Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Stroke is a leading cause of death and disability worldwide. Stem cell therapy is an emerging therapeutic modality with evidence of significant benefits in preclinical stroke models. A number of phase I and II clinical trials have now been completed, with several more currently under way. Translation to the bedside, however, remains a long way off, and there are many questions that remain unanswered. This review will summarize the current evidence and ongoing clinical trials worldwide, and explore the challenges to making this a realistic treatment option for the future.
Keywords:
Introduction
Stroke is the second-commonest single cause of death worldwide (after ischemic heart disease), with over 5 million deaths per year globally. It is also the most common cause of adult disability, with 250,000 people in Europe becoming disabled after their first stroke each year. Despite advances in acute care and secondary preventive strategies, stroke remains a major burden on health-care resources worldwide. Thrombolysis with tissue plasminogen activator is now a well-established treatment for acute ischemic stroke and is associated with significant improvements in outcomes. However, its use is limited to a narrow time window of only 4.5 hours from symptom onset, and in the UK only 5% of stroke patients currently receive this treatment.Citation1
Stem cell therapy is an emerging therapeutic modality in the treatment of stroke. Its basis stems from the observation that certain parts of the adult brain are capable of regeneration (a relatively recent discovery).Citation2,Citation3 Neurogenesis in the adult brain has been demonstrated in the dentate nucleus of the hippocampus and the subventricular zone. In a study of patients with ischemic stroke, neurogenesis was demonstrated in the ischemic penumbra, where cells were found to preferentially localize to the vicinity of blood vessels.Citation4 These findings are suggestive of poststroke compensatory neurogenesis, which may contribute to recovery after the insult. While the regenerative capacity of certain parts of the brain has been demonstrated, it is clear that this endogenous repair process is unable to overcome the devastating damage to brain tissue that occurs after acute, severe stroke. Cell-based therapies have the potential to open up new avenues of treatment in this arena. Targets for stem cell therapy include neuroprotective approaches aimed at protecting at-risk tissue during the acute phase of stroke, as well as neuroreparative approaches which may involve direct replacement of damaged brain tissue, or alternatively promotion of the brain’s endogenous repair processes.
Broadly speaking, clinical approaches to stem cell therapy can be divided into “endogenous” and “exogenous” approaches:
The endogenous approach aims to stimulate mobilization of stem cells already present within the individual. Examples of this approach include the use of granulocyte-colony stimulating factor (G-CSF) used to mobilize hematopoietic stem cells into the peripheral blood. G-CSF use has been shown to have both neuroprotective as well as neuroregenerative properties,Citation5,Citation6 and additionally appears to have direct effects beyond simply mobilization of stem cells. Further discussion of this approach is beyond the scope of this article.
The exogenous approach involves transplantation of the patient with stem cells delivered locally (eg, direct intracerebral implantation) or systemically (eg, intravenous or intra-arterial) and may involve in vitro culture of cells for the expansion of cell numbers prior to administration. There is a large body of preclinical data and now mounting data from clinical trials that have utilized exogenous approaches to stem cell therapy for stroke. This review will discuss these, and the challenges posed in translating this therapy to the bedside, in more detail. Of note, the vast majority of work has focused on ischemic rather than hemorrhagic stroke, and therefore we refer to data from ischemic stroke studies, unless stated otherwise.
Stem cell therapy in stroke patients: the challenges
Significant advances have been made in the field of stem cell therapy for stroke, and the potential benefits of such treatments are vast. However, several important questions remain unanswered, and translation to the bedside remains distant. The important areas of uncertainty are discussed below.
Which stem cells should be used?
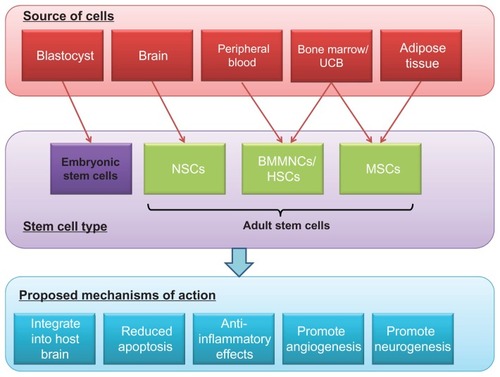
Stem cells can be defined as clonogenic cells that have the capacity to self-renew and differentiate into multiple cell lineages.Citation7 The two major types of stem cells, as classified by source, are embryonic stem cells (ESCs) and adult stem cells (). Human ESCs are pluripotent and are isolated from 5-day-old human blastocysts. However, several factors limit the widespread use of ESCs. These include ethical concerns regarding the use of unwanted embryos and concerns regarding tumorigenicity, specifically the risk of teratoma formation in vivo.Citation8 In contrast to ESCs, adult stem cells are multipotent stem cells that can be obtained from adults as well as children, including from umbilical cord blood. They are present within various organs, including the brain and bone marrow, and have the advantage of being suitable for autologous as well as allogeneic use. Of note, one disadvantage of these cells is that they have less differentiation potential than ESCs.
Figure 1 Stem cell types used in stroke trials, and the proposed mechanisms of action.
A number of different types of stem cells, obtained from different sources, have been shown to improve clinical and radiological outcomes in preclinical models of stroke. The choice of cell type for clinical trial use should consider not only efficacy, but also ease of obtaining the cells, issues regarding cell culture for expansion, need for immunosuppression, and questions regarding dosage. A number of autologous and allogeneic cells have been tested in the preclinical arena. Issues specific to autologous cells include questions regarding extraction of consistent, adequate numbers of cells, as well as potency of the cells obtained (eg, potency may fall with the age of the donor). Allogeneic cells must have the capacity for expansion to provide adequate numbers for widespread use, while ethical issues regarding the source will also need to be considered when using ESCs or fetal tissue, as previously mentioned. Cell-culturing techniques used for autologous or allogeneic cells will need to be consistent and adhere to strict safety criteria (good manufacturing practice). Long-term biological safety of any cell-based therapy is a further area of great importance. There are therefore a host of factors to consider when deciding which cell type is best to use. The different types of cells tested in preclinical studies are discussed in more detail below.
