Abstract
β-blockers are effective antihypertensive agents and, together with diuretics, have been the cornerstone of pioneering studies showing their benefits on cardiovascular morbidity and mortality as a consequence of blood pressure reduction in patients with hypertension. However, evidence from recent meta-analyses have demonstrated no benefit afforded by atenolol compared with placebo in risk of mortality, myocardial infarction, or stroke, and a higher risk of mortality and stroke with atenolol/propranolol compared with other antihypertensive drug classes. Thus, the effect of these agents on cardiovascular morbidity and mortality in hypertensive patients, especially their use in uncomplicated hypertension, has remained largely controversial. However, it is recognized that the clinical studies used in these meta-analyses were mainly based on the older second-generation β-blockers, such as atenolol and metoprolol. Actually, considerable heterogeneity in, eg, pharmacokinetic, pharmacological, and physicochemical properties exists across the different classes of β-blockers, particularly between the second-generation and newer third-generation agents. Carvedilol is a vasodilating noncardioselective third-generation β-blocker, without the negative hemodynamic and metabolic effects of traditional β-blockers, which can be used as a cardioprotective agent. Compared with conventional β-blockers, carvedilol maintains cardiac output, has a reduced prolonged effect on heart rate, and reduces blood pressure by decreasing vascular resistance. Studies have also shown that carvedilol exhibits favorable effects on metabolic parameters, eg, glycemic control, insulin sensitivity, and lipid metabolism, suggesting that it could be considered in the treatment of patients with metabolic syndrome or diabetes. The present report provides an overview of the main clinical studies concerning carvedilol administered as either monotherapy or in combination with another antihypertensive or more frequently a diuretic agent, with particular focus on the additional benefits beyond blood pressure reduction.
Introduction
Arterial hypertension is a major risk factor for stroke, coronary events, and renal failure.Citation1–Citation3 Current estimates suggest that over 70 million adults in the United States and approximately one billion adults worldwide have hypertension.Citation4,Citation5 These poor figures can be attributed to undetected hypertensive patients (blood pressure [BP] never previously measured), known but untreated hypertension, and known hypertensive patients with low adherence to both antihypertensive drug therapies and lifestyle recommendations.Citation4,Citation6
Due to the need to obtain BP normalcy, guidelines published by the European Society of Hypertension/European Society of Cardiology recommend initiation of monotherapy in patients with baseline first-degree arterial hypertension, mild/moderate global cardiovascular risk, or a target BP < 140/90 mmHg, while combination therapy is suggested in patients with baseline second-degree or more arterial hypertension, high or very high global cardiovascular risk, or a target BP < 130/80 mmHg. Combination therapy is particularly recommended when monotherapy fails to reach BP goals or in patients at high global cardiovascular risk.Citation1–Citation3
For the past four decades, β-blockers have been used to treat hypertension.Citation7,Citation8 These agents have been shown to reduce cardiovascular-related mortality in clinical trials, and following these observations, both the European Society of Hypertension/European Society of Cardiology and JNC-7 guidelines recommend use of β-blockers as first-line or second-line antihypertensive agents.Citation1–Citation3
However, in recent years the use of β-blockers (especially for uncomplicated hypertension) has been controversial and widely debated.Citation9–Citation12 This has been mainly due to the findings from meta-analyses and clinical trials demonstrating a lack of benefit from β-blockers compared with placebo or other antihypertensive agents.Citation13–Citation19 Following this, the National Institute for Health and Clinical Excellence hypertension guidelines in the UK downgraded the use of β-blockers from first-line agents for hypertension to fourth-line add-on therapy.Citation20,Citation21 More recent National Institute for Health and Clinical Excellence guidelines state that β-blockers are not a preferred initial therapy for hypertension, but may be considered in younger people, particularly those with an intolerance or contraindication to angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers, women of child-bearing potential, and people with evidence of increased sympathetic drive.Citation22
Although conclusions drawn from these meta-analyses and later incorporated into the hypertension guidelines appear to cast β-blockers in a poor light, it needs to be pointed out that there were some limitations in these studies that may in part account for the poor effects observed. Atenolol was used in many of these studies as a once-daily dose, whereas ideally it should be taken more frequently, based on its pharmacokinetic properties.Citation23 In addition, the majority of trials included elderly patients, who are recognized to be not as responsive to β-blockers as younger patients.Citation24 However, the major critical weakness lies in the fact that most of the studies included older “traditional” agents (eg, propranolol and atenolol) that have no vasodilatory effects. This observation is extremely important, given that β-blockers are not a homogeneous class and exert markedly different effects according to their individual physicochemical and pharmacological characteristics.Citation20
In fact, current JNC-7 guidelines recommend use of β-blockers for the initial treatment of patients with stage 1 hypertension and compelling indications, eg, previous myocardial infarction, ischemic heart disease, heart failure, diabetes, or high risk of coronary artery disease.Citation1 Furthermore, β-blockers are also recommended for initial treatment in patients with stage 1 hypertension without compelling indications and in patients with stage 2 hypertension who require a combination of drugs to achieve BP control.Citation1
Third-generation vasodilating β-blockers such as celiprolol, carvedilol, and nebivolol, do not possess some of the unfavorable effects often associated with other β-blocker compounds.Citation3 These newer drugs reduce BP as well if not better than other antihypertensive agents.Citation25,Citation26 It is also recognized that vasodilating β-blockers have a favorable metabolic and tolerability profile compared with older traditional β-blockers.Citation7,Citation27,Citation28 Furthermore, both carvedilol and nebivolol have been used in outcome studies of chronic heart failure and were shown to reduce the primary endpoint of mortality and hospitalization.Citation29
With regard to carvedilol, the antihypertensive and ancillary benefits conferred by this vasodilating β-blocker are worth highlighting. Compared with other antihypertensive drugs, carvedilol has been shown to achieve superior or comparable BP reduction in hypertensive patients, whether administered as monotherapy (25 mg/day)Citation25,Citation26,Citation30 or in combination with another antihypertensive agent, such as a diuretic.Citation31,Citation32 Additional benefits afforded by carvedilol include: its use in specific hypertensive patients at risk of coronary artery disease, where it has been shown to increase coronary flow reserve;Citation33,Citation34 the post-myocardial infarction setting, where carvedilol is indicated;Citation35 and in patients with diabetes or metabolic syndrome, in whom carvedilol has favorable metabolic characteristicsCitation36 in addition to providing renal protection.Citation37,Citation38 This review article summarizes the main findings from clinical studies examining the pharmacologic and metabolic properties of carvedilol in hypertension and concomitant diseases.
Mode of action
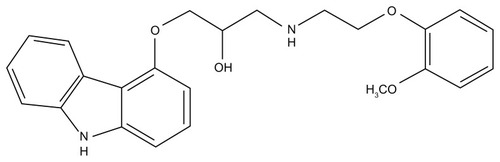
Carvedilol is a racemic mixture of (±)-1-(carbazol-4- yloxy)-3-[[2-(o-methoxyphenoxy) ethyl]amino]-2-propanol (). It is a lipophilic vasodilating noncardioselective β-blocker which lacks intrinsic sympathomimetic activity, thus having improved tolerability compared with older β-blockers.Citation28,Citation39 Carvedilol is absorbed rapidly following oral administration and is extensively metabolized in the liver.Citation40 The older generation “traditional” β-blockers selectively antagonize β1-adrenergic receptors or antagonize both β1-adrenergic and β2-adrenergic receptors.Citation41 They also reduce BP mainly through a reduction in cardiac output, while systemic vascular resistance remains largely unchanged.Citation9 In contrast, carvedilol blocks norepinephrine binding to α1-adrenergic receptors in addition to both β1-adrenergic and β2-adrenergic receptors.Citation28,Citation39,Citation42 This results in a reduction in arterial BP by maintaining cardiac output and decreasing total β-adrenoreceptor vasoconstrictor tone.Citation9,Citation43 Therefore, as can be seen in , the hemodynamic effect exerted by carvedilol is similar to that of angiotensin-converting enzyme inhibitors and markedly superior to that of traditional β-blockers.
