citation25
We used a 7-item frailty screening scale, that is a cumulative deficit model of frailty, but unlike the Rockwood cumulative deficit Frailty Index, it does not include CVD and other diseases that are associated with vascular stiffness and does not directly evaluate muscle mass and strength as a phenotype frailty model.Citation10 Thus, it can explain a lack of association between frailty status and arterial stiffness in the current study.
High arterial stiffness can be responsible for the disturbance of upright posture maintenance. Previously, arterial stiffness is considered to be a risk factors of falls due to developing orthostatic hypotension.Citation4 In our study we found no direct link between fall-related injuries and orthostatic hypotension, however, we revealed a strong association between a drop in SBP in minute 2 after standing up and high arterial stiffness.
Arterial stiffness is linked with all components of cerebral small vessel disease (silent lacunar infarcts, white matter lesions or leukoaraiosis, microbleeds), stroke and cognitive decline. Recently, white matter lesions and stroke have been identified as independent factors of risk of falls.Citation26,Citation27 Several potential mechanisms can underlie the association between white matter lesions and fall risk. First, impact on initiation of movement, direction of movement, and speed and duration of movement by damage in the integrity of the neural network within the brain and the long descending motor fibers.Citation28 Second, impair of executive function due to cognitive decline.Citation28 In current study, high CAVI was also associated with stroke that are closely linked with cerebral small vessel disease and high risk of falls in older adults.
Arterial stiffness is associated with low bone mineral density that can increase risk of fracture during the falls.Citation29–Citation31 For example, in observational cross-sectional study of inpatients aged 50 years and older from the Department of Geriatrics, CAVI values were negatively correlated with femoral neck and total hip bone mineral density assessed using Dual-energy X-ray.Citation31 We detected negligible negative correlation between the OST score and CAVI value that could increase risk of injuries in our population.
We revealed an association between high CAVI and low BMI, and low waist circumference. This association was confirmed in other research.Citation32 Several hypotheses have been proposed to explain this relationship, however, the mechanism and the threshold of the effect of BMI on change in arterial stiffness are not fully understood.Citation32 On the other hand, previously, low BMI was identified as a high risk factors of falls in older adults.Citation33
Strengths and Limitations
The limitation of our study was that 99% of the study's participants had CVD or diabetes, as a result of which we cannot make a judgment about the association of arterial stiffness and fall injuries or frail status in people without CVD. Given the cross-sectional design of the study, we cannot speak with confidence about the possible prediction of the development of fall-related injuries in patients with high CAVI. So, prospective studies are needed in the future to show the causal relationship between CAVI, falls injuries, and frailty.
The strength of our work is that we examined a random sample of a population of people over 60 years of age living in two different regions of Russia. Thus, even those patients who usually do not see a doctor at the clinic took part in the study, which made it possible to more objectively evaluate the impact of CAVI on the risk of fall injuries and frailty. We expect more research to be done on basis of this study in the future.
Conclusion
This cross-sectional study revealed an independent association between high CAVI and fall-related injuries in adults 60 years and older. This suggested that clinicians, especially geriatricians, should pay attention to arterial stiffness of patients with fall-related injuries. Similarly, the patients with high CAVI should be assessed on risk of falls for prevention of fall-related injuries.
Disclosure
The authors report no conflicts of interest in this work. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
References
- Tkacheva ON, Frolove EV, Yahno NN. Geriatrics. Nat Guideline. 2018;163–175.
- Xue Q, Qin MZ, Jia J, Liu JP, Wang Y. Association between frailty and the cardio-ankle vascular index. Clin Interv Aging. 2019;14:735742. doi:10.2147/CIA.S195109
- Cheng MH, Chang SF. Frailty as a risk factor for falls among community dwelling people: evidence from a meta-analysis. J Nurs Scholarsh. 2017;49(5):529536. doi:10.1111/jnu.12322
- Boddaert J, Tamim H, Verny M, Belmin J. Arterial stiffness is associated with orthostatic hypotension in elderly subjects with history of falls. J Am Geriatr Soc. 2004;52(4):568572. doi:10.1111/j.1532-5415.2004.52163.x
- Asmar R. Principles and usefulness of the cardio-ankle vascular index (CAVI): a new global arterial stiffness index. Eur Heart J Suppl. 2017;19(suppl_B):B4B10. doi:10.1093/eurheartj/suw058
- Topouchian J, Labat C, Gautier S, et al. Effects of metabolic syndrome on arterial function in different age groups: the advanced approach to arterial stiffness study. J Hypertens. 2018;36(4):824833. doi:10.1097/HJH.0000000000001631
- Miyoshi T, Ito H. Assessment of arterial stiffness using the cardio-ankle vascular index. Pulse. 2016;4(1):1123. doi:10.1159/000445214
- Shirai K, Utino J, Otsuka K, Takata M. A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb. 2006;13(2):101107. doi:10.5551/jat.13.101
- Turusheva АV, Kotovskaya JV, Frolova EV, Kiseleva GV. Validation of cardio ankle vascular index as a marker of risk of stroke in older adults in St Petersburg and Bashkortostan. Arterial’naya Gipertenziya. 2019;25(3):258–266. doi:10.18705/1607-419X-2019-25-3-258-266
- Tkacheva ON, Runikhina NK, Ostapenko VS, et al. Validation of the questionnaire for screening frailty. Adv Gerontol. 2017;30(2):236–242.
