Abstract
Background
The inferior vena cava (IVC) diameter and degree of inspiratory collapse are used as echocardiographic indices in the estimation of right atrial pressure. Brain-natriuretic peptides (BNPs) are established biomarkers of myocardial wall stress. There is no information available regarding the association between the IVC diameter and BNPs in patients with heart failure and various degrees of systolic performance. The purpose of this investigation is to quantify the degree to which natriuretic peptides (BNP and N-terminal pro-B natriuretic peptide [NT-ProBNP]) and echocardiographic-derived indices of right atrial pressure correlate in this patient population.
Methods
We examined 77 patients (mean age 61 ± 17 years, 44% male) with decompensated heart failure who underwent transthoracic echocardiography and, within a timeframe of 24 hours, determination of BNP and NT-ProBNP levels in venous blood. BNP and NT-ProBNP were analyzed after log transformation. The degree of association was measured by the correlation coefficient using the Pearson’s method.
Results
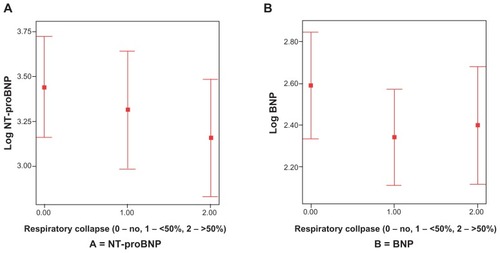
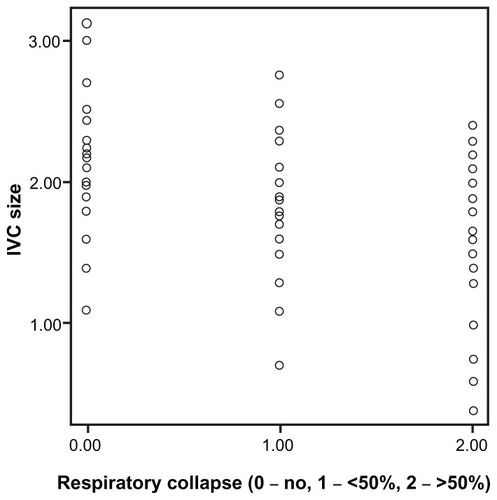
The mean ejection fraction was 50% ± 20%, and 33% of the study cohort had a remote history of heart failure. The mean IVC diameter was 1.85 cm ± 0.5, the mean BNP was 274 pg/mL, the confidence interval (CI) was 95% (95% CI: 197–382), and the mean NT-ProBNP was 1994 pg/mL (95% CI: 1331–2989). There was a positive, albeit small, association between IVC diameter and BNP (r = 0.24, 95% CI: 0.01–0.44; P = 0.03) and NT-ProBNP (r = 0.27, 95% CI: 0.05–0.47; P = 0.01). Among patients with different degrees of IVC collapse in response to inspiration, values for BNP and NT-ProBNP did not differ substantially (P = 0.36 and 0.46 for BNP and NT-ProBNP, respectively).
Conclusion
Natriuretic peptides correlate weakly with IVC size and do not predict changes in response to intrathoracic pressure.
Background
Congestive heart failure is a leading cause of morbidity and mortality worldwide.Citation1 In the USA, over 1,000,000 patients are admitted each year with this diagnosis and 5,000,000 live with the disease, at a cost of 27.9 billion dollars, which represents the costliest Medicare expenditure.Citation2,Citation3
Accurate estimation of volume status is of paramount importance in the management of acutely decompensated heart failure (ADHF), as patients with elevated filling pressures prior to discharge have higher rehospitalization rates.Citation4 Physical examination is inaccurate in estimating filling pressures, and invasive hemodynamic monitoring is infrequently used in the management of patients with ADHF.Citation5,Citation6
Brain natriuretic peptides (BNPs) and echocardiography are commonly used in clinical practice to assess patients with ADHF. BNP and its precursor, N-terminal pro-B natriuretic peptide (NT-ProBNP), are released in response to myocardial wall stress and correlate well with pulmonary capillary pressure.Citation7,Citation8 Echocardiography provides information regarding systolic and diastolic properties, left- and right-sided filling pressures, pulmonary artery pressure, and cardiac output.Citation9
The purpose of this investigation was to quantify the degree to which natriuretic peptides (BNP and NT-ProBNP) and echocardiographic-derived indices of right atrial pressure correlate in patients with ADHF.
