Abstract
Introduction
Cerebral venous thrombosis (CVT) remains one of the most frequent cause of stroke in young adults although it is a rare disorder. It has a serious emergency manifestation during pregnancy and postpartum. It is frequently under diagnosed and limited publications in developing countries especially sub-Saharan Africa.
Case Presentation
Here, we report the case of a 35-year-old female, para 8 and gravida 8, brought to emergency department on her ninth day postpartum, having severe headaches and confusion; during her admission to emergency, she suffered two episodes of generalized seizure. On admission, the patient's blood pressure was 200/120 mmHg. The patient was firstly diagnosed with postpartum eclampsia and managed with magnesium sulfate for seizures and hydralazine for blood pressure control. On ward admission, she continued having seizures and her level of consciousness decreased with left side weakness. An urgent MRI of head and MR venography performed immediately revealed acute thrombosis involving the anterior aspect of superior sagittal sinus and the left transverse sinus. The patient was moved to the ICU. Anti-coagulant LMW enoxaparin and anticonvulsant were started. After improving on clinical and biochemical tests, the patient was transferred to the inpatient ward on fifth day. Another two days later in the ward, she improved significantly, and then a head CT (contrast) angiography/venography was performed before she was discharge and showed no evidence of filling defect in cortical/dural venous sinuses.
Conclusion
Cerebral venous sinus thrombosis (CVST) and postpartum eclampsia may have similar manifestations in young women of reproductive age. Early prompt diagnosing and therapeutic intervention of CVST can prevent further neurological deterioration and immediately improve the patient.
Introduction
Cerebral venous thrombosis (CVT) is a rare illness in pregnancy and the postpartum period, accounting for 0.5% to 1% of all cases of stroke worldwide.Citation1 Cerebral venous sinus thrombosis (CVST) patients frequently present with headaches, seizures, and may be associated with focal neurological deficit manifestation. The manifestations are developed from either occlusion of transverse sinus, superior sagittal, straight sinus, cortical veins, and jugular veins or internal cerebral veins of cerebral venous sinuses and compromised drainage of cerebrospinal fluid lead to intracranial hypertension.Citation2
Although the diagnosis of the CVST is not easy due to very clinical similarities or coexist on posterior reversible encephalopathy and postpartum eclampsia.Citation3
CVST is potentially fatal and early diagnoses and management is crucial. We report a case of a CVT patient who was misdiagnosed with postpartum eclampsia.
Case Presentation
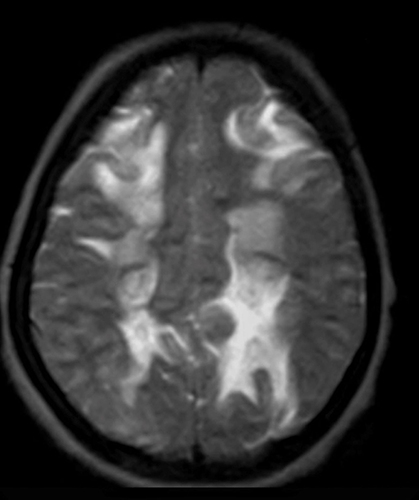
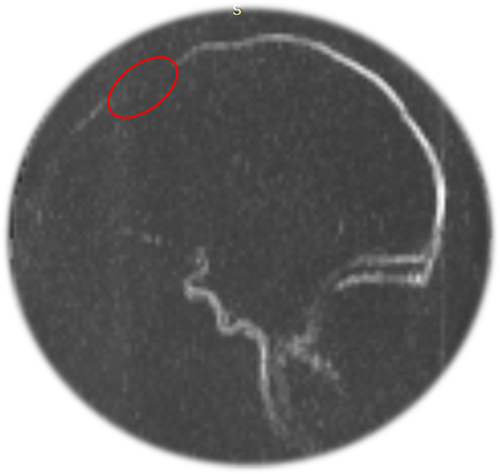
A 35-year-old female, para 8, gravida 8 presented to the emergency department on the ninth day postpartum having experienced of severe headaches and confusion, in the ER she had two episodes of generalized seizures, the generalized seizure action was firstly observed in the ER. On Her severe headaches started in the last trimester but worsened postpartum. She has history of spontaneous, similar postpartum headaches after her last pregnancy, although she had not attended antenatal care for any previous pregnancies. On ER admission the patient's blood pressure was 200/120 mmHg, and biochemistry tests and urine analysis were taken on presentation at the ER. Treatment of presumed postpartum eclamptic seizure was started at 6g/8mL bolus of intravenous magnesium sulfate diluted 12mL of normal saline slowly over 20 minutes and hydralazine 20mg/2mL intravenously over 4 minutes for blood pressure control. After that, the patient was transferred to the ward where she continued having seizures while presumed eclamptic treatment was administered. She also developed left sided weakness with altered mental status. An urgent MRI with Magnetic Resonance venography (MRV) were performed. The MRV with MRI showed acute thrombosis involving the anterior aspect of the superior sagittal sinus and left transverse sinus with subcortical and deep white matter T2/FLAIR hyperintensities involving the