Table 1 Effects of different antihypertensive drugs in hypertensive patients
In addition to its BP-reducing effects, carvedilol also has a superior metabolic profile in terms of lipid and glucose metabolism compared with traditional β-blockersCitation44 (). This specific effect is addressed in further detail later in this review. In addition, carvedilol also exerts antioxidant effects attributable to stimulation of nitric oxide production, as well as having anti-inflammatory effects.Citation39,Citation45,Citation46
BP-lowering as monotherapy
Regardless of the drug employed, monotherapy allows achievement of BP target values in a limited number of hypertensive patients.Citation2,Citation3 Carvedilol is indicated for the treatment of essential hypertension. It can be administered alone or in combination with other antihypertensives, particularly with a thiazide diuretic.
Early studies have shown that single administration of carvedilol 25–50 mg results in a consistent reduction in BP over 24 hours compared with placebo, confirming its activity throughout daily activity and sleeping periods.Citation47,Citation48 Approximately 90% of the peak reduction in BP is observed at the time of the next dose.
In addition, clinical studies have shown that carvedilol 25 mg once daily decreases arterial BP to a greater extent than the traditional β-blocker, atenolol, in patients with moderate and essential hypertension, respectively.Citation49,Citation50
Furthermore, comparative studies have also shown that carvedilol reduces BP to a similar extent as other antihypertensive drugs in patients with essential hypertension. A review by Moser et al reported data from three different studies with carvedilol compared with captopril, an angiotensin-converting enzyme inhibitor, slow-release nifedipine, a long-acting calcium channel blocker, and hydrochlorothiazide, a diuretic.Citation51 The extent of BP reduction with carvedilol was similar to that achieved by comparator drugs ().
Figure 2 Antihypertensive effect of carvedilol compared with captopril, slow-release nifedipine, hydrochlorothiazide, and nebivolol. (A) Carvedilol was administered at 25–50 mg once daily. Captopril was administered at 25–50 mg twice daily. Slow-release nifedipine was administered at 20–40 mg twice daily and hydrochlorothiazide was administered at 25–50 mg once daily. Reprinted by permission from Macmillan Publishers Ltd: American Journal of Hypertension. Moser M, Frishman W. Results of therapy with carvedilol, a beta-blocker vasodilator with antioxidant properties, in hypertensive patients. Am J Hypertens. 1998;11(1 Pt 2):15S–22S. Copyright 1998.Citation51 (B) Antihypertensive effect of carvedilol 5 mg/day versus nebivolol 5 mg/day. Copyright (c) 2011, Aves Yayincilik. Adapted with permission from Erdoğan O, Ertem B, Altun A. Comparison of antihypertensive efficacy of carvedilol and nebivolol in mild-to-moderate primary hypertension: a randomized trial. Anadolu Kardiyol Derg. 2011;11(4):310–313. Turkish.Citation30
Abbreviations: SR-Nifedip, slow-release nifedipine; Carved, carvedilol; HCTZ, hydrochlorothiazide.
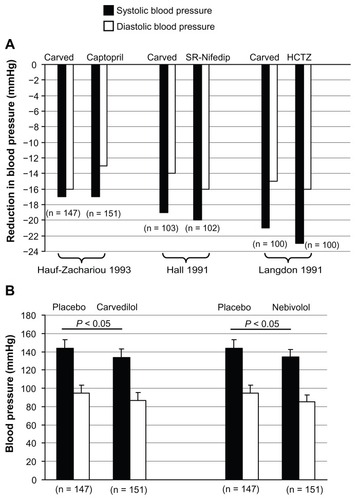
In addition, a more recent clinical trial examined the antihypertensive effect of carvedilol 25–50 mg/day compared with another calcium channel blocker, amlodipine, at 5–10 mg/day in patients with mild-to-moderate hypertension.Citation26 Both drugs reduced systolic and diastolic BP in a dose-dependent manner, and although amlodipine reduced systolic BP to a greater extent, the reduction in diastolic BP was similar for both agents. These findings suggest that carvedilol can be considered as an alternative option for the treatment of mild-to-moderate hypertension. Although carvedilol has a clearcut advantage over traditional β-blockers in terms of BP reduction, these hemodynamic effects also rival those of nebivolol, another third-generation vasodilatory β-blocker. The antihypertensive effect was examined between carvedilol 25 mg/day and nebivolol 5 mg/day in patients with mild-to-moderate hypertension.Citation30 Patients experienced a significant reduction in both systolic and diastolic BP on carvedilol or nebivolol compared with placebo (P < 0.05, ). No significant difference was observed in the extent of BP reduction between carvedilol and nebivolol (). Collectively, these clinical studies show that once-daily administration of carvedilol 25 mg as monotherapy provides a reduction in BP that is equivalent to, if not better than, other antihypertensive agents.
BP-lowering in combination therapy
Although it can now be seen that carvedilol is an effective antihypertensive agent when administered as monotherapy, it is most frequently administered in combination with another antihypertensive agent, such as a diuretic. In fact, both the European and JNC-7 guidelines recommend combination therapy, especially when monotherapy fails to reach BP goals or in patients at high cardiovascular risk.Citation1–Citation3
Over 20 years ago, a small double-blind comparative trial conducted in 126 patients with mild-to-moderate hypertension showed that long-term administration of carvedilol 25 mg/day decreased BP to a greater extent than atenolol 50 mg/day. However, a combination of either of these drugs with hydrochlorothiazide produced an additive and equivalent response.Citation31 This additive effect was also observed to a similar extent by the same authors in different patients (n = 122), this time pretreated with hydrochlorothiazide 25 mg for 4 weeks and then given atenolol 50 mg/day or carvedilol 25 mg/day.Citation49 Both carvedilol and atenolol were safe when given alone or in combination with hydrochlorothiazide.
This additive effect was also observed in other studies. A single-blind single-center study examined the short-term efficacy and safety of adding carvedilol 25 mg/day to hydrochlorothiazide 25 mg/day in patients inadequately treated with hydrochlorothiazide alone.Citation52 After 7 days of combined treatment, 53% of patients achieved diastolic BP levels < 90 mmHg and 93% of patients achieved BP levels < 95 mmHg. Furthermore, another clinical trial has investigated the antihypertensive effect of the carvedilol– hydrochlorothiazide combination in 26 severely hypertensive patients.Citation53 Initially patients were inadequately treated with hydrochlorothiazide (diastolic BP > 120 mmHg); however, after 8 weeks of daily administration of carvedilol (10 mg or 20 mg) on an outpatient basis, both systolic and diastolic BP were significantly decreased (P < 0.001 for both). No patient experienced bradycardia, and carvedilol was generally well tolerated.
Overall, these studies demonstrate that carvedilol 10–25 mg once daily in combination with hydrochlorothiazide is an effective and safe therapeutic option for patients with mild-to-moderate or severe hypertension. In addition to hydrochlorothiazide, the BP-lowering effect of carvedilol has also been examined in combination with the third-generation vasodilatory β-blocker, nebivolol.Citation54 This retrospective study examined the effect of atenolol 50–100 mg/day, a carvedilol-nebivolol combination (25 + 25 mg/day and 5 mg/day, respectively) and patients chronically treated with angiotensin II receptor blockers.Citation54 The findings of this study revealed that patients treated with angiotensin II receptor blockers or the carvedilol-nebivolol combination were associated with lower central systolic BP than atenolol treatment, suggesting that, like angiotensin II receptor blockers, vasodilating β-blockers can exert more favorable central hemodynamic effects than atenolol.