Neural stem/progenitor cells
Neural stem cells (NSCs) have the capacity to differentiate into neurons, astrocytes, and oligodendrocytes. There are a wide variety of sources of exogenous neural stem cells, with much work being done on transplantation of embryonic and fetal-derived NSCs in experimental stroke models.Citation9–Citation13 However, the use of such embryonic or fetal tissue is limited by ethicolegal implications, in addition to important biological questions regarding the long-term risk of teratoma formation by ESCs. The emergence of induced pluripotency, whereby skin fibroblasts from patients can be transformed into ESC-like cells, may overcome the ethical issues of using fetal or embryonic tissue in future studies, while also providing a source of autologous cells, thereby removing any questions regarding immune rejection.Citation14–Citation16
Neural stem cells derived from the adult central nervous system are a possible alternative source of cells for transplantation. Studies have documented the isolation of NSCs from the adult rodent brainCitation17,Citation18 as well as (more recently) the adult human brain.Citation19,Citation20 One study demonstrated that adult NSCs derived from the subventricular zone of young adult rats could survive and migrate towards the lesion in rats with an ischemic stroke following intracisternal administration.Citation21 Electron microscopy examination also suggested that the transplanted cells showed signs of neuronal differentiation.
Although possible in principle, brain biopsies for isolation of adult human NSCs and autologous transplantation poststroke is technically difficult, and no clinical trials utilizing adult NSCs have been undertaken.
Immortalized cell lines
A number of human immortalized cell lines have been shown to improve functional outcomes after experimental stroke in rodent models. These cell lines have the advantage of providing an abundant source of cells for transplantation, available ready-prepared, at the time of a stroke. Biological safety of such cell lines, however, remains a concern in the long term.
The immortalized cell line NTera-2 (NT2) was derived from a human teratocarcinoma.Citation22 After several weeks’ exposure to retinoic acid and mitotic inhibitors, these cells differentiate into postmitotic neuron-like cells, named NT2N cells (also known as hNT neurones).Citation23 Terminal differentiation of these cells only occurs following transplantation into an adult brain.Citation24 The transplantation of NT2N cells into the ipsilateral striatum of ischemic rat brains improved functional recovery, with some parameters of behavioral improvement persisting for up to 6 months post-transplantation. Citation25–Citation27 No evidence of tumorigenicity was found following post-mortem examination of the rats. Citation24
The CTX0E03 cell line developed by ReNeuron (Guildford, UK) is a fetally derived multipotent neural stem cell line that is conditionally immortalized with c-myc-ER, such that proliferation only occurs in the presence of the drug 4-hydroxy-tamoxifen.Citation28 It has been shown to effect a dose-dependent improvement in sensorimotor function in rodent models of middle cerebral artery ischemic stroke when delivered intracerebrally.Citation29
Hematopoietic stem/progenitor cells
Hematopoietic stem cells (HSCs) can be obtained from bone marrow, peripheral blood, or umbilical cord blood. The advantage of such cells is that they are suitable for both autologous as well as allogeneic use, and furthermore are not associated with the ethical issues surrounding ESC or fetally derived stem cells. It is contentious whether these cells can differentiate into neuronal cells. However, preclinical studies of CD34+ cells have shown significant benefits in rodent models of stroke, with evidence of functional improvement as well as reduced infarct volume. Potential disadvantages of these cells include issues with consistency of numbers and potency of cells obtained from the bone marrow, as well as the need for ex vivo expansion of cells, when using umbilical cord blood as the source.
In one study, CD34+ cell transplantation delivered intravenously resulted in increased perilesional angiogenesis and subsequent neurogenesis in mice at 48 hours poststroke.Citation30 A further study investigating direct intracerebral implantation of CD34+ cells 1 week after induced stroke was also able to show evidence of neurogenesis and angiogenesis, with differentiation of transplanted cells into cells expressing markers for neurons, glial cells, and vascular endothelial cells.Citation31
Mesenchymal stem cells
Mesenchymal stem cells (MSCs), also known as bone marrow stromal cells, can be obtained from bone marrow as well as such other sources as adipose tissue. As with HSCs, they are suitable for autologous as well as allogeneic use. One disadvantage of this cell type is the requirement for several weeks of cell culture to generate sufficient numbers, thereby making the use of autologous MSCs in the acute phase of stroke an unviable option.
These cells have shown significant functional benefits in rodent models of stroke in the acute as well as chronic setting (up to 1 month poststroke) and when delivered by a variety of routes (intravenous, intra-arterial and intracerebral).Citation32–Citation35 The mechanism of improvement remains unclear, though promotion of endogenous neurogenesis, reduction of apoptosis, and induction of angiogenesis have been demonstrated in different studies.Citation36,Citation37
Bone marrow mononuclear cells (BMMNCs)
Mononuclear cells obtained from bone marrow contain populations of both mesenchymal and hematopoietic stem cells. They have been shown to reduce neurological deficits as well as infarct size in animal models of stroke.Citation38,Citation39 These cells are easy to obtain from bone marrow, and are suitable for autologous and allogeneic use. Transplantation with HSCs (CD34+ cells) or MSCs provides purer, more concentrated cell populations, though BMMNCs have the advantage of being easier to prepare and separate from bone marrow, making them theoretically more practical, particularly in the acute setting. As with HSCs, there are issues with obtaining consistent numbers of cells from bone marrow aspiration and questions regarding potency of cells, particularly in older patients.Citation40 Potential mechanisms of action include paracrine effects secreting trophic factors (such as vascular endothelial growth factor [VEGF] and stromal cell–derived factor-1), as well as possible immunomodulatory benefits.Citation38,Citation41
What is the mechanism of action?
Elucidation of potential mechanisms of action is vital to the further development of stem cell therapy techniques and ultimately translation to the bedside. There are a number of proposed mechanisms that have been investigated in preclinical stroke models ().