Methods
Patients
Eligible patients were retrospectively identified from our cardiac biomarker and echocardiography electronic databases using unique patient identifiers.
Inclusion criteria
Patients were eligible for participation in the study if they underwent echocardiographic and biomarker evaluation within 24 hours of each other for the management and/or diagnosis of heart failure at the University of Minnesota Medical Center during the study period from June 1 to December 1, 2006. The setting in which patients underwent echocardiography and biomarker evaluation was the coronary care or telemetry unit (88%), or the emergency department (12%). For inpatients with more than one biomarker and/or echocardiogram assessment during the index admission, only the one performed within 48 hours of hospital admission was considered for the study.
Exclusion criteria
Patients with severe left ventricular systolic dysfunction (ejection fraction [EF] <35%), left ventricular assist devices, and transplant recipients were excluded. Patients with acute coronary syndromes or receiving positive pressure ventilation or inotropic agents were also excluded. The study was approved by the Institutional Review Board and Ethics Committee at the University of Minnesota.
Echocardiography and biomarkers
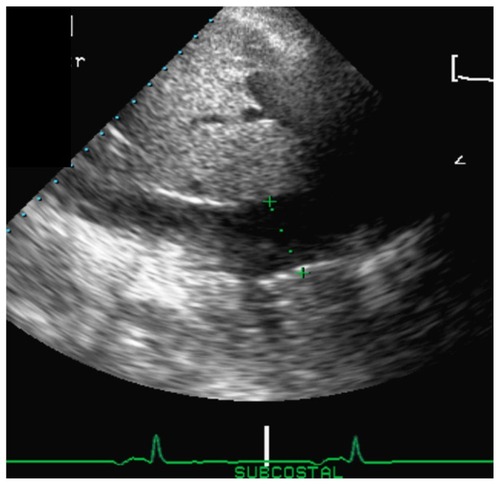
Echocardiography was performed by trained sonographers using a transthoracic approach in the standard parasternal, apical, and subcostal views. Two investigators blinded to biomarker levels reviewed all echocardiograms. Cardiac chamber dimensions were estimated from the parasternal long-axis view using two-dimensional (2D)-guided linear measurements, as recommended by the American Society of Echocardiography (ASE).Citation10 Right ventricular (RV) function was qualitatively assessed after integration of multiple views, as recommended by the ASE. The main criterion used to assess RV function was the degree of tricuspid annulus displacement toward the apex in systole (normal displacement is 1.5–2 cm).Citation10 RV systolic pressure was determined by measuring the peak velocity of the tricuspid regurgitation jet using multiple views. Inferior vena cava (IVC) dimension was measured from a subcostal view 1 cm from the junction between the IVC and the right atrium during quiet respiration (). Changes in IVC dimension in response to respiration were described as collapse ≥ 50% or <50%, or no change. The NT-ProBNP and BNP levels were measured using commercially available immunoassays (Elecsys proBNP; Roche Diagnostics, Basel, Switzerland and Triage BNP Test; Biosite Diagnostics, San Diego, CA, respectively).
Statistical analysis
The baseline characteristics of study patients are presented as percentages for dichotomous variables and mean ± standard deviation (SD), or median ± with interquartile ranges for continuous variables, as appropriate. BNP and NT-ProBNP values were analyzed after log transformation. The degree of association between IVC size and biomarkers was measured by the correlation coefficient using the Pearson’s method and depicted in scatter plots. Analysis of variance was used to perform comparisons across the three groups of IVC collapse. Interobserver agreement between the two readers was assessed in 20 patients using the κ statistic, an index that compares agreement against what might be expected by chance. Possible values range from 1 (perfect agreement) via 0 (no agreement above that expected by chance) to −1 (complete disagreement). The software programs SPSS (version 11.0; SPSS Inc, Chicago, IL) and MedCalc for Windows (version 9.5.0.0; MedCalc Software, Mariakerke, Belgium) were used for data analysis.