Effects on lipid metabolism
Previous studies have shown that traditional β-blockers can have detrimental effects on serum lipids, including increasing triglycerides and decreasing high-density lipoprotein levels.Citation9,Citation55–Citation58 Carvedilol, on the other hand, has been shown to have a neutral or beneficial effect on lipoprotein lipase activity and levels of triglycerides and high-density lipoprotein cholesterolCitation9,Citation59 ().
Figure 3 Comparison of the effects of carvedilol and atenolol on lipid parameters in patients with hypertension. P values represent significant differences in HDL cholesterol (B) and triglycerides (C) between carvedilol and atenolol treatment; the difference for total cholesterol was not significant (A). Open bars represent baseline and filled bars represent the 6-month time point.
Abbreviation: HDL, high-density lipoprotein.
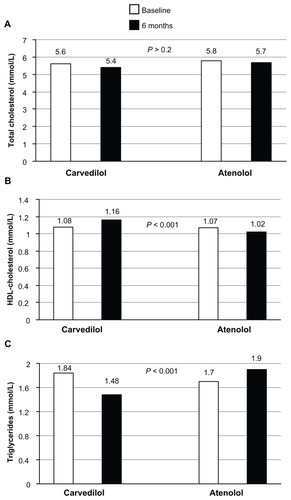
These favorable effects on lipid metabolism were confirmed later in the GEMINI (Glycemic Effects in Diabetes Mellitus: Carvedilol-Metoprolol Comparison in Hypertensives) trial, a large (n = 1235) randomized, double-blind comparison of the effect of carvedilol versus metoprolol in hypertensive diabetic patients. This study showed that patients treated with carvedilol had decreased low-density lipoprotein cholesterol, but not with metoprolol, and triglyceride levels were not increased, as with metoprolol.Citation36,Citation60
Another comparative randomized trial examined the effect of once-daily extended-release carvedilol or extended-release metoprolol in hypertensive patients without diabetes and not requiring lipid-lowering therapy.Citation61 Although there was no difference in the effect of the two drugs on high-density lipoprotein or BP, triglyceride levels were increased by metoprolol but not by carvedilol. This differential metabolic profile could be important in determining treatment options in this patient group.
A recent review article examined 12 published studies and case reports that evaluated the impact of carvedilol on lipid profile.Citation62 Although it was clear that β1-selective antagonists worsen the lipid profile compared with carvedilol, it remained unclear as to whether carvedilol independently improves or has a neutral effect on lipid profile. Regardless, carvedilol should still be considered a favorable choice for the treatment of patients with heart failure and/or hypertension with dyslipidemia.
Effects in diabetes
It is well recognized that conventional β-blockers exert negative effects on glucose control and insulin sensitivity, while also increasing the risk of new-onset diabetes in hypertensive patients.Citation9,Citation18,Citation63 However, earlier studies with β-blockers having vasodilatory properties have shown beneficial effects on glycemic control and insulin sensitivity.Citation64,Citation65 More recently, the effects of carvedilol and atenolol were examined in hypertensive patients with type 2 diabetes. This study demonstrated that after 24 weeks of treatment, fasting plasma glucose and glycosylated hemoglobin (HbA1c) were decreased and insulin sensitivity was increased with carvedilol, whereas atenolol had the opposite resultsCitation59 ().
Figure 4 Comparison of the effects of carvedilol and atenolol on metabolic parameters in patients with hypertension. P values represent significant differences in metabolic parameters (A–C) between carvedilol and atenolol treatment. Open bars represent baseline and filled bars represent the 6-month time point.
Abbreviation: HbA1c, glycosylated hemoglobin.
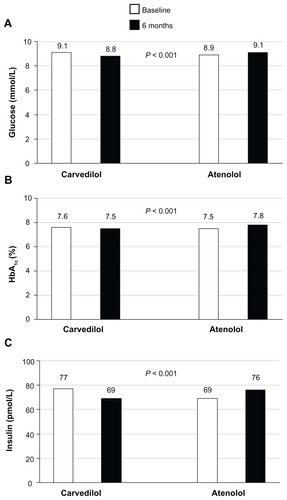
Furthermore, in COMET (Carvedilol or Metoprolol European Trial), the risk for new-onset diabetes was 22% lower in patients receiving carvedilol than those receiving metoprolol.Citation66 The effects of carvedilol were next examined in a large comparative trial in patients with type 2 diabetes. In the GEMINI trial, the effect of carvedilol treatment was compared with metoprolol in 1235 patients with hypertension and type 2 diabetes.Citation36,Citation67 At the end of the study, carvedilol lowered systolic and diastolic BP to the same extent as metoprolol.Citation36 However, the discontinuation rate because of poor glycemic control was 2.2% with metoprolol but only 0.6% with carvedilol (P < 0.04). Furthermore, carvedilol had no adverse effect on HbA1c values. Citation67 While nonvasodilating β-blockers are often associated with undesirable effects on insulin sensitivity and masking of symptoms of hypoglycemia in this patient population, findings from the GEMINI study suggest that carvedilol does not share these negative effects. It is also worth noting that the progression to microalbuminuria was less frequent with carvedilol than with metoprolol (6.4% versus 10.3%; odds ratio 0.60; 95% confidence interval: 0.36–0.97; P = 0.04). This difference may be due to an improvement in insulin resistance or to an effect on oxidant stress by carvedilol.Citation59
Many of these earlier comparative studies were included (from the period of 1980–2008) in a recent schematic review that examined the effect of both nonvasodilating and vasodilating β-blockers (including carvedilol) on glucose, metabolic, and lipid parameters.Citation27 The main findings from this analysis demonstrated that vasodilatory β-blockers were associated with more favorable effects on glucose and lipid profiles than nonvasodilating β-blockers.
More recently, a clinical trial has examined the effect of metoprolol versus carvedilol on endothelial function and insulin-stimulated endothelial function in patients with type 2 diabetes.Citation44 Insulin-stimulated endothelial function deteriorated after treatment with metoprolol, whereas there was no change with carvedilol. This study demonstrated that vascular insulin sensitivity was preserved in diabetic patients treated with carvedilol but blunted during treatment with metoprolol.Citation44
Effects in metabolic syndrome
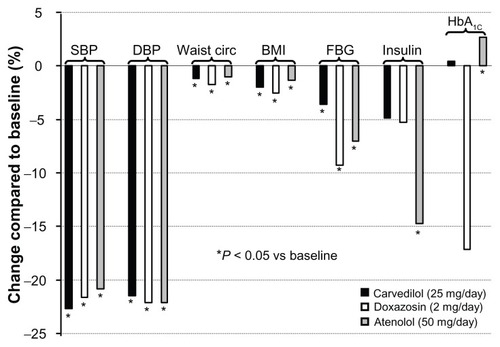
In addition to diabetic patients, carvedilol is also recognized to have beneficial effects in patients with metabolic syndrome.Citation68 A recent randomized comparative study examined the effect of carvedilol versus atenolol or doxazosin for 3 months in 77 patients with metabolic syndrome. Citation69 At the end of the study period, a similar reduction in both systolic and diastolic BP was observed for all three treatment groups. Furthermore, no significant differences were observed between the three groups for a range of biochemical parameters, including plasma glucose, uric acid, urea, cholesterol (total and low-density lipoprotein), triglycerides, apoproteins, insulin, HbA1c, and homeostasis model assessment-insulin resistance (HOMA-IR). However, only carvedilol did not alter low-density lipoprotein levels (percent change for doxazosin −5.6 ± 13.5 and atenolol −8 ± 9.8 versus carvedilol −0.1 ± 12.2, respectively; P < 0.05).Citation69 Furthermore, these favorable effects of carvedilol were observed on other parameters (in addition to reduction in BP) that identify the metabolic syndrome, such as reduction in waist circumference, body mass index, and fasting blood glucose (). It is worth noting that the effects of atenolol on insulin sensitivity may be attributed, in part, to the lower insulin levels and higher HbA1c levels in this group than in the other treatment groups.Citation69 Furthermore, differences in the glucose-lowering and insulin-lowering effects of atenolol between the studies by Giugliano et al () and Uzunlulu et al () may be due to the aforementioned differences in baseline insulin and HbA1c levels, as well as the additional counseling on diet and exercise received by these patients.Citation59,Citation69
Figure 5 Effects of different antihypertensive drugs on metabolic parameters in patients with metabolic syndrome.