parasagittal regions of both sides of the frontal, parietal and occipital lobes and left temporal lobe also reported no evidence of intracerebral hemorrhage or recent arterial ischemia (). After that, the patient was admitted to the intensive care unit (ICU), where endotracheal intubation was done to secure the airway and sedated to stabilize and control the seizures. To do this, a therapeutic dose of enoxaparin 4000I.U/0.4mL (40mg) was administered subcutaneously twice a day while an anti-coagulant was initiated according to the patient’s body weight of 80kg (1mg/kg/bid) and levetiracetam tablet of 500mg two times a day for seizure treatment through nasogastric tube. Days later, the neurological symptoms slowly improve while the initial laboratory investigation of the coagulation profile indicate that prothrombin time (PT) was 13.4 sec equivalent to INR of 1.1, partial thromboplastin time was 45 sec and D-dimer was 550ng/mL in the normal range. After four days in the ICU, the patient was transferred to an inpatient ward. After two days of post-ward admission, the patient clinically (GCS 15/15) and mentally improved, on this day we repeated CT head angiography/venography with contrast and reported no evidence of filling defects in the dural venous sinuses (). On day 16 postpartum, she was discharged fwith warfarin 5mg/day for 3 months with INR follow up.
Figure 1 MRV of brain showing superior sagittal sinus thrombosis at anterior aspect. The red circled area is indicating the location of the thrombus.
Discussion
CVT is uncommon illness that has a critical outcome. The rate from 0.018% to 0.2% had been reported for developing venous thrombosis during pregnancy and puerperium.Citation4 The prevalence of CVT has long been likely to be about 0.3–0.5/100,000 per year, nevertheless latest studies have been declared a greater level of around 1–1.5/100,000 per year.Citation5,Citation6 While the rise in incidence has been reflected to simply greater awareness of this condition, developments and availability of imaging practices which result in the detection of rare-severe cases are most likely to be important contributing factors.
CVT has known risk factors and causes, which are pregnancy, postpartum, venous thromboembolism, contraceptives medications, estrogen therapies, thrombophilia and hypercoagulability which is part from local infections and inflammatory conditions although CVST is three times more common in women of reproductive age than in men, probably due to the use of oral contraceptives, postpartum condition and pregnancy.Citation6 The most two probable mechanisms that means females are more vulnerable to CVT during the postpartum period are, impairment of cerebral venous sinuses during the labor process secondary from instabilities of intracranial pressure and the hypercoagulability state during pregnancy that could lead to this rare condition during the postpartum period.
In this case, CVST seemed to be without other risk factors, except postpartum and the patient had a COVID-19 negative status. CVST has challenging on diagnosing initially on clinical. In specific, distinguishing between CVST and postpartum eclampsia can be very difficult due to the similar clinical presentations and lack of experience or lack of awareness about rare-serious disorders, so it is crucial to diagnose it urgently and to manage it correctly.
Symptoms of CVST appeared in the first three weeks postpartum in most cases, with severe headaches being the most common complaint.Citation7 Patients of CVT usually presenting with severe headache, papilledema, nausea, and altered consciousness level (intracranial hypertension) associated with seizures and other focal neurological deficit usually experienced in patient cases where there is thrombosis of superficial cerebral veins, subcortical or cortical lesions.Citation8 Once a pregnant, or postpartum, female experiences recent onset stroke symptoms, such as severe headaches and seizures, it is important to observe for the common CVT known risk factors, If CVT is suspicious, MR venography or CT venography should be performed without any delay and MR venography is the first indicate and sensitive in acute phase of thrombosis.Citation9 MRV is the gold standard diagnostic modalities choose for this case.