Results
Baseline characteristics
The mean age (±SD) of the study group was 61 ± 17 years and 44% were male. A third of the group had a remote history of congestive heart failure or coronary artery disease.
At presentation, 57% had worsening dyspnea (functional class III–IV), and virtually all patients (99%) showed one or more physical signs of decompensated heart failure upon examination. These included crackles (17%), lower extremity edema (49%), third heart sound (S3) (3.5%), and elevation in jugular venous pressure (30%).
The mean ejection fraction, end-systolic dimension, and left atria size were 50% ± 20%, 34 ± 13 mm, and 43 ± 9 mm, respectively. Background medical therapies at the time of presentation included beta-blockers (54%), diuretics (64%), angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (35%). Other baseline clinical, laboratory, and echocardiographic characteristics are described in and .
Table 1 Baseline characteristics of the study cohort (n = 77)
Table 2 Echocardiographic characteristics of study patients (n = 77)
Inferior vena cava and biomarker assessment
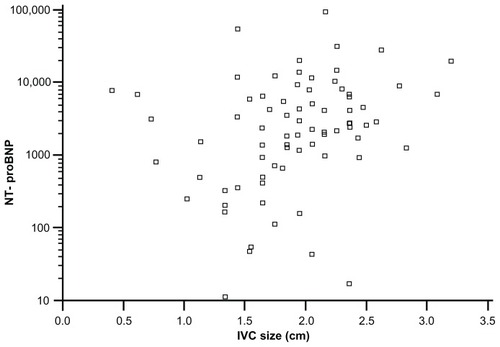
Interobserver agreement for IVC size and collapsibility measurements was very good (κ = 0.85 and 0.88, respectively). The mean IVC diameter was 1.85 ± 0.5 cm, the mean BNP was 274 pg/mL (95% CI: 197–382), and the mean NT-ProBNP was 1994 pg/mL (95% CI: 1331–2989). There was a positive correlation between IVC diameter and both BNP and pro-BNP. The correlation coefficient for BNP, as it relates to IVC diameter (), was 0.24 (95% CI: 0.01–0.44; P = 0.03). The correlation coefficient for NT-ProBNP and IVC diameter () was 0.27 (95% CI: 0.05–0.47; P = 0.01).
Figure 2 Scatter plot of log-transformed brain natriuretic peptide (BNP) and inferior vena cava size (IVC).
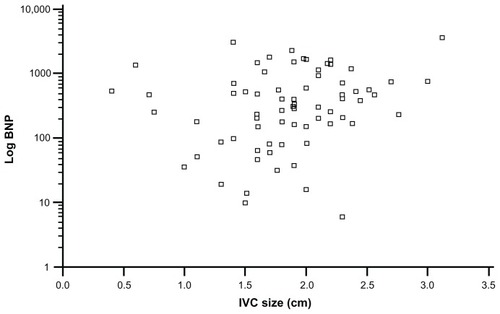
Figure 3 Scatter plot of log-transformed N-terminal pro-brain natriuretic peptide (NT-ProBNP) and inferior vena cava size (IVC).
Subgroup analysis stratified by sex showed a more robust association between natriuretic peptides and IVC size among men (correlation coefficient for BNP was 0.33, P = 0.05; and for NT-proBNP it was 0.36; P = 0.03) when compared to women (correlation coefficient for BNP was 0.14, P = 0.35; and for NT-proBNP it was 0.17; P = 0.27).
Values for BNP and NT-ProBNP overlapped substantially across different IVC collapsibility subgroups (; P = 0.36 and 0.46 for BNP and NT-ProBNP, respectively). In contrast, baseline IVC diameter correlated well with variations in IVC size in response to changes in intrathoracic pressure (correlation coefficient = 0.46, P < 0.001; ).
