Abstract
Background
Rheological disorders of red blood cells (RBC) and decreased RBC deformability have been involved in the development of diabetic microangiopathy. However, few studies have evaluated the association of RBC count with microvascular complications in patients with type 2 diabetes mellitus (T2DM). The purpose of this study was to investigate the association of RBC count with microvascular complications in patients with T2DM.
Methods
This study involved 369 patients with T2DM: 243 with one or more microvascular complications and 126 without microvascular complications. Anticoagulated blood was collected and analyzed in an automated blood cell counter. The presence of risk factors for microvascular complications was determined.
Results
The proportion of patients with microvascular complications increased as the RBC count decreased (P < 0.001). After adjustment for known risk factors for microvascular complications by logistic regression analysis, lower quartiles of RBC count were associated with a higher risk of microvascular complications compared with the reference group composed of the highest quartile (first quartile, odds ratio 4.98, 95% confidence interval 1.54–6.19, P = 0.008; second quartile, odds ratio 3.21, 95% confidence interval 1.17–5.28, P = 0.024).
Conclusion
A decreased RBC count is associated with microvascular complications in Chinese patients with T2DM. The RBC count is a potential marker to improve further the ability to identify diabetic patients at high risk of microvascular complications.
Introduction
Diabetes is a complex and chronic metabolic disease characterized by hyperglycemia resulting from defects in the secretion and action of insulin. Type 2 diabetes mellitus (T2DM) is the most common form of diabetes, and is associated with the development of a number of devastating microvascular complications, including diabetic retinopathy (DR), diabetic peripheral neuropathy (DPN), and diabetic nephropathy (DN).Citation1 Diabetes-induced microvascular complications are the major causes of morbidity and mortality in patients with T2DM.Citation2 As these microvascular complications are important causes of morbidity, early diagnosis of the presence of such complications would help in reducing adverse cardiovascular events and associated health-care costs.Citation3 Many conventional risk factors have been shown to be important contributors to the development of microvascular complications.Citation4 Nevertheless, these risk factors cannot fully account for the excess risk produced by diabetes.Citation5 Considerable effort has been expended in identifying patients at greater risk of microvascular complications, in particular because the traditional risk factors do not entirely explain the increased risk in diabetes. Multiple pathophysiological disorders have been involved in the development of diabetic microangiopathy, including rheological disorders of red blood cells (RBCs) and decreased RBC deformability.Citation6,Citation7 RBCs of patients with T2DM aggregate more readily than those of normal subjects. The abnormalities have been shown to markedly increase whole-blood viscosity, and the increased blood viscosity adversely affects the microcirculation in diabetes, leading to microangiopathy.Citation8 In this study, we investigated the association of RBC count with microvascular complications in Chinese patients with T2DM.
Materials and methods
Study population
The study population comprised 369 patients with T2DM attending the diabetic department of our hospital between January 2011 and July 2011. The patients we studied with different disease duration were mainly from northeast China and were mostly Han people, which is the largest ethnic group in the People’s Republic of China. Patients with known hematologic diseases, such as hemolytic anemia, neoplastic metastases to marrow, pregnancy, severe arthritis, hypothyroidism, liver cirrhosis, posthemorrhagic anemia, renal anemia, inflammatory bowel diseases, and serious infection, in the past month that may have affected RBC count were excluded from the study.
Diagnosis of T2DM was established using World Health Organization 1999 criteria. The diagnostic criteria for DN, DPN, and DR were based upon the guidelines for T2DM treatment and prevention in the People’s Republic of China (2010 edition).Citation9 DR was defined by the presence of microaneurysms and/or retinal hemorrhage and/or neovascularization. DN was defined as microalbuminuria (30–300 mg/24 hours’ urinary protein excretion) or macroalbuminuria (>300 mg/24 hours’ urinary protein excretion). DPN was diagnosed based on clinical symptoms of allodynia/abnormal ankle reflex/abnormal vibration sense or pressure sense abnormality. Data analyzed included age, sex, diabetes duration, smoking status, alcohol consumption, antihypertensive, antilipidemic, and antidiabetic medication, blood pressure, body mass index (BMI), fasting blood glucose, glycated hemoglobin (HbA1c), lipid levels (including total cholesterol, high-density lipoprotein [HDL] cholesterol, triglycerides, and low-density lipoprotein [LDL] cholesterol), RBC count, hemoglobin, RBC distribution width (RDW), platelet count, and white blood cell (WBC) count. The study protocol was assessed and approved by the institutional ethics committee of the First Affiliated Hospital of China Medical University.