Formation of new neuronal circuitry
There is very little evidence that adult stem cells integrate into the ischemic brain and form functional neurons with adequate synaptic connections. Most studies have shown very limited numbers of engrafted cells, with functional benefits in excess of what would be expected based on the degree of engraftment.Citation10,Citation29
Reduced apoptosis
Following an ischemic stroke, neurons and glia die by a mixture of necrosis and apoptosis. Cell transplantation may elicit a neuroprotective response by rescuing the apoptotic cells, particularly in penumbral tissue. This is likely to be mediated by the secretion and upregulation of certain trophins, such as basic fibroblast growth factor, brain-derived neurotrophic factor, VEGF, glial cell-line-derived factor, and nerve growth factor. Several studies have suggested that a reduction in apoptosis in the ischemic boundary area occurs following cellular therapy that is associated with improved neurological recovery in experimental models.Citation36,Citation42,Citation43
Reduced inflammation
Immunomodulatory effects of transplanted cells may have a role in neuroprotection. Preclinical studies have shown evidence of upregulation of anti-inflammatory cytokines and attenuation of expression of proinflammatory cytokines in both ischemic and hemorrhagic stroke.Citation44,Citation45 If an anti-inflammatory effect is to play an important role, delivery of the cells will need to be in the early stages of the stroke.
Promotion of angiogenesis
Following a stroke, regenerative strategies should be aimed at not only restoration of neural elements but also supporting structures such as blood vessels. Angiogenesis has been demonstrated after cell transplantation with various stem cells, including NSCs,Citation46 CD34+ cells,Citation30,Citation31 and MSCs.Citation37 Direct incorporation of the transplanted cells into new blood vessels has also been demonstrated.Citation30 However, more likely mechanisms of action include the release of VEGF and also the increase in endogenous levels of other factors (such as brain-derived neurotrophic factor and fibroblast growth factor) that play a role in neovascularisation.Citation36,Citation47
Promotion of neurogenesis
Endogenous neurogenesis is increased per se after a stroke, likely reflecting an intrinsic host-repair mechanism.Citation48 Administration of cord blood cells and mesenchymal cells have been reported to enhance endogenous neurogenesis,Citation49 although whether this is likely to be functionally significant is still unclear.
Promotion of other endogenous repair processes
It is possible that transplantation of various stem cells may amplify endogenous plasticity responses, again mediated by the secretion of trophic factors. One study suggested that intracarotid administration of MSCs facilitated host neuronal and synaptic plasticity, with increased synaptophysin expression in the ischemic penumbra.Citation50 Furthermore, axonal sprouting from the nonischemic to the contralateral hemisphere was observed following the intravenous administration of human cord blood cells.Citation51
Other stem/progenitor cells are also increased following cerebral ischemia. Under physiological conditions, a relatively small pool of CD34+ stem/progenitor cells circulates in the peripheral blood. Ischemic stroke is known to increase levels of CD34+ cells (mobilized from the bone marrow) in the peripheral blood.Citation52 In addition, there is evidence that increased CD34+ mobilisation into the peripheral blood in patients with acute ischemic stroke correlates with neurological recovery, with higher counts associated with better recovery. Citation53 Treatment with G-CSF, for example, which mobilizes CD34+ cells into the peripheral circulation, may potentially enhance this endogenous repair mechanism.
Which patients will benefit?
A crucial question for upcoming clinical trials is which patients will benefit from stem cell therapy. The pathological type and anatomical location of the stroke are important issues, which are discussed in more detail below. In addition, demographic differences, in particular differences in age and gender, are also likely to affect how patients respond to treatment.Citation54 The vast majority of preclinical work has been conducted on young, previously healthy, male animals. Elderly patients, who represent the largest subset of stroke victims, may not derive the same benefit as that seen in such animal studies.
As stated previously, the majority of preclinical work has focused on ischemic rather than hemorrhagic strokes. In view of this, the ongoing and completed clinical trials have almost exclusively concentrated on ischemic stroke patients. Of the published clinical trials to date, only one has included any patients with hemorrhagic strokes.Citation55
Within the ischemic stroke subgroup, the majority of preclinical evidence for benefit has been obtained from animal models with predominantly striatal infarcts. A smaller number of trials have investigated cortical models of stroke, with mixed results.Citation13,Citation30,Citation56 Cortical strokes are associated with larger, more damaging infarcts, and it may be that these are too large to effect any repair. A direct comparison between subcortical and cortical infarcts in addition to various doses of cells would be useful in order to optimize patient selection. For example, one preclinical study that compared anatomical location found the benefit of stem cell therapy to be more pronounced in striatal infarcts, rather than larger cortical lesions.Citation57
Further issues to consider when designing clinical trials are stability of patients and associated comorbidities. Patients with larger strokes are commonly medically unwell due to multiple reasons (eg, aspiration pneumonia, cardiac arrhythmias), which could preclude them from entry into acute trials despite being eligible. Furthermore, multiple comorbidities are also likely to affect the response of the patient to stem cell therapy.
What is the optimum timing for treatment?
Preclinical studies have shown benefits of stem cell therapy in both acute and chronic models of stroke. Decisions regarding ideal timing need to take into account the likely mechanism of action. A neuroprotective mechanism would require acute delivery, although graft survival may be affected by the damaging effects of ischemia and reperfusion, mediated via excitotoxic neurotransmitters, free radicals, and other inflammatory mediators.Citation58 If the aim is to enhance endogenous repair mechanisms and inhibit neuronal apoptosis, then acute or subacute delivery would be desirable, as these processes occur predominantly in the first few weeks postischemia.Citation59,Citation60 A neuroreparative approach aiming for direct replacement of damaged tissue with new neuronal circuitry (using intracerebral transplantation), would benefit from a later timescale, once neuroinflammation has subsided.Citation12 Such a strategy would be looking at treatment delivered weeks to months after the stroke, in keeping with ongoing host plasticity during that time.
Future studies will need to address questions regarding timing, with direct comparisons between acute and chronic delivery. One animal study demonstrated significant neurological improvements with intravenous injection of BMMNCs at 24 and 72 hours poststroke, but showed no improvement in animals treated at 7 days poststroke.Citation61 Other studies comparing acute to chronic delivery of cells have shown conflicting results, though there were important differences between these trials in terms of the cells used, animal model, and exact timing of transplantation.Citation62,Citation63 Such comparative data is sparse in the preclinical arena and sorely lacking in the clinical arena, and at present the optimal timing of treatment is yet to be determined.
Which is the best route of delivery?