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; waist circ, waist circumference; BMI, body mass index; FBG, fasting blood glucose; HbA1c, glycosylated hemoglobin.
Although renin-angiotensin system inhibitors are recommended for the management of hypertensive patients with metabolic syndrome, head-to-head trials examining these agents against carvedilol are lacking. Overall, the evidence underscores the benefits of carvedilol and suggests that this drug should be considered as a promising therapeutic option in hypertensive patients with metabolic syndrome.
Effect on left-ventricular hypertrophy
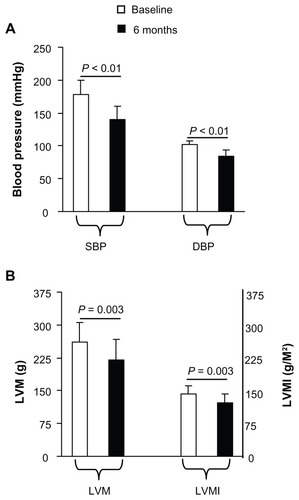
Development of left-ventricular hypertrophy (LVH) in hypertensive patients is associated with an increased risk of cardiovascular mortality and morbidity.Citation70 Although there is evidence that the older traditional β-blockers are not as effective at reducing LVH as other drug classes,Citation71,Citation72 these early studies did not examine vasodilatory β-blockers like carvedilol or nebivolol. Therefore, it is plausible that the α-blocking effect of carvedilol may provide superior benefit in terms of LVH regression, compared with traditional β-blockers. In fact, there are several preclinical and clinical studies available to suggest that carvedilol may be effective in the regression of LVH.Citation73–Citation75 In particular, the study by Verza et al examined the effect of 6 months of daily therapy with carvedilol 25 mg on LVH in elderly patients (mean age 69 years) with essential hypertension and LVH.Citation74 Carvedilol caused a significant reduction in systolic and diastolic BP () and LVH, as measured by left ventricular mass in addition to left ventricular mass index ().
Figure 6 Effect of carvedilol on left ventricular hypertrophy in hypertensive patients.
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; LVM, left ventricular mass; LVMI, left ventricular mass index.
In addition, a clinical trial evaluated the independent and combined effects of captopril and carvedilol on left ventricular remodeling in chronic heart failure in 57 patients.Citation76 Although angiotensin-converting enzyme inhibitor therapy did not alter left ventricular volume, treatment with carvedilol was associated with a reduction in chamber volume. Both drugs reduced left ventricular mass and sphericity. These beneficial effects on remodeling may help explain the relative prognostic benefits of these therapies.
Effect on coronary flow reserve
It is recognized that patients with LVH have lower coronary flow reserve, and there is evidence demonstrating that carvedilol can increase coronary flow reserve in these patients.Citation33,Citation77 A study performed in 63 hypertensive patients with LVH showed that carvedilol, but not metoprolol, increased coronary flow reserve in addition to decreasing left-ventricular mass indexCitation33 ().
Figure 7 Effect of carvedilol, metoprolol, and nebivolol on coronary flow reserve. (A) Carvedilol was administered at 10 mg twice daily (n = 28) and metoprolol was administered at 50 mg twice daily (n = 29). P values denote statistically significant differences between duration and type of treatment. Adapted from Xiaozhen et al.Citation33 (B) Carvedilol was administered at 20–50 mg daily and (C) nebivolol was administered at 5 mg daily. Copyright (c) 2008, ADIS Press. Adapted with permission from Galderisi M, D’Errico A. Beta-blockers and coronary flow reserve: the importance of a vasodilatory action. Drugs. 2008;68(5):579–590.Citation34
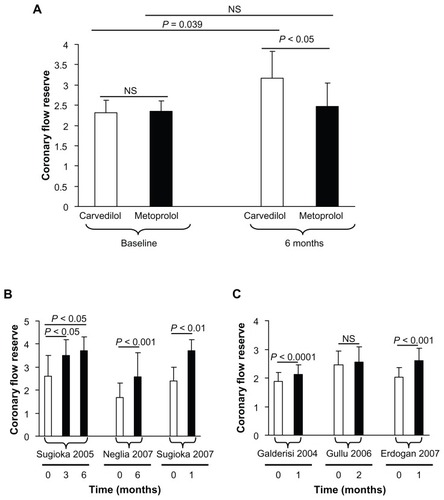
Further, three clinical studies clearly confirm the beneficial effect of carvedilol therapy for 1–6 months on coronary flow reserve (),Citation78–Citation80 the magnitude of this benefit (absolute increase in coronary flow reserve) being greater than in three studies that examined the effect of nebivolol on coronary flow reserve ().Citation81–Citation83 This improvement in coronary blood flow strongly suggests the use of vasodilating β-blockers, such as carvedilol, in patients at risk of atherosclerosis or coronary artery disease.Citation34
Following myocardial infarction
Previous trials have shown benefit in patients receiving β-blocker therapy following myocardial infarction.Citation35,Citation84–Citation87 The American Heart Association guidelines recommend that patients without a clear contraindication to β-blocker therapy should receive β-blockers within a few days of myocardial infarction and continue them indefinitely.Citation88,Citation89 Likewise, both the JNC-7 and European Society of Hypertension/European Society of Cardiology guidelines recommend β-blockers (as well as other antihypertensive agents) in hypertensive patients after myocardial infarction.Citation1–Citation3 The CAPRICORN (Carvedilol Post-Infarct Survival Control in Left Ventricular Dysfunction) trial was specifically designed to examine the benefits afforded by carvedilol in patients with left ventricular systolic dysfunction following acute myocardial infarction.Citation35 Although the primary endpoint of this trial failed to reach statistical significance (all-cause mortality or cardiovascular hospitalization), all-cause mortality alone was significantly lower in the carvedilol group than in the placebo group (116 [12%] versus 151 [15%]; 95% confidence interval: 0·77 [0·60–0·98], P = 0.03) and confirmed data from other studies. Based on findings from this trial, the guidelines now indicate carvedilol in this patient group. A recent Norwegian trial compared the antioxidative effects of carvedilol and atenolol in 232 patients with acute myocardial infarction.Citation90 The findings of this study showed that carvedilol had a more pronounced antioxidative effect than atenolol in post-acute myocardial infarction patients. Together, these studies show that carvedilol is effective and superior to other β-blockers in the treatment of patients following acute myocardial infarction.