Laboratory assays
Blood samples were obtained from fasting patients. Two milliliters of venous blood was collected directly in an ethylenediaminetetraacetic acid vacutainer in sitting position from antecubital vein and analyzed after exactly 2 hours. Plasma glucose was measured by the hexokinase method (7600-100 automated analyzer; Hitachi, Tokyo, Japan). HbA1c was measured using high-performance liquid chromatography (Variant II HbA1c HPLC System; BioRad Laboratories, Hercules, CA, USA). Total cholesterol (cholesterol oxidase method), triglycerides (removing free glycerol method), and HDL cholesterol (chemically modified enzyme method) were measured on the Hitachi 7600-110 automated analyzer using reagent kits supplied by Kyowa Medex (Tokyo, Japan). LDL cholesterol (selective melting method) was measured on the Hitachi 7600-110 automated analyzer using reagent kits supplied by Kyowa Medex. Urinary creatinine was measured by enzymatic methods on the Hitachi 7600-110 automated analyzer using reagent kits supplied by Kyowa Medex. Urinary albumin was measured by immunoturbidimetry on a BN II automated analyzer (Siemens, Munich, Germany) using reagent kits supplied by Kyowa Medex. A complete blood profile was determined using an automated cell counter (XE 2100; Sysmex, Kobe, Japan). The precision performance of these assays was within the manufacturers’ specifications.
Statistical analysis
Data are presented as means ± standard deviation for all normally distributed continuous variables, and median with interquartile ranges for non-normally distributed variables. One-way analysis of variance or Kruskal–Wallis tests were used as appropriate for between-group comparisons for continuous variables. Using data from clinical history, physical examination, and laboratory testing, Pearson’s correlation coefficient was used in the context of normality to test univariate correlations with RBC count, and Spearman’s correlation coefficient was used for correlation testing of non-normally distributed variables. Categorical variables were compared using the chi-squared test. Variables with a P-value < 0.10 in univariate analysis were included in the multivariate model to identify predictors for the occurrence of diabetic microvascular complications. Predictors were removed from the model if their P-value exceeded 0.10. RBC count was grouped into quartiles, and the adjusted odds ratio (OR) for each quartile was determined with the highest quartile as the reference group. The logistic regression model was used to estimate the OR and 95% confidence interval (CI) for diabetic microvascular complications. In the regression analysis, known conventional risk factors for diabetic microvascular complications were included as covariates in the model. All tests were two-sided, and a P-value < 0.05 was considered statistically significant. All data were analyzed by SPSS software (IBM, Armonk, NY, USA).
Results
The study population comprised 369 patients (204 male, 165 female; mean age 56.1 ± 13.6 years). Complete information about diabetic microvascular complications was available for all patients. The patients were stratified into four groups according to quartiles of RBC count, and the baseline characteristics of the groups are presented in . Clinical characteristics and laboratory findings of patients with or without microvascular complications are presented in . The proportion of patients with microvascular complications was 57.2% in male patients and 42.8% in female patients. The mean age of diabetic patients without complications was 50.1 ± 14.2 years, compared with 59.3 ± 12.2 years in the group with complications. The mean RBC count was 4.39 ± 0.67 × 1012/L. Univariate analysis revealed that sex, smoking, alcohol consumption, age, duration of diabetes, BMI, systolic blood pressure, diastolic blood pressure, fasting plasma glucose, HbA1c, HDL cholesterol, triglycerides, WBC count, hemoglobin, RDW, and antihypertensive drugs were significantly different among the four groups (P < 0.05). Correlation analysis revealed positive associations of RBC count with BMI, diastolic blood pressure, fasting plasma glucose, HbA1c, triglycerides, WBC count, and hemoglobin, and negative associations with age, disease duration, systolic blood pressure, HDL cholesterol, and RDW (P < 0.05).
Table 1 Baseline clinical characteristics and laboratory findings of patients with type 2 diabetes mellitus by quartiles of red blood cell count (×1012/L)
Table 2 Clinical characteristics and laboratory findings of type 2 diabetes mellitus patients with or without microvascular complications
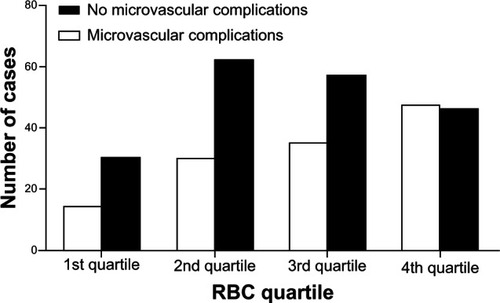
At baseline, the total proportion of patients with microvascular complications was 65.9%. The proportions of DN and DR in patients with microvascular complications were 46.9% and 35.4%, respectively. The proportion of patients with microvascular complications increased as the RBC count decreased (P < 0.001) ().
Figure 1 Percentage of the cases of type 2 diabetes mellitus with or without microvascular complications in patients within each quartile of red blood cell count.
Abbreviation: RBC, red blood cell.