Studies in the preclinical and clinical settings have used a variety of different routes of stem cell delivery, illustrating the point that the best delivery method remains unclear. Benefits have been seen using direct intracerebral implantation as well as systemic delivery using the intravenous and intra-arterial routes.Citation31,Citation32,Citation34 Intracerebral implantation allows direct delivery of cells to the affected site, but is invasive and may present issues of disrupting the underlying brain tissue. Use of a general anesthetic for intracerebral delivery, particularly in the acute stroke patient, is problematic, though alternatively a local anesthetic can be used. The intravenous route is the safest, easiest route of delivery, though there are issues regarding accumulation of cells in nontarget organs, with only a small proportion reaching the brain.Citation64 The size of the cells used is important in this regard. The intra-arterial route allows more direct delivery of cells, allowing better first-pass delivery while being less invasive than direct surgical implantation.
Decisions regarding the route of delivery will need to take into account issues regarding practicality and safety, as well as cell type/dosage and proposed mechanism of action. The best route of delivery is yet to be determined, and there is a paucity of preclinical data comparing the different available delivery methods. One study of ischemic stroke in rats compared intravenous to intra-arterial delivery of neural progenitor cells. Their data showed superior cell delivery to the ischemic hemisphere with the intra-arterial route.Citation65 However, as mentioned previously, all three modes of delivery have clearly shown benefits in different preclinical studies, which raises the question: is it necessary for cells to enter the brain to have their beneficial effect? More well-designed trials are needed to directly compare different routes of delivery using standardized criteria, in order to help answer these vital questions.
How can transplanted cells be tracked?
Tracking of cells is paramount to improving our understanding of cell migration and mechanisms of action. Currently there is no ideal method of doing this, with the techniques available being suboptimal for a number of reasons.
One commonly employed tracking method in preclinical studies is cell labeling with superparamagnetic iron oxide particles, which allows the anatomical location of transplanted cells to be determined using magnetic resonance imaging (MRI).Citation66,Citation67 Other examples of imaging modalities used to track labeled cells include positron emission tomography (PET), bioluminescence imaging (BLI), and single-photon-emission computed tomography (SPECT).Citation65,Citation68 One drawback of many cell-labeling techniques is the difficulty tracing the labeled cells when they divide, either due to failure of uptake of the label or presence of a weaker signal in the new cells. In addition, if the cell dies and is phagocytosed by macrophages, any signal received will be misleading.Citation69 BLI overcomes this issue, as it picks up luminescence signals emitted from living cells. However, one of the concerns with BLI is poor spatial resolution, an important drawback of this modality.Citation70
To date, only one clinical trial of stem cell therapy in stroke patients has investigated the role of tracking the transplanted cells. A study of BMMNCs labelled with technetium-99m (99mTc) looked at cell homing and uptake using whole-body scintigraphy and SPECT scanning.Citation71 They confirmed the presence of cells in the brain at 2 hours, as well as distribution to the liver, lungs, spleen, kidneys, and bladder. Furthermore, preferential accumulation of radioactivity was seen in the ipsilateral affected hemisphere (compared to the contralateral hemisphere) in all patients at 2 hours postinfusion.
In addition to tracking cells, imaging modalities are also required to evaluate the functional outcome of transplanted cells. Diffusion-weighted MR studies can be used to assess for neovascularization, PET scanning to assess metabolic changes, diffusion-tensor imaging to assess fiber-tract integrity, and functional MRI to assess neuroplasticity. It is likely, therefore, that a combination of imaging modalities will eventually be required to give a better overall assessment of the fate of transplanted cells, in order to further the understanding of their mechanisms of action.
Stem cell therapy in stroke patients: clinical trials
Clinical trials of stem cell therapy in stroke patients are still in their infancy. There have been a number of recent phase I/II trials, primarily investigating the role in ischemic stroke patients. However, these trials have not clearly defined the best cell type, route of delivery, or timing of therapy, and more coordinated research is needed to better answer these uncertainties.
The majority of preclinical work has focused on treatment in the acute or subacute phases of stroke. In contrast, all the early clinical trials have concentrated on chronic stroke patients. There is certainly preclinical evidence pointing to benefit in the chronic subgroup. In addition, patients are more stable and chronic delivery occurs well after the acute inflammatory response has subsided. There are now an emerging number of acute human trials that have also been completed. Reasons for acute delivery of cells have been discussed previously. It is important to note that the pathophysiological processes and proposed mechanisms of action in the acute phase are quite different to the chronic phase of stroke, and it is not possible to extrapolate data gleaned from one setting to the other. Future studies will need to address questions regarding the ideal timing of transplantation.
The currently available clinical trial data utilizing human stem cells will be discussed further, as well as a discussion on ongoing trials, of which there are now several scattered across different centers worldwide.
Chronic stroke trials
NT2N cells
NT2N were the first human cells to be tested in stroke clinical trials. A phase I trial examined the safety of direct stereotactic transplantation of cells into patients with basal ganglia stroke that had occurred 6 months to 6 years previously.Citation72 Twelve patients with stable motor deficits were treated, along with an immunosuppressive regimen of cyclosporine-A due to the allogeneic nature of the treatment. Two doses of cells were used: 2 × 106 and 6 × 106 cells. There was a trend towards improved functional outcome in the four patients who received the higher dose of cells. Autopsy on one patient, who died of myocardial infarction 27 months post-transplantation, showed apparent survival of NT2N cells in the brain.Citation73 Furthermore, PET scanning at 6 months post-transplantation showed increased metabolic activity at the site of infarct in six patients.Citation74 This initial safety trial led to a phase II study assessing the effect of NT2N cell transplantation in 18 patients with a basal ganglia stroke between 1 and 6 years previously.Citation55 Stereotactic cellular transplantation plus two months of rehabilitation (n = 14) was compared to control patients who received rehabilitation alone (n = 4). Six of the 14 patients who received a transplant appeared to show improvement on a standardized stroke scale, but this was not statistically significant against control patients. Of note, this trial included ischemic (n = 9) and hemorrhagic strokes (n = 9).