Discussion
In this cohort of patients with acute heart failure and preserved or mildly reduced systolic function, we found a positive association between the natriuretic peptides BNP and NT-ProBNP, and IVC size. In contrast, neither BNP nor NT-ProBNP showed a good correlation with the response of the IVC to changes in intrathoracic pressure. Using the 100r2 formula, which is the percentage of the variability of the data that is explained by the association of the two variables, it can be concluded that biomarkers explain less than 10% of the variability in IVC dimensions without major differences between BNP and NT-ProBNP. Citation10 The results of this study suggest that commonly used indices of right atrial pressure (IVC size and response to respiration) and left ventricular end-diastolic pressure (natriuretic peptides) complement each other by providing information about filling pressures in both heart chambers.
Among patients with systolic heart failure, BNP has been shown to correlate with IVC size.Citation11 The magnitude of this association was stronger with systolic heart failure patients than in our study of patients with preserved or mildly reduced ejection fraction. This phenomenon, whereby echocardiography-derived indices of filling pressures perform better among patients with systolic dysfunction, has been reported previously for E/e’ and other indices of pulmonary capillary pressure.Citation12 Alternatively, patients with better preserved EF may not have as much elevation in right atrial pressure as those with systolic heart failure, despite the presence of RV diastolic dysfunction.Citation13
The finding of a lack of correlation between natriuretic peptides and IVC among women is interesting, although caution is advised when interpreting this finding due to the small sample size (type II statistical error). This finding needs to be confirmed in larger studies.
The mechanism underlying increased natriuretic peptides in females is unclear, although Redfield et al reported 21% higher BNP levels in women taking hormone replacement therapy, which may suggest that estrogens play a role in the increased levels.Citation14
The IVC is a compliant intra-abdominal vessel that changes in diameter in response to fluctuations in right atrial pressure and volume overload.Citation15 As shown in our study, the degree of IVC collapse in response to intrathoracic pressure correlates with baseline IVC diameter, and when used in conjunction with IVC size provides an accurate, noninvasive estimation of right atrial pressure.Citation16 A rapid assessment of IVC physiology could be performed at the bedside by a noncardiologist and also in the emergency department for patients with unexplained dyspnea.Citation17,Citation18
BNP and NT-ProBNP are useful in the diagnosis of ADHF and provide independent prognostic information that allows optimization of medical therapies.Citation7,Citation8,Citation19,Citation20 Both natriuretic peptides and echocardiography are routinely used in the management of patients with decompensated heart failure.Citation21 Our data suggests that natriuretic peptides and echocardiography provide complementary data with regard to the status of right- and left-sided filling pressures.
Limitations
Our study has several limitations intrinsic to this type of study design (retrospective chart review). First, invasive hemodynamic measurement was not routinely applied in our study population. Second, the majority of the patients included in the study were hospitalized with decompensated heart failure at the time of the study. Therefore, the association between natriuretic peptides and IVC dimension described may not apply to an outpatient, compensated heart failure cohort. Third, we did not perform serial IVC or biomarker measurements, nor did we collect information regarding medication administration that could potentially influence both natriuretic peptides and IVC size (ie, diuretics) during the index admission. Therefore, we are unable to comment on any dynamic changes that may occur between IVC size and natriuretic peptides during the treatment of ADHF. Finally, elevation in natriuretic peptides is not solely a reflection of cardiac filling pressures.Citation22,Citation23 Factors known to have an impact on natriuretic peptides, such as age, sex, creatinine clearance, and body mass index, could have influenced our results and may explain the weak correlation between natriuretic peptides and IVC size and collapsibility.
Conclusion
Among patients with acutely decompensated heart failure, natriuretic peptides correlate weakly with IVC size and do not predict changes in response to intrathoracic pressure. These data suggest a complementary role for right-sided echocardiography and biomarker evaluation.
Disclosure
The authors report no conflict of interest in this work.