Treatment of CVST emphasises anticoagulation and management of symptoms to prevent neurological complications and death, while nearly two thirds of patients have venous hemorrhaging in the acute phase infarcts, anticoagulation with low molecular weight heparin was acclaimed treatment for CVT cases including pregnant females (enoxaparin 100 I.U/kgx2) as guidelines for European Federation of Neurological Societies.Citation10 The percentage of mortality for all causes of CVST is about 2–10%, nevertheless it is considerably lower in the gravid female population.Citation11
Particularly for this case, the MRI with MRV imaging results urged the cessation of magnesium sulfate and the use of antiepileptic and anticoagulation therapies. Finally the patient improved. In this case, we present due to the origin, underdiagnosed, critical outcome and lack of case reports or studies in eastern Africa.
Conclusion
We presented a rare case origin of CVST in postpartum patient initially misdiagnosed as postpartum eclampsia in Somalia. This case report has geographical epidemiology of its origin in Africa due to its frequent underdiagnoses, lack of case reports and limited cases studies in Africa especially the East Africa region.
The case highlights the importance of conserving a broad differential diagnosis in females experiencing severe headaches with seizure on postpartum period. Maternity Healthcare workers should enhance the care for this patient by seeing causes rarer than postpartum eclampsia and conducting tests that could differentiate them. It is important for early diagnosing and managing for prevent complications and death.
Informed Consent
A Written consent form was attained from the patient for publication of this case report and the attaching images. In our institution, ethical approval is not required for case reports.
Disclosure
The authors report no any financial or conflicts of interest in this case report.
Acknowledgments
We would like to express our sincere gratitude and deep appreciation to Dr. Bashiru Garba for his guidance and recommendations in this case report. We also express our deep gratitude to Dr. Omar Hassan Badawi for his support on imaging interpretations.
References
- Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352(17):1791–1798. doi:10.1056/NEJMra2106545
- McCaulley JA, Pates JA. Postpartum cerebral venous thrombosis. Obstet Gynecol. 2011;118(2 Pt 2):423–425. doi:10.1097/AOG.0b013e318212fca2
- KöRoglu N, Sudolmus S, Sarioglu EA, Alkan A, Dansuk R. Cerebral venous sinus thrombosis and posterior reversible encephalopathy syndrome in a preeclamptic woman. J Clin Diagn Res. 2015;9(1):QD09–QD11. doi:10.7860/JCDR/2015/9420.5408
- Oh MK, Ryu JH, Jeon WJ, Lee CW, Cho SY. Case report: postpartum cerebral venous thrombosis misdiagnosed as postdural puncture headache. BMC Anesthesiol. 2020;20(1):80. doi:10.1186/s12871-020-00992-1
- Silvis SM, de Sousa DA, Ferro JM, Coutinho JM. Cerebral venous thrombosis. Nat Rev Neurol. 2017;13(9):555–565. doi:10.1038/nrneurol.2017.104
- Devasagayam S, Wyatt B, Leyden J, Kleinig T. Cerebral venous sinus thrombosis incidence is higher than previously thought: a retrospective population-based study. Stroke. 2016;47(9):2180–2182. doi:10.1161/STROKEAHA.116.013617
- Cantú C, Barinagarrementeria F. Cerebral venous thrombosis associated with pregnancy and puerperium. Review of 67 cases. Stroke. 1993;24(12):1880–1884. doi:10.1161/01.str.24.12.1880
- Kristoffersen ES, Harper CE, Vetvik KG, Faiz KW. Cerebral venous thrombosis - epidemiology, diagnosis and treatment. Cerebral venetrombose – forekomst, diagnostikkogbehandling. Tidsskr Nor Laegeforen. 2018;138(12). doi:10.4045/tidsskr.17.1047
- Saposnik G, Barinagarrementeria F, Brown RD Jr, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158–1192. doi:10.1161/STR.0b013e31820a8364
- Ferro JM, Bousser MG, Canhão P, et al. European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis - endorsed by the European Academy of Neurology. Eur J Neurol. 2017;24(10):1203–1213. doi:10.1111/ene.13381
- Lanska DJ, Kryscio RJ. Risk factors for peripartum and postpartum stroke and intracranial venous thrombosis. Stroke. 2000;31(6):1274–1282. doi:10.1161/01.str.31.6.1274