Mesenchymal stem cells
The extensive preclinical work on MSCs described previously led to a phase I/II clinical trial using autologous culture-expanded MSCs in patients with ischemic middle cerebral artery (MCA)-territory stroke.Citation75 Thirty patients with established stroke (>1 month postinfarct) were randomized to receive MSCs by the intravenous route (n = 5) or no MSCs (n = 15). Cells were extracted by bone marrow aspiration and culture-expanded prior to infusion. There was no cell-related toxicity related to the MSC administration, and the authors suggested that functional improvement may have been better in the transplanted group compared with the control group, although this was not statistically significant. There were no significant differences between the two groups in relation to changes in infarct volume at 1-year follow-up. Following on from this study, the same group conducted a trial looking at the long-term (5-year) effects of MSC transplantation in patients with severe MCA-territory stroke.Citation76 Sixteen patients (versus 36 controls) were treated with intravenously delivered, autologous, culture-expanded MSCs. There was no difference in adverse events between the two groups. Functional outcome appeared to be better in the treated group, with a significantly increased proportion of patients with a modified Rankin score of 0–3, compared to the controls.
A further trial of autologous MSCs administered in ischemic stroke patients, within 6 months of their event, was recently reported.Citation77 Cells were delivered intravenously 36–133 days poststroke, in an open-label study of 12 patients. MSCs were serum-expanded prior to infusion. The treatment was shown to be safe and feasible, with no significant adverse events. Furthermore, mean infarct volume as assessed by MRI was reduced by >20% at 1 week postinfusion. Of note, the culturing conditions and media were different between the two MSC trials described above.
Bone marrow mononuclear cells
Two trials utilising BMMNCs have been reported in chronic stroke patients. One open-label study treated six male patients with MCA-territory ischemic stroke within 90 days of the event.Citation78 Autologous BMMNCs were isolated after bone marrow aspiration. The cells were then delivered intra-arterially, with a proportion of these labeled with 99mTc. There were no treatment-related adverse events up to 6 months follow-up. Evidence was seen of cell migration to the brain at 2 hours postinfusion in all six patients, though at 24 hours this number had dropped to two patients.Citation71 All patients showed improvements in their National Institutes of Health Stroke Scale scores by 6 months. In a separate study, autologous bone marrow stem cells obtained by bone marrow aspiration were transplanted stereotactically in five patients with established stroke.Citation79 The procedure was well tolerated, with no adverse events up to 1 year follow-up.
Ongoing chronic trials
There are at least ten other ongoing or completed trials in chronic (>4 weeks postevent) stroke patients that are yet to report. Details of these unreported trials are listed in . A number of different cell types at different time points and via different methods of delivery are being tested. These include allogeneic cells such as the CTX0E03 neural stem cell line, which has been discussed previously. Such commercially developed cell lines, if shown to be beneficial, are an exciting prospect owing to the ability to develop them for “off the shelf ” use, available ready-prepared at the time of a stroke. The results of these various trials are awaited with interest, though it is clear to see that meaningful comparisons between the different trials will be difficult to make, and how far these trials will go towards answering the outstanding questions in this field is difficult to say.
Table 1 Summary of ongoing or completed (but unreported) chronic stroke trials
Acute stroke trials
Bone marrow mononuclear cells
There are currently three published trials of stem cell therapy in acute stroke patients. All three trials utilized BMMNCs and were able to demonstrate safety and feasibility in the treated subjects. One study treated ischemic stroke (MCA territory) patients at 24–72 hours postevent with intravenously delivered cells.Citation80 Ten patients were treated in an open-label study, with no evidence of study-related serious adverse events up to 6 months follow-up. All patients had shifted down by at least 1 point on the modified Rankin Scale (mRS) at 6 months compared to at day 7. The second study (also open-label) treated 20 patients with MCA-territory ischemic stroke at 3–7 days postevent, with the cells delivered intra-arterially.Citation81 There were no procedure-related adverse events reported up to 6 months follow-up. A good outcome (defined as an mRS of ≤2) was seen in eight of the 20 patients at 90 days. The third, most recently published trial treated ten patients with BMMNCs delivered intra-arterially at 5–9 days after stroke.Citation82 This was a single-blind, controlled study (ten consecutive controls; nonrandomized). Two of the treated patients had isolated partial seizures at 3 months. There were no significant differences in neurological outcome between the two groups at final 180-day follow-up. None of these these trials was powered to demonstrate efficacy.
Ongoing acute/subacute trials
A further six acute/subacute trials (<4 weeks poststroke) are ongoing or yet to report (). As with the chronic stroke trials, these are utilizing a variety of different cell types, including BMMNCs, CD34+ cells, and MSCs, as well as commercially developed stem cell lines. We have investigated the use of intra-arterially delivered CD34+ cells in patients with severe MCA-territory ischemic stroke, recruited within 7 days of the event (ClinicalTrials.gov identifier NCT00535197). To date, no trial has reported on the effects of immunoselected CD34+ cells for acute or chronic ischemic stroke. Such cells have been shown to improve functional outcome and infarct size in preclinical models. Furthermore, a recently published trial of BMMNC treatment in acute ischemic stroke showed a trend towards positive correlation between number of CD34+ cells injected and functional outcome at 1 month.Citation82 We have demonstrated safety and feasibility in our patient cohort, as well as improvements in clinical scores and functional status at 6-month follow-up (unpublished data). Of the other ongoing studies, one is investigating the use of MSCs in hemorrhagic as well as ischemic strokes. This will be of interest, as the use of stem cells for hemorrhagic stroke has not been well investigated in the clinical arena. It must be borne in mind however, that the underlying pathophysiological processes at play and therefore mechanisms of recovery are quite different between these subtypes of stroke. The completed results of these various trials are eagerly awaited.
Table 2 Summary of ongoing or completed (but unreported) acute/subacute stroke trials
The future
Routine use of stem cells at the bedside for stroke patients is an exciting prospect, though realistically remains a long way off. The future may well see the availability of “off-the-shelf ” stem cell products available for immediate use. Perhaps patients will receive individually tailored stem cell products, engineered to secrete specific trophic factors, to suit their specific subtype and duration of stroke. There is clearly a long way to go in both preclinical and clinical research, and long-term biosafety measures will be an essential consideration in this regard.