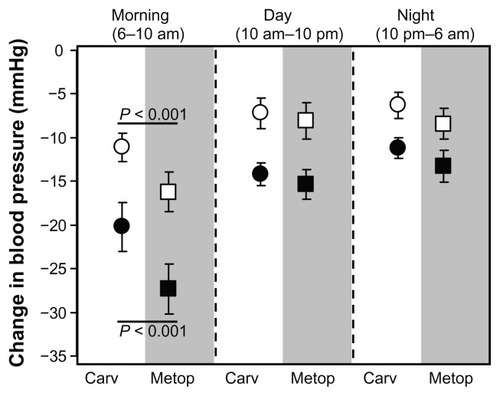
Regression of atherosclerosis
Carvedilol is known to have many effects which are directly linked to prevention of atherosclerosis. Carotid internalmedial thickness (CIMT) has been shown to be directly associated with changes in morning BP. Therefore, carotid atherosclerosis may be prevented by control of morning BP. In a randomized controlled trial performed in 128 hypertensive patients, treatment with carvedilol for 12 months was shown to decrease morning BP significantly ().Citation91 Furthermore, in this study, it was observed that CIMT regression occurred in 49% of patients treated with carvedilol compared with only 18% of patients treated with metoprolol (P < 0.01).Citation91
Figure 8 Control of morning blood pressure in newly diagnosed hypertensive patients. The effects of carvedilol 12.5–20 mg and metoprolol 10–20 mg on both systolic (filled dots) and diastolic blood pressure (open dots) were compared over a 24-hour period. Reprinted by permission from Macmillan Publishers Ltd: American Journal of Hypertension. Marfella R, Siniscalchi M, Nappo F, et al. Regression of carotid atherosclerosis by control of morning blood pressure peak in newly diagnosed hypertensive patients. Am J Hypertens. 2005;18(3):308–318. Copyright 2005.Citation91
Abbreviations: Carv, carvedilol; Metop, metoprolol.
Matrix metalloproteinase (MMP) is also critical for atherosclerosis formation after vascular injury, and carvedilol, a pharmacological antioxidant, is able to inhibit the expression of MMP-2 and MMP-9 both in vivo and in vitro. This points towards a potential clinical indication for carvedilol in the prevention of atherosclerosis.Citation92 Antioxidant and antiinflammatory actions and an ability to decrease the rate of apoptosis of smooth muscle cells are additional features of carvedilol which, collectively, are able to stabilize atherosclerotic plaques.Citation45,Citation93 An early sign of atherogenesis is endothelial adhesiveness to human mononuclear cells, induced by tumor necrosis factor-alpha, which has been shown to be reduced by carvedilol by inhibiting production of intracellular reactive oxygen species, activation of transcription factors, and increasing expression of vascular cell adhesion protein-1 and E-selectin, suggesting its potential role in clinical atherosclerosis.Citation94 Although accumulating evidence suggests a clinically relevant antiatherogenic role for carvedilol, clinical trials with well defined endpoints are needed to confirm these preliminary findings.
Kidney disease
Current opinion favors the use of β-blockers in patients with chronic kidney disease.Citation95 In fact, a recent meta-analysis of eight studies (n = 5972) showed that β-blocker therapy improved all-cause mortality in patients with chronic kidney disease and chronic systolic heart failure, reinforcing the use of these agents in this group.Citation96 With regard to carvedilol, there is also evidence indicating that this agent exerts renoprotective effects. Earlier studies showed beneficial effects on renal hemodynamics, including decreased renal vascular resistance, in patients with heart failure, despite decreasing systemic BP.Citation97 Carvedilol has also been shown to decrease both systolic and diastolic BP without decreasing renal blood flow or glomerular filtration rate, while reducing renal vascular resistance.Citation98 Few studies have examined the effects of carvedilol on renal function or clinical outcomes in patients with heart failure and renal dysfunction. However, in one comparative study, metoprolol was observed to decrease estimated glomerular filtration rate significantly, but this did not change in those who received carvedilol.Citation99 A metaanalysis performed on the CAPRICORN and COPERNICUS (Carvedilol Prospective Randomized Cumulative Survival) trials including 4217 patientsCitation35,Citation100 suggests that the benefits of carvedilol therapy in patients with left ventricular systolic dysfunction with or without symptoms of heart failure are consistent even in the presence of mild to moderate chronic kidney disease.Citation101 Actually, in individuals without chronic kidney disease, the use of carvedilol in the long-term has been shown to improve symptoms of heart failure, increase left ventricular ejection fraction, mitigate neurohormonal activation and peripheral vasoconstriction, and decrease sympathetic overactivity, as well as decrease salt and water retention.Citation102,Citation103 In contrast with traditional β-blockers, several trials have demonstrated a beneficial effect of carvedilol on kidney function in terms of increased renal blood flow and a reduction in microalbuminuria.Citation37,Citation38,Citation104,Citation105 In addition, among patients with normal urine albumin excretion at baseline in the GEMINI trial, fewer treated with carvedilol progressed to microalbuminuria than those treated with metoprolol (6.4% versus 10.3%, respectively).Citation36 It is tempting to speculate that carvedilol may vasodilate efferent arterioles, but definitive evidence is not yet available to confirm this. Overall, these findings support a beneficial role for carvedilol on renal function. To assess these renoprotective effects fully, randomized controlled trials with well defined endpoints are needed in patients with nephropathy.
Additional pleiotropic effects
In addition to the recognized BP-lowering and favorable metabolic effects of carvedilol in a broad range of hypertensive patients, recent preclinical and clinical studies indicate that carvedilol exerts other pleiotropic effects. Although it is recognized that carvedilol is effective in the treatment of patients following acute myocardial infarction,Citation35 few studies have compared the additive effects of carvedilol and reninangiotensin system inhibitors. A clinical study retrospectively investigated 251 patients with acute myocardial infarction treated with angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and divided them into two groups, ie, those treated without β-blockers (n = 80) and those treated with β-blockers (β-blocker group, n = 171; carvedilol or bisoprolol, n = 80).Citation106 After one year of follow-up, it was found that both survival and cardiac event-free rates in the β-blocker group were significantly higher than in the group not treated with β-blockers. Although the percent change in BP did not significantly differ between the two groups, levels of brain natriuretic peptide, MMP-2, and MMP-9, and left ventricular ejection fraction improved significantly in the β-blocker group. Furthermore, treatment with carvedilol achieved more favorable outcomes than bisoprolol. This study demonstrates that β-blocker therapy combined with a renin-angiotensin system inhibitor is more effective than treatment with a renin-angiotensin system inhibitor alone in patients with acute myocardial infarction.
Carvedilol has also been shown to inhibit neointimal hyperplasia in patients with coronary artery disease. The effects of carvedilol-loaded stents compared with bare metal stents on clinical outcomes at 2 years was examined in patients with coronary artery disease.Citation107 Patients receiving carvedilol-coated stents had an increased luminal area and reduced neointimal thickening compared with patients receiving bare metal stents. These findings demonstrate that carvedilol-loaded stents can inhibit neointimal hyperplasia without increased risk of cardiac death, myocardial infarction, or stent thrombosis at 2-year follow-up.
Tolerability
β-blockers are traditionally associated with side effects including depression, fatigue, sexual dysfunction, and cold extremities.Citation108 However, evidence is available from several studies indicating that carvedilol has a good tolerability profile. For example, carvedilol therapy was observed to be safe in patients with Duchenne’s or Becker’s muscular dystrophy, in addition to producing a modest improvement in systolic and diastolic function.Citation109 Results from the SATELLITE survey demonstrated that initiation and uptitration of carvedilol in ambulatory care patients with chronic heart failure was feasible and safe.Citation110 In this survey, the efficacy and tolerability of carvedilol were at least as good as in the clinical trials, while amelioration of patient well being was significant despite suboptimal dosing. In pediatric patients, carvedilol also appears to be well tolerated. Pediatric patients with chronic heart failure who were not responding to standard therapy benefited from treatment with oral carvedilol, although, because of increased elimination of carvedilol, an age-appropriate optimized carvedilol dosing strategy was used.Citation111,Citation112 The safety and efficacy of carvedilol has also been examined in very elderly diabetic patients with heart failure. However, beta-blockers are usually prescribed with caution in these patients because of their perceived unfavorable effects on glucose metabolism, regardless of evidence of their effectiveness and safety in middle-aged diabetic patients. In a recent study of elderly diabetic patients, no worsening of fasting glucose, HbA1c or creatinine levels, or increased incidence of deaths and hospitalizations was observed in elderly diabetics treated with carvedilol.Citation113
Furthermore, carvedilol appears to be well tolerated in elderly patients with chronic heart failure, although the very elderly (>80 years) tolerate carvedilol less well than their younger counterparts (70–79 years). Regardless, carvedilol was tolerated in more than 76% of elderly patients with chronic heart failure at a dose higher than the starting dose. Therefore, the elderly with chronic heart failure should not be denied treatment with carvedilol due to concerns regarding tolerability.Citation114 Other studies which have investigated the tolerability of carvedilol in the elderly all conclude that this drug can be administered safely in this age group.Citation115–Citation119 Overall, these studies indicate that carvedilol has an excellent tolerability profile across a wide range of patient types, thus improving the potential for compliance.