References
- YusufSReddiSÔunpuuSAnandSGlobal burden of cardiovascular diseases. Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanizationCirculation20011042746275311723030
- HuntSAAbrahamWTChinMHACC/AHA 2005 guideline update for the diagnosis and management of heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) Available from: http://www.acc.org/clinical/guidelines/failure/index.pdfAccessed on March 20, 2012
- MassieBMShahNBEvolving trends in the epidemiologic factors of heart failure: rationale for preventing strategies and comprehensive disease managementAm Heart J19971337037129200399
- WhalleyGADoughtyRNGambleGDPseudonormal mitral filling pattern predicts hospital re-admission in patients with congestive heart failureJ Am Coll Cardiol2002391787179512039492
- WangCSFitzGeraldMSchulzerMDoes this dyspneic patient in the emergency department have congestive heart failure?JAMA20052941944195616234501
- WienerRSWelchGTrends in the use of the pulmonary artery catheter in the United States, 1993—2004JAMA200729842342917652296
- LainchburyJGCampbellEFramptonCMYandleTGNichollsMGRichardsAMBrain natriuretic peptide and n-terminal brain natriuretic peptide in the diagnosis of heart failure in patients with acute shortness of breathJ Am Coll Cardiol200342472873512932611
- MaiselASMcCordJNowakRMBreathing Not Properly Multinational Study InvestigatorsBedside B-Type natriuretic peptide in the emergency diagnosis of heart failure with reduced or preserved ejection fraction. Results from the Breathing Not Properly Multinational StudyJ Am Coll Cardiol200341112010201712798574
- KirkpatrickJNVannanMANarulaJLangRMEchocardiography in heart failure: Applications, utility, and new horizonsJ Am Coll Cardiol20075038139617662389
- LangRMBierigMDevereuxRBRecommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of CardiologyJ Am Soc Echocardiogr2005181440146316376782
- PudilRTichyMPrausRBlahaVVojacekJNT-proBNP and echocardiographic parameters in patients with acute heart failureActa Medica (Hradec Kralove)2007501515617654836
- OmmenSRNishimuraRAAppletonCPClinical utility of doppler echocardiography and tissue-doppler imaging in the estimation of left ventricular filing pressures: a comparative simultaneous doppler-catheterization studyCirculation20001021788179411023933
- YuCMSandersonJEChanSYeungLHungYTWooKSRight ventricular diastolic dysfunction in heart failureCirculation199693150915148608618
- RedfieldMMRodehefferRJJacobsenSJMahoneyDWBaileyKRBurnettJCPlasma brain natriuretic peptide concentration: impact of age and genderJ Am Coll Cardiol20024097698212225726
- SteinJHNeumannAMarcusRHComparison of estimates of right atrial pressure by physical examination and echocardiography in patients with congestive heart failure and reasons for discrepanciesAm J Cardiol199780161516189416951
- KirscherBJHimelmanRBSchillerNBNoninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cavaAm J Cardiol1990664934962386120
- KimuraBJShawDJAganDLAmundsonSAPingACDeMariaANValue of a cardiovascular limited ultrasound examination using a hand-carried ultrasound device on clinical management in an outpatient medical clinicAm J Cardiol200710032132517631091
- JangTAubinCNaunheimRCharDUltrasonography of the internal jugular vein in patients with dyspnea without jugular venous distension on physical examinationAnn Emerg Med200444216016815278091
- HartmannFPackerMCoatsAJPrognostic impact of plasma N-terminal pro-brain natriuretic peptide in severe chronic congestive heart failure: a sub-study of the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) trialCirculation20041101780178615381643
- GackowskiAIsnardRGolmardJLComparison of echocardiography and plasma B-type natriuretic peptide for monitoring the response to treatment in acute heart failureEur Heart J2004201788179615474693
- GoonewardenaSNGemignaniARonanAComparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failureJACC Cardiovasc Imaging2008159560119356487
- DanielsLBMaiselALNatriuretic peptidesJ Am Coll Cardiol2007502357236818154959
- GalaskoGIWLahiriABarnesSCCollisonPSeniorRWhat is the normal range for N-terminal pro-brain natriuretic peptide? How well does this normal range screen for cardiovascular disease?Eur Heart J2005262269227616040618