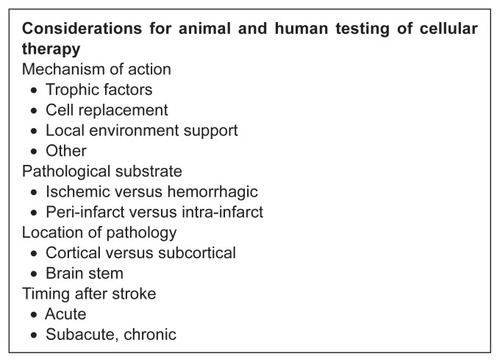
A number of clinical trials have now begun to demonstrate the safety and feasibility of different approaches to stem cell therapy. However, there are a large number of unanswered questions that remain. The great variation in the stem cell trials completed to date means that it is difficult to make any meaningful comparisons between them. Future clinical trials will need to start trying to address the important outstanding questions. It is imperative that trials are therefore designed with this in mind. Careful planning and collaborative work need to take place in order to maximize the likelihood of getting a useful answer from these studies. This includes such considerations as incorporation of a dose-escalation design and comparisons between different methods of delivery as well as different time points for delivery. The Stroke Therapy Academic Industry Roundtable (STAIR) II meeting elucidated the important considerations when designing future phase IIb studies.Citation83 Many of these recommendations are particularly relevant to the field of stem cell research (see ; important factors highlighted). They emphasized that “lack of establishing the optimal dose, duration of therapy, and time window may have contributed to the failure of neuroprotection trials.” Therefore, refinement and identification of the target population is essential. In addition, narrowing selection criteria in phase IIb studies to target patients more likely to respond based on clinical and imaging characteristics may optimize the chances of detecting a biologically relevant drug effect (STAIR IV recommendations).Citation84 Subsequent to these publications, the Stem Cell Therapies as an Emerging Paradigm in Stroke (STEPS) meeting sought to develop a framework specifically to help guide design of future preclinical and clinical studies in the field of cell-based therapies ().Citation85 These recommendations from experts from the preclinical and clinical arenas should be carefully borne in mind before commencing any future trials.
Figure 2 Stroke Therapy Academic Industry Roundtable (STAIR) II recommendations. Adapted from Stroke Therapy Academic Industry Roundtable II (STAIR-II). Recommendations for clinical trial evaluation of acute stroke therapies. Stroke. 2001;32:1598–1606.Citation83
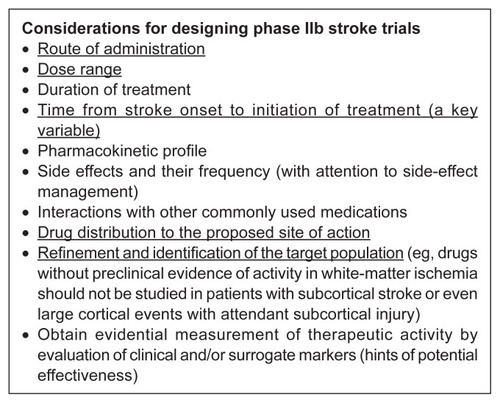
Figure 3 Stem Cell Therapies as an Emerging Paradigm in Stroke (STEPS) recommendations.
Adapted from Stem Cell Therapies as an Emerging Paradigm in Stroke participants. Stem Cell Therapies as an Emerging Paradigm in Stroke (STEPS): bridging basic and clinical science for cellular and neurogenic factor therapy in treating stroke. Stroke. 2009;40:510–515.Citation85
In conclusion, there have been significant advances made in the field of stem cell research over the last two decades, with evidence of significant benefits in both acute and chronic animal models of stroke. Translation to clinical practice, however, remains a long way off. A number of trials are under way, though future work will need to concentrate on overcoming the still-significant challenges standing in the way of this becoming a realistic treatment option for the future.
Contributors
All authors participated in the writing of the manuscript.
Disclosure
All authors are involved in an ongoing clinical trial of autologous CD34+ stem cell therapy in ischemic stroke. Nagy Habib has shares in OmniCyte.
References
- Intercollegiate Stroke Working PartyNational Sentinel Stroke Clinical Audit 2010: Public Report for England, Wales and Northern IrelandLondonRoyal College of Physicians2011
- ErikssonPSPerfilievaEBjork-ErikssonTNeurogenesis in the adult human hippocampusNat Med19984131313179809557
- CurtisMAKamMNannmarkUHuman neuroblasts migrate to the olfactory bulb via a lateral ventricular extensionScience20073151243124917303719
- JinKWangXXieLEvidence for stroke-induced neurogenesis in the human brainProc Natl Acad Sci U S A2006103131981320216924107
- ShyuWCLinSZYangHIFunctional recovery of stroke rats induced by granulocyte colony-stimulating factor–stimulated stem cellsCirculation20041101847185415381647
- SchäbitzWRKollmarRSchwaningerMNeuroprotective effect of granulocyte colony stimulating factor after focal cerebral ischemiaStroke20033474575112624302
- WeissmanILAndersonDJGageFStem and progenitor cells:origins, phenotypes, lineage commitments, and transdifferentiationsAnnu Rev Cell Dev Biol20011738740311687494
- ThomsonJAItskovitz-EldorJShapiroSSEmbryonic stem cell lines derived from human blastocystsScience1998282114511479804556
- ChuKKimMJeongSWKimSUYoonBWHuman neural stem cells can migrate, differentiate, and integrate after intravenous transplantation in adult rats with transient forebrain ischemiaNeurosci Lett200334312913312759181
- ChuKKimMParkKIHuman neural stem cells improve sensorimotor deficits in the adult rat brain with experimental focal ischemiaBrain Res2004101614515315246850
- JeongSWChuKJungKHKimSUKimMRohJKHuman neural stem cell transplantation promotes functional recovery in rats with experimental intracerebral hemorrhageStroke2003342258226312881607
- KellySBlissTMShahAKTransplanted human fetal neural stem cells survive, migrate, and differentiate in ischemic rat cerebral cortexProc Natl Acad Sci U S A2004101118391184415280535
- HicksAULappalainenRSNarkilahtiSTransplantation of human embryonic stem cell-derived neural precursor cells and enriched environment after cortical stroke in rats: cell survival and functional recoveryEur J Neurosci20092956257419175403
- TakahashiKYamanakaSInduction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factorsCell200612666367616904174
- TakahashiKTanabeKOhrukiMInduction of pluripotent stem cells from adult human fibroblasts by defined factorsCell200713186187218035408
- YuJVodyanikMASmuge-OttoKInduced pluripotent stem cell lines derived from human somatic cellsScience20073181917192018029452