Conclusion
This report provides compelling evidence for the use of carvedilol as an antihypertensive agent in a wide range of hypertensive population types. Current JNC-7 guidelines recommend use of β-blockers such as carvedilol for initial treatment of patients with stage 1 hypertension and compelling indications, eg, previous myocardial infarction, ischemic heart disease, heart failure, diabetes, or high risk of coronary artery disease.Citation1 β-blockers are also recommended for initial treatment of patients with stage 1 hypertension without compelling indications and in patients with stage 2 hypertension who require a combination of drugs to achieve BP control.Citation1,Citation120
Carvedilol, a vasodilating noncardioselective β-blocker, allows the opportunity to use a cardioprotective agent without the concerning hemodynamic and metabolic effects associated with traditional β-blocker therapy. In contrast with classical β-blockers, carvedilol maintains cardiac output, has a reduced effect on heart rate, and decreases BP mainly by decreasing vascular resistance. Studies comparing carvedilol with conventional β-blockers have shown that carvedilol has greater benefit in terms of BP-lowering effects whether administered as monotherapy or combined with a diuretic or renin-angiotensin system inhibitor, in addition to improving glycemic control, insulin sensitivity, and lipid metabolism, suggesting that it could be used in subjects with metabolic syndrome or diabetes. Furthermore, the evidence shows that carvedilol can improve LVH and coronary flow reserve, in addition to reducing progression of atherosclerosis and neointimal hyperplasia in patients with coronary artery disease. Carvedilol is also currently indicated in the post-myocardial infarction setting. These distinct multifaceted hemodynamic and metabolic features specific to carvedilol could result in potential beneficial effects in other likely concomitant diseases, such as renal disease and peripheral vascular disease. To assess these further effects fully, randomized controlled trials with well defined endpoints in specific patient populations with underlying hypertension are now required.
Disclosure
CGE received fees for manuscript preparation on behalf of Primula Multimedia SRL. GL received fees for critical revision of the manuscript. This study was funded by Roche SpA, Italy.
References
- ChobanianAVBakrisGLBlackHRThe seventh report of the joint national committee on Prevention, Detection, Evaluation, and Treatment of High Blood pressure: the JNC 7 reportJAMA2003289192560257212748199
- ManciaGDe BackerGDominiczakA2007ESH-ESC Practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial HypertensionJ Hypertens20072591751176217762635
- ManciaGLaurentSAgabiti-RoseiEReappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force documentJ Hypertens200927112121215819838131
- Wolf-MaierKCooperRSKramerHHypertension treatment and control in five European countries, Canada, and the United StatesHypertension2004431101714638619
- SarafidisPABakrisGLState of hypertension management in the United States: confluence of risk factors and the prevalence of resistant hypertensionJ Clin Hypertens (Greenwich)200810213013918256578
- VolpeMTocciGTrimarcoBBlood pressure control in Italy: results of recent surveys on hypertensionJ Hypertens20072571491149817563573
- SarafidisPABakrisGLAntihypertensive treatment with betablockers and the spectrum of glycaemic controlQJM200699743143616766516
- FrishmanWHA historical perspective on the development of betaa-drenergic blockersJ Clin Hypertens200794 Suppl 31927
- MesserliFHGrossmanEBeta-blockers in hypertension: is carvedilol different?Am J Cardiol200493Suppl7B12B
- BlackHRSicaDAA modern perspective on beta-blocker use in hypertension: clinical trials and their influence on clinical practiceJ Clin Hypertens (Greenwich)200794 Suppl 31018
- CheQSchreiberMJJrRafeyMABeta-blockers for hypertension: are they going out of style?Cleve Clin J Med200976953354219726558
- De CaterinaARLeoneAMThe role of beta-blockers as first-line therapy in hypertensionCurr Atheroscler Rep201113214715321207202
- MesserliFHGrossmanEGoldbourtUAre beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic reviewJAMA199827923190319079634263
- DahlöfBDevereuxRBKjeldsenSEfor the LIFE Study GroupCardiovascular morbidity and mortality in the Losartan Intervention For Endpoint Reduction in Hypertension study (LIFE): a randomised trial against atenololLancet20023599311995100311937178
- CarlbergBSamuelssonOLindholmLHAtenolol in hypertension: is it a wise choice?Lancet200436494461684168915530629
- LindholmLHCarlbergBSamuelssonOShould beta blockers remain first choice in the treatment of primary hypertension? A meta-analysisLancet200536694961545155316257341
- DahlöfBSeversPSPoulterNRPrevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering arm (ASCOT-BPLA): a multicentre randomized controlled trialLancet2005366948989590616154016
- BangaloreSParkarSGrossmanEMesserliFHA meta-analysis of 94,492 patients with hypertension treated with beta blockers to determine the risk of new-onset diabetes mellitusAm J Cardiol200710081254126217920367
- WiysongeCSBradleyHMayosiBMBeta-blockers for hypertensionCochrane Database Syst Rev2007241CD00200317253471
- WilliamsBPoulterNRBrownMJGuidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IVJ Hum Hypertens200418313918514973512
- National Institute for Health and Clinical ExcellenceHypertension: Management of Hypertension in Adults in Primary Care: Pharmacological UpdateNICE Clinical Guideline 34London, UKNational Institute for Health and Clinical Excellence2006
- RitchieLDCampbellNCMurchiePNew NICE guidelines for hypertensionBr Med J2011343d564421900351
- NeutelJMSmithDHRamCVApplication of ambulatory blood pressure monitoring in differentiating between antihypertensive agentsAm J Med19939421811878430713
- Ali RazaJMovahedAUse of cardiovascular medications in the elderlyInt J Cardiol2002852–320321512208585
- MoserMClinical experience with carvedilolJ Hum Hypertens19937Suppl 1S16S208098064
- VermaUBanoGMohan LalBSharmaKPSharmRAntihypertensive efficacy of carvedilol and amlodipine in patients of mild to moderate hypertension – a comparative studyJK Science200464193196
- FonsecaVAEffects of beta-blockers on glucose and lipid metabolismCurr Med Res Opin201026361562920067434
- McTavishDCampoli-RichardsDSorkinEMCarvedilol. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacyDrugs19934522322587681374
- DicksteinKCohen-SolalAFilippatosGESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM)Eur J Heart Fail2008101093398918826876
- ErdoğanOErtemBAltunAComparison of antihypertensive efficacy of carvedilol and nebivolol in mild-to-moderate primary hypertension: a randomized trialAnadolu Kardiyol Derg2011114310313 Turkish21543293
- WidmannLvan der DoesRHörrmannMMachwirthMSafety and antihypertensive efficacy of carvedilol and atenolol alone and in combination with hydrochlorothiazideEur J Clin Pharmacol199038Suppl 2S143S1461974505
- TedescoMANataleFCalabròREffects of monotherapy and combination therapy on blood pressure control and target organ damage: a randomized prospective intervention study in a large population of hypertensive patientsJ Clin Hypertens (Greenwich)20068963464116957425
- XiaozhenHYunZMeiZYuSEffect of carvedilol on coronary flow reserve in patients with hypertensive left-ventricular hypertrophyBlood Press2010191404720001392