- Subramaniam S, Ima-Nirwana S, Chin KY. Performance of Osteoporosis Self-Assessment Tool (OST) in predicting osteoporosis-a review. Int J Environ Res Public Health. 2018;15(7):1445. doi:10.3390/ijerph15071445
- Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the european society of cardiology and the european society of hypertension: the task force for the management of arterial hypertension of the european society of cardiology and the european society of hypertension [published correction appears in J Hypertens. 2019 Jan;37(1):226]. J Hypertens. 2018;36(10):19532041. doi:10.1097/HJH.000000000000194013
- Mol A, Bui Hoang PTS, Sharmin S, et al. Orthostatic hypotension and falls in older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(5):589597.e5. doi:10.1016/j.jamda.2018.11.003
- Institute of Medicine (US) Division of Health Promotion and Disease Prevention. The Second Fifty Years: Promoting Health and Preventing Disability. Berg RL, Cassells JS, eds. Washington (DC): National Academies Press (US); 1992.
- Orkaby AR, Lunetta KL, Sun FJ, et al. Cross-sectional association of frailty and arterial stiffness in community-dwelling older adults: the framingham heart study. J Gerontol a Biol Sci Med Sci. 2019;74(3):373379. doi:10.1093/gerona/gly134
- Sampaio RA, Sewo Sampaio PY, Yamada M, et al. Arterial stiffness is associated with low skeletal muscle mass in Japanese community-dwelling older adults. Geriatr Gerontol Int. 2014;14(Suppl 1):109114. doi:10.1111/ggi.12206
- Cesari M, Landi F, Vellas B, Bernabei R, Marzetti E. Sarcopenia and physical frailty: two sides of the same coin. Front Aging Neurosci. 2014;6:192. doi:10.3389/fnagi.2014.00192
- Zhang L, Guo Q, Feng BL, et al. A cross-sectional study of the association between arterial stiffness and sarcopenia in chinese community-dwelling elderly using the asian working group for sarcopenia criteria. J Nutr Health Aging. 2019;23(2):195201. doi:10.1007/s12603-018-1147-9
- Koh AS, et al. Sarcopenia and vascular function among community elderly journal of the American. College Cardiol. 2017;69:2051. doi:10.1016/S0735-1097(17)35440-2
- Benetos A. Assessment of arterial stiffness in an older population: the interest of the cardio-ankle vascular index (CAVI). Eur Heart J Suppl. 2017;19(suppl_B):B11B16. doi:10.1093/eurheartj/suw059
- Mozos I, Malainer C, Horbańczuk J, et al. Inflammatory markers for arterial stiffness in cardiovascular diseases. Front Immunol. 2017;8:1058. doi:10.3389/fimmu.2017.01058
- Park S, Lakatta EG. Role of inflammation in the pathogenesis of arterial stiffness. Yonsei Med J. 2012;53(2):258261. doi:10.3349/ymj.2012.53.2.258
- Mitchell GF. Arterial stiffness and hypertension: chicken or egg? Hypertension. 2014;64(2):210214. doi:10.1161/HYPERTENSIONAHA.114.03449
- Gajdova J, Karasek D, Goldmannova D, et al. Pulse wave analysis and diabetes mellitus. A systematic review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2017;161(3):223233. doi:10.5507/bp.2017.028
- Cecelja M, Chowienczyk P. Role of arterial stiffness in cardiovascular disease. JRSM Cardiovasc Dis. 2012;1(4):cvd.2012.012016. doi:10.1258/cvd.2012.012016
- Srikanth V, Beare R, Blizzard L, et al. Cerebral white matter lesions, gait, and the risk of incident falls: a prospective population-based study. Stroke. 2009;40(1):175180. doi:10.1161/STROKEAHA.108.524355
- Xu T, Clemson L, O’Loughlin K, Lannin NA, Dean C, Koh G. Risk factors for falls in community stroke survivors: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(3):563573.e5. doi:10.1016/j.apmr.2017.06.032
- Zheng JJ, Delbaere K, Close JC, Sachdev PS, Lord SR. Impact of white matter lesions on physical functioning and fall risk in older people: a systematic review. Stroke. 2011;42(7):20862090. doi:10.1161/STROKEAHA.110.610360
- Masugata H, Senda S, Inukai M, et al. Association between bone mineral density and arterial stiffness in hypertensive patients. Tohoku J Exp Med. 2011;223(2):8590. doi:10.1620/tjem.223.85
- Avramovski P, Avramovska M, Sikole A. Bone strength and arterial stiffness impact on cardiovascular mortality in a general population. J Osteoporos. 2016;2016:7030272. doi:10.1155/2016/7030272
- Zhang M, Bai L, Kang J, Ge J, Peng W. Links between arterial stiffness and bone mineral density in middle-aged and elderly Chinese individuals: a cross-sectional study. BMJ Open. 2019;9(8):e029946. doi:10.1136/bmjopen-2019-029946
- Nagayama D, Imamura H, Sato Y, et al. Inverse relationship of cardioankle vascular index with BMI in healthy Japanese subjects: a cross-sectional study. Vasc Health Risk Manag. 2016;13:19. doi:10.2147/VHRM.S119646
- Sheehan KJ, O’Connell MD, Cunningham C, Crosby L, Kenny RA. The relationship between increased body mass index and frailty on falls in community dwelling older adults. BMC Geriatr. 2013;13:132. doi:10.1186/1471-2318-13-132