- ReynoldsBAWeissSGeneration of neurons and astrocytes from isolated cells of the adult mammalian central nervous systemScience1992255170717101553558
- WachsFPCouillard-DespresSEngelhardtMHigh efficacy of clonal growth and expansion of adult neural stem cellsLab Invest20038394996212861035
- NunesMCRoyNSKeyoungHMIdentification and isolation of multipotential neural progenitor cells from the subcortical white matter of the adult human brainNat Med2003943944712627226
- ArsenijevicYVillemureJGBrunetJFIsolation of multipotent neural precursors residing in the cortex of the adult human brainExp Neurol2001170486211421583
- ZhangZGJiangQZhangRMagnetic resonance imaging and neurosphere therapy of stroke in ratAnn Neurol20035325926312557295
- AndrewsPWDamjanovISimonDPluripotent embryonal carcinoma clones derived from the human teratocarcinoma cell line Tera-2. Differentiation in vivo and in vitroLab Invest1984501471626694356
- PleasureSJLeeVMNTera 2 cells: a human cell line which displays characteristics expected of a human committed neuronal progenitor cellJ Neurosci Res1993355856028411264
- KleppnerSRRobinsonKATrojanowskiJQLeeVMTransplanted human neurons derived from a teratocarcinoma cell line (NTera-2) mature, integrate, and survive for over 1 year in the nude mouse brainJ Comp Neurol19953576186327673487
- BorlonganCVTajimaYTrojanowskiJQLeeVMSanbergPRTransplantation of cryopreserved human embryonal carcinoma-derived neurons (NT2N cells) promotes functional recovery in ischemic ratsExp Neurol19981493103219500961
- BorlonganCVTajimaYTrojanowskiJQLeeVMSanbergPRCerebral ischemia and CNS transplantation: differential effects of grafted fetal rat striatal cells and human neurons derived from a clonal cell lineNeuroreport19989370337099858383
- SaportaSBorlonganCVSanbergPRNeural transplantation of human neuroteratocarcinoma (hNT) neurons into ischemic rats. A quantitative dose-response analysis of cell survival and behavioral recoveryNeuroscience19999151952510366009
- StroemerPHopeAPatelSPollockKSindenJDevelopment of a human neural stem cell line for use in recovery from disability after strokeFront Biosci2008132290229217981710
- StroemerPPatelSHopeAThe neural stem cell line CTX0E03 promotes behavioral recovery and endogenous neurogenesis after experimental stroke in a dose-dependent fashionNeurorehabil Neural Repair20092389590919633272
- TaguchiASomaTTanakaHAdministration of CD34+ cells after stroke enhances neurogenesis via angiogenesis in a mouse modelJ Clin Invest200411433033815286799
- ShyuWCLinSZChiangMFSuCYLiHIntracerebral peripheral blood stem cell (CD34+) implantation induces neuroplasticity by enhancing beta1 integrin-mediated angiogenesis in chronic stroke ratsJ Neurosci2006263444345316571751
- ChenJLiYWangLTherapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in ratsStroke2001321005101111283404
- ShenLHLiYChenJTherapeutic benefit of bone marrow stromal cells administered 1 month after strokeJ Cereb Blood Flow Metab20072761316596121
- LiYChenJWangLLuMChoppMTreatment of stroke in rat with intracarotid administration of marrow stromal cellsNeurology2001561666167211425931
- LiYChoppMChenJIntrastriatal transplantation of bone marrow nonhematopoietic cells improves functional recovery after stroke in adult miceJ Cereb Blood Flow Metab2000201311131910994853
- ChenJLiYKatakowskiMIntravenous bone marrow stromal cell therapy reduces apoptosis and promotes endogenous cell proliferation after stroke in female ratJ Neurosci Res20037377878612949903
- ChenJZhangZGLiYIntravenous administration of human bone marrow stromal cells induces angiogenesis in the ischemic boundary zone after stroke in ratsCirc Res20039269269912609969
- BrennemanMSharmaSHartingMAutologous bone marrow mononuclear cells enhance recovery after acute ischemic stroke in young and middle-aged ratsJ Cereb Blood Flow Metab20103014014919773802
- Giraldi-GuimaraesARezende-LimaMBrunoFPMendez-OteroRTreatment with bone marrow mononuclear cells induces functional recovery and decreases neurodegeneration after sensorimotor cortical ischemia in ratsBrain Res20091266108120
- LiTSKuboMUedaKIdentification of risk factors related to poor angiogenic potency of bone marrow cells from different patientsCirculation2009120Suppl 11S255S26119752376
- SharmaSYangBStrongRBone marrow mononuclear cells protect neurons and modulate microglia in cell culture models of ischemic strokeJ Neurosci Res2010882869287620629187
- KurozumiKNakamuraKTamiyaTMesenchymal stem cells that produce neurotrophic factors reduce ischemic damage in the rat middle cerebral artery occlusion modelMol Ther2005119610415585410
- LladoJHaenggeliCMaragakisNJSnyderEYRothsteinJDNeural stem cells protect against glutamate-induced excitotoxicity and promote survival of injured motor neurons through the secretion of neurotrophic factorsMol Cell Neurosci20042732233115519246
- VendrameMGemmaCde MesquitaDAnti-inflammatory effects of human cord blood cells in a rat model of strokeStem Cells Dev20051459560416305344
- LeeSTChuKJungKHAnti-inflammatory mechanism of intravascular neural stem cell transplantation in haemorrhagic strokeBrain200813161662918156155
- JiangQZhangZGDingGLInvestigation of neural progenitor cell induced angiogenesis after embolic stroke in rat using MRINeuroimage20052869870716112879
- ChengXWangZYangJAcidic fibroblast growth factor delivered intranasally induces neurogenesis and angiogenesis in rats after ischemic strokeNeurol Res20113367568021756545
- ArvidssonACollinTKirikDKokaiaZLindvallONeuronal replacement from endogenous precursors in the adult brain after strokeNat Med2002896397012161747
- NakatomiHKuriuTOkabeSRegeneration of hippocampal pyramidal neurons after ischemic brain injury by recruitment of endogenous neural progenitorsCell200211042944112202033
- ShenLHLiYChenJIntracarotid transplantation of bone marrow stromal cells increases axon-myelin remodeling after strokeNeuroscience200613739339916298076