- GalderisiMD’ErricoABeta-blockers and coronary flow reserve: the importance of a vasodilatory actionDrugs200868557959018370439
- DargieHColucciWSFordIEffect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trialLancet200135792661385139011356434
- BakrisGLFonsecaVKatholiREGEMINI InvestigatorsMetabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trialJAMA2004292182227223615536109
- DupontAGCarvedilol and the kidneyClin Investig199270Suppl 1S127S131
- MarchiFCirielloGEfficacy of carvedilol in mild to moderate essential hypertension and effects on microalbuminuria: a multicenter, randomized, open-label, controlled study versus atenololAdv Ther199512421222110155349
- TodaNVasodilating beta-adrenoceptor blockers as cardiovascular therapeuticsPharmacol Ther2003100321523414652111
- StafylasPCSarafidisPACarvedilol in hypertension treatmentVasc Health Risk Manag200841233018629377
- FrishmanWHHendersonLSLukasMAControlled-release carvedilol in the management of systemic hypertension and myocardial dysfunctionVasc Health Risk Manag2008461387140019337551
- PedersenMECockcroftJRThe vasodilatory beta-blockersCurr Hypertens Rep20079426927717686376
- FrishmanWHCarvedilolN Engl J Med199833924175917659845712
- KveiborgBHermannTSMajor-PedersenAMetoprolol compared with carvedilol deteriorates insulin-stimulated endothelial function in patients with type 2 diabetes – a randomized studyCardiovasc Diabetol201092120500877
- DandonaPGhanimHBrooksDPAntioxidant activity of carvedilol in cardiovascular diseaseJ Hypertens200725473174117351362
- CalòLASempliciniADavisPAAntioxidant and antiinflammatory effect of carvedilol in mononuclear cells of hypertensive patientsAm J Med20051182201202
- Meyer-SabellekWSchulteKLDistlerAGotzenRCircadian antihypertensive profile of carvedilol (BM 14190)J Cardiovasc Pharmacol198710Suppl 11S119S1232454357
- Lund-JohansenPOmvikPNordrehaugJEWhiteWCarvedilol in hypertension: effects on hemodynamics and 24-hour blood pressureJ Cardiovasc Pharmacol199219Suppl 1S27S341378146
- van der DoesRWidmannLUberbacherHJHörrmannMMachwirthMStienenUEfficacy and safety of carvedilol in comparison with atenolol in hypertensive patients pretreated with hydrochlorothiazideEur J Clin Pharmacol199038Suppl 2S147S1521974506
- HallSPrescottRIHallmanRJA comparative study of carvedilol, slow-release nifedipine, and atenolol in the management of essential hypertensionJ Cardiovasc Pharmacol19918SupplS35S381721977
- MoserMFrishmanWResults of therapy with carvedilol, a beta-blocker vasodilator with antioxidant properties, in hypertensive patientsAm J Hypertens1998111 Pt 215S22S9503102
- DupontAGSchoorsDFVenutiRPThe safety of adding carvedilol to hypertensive patients inadequately treated with diureticsEur J Clin Pharmacol199038Suppl 2S153S1571974507
- OgiharaTYoshinagaKKamaharaYClinical efficacy of carvedilol in severe hypertensionJ Cardiovasc Pharmacol199118Suppl 4S69S721721983
- PolóniaJBarbosaLSilvaJABertoquiniSDifferent patterns of peripheral versus central blood pressure in hypertensive patients treated with β-blockers either with or without vasodilator properties or with angiotensin receptor blockersBlood Press Monit201015523523920577082
- AronowWSCurrent role of beta-blockers in the treatment of hypertensionExpert Opin Pharmacother201011162599260720426702
- KasiskeBLMaJZKalilRSEffects of antihypertensive therapy on serum lipidsAnn Intern Med199512221331417992988
- BrookRDMechanism of differential effects of antihypertensive agents on serum lipidsCurr Hypertens Rep20002437037710981172
- Maitland-van der ZeeAHKlungelOHKloostermanJMThe association between antihypertensive drug therapies and plasma lipid levels in the general populationJ Hum Hypertens2001151070170511607800
- GiuglianoDAcamporaRMarfellaRMetabolic and cardiovascular effects of carvedilol and atenolol in non-insulin-dependent diabetes mellitus and hypertension. A randomized, controlled trialAnn Intern Med1997126129559599182472
- MesserliFHBellDSFonsecaVGEMINI InvestigatorsBody weight changes with beta-blocker use: results from GEMINIAm J Med2007120761061517602935
- FonarowGCDeedwaniaPFonsecaVDifferential effects of extended-release carvedilol and extended-release metoprolol on lipid profiles in patients with hypertension: results of the Extended- Release Carvedilol Lipid TrialJ Am Soc Hypertens20093321022020409961
- SharpRPSirajuddinRShariefIMImpact of carvedilol on the serum lipid profileAnn Pharmacother200842456457118364407
- JacobSRettKWicklmayrMDifferential effect of chronic treatment with two beta-blocking agents on insulin sensitivity: the carvedilol-metoprolol studyJ Hypertens19961444894948761899
- HaenniALithellHTreatment with a beta-blocker with beta 2-agonism improves glucose and lipid metabolism in essential hypertensionMetabolism19944344554618159103
- MalminiemiKAssociation between serum lipids, glucose tolerance, and insulin sensitivity during 12 months of celiprolol treatmentCardiovasc Drugs Ther1995922953047662596
- Poole-WilsonPASwedbergKClelandJGCarvedilol or Metoprolol European Trial InvestigatorsComparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol or Metoprolol European Trial (COMET): randomised controlled trialLancet2003362937771312853193
- WrightJTJrBakrisGLBellDSLowering blood pressure with beta-blockers in combination with other renin-angiotensin system blockers in patients with hypertension and type 2 diabetes: results from the GEMINI TrialJ Clin Hypertens (Greenwich)200791184284917978591
- CarellaAMAntonucciGConteMAntihypertensive treatment with beta-blockers in the metabolic syndrome: a reviewCurr Diabetes Rev20106421522120459394
- UzunluluMOguzAYorulmazEThe effect of carvedilol on metabolic parameters in patients with metabolic syndromeInt Heart J200647342143016823248
- HaiderAWLarsonMGBenjaminEJLevyDIncreased left ventricular mass and hypertrophy are associated with increased risk for sudden deathJ Am Coll Cardiol1998325145414599809962
- CruickshankJMLewisJMooreVDoddCReversibility of left ventricular hypertrophy by differing types of antihypertensive therapyJ Hum Hypertens19926285901534582
- DahlofBPennertKHanssonLReversal of left ventricular hypertrophy in hypertensive patients: a meta-analysis of 109 treatment studiesAm J Hypertens199252951101532319
- EichstaedtHDanneOSchroederRJKreuzDLeft ventricular hypertrophy regression during antihypertensive treatmentClin Investig199270Suppl 1S79S86
- VerzaMAmmendolaSCambardellaARegression of left ventricular hypertrophy in hypertensive elderly patients with carvedilolArch Gerontol Geriatr199622Suppl 114314718653022
- TualLMorelOEFavretFCarvedilol inhibits right ventricular hypertrophy induced by chronic hypobaric hypoxiaPflugers Arch2006452437137916639551
- KhattarRSSeniorRSomanPvan der DoesRLahiriARegression of left ventricular remodeling in chronic heart failure: comparative and combined effects of captopril and carvedilolAm Heart J2001142470471311579363
- NemesANeuKForsterTKovacsZCsanadyMCoronary flow velocity reserve is diminished in hypertensive left ventricular hypertrophyKardiol Pol200562115 Polish15815773
- SugiokaKHozumiTTakemotoYEarly recovery of impaired coronary flow reserve by carvedilol therapy in patients with idiopathic dilated cardiomyopathy: a serial transthoracic Doppler echocardiographic studyJ Am Coll Cardiol200545231831915653035