- XiaoJNanZMotookaYLowWCTransplantation of a novel cell line population of umbilical cord blood stem cells ameliorates neurological deficits associated with ischemic brain injuryStem Cells Dev20051472273316433627
- PaczkowskaELaryszBRzeuskiRHuman hematopoietic stem/progenitor-enriched CD34(+) cells are mobilized into peripheral blood during stress related to ischemic stroke or acute myocardial infarctionEur J Haematol20057546146716313257
- DunacAFrelinCPopolo-BlondeauMNeurological and functional recovery in human stroke are associated with peripheral blood CD34+ cell mobilizationJ Neurol200725432733217345048
- LiuFYuanRBenashskiSEMcCulloughLDChanges in experimental stroke outcome across the life spanJ Cereb Blood Flow Metab20092979280219223913
- KondziolkaDSteinbergGKWechslerLNeurotransplantation for patients with subcortical motor stroke: a phase 2 randomized trialJ Neurosurg2005103384516121971
- HicksAUMacLellanCLChernenkoGACorbettDLong-term assessment of enriched housing and subventricular zone derived cell transplantation after focal ischemia in ratsBrain Res2008123110311218675262
- SmithEJStroemerRPGorenkovaNImplantation site and lesion topology determine efficacy of a human neural stem cell line in a rat model of chronic strokeStem Cells20123078579622213183
- MitsiosNGaffneyJKumarPKrupinskiJKumarSSlevinMPathophysiology of acute ischaemic stroke: an analysis of common signalling mechanisms and identification of new molecular targetsPathobiology20067315917517119345
- HayashiTNoshitaNSugawaraTChanPHTemporal profile of angiogenesis and expression of related genes in the brain after ischemiaJ Cereb Blood Flow Metab20032316618012571448
- CarmichaelSTCellular and molecular mechanisms of neural repair after stroke: making wavesAnn Neurol20065973574216634041
- YangBStrongRSharmaSTherapeutic time window and dose response of autologous bone marrow mononuclear cells for ischemic strokeJ Neurosci Res20118983383921412816
- GrabowskiMJohanssonBBBrundinPSurvival of fetal neocortical grafts implanted in brain infarcts of adult rats: the influence of postlesion time and age of donor tissueExp Neurol19941271261368200430
- DarsaliaVAllisonSJCusulinCCell number and timing of transplantation determine survival of human neural stem cell grafts in stroke-damaged rat brainJ Cereb Blood Flow Metab20113123524220531461
- FischerUMHartingMTJimenezFPulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effectStem Cells Dev20091868369219099374
- LappalainenRSNarkilahtiSHuhtalaTThe SPECT imaging shows the accumulation of neural progenitor cells into internal organs after systemic administration in middle cerebral artery occlusion ratsNeurosci Lett200844024625018572314
- BulteJWDuncanIDFrankJAIn vivo magnetic resonance tracking of magnetically labeled cells after transplantationJ Cereb Blood Flow Metab20022289990712172375
- HoehnMKustermannEBlunkJMonitoring of implanted stem cell migration in vivo: a highly resolved in vivo magnetic resonance imaging investigation of experimental stroke in ratProc Natl Acad Sci U S A200299162671627212444255
- LoveZWangFDennisJImaging of mesenchymal stem cell transplant by bioluminescence and PETJ Nucl Med2007482011202018006616
- McColganPSharmaPBentleyPStem cell tracking in human trials: a meta-regressionStem Cell Rev201171031104021475954
- BlissTAndresRHSteinbergGKOptimizing the success of cell transplantation therapy for strokeNeurobiol Dis20103727528319822211
- Barbosa da FonsecaLMGutfilenBRosado de CastroPHMigration and homing of bone-marrow mononuclear cells in chronic ischemic stroke after intra-arterial injectionExp Neurol201022112212819853605
- KondziolkaDWechslerLGoldsteinSTransplantation of cultured human neuronal cells for patients with strokeNeurology20005556556910953194
- NelsonPTKondziolkaDWechslerLClonal human (hNT) neuron grafts for stroke therapy: neuropathology in a patient 27 months after implantationAm J Pathol20021601201120611943704
- MeltzerCCKondziolkaDVillemagneVLSerial [18F] fluorodeoxyglucose positron emission tomography after human neuronal implantation for strokeNeurosurgery200149586591 discussion 591–59211523668
- BangOYLeeJSLeePHLeeGAutologous mesenchymal stem cell transplantation in stroke patientsAnn Neurol20055787488215929052
- LeeJSHongJMMoonGJA long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic strokeStem Cells2010281099110620506226
- HonmouOHoukinKMatsunagaTIntravenous administration of auto serum-expanded autologous mesenchymal stem cells in strokeBrain2011134Pt 61790180721493695
- BattistellaVFreitasGDiasVSafety of autologous bone marrow mononuclear cell transplantation in patients with nonacute ischemic strokeRegen Med20116455221175286
- Suárez-MonteagudoCHernández-RamírezPAlvarez-GonzálezLAutologous bone marrow stem cell neurotransplantation in stroke patients. An open studyRestor Neurol Neurosci20092715116119531871
- SavitzSIMisraVKasamMIntravenous autologous bone marrow mononuclear cells for ischemic strokeAnn Neurol201170596921786299
- FriedrichMIntra-arterial infusion of autologous bone-marrow mononuclear cells in patients with moderate to severe middle-cerebralartery acute ischemic strokeCell Transplant201221Suppl 11321
- MonicheFGonzalezAGonzalez-MarcosJRIntra-arterial bone marrow mononuclear cells in ischemic stroke: a pilot clinical trialStroke2012432242224422764211
- Stroke Therapy Academic Industry Roundtable II (STAIR-II)Recommendations for clinical trial evaluation of acute stroke therapiesStroke2001321598160611441207
- FisherMAlbersGWDonnanGEnhancing the development and approval of acute stroke therapies: Stroke Therapy Academic Industry RoundtableStroke2005361808181316020764
- Stem Cell Therapies as an Emerging Paradigm in Stroke participants. Stem Cell Therapies as an Emerging Paradigm in Stroke (STEPS): bridging basic and clinical science for cellular and neurogenic factor therapy in treating strokeStroke20094051051519095993