- NegliaDDe MariaRMasiSEffects of long-term treatment with carvedilol on myocardial blood flow in idiopathic dilated cardiomyopathyHeart200793780881317237134
- SugiokaKHozumiTTakemotoYRelation of early improvement in coronary flow reserve to late recovery of left ventricular function after beta-blocker therapy in patients with idiopathic dilated cardiomyopathyAm Heart J200715361080.e1e617540213
- GalderisiMCicalaSD’ErricoAde DivitiisOde SimoneGNebivolol improves coronary flow reserve in hypertensive patients without coronary heart diseaseJ Hypertens200422112201220815480106
- GulluHErdoganDCaliskanMDifferent effects of atenolol and nebivolol on coronary flow reserveHeart200692111690169117041122
- ErdoganDGulluHCaliskanMNebivolol improves coronary flow reserve in patients with idiopathic dilated cardiomyopathyHeart200793331932417065184
- YusufSPetoRLewisJBeta blockade during and after myocardial infarction: an overview of the randomized trialsProg Cardiovasc Dis19852753353712858114
- Beta-Blocker Heart Attack Trial Research Group (BHAT)A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality resultsJAMA198224712170717147038157
- HerlitzJKarlsonBWHjalmarsonATen year mortality in relation to original size of myocardial infarct: results from the Gothenburg metoprolol studyBr Heart J19947132382418142192
- [No authors listed]Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarctionN Engl J Med1981304148018077010157
- SmithSCJrAllenJBlairSNACC/AHA guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood InstituteCirculation2006113192363237216702489
- RosendorffCBlackHRCannonCPTreatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and PreventionCirculation2007115212761278817502569
- JonssonGAbdelnoorMSeljeflotIThe antioxidative effects of long-term treatment are more pronounced for carvedilol than for atenolol in post-myocardial infarction patientsJ Cardiovasc Pharmacol2007491273217261960
- MarfellaRSiniscalchiMNappoFRegression of carotid atherosclerosis by control of morning blood pressure peak in newly diagnosed hypertensive patientsAm J Hypertens200518330831815797646
- WuTCChenYHLeuHBCarvedilol, a pharmacological antioxidant, inhibits neointimal matrix metalloproteinase-2 and -9 in experimental atherosclerosisFree Radic Biol Med200743111508152217964422
- GuanYYYeBHLuHHStudy of carvedilol on plaque stability in carotid atherosclerotic rabbits transfected by p53 geneZhonghua Xin Xue Guan Bing Za Zhi20073516368 Chinese17386169
- ChenJWLinFYChenYHCarvedilol inhibits tumor necrosis factor-alpha-induced endothelial transcription factor activation, adhesion molecule expression, and adhesiveness to human mononuclear cellsArterioscler Thromb Vasc Biol200424112075208115374848
- KalaitzidisRBakrisGShould nephrologists use beta-blockers? A perspectiveNephrol Dial Transplant200924370170219073654
- BadveSVRobertsMAHawleyCMEffects of beta-adrenergic antagonists in patients with chronic kidney disease: a systematic review and meta-analysisJ Am Coll Cardiol201158111152116121884954
- AbrahamWTTsvetkovaTLowesBDCarvedilol improves renal hemodynamics in patients with chronic heart failureJ Card Fail199898Suppl 1378379
- TomitaKMarumoFEffect of long-term carvedilol therapy on renal function in essential hypertensionJ Cardiovasc Pharmacol199219Suppl 1S97S1011378158
- ItoHNagatomoYKohnoTDifferential effects of carvedilol and metoprolol on renal function in patients with heart failureCirc J20107481578158320562496
- PackerMFowlerMBRoeckerEBCarvedilol Prospective Randomized Cumulative Survival (COPERNICUS) Study GroupEffect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) studyCirculation2002106172194219912390947
- WaliRKIyengarMBeckGJEfficacy and safety of carvedilol in treatment of heart failure with chronic kidney disease: a meta-analysis of randomized trialsCirc Heart Fail201141182621036889
- HillegeHLGirbesARde KamPJRenal function, neurohormonal activation, and survival in patients with chronic heart failureCirculation2000102220321010889132
- MadsenBKKellerNChristiansenEChristensenNJPrognostic value of plasma catecholamines, plasma renin activity, and plasma atrial natriuretic peptide at rest and during exercise in congestive heart failure: comparison with clinical evaluation, ejection fraction, and exercise capacityJ Card Fail1995132072169420653
- AgrawalBWolfKBergerALuftFCEffect of antihypertensive treatment on qualitative estimates of microalbuminuriaJ Hum Hypertens19961085515558895040
- FassbinderWQuarderOWaltzATreatment with carvedilol is associated with a significant reduction in microalbuminuria: a multicentre randomised studyInt J Clin Pract199953751952210692737
- KonishiMHaraguchiGYoshikawaSAdditive effects of β-blockers on renin-angiotensin system inhibitors for patients after acute myocardial infarction treated with primary coronary revascularizationCirc J20117581982199121697605
- KimHKHongYJJeongMHTwo-year clinical outcome after carvedilol-loaded stent implantation in patients with coronary artery diseaseKorean J Intern Med2011261414621437161
- ChakrabortySShuklaDMishraBSinghSClinical updates on carvedilol: a first choice beta-blocker in the treatment of cardiovascular diseasesExpert Opin Drug Metab Toxicol20106223725020073998
- RhodesJMargossianRDarrasBTSafety and efficacy of carvedilol therapy for patients with dilated cardiomyopathy secondary to muscular dystrophyPediatr Cardiol200829234335117885779
- LainscakMMoulletCSchönNTenderaMTreatment of chronic heart failure with carvedilol in daily practice: the SATELLITE survey experienceInt J Cardiol2007122214915517804098
- LäerSMirTSBehnFCarvedilol therapy in pediatric patients with congestive heart failure: a study investigating clinical and pharmacokinetic parametersAm Heart J2002143591692212040358
- AlbersSMeibohmBMirTSLäerSPopulation pharmacokinetics and dose simulation of carvedilol in paediatric patients with congestive heart failureBr J Clin Pharmacol200865451152217995971
- Del SindacoDPulignanoGCioffiGSafety and efficacy of carvedilol in very elderly diabetic patients with heart failureJ Cardiovasc Med (Hagerstown)20078967568217700396
- KrumHHillJFruhwaldFTolerability of beta-blockers in elderly patients with chronic heart failure: the COLA II studyEur J Heart Fail20068330230716198627
- NulDZambranoCDiazAGrupo de Estudio de la Sobrevida en la Insuficiencia Cardiaca en ArgentinaImpact of a standardized titration protocol with carvedilol in heart failure: safety, tolerability, and efficacy – a report from the GESICA registryCardiovasc Drugs Ther200519212513416025231
- LawlessCETamlynTShahRTitration of carvedilol in elderly heart failure patientsAm J Geriatr Cardiol200514523023516247281
- Leonetti LupariniRCelliVPiccirilloGCarvedilol in elderly patients with chronic heart failure, a 12 weeks randomized, placebo controlled open trialArch Gerontol Geriatr199929327528215374060
- RickliHSteinerSMüllerKHessOMBetablockers in heart failure: Carvedilol Safety Assessment (CASA 2-trial)Eur J Heart Fail20046676176815542414
- OpasichCBoccanelliACafieroMBRING-UP 2 InvestigatorsProgramme to improve the use of beta-blockers for heart failure in the elderly and in those with severe symptoms: results of the BRING-UP 2 StudyEur J Heart Fail20068664965716466962
- ManriqueCGilesTDFerdinandKCSowersJRRealities of newer beta-blockers for the management of hypertensionJ Clin Hypertens (Greenwich)200911736937519583633