Patients with lower RBC counts remained at increased risk of microvascular complications after adjustment for sex, age, smoking, duration of diabetes, BMI, systolic blood pressure, diastolic blood pressure, HbA1c, HDL cholesterol, triglycerides, WBC count, hemoglobin, RDW, and antihypertensive drugs (P < 0.001). Lower RBC quartiles were associated with a higher risk of microvascular complications compared with the reference group (first quartile, OR 4.98, 95% CI 1.54–6.19, P = 0.008; second quartile, OR 3.21, 95% CI 1.17–5.28, P = 0.024). Other independent predictors of microvascular complications in the study included age (OR 1.05, 95% CI 1.02–1.07, P < 0.001), duration of diabetes (OR 1.11, 95% CI 1.07–1.16, P < 0.001), and HbA1c (OR 1.16, 95% CI 1.04–1.29, P = 0.007). After RBC count was entered as a continuous variable into the model, the result did not change: RBC count remained significant. A 1-unit (1 × 1012/L) increase in RBC count was associated with a decreased risk of microvascular complications (OR 0.51, 95% CI 0.28–0.93, P = 0.028), DPN (OR 0.63, 95% CI 0.43–0.91, P = 0.016), DN (OR 0.62, 95% CI 0.40–0.94, P = 0.028), and DR (OR 0.57, 95% CI 0.46–0.96, P = 0.003).
Discussion
The principal finding of this study is that lower RBC counts, as reflected by RBC quartiles, are an independent predictor of the risk of microvascular complications in patients with T2DM, after controlling for conventional risk factors, including smoking, diabetes duration, BMI, blood pressure, lipids, and glucose.
Our data demonstrated that the risk of microvascular complications was 4.98-fold higher in patients with an RBC count < 4.07 × 1012/L and 3.21-fold higher in patients with an RBC count 4.08–4.43 × 1012/L than in those with an RBC count > 4.84 × 1012/L. The OR of microvascular complications increased in a stepwise manner with a decrease in quartile of RBC count.
The hypothesis for the mechanism of the correlation between RBC count and microvascular complications might be that it is partly mediated through an effect of decreased RBC count on RBC function. There have been a few studies to support this notion in patients with DM in the available literature. First, structural alterations of the RBC membrane proteins are associated with the development of microvascular complications in diabetes.Citation10 Chronic hyperglycemia causes nonenzymatic glycosylation of RBC membrane proteins, which reduces the negative surface electric charge, leading to accelerated aging of RBCs.Citation11–Citation13 The decreased RBC count can further reduce the negative charge of RBCs. Sialic acid moieties of RBC membrane glycoproteins are the principal determinants of the negative charge on the cell surface. The decreased cell surface charge is thought to firm adhesion between surfaces.Citation14 The resultant electrostatic repulsion between the cells diminishes RBC aggregation, resulting in low shear-rate viscosity and yield stress of blood.Citation15,Citation16 Therefore, a decrease in the negative charge of RBCs may increase microviscosity, aggregation, and adhesiveness of RBCs. The decrease of surface charge leads to a collinear decrease of membrane deformability.Citation17 RBC velocity becomes intermittent and/or RBCs come to a complete standstill when RBCs entering and moving through capillary segments are decreased by a reduction in the net surface charge of RBCs.Citation18 Older RBCs demonstrate increased mechanical fragility, decreased deformability, and increased ability to aggregate compared with younger RBCs.Citation19 Some hemoglobin molecules of aging RBCs are aggregated and attach to the inside of the cell membrane.Citation17 The binding of hemoglobin to the inside of the cell membrane can lead to a reduction in membrane flexibility and influence the oxygenation of hemoglobin.Citation20 A low RBC negative charge in patients with T2DM is also associated with DR and changes in the properties of the retinal basement membrane.Citation21 These changes cause breakdown of the blood–retinal barrier, which results in capillary hyperpermeability and leakage of proteins into the deep and superficial layers of the retina.Citation22 In normal mammalian cells, phosphatidylserine, which contains a negative charge, is exclusively confined to the inner layer of the plasma membrane.Citation23,Citation24 Increased intracellular oxidative stress can impair maintenance of phospholipid asymmetry, resulting in phosphatidylserine externalization.Citation25 Loss of this asymmetric distribution and exposure of phosphatidylserine on the external surface generate a thrombogenic surface and signal macrophages to remove cells by phagocytosis.Citation26 An enhancement of blood coagulation was also observed in the presence of erythrocytes, leukocytes, and phosphatidylserine.Citation27
Second, reduced hemoglobin levels independently identify diabetic patients with an increased risk of microvascular complications.Citation28,Citation29 Anemia causes tissue hypoxia that has a multitude of fibrogenic and mitogenic effects in an already-compromised kidney via expression of multiple growth factors, hormones, vasoactive reagents, and enzymes.Citation30,Citation31 Hypoxia can also contribute to renal vasoconstriction by stimulating the sympathetic nervous system and resultant activation of the intrarenal renin–angiotensin system.Citation32 The renal vasoconstriction may initiate nephropathy. In this study, the RBC count showed a positive correlation with the serum hemoglobin level. The decrease in RBC count in diabetics may contribute to the occurrence of microvascular complications mediated by a decreased hemoglobin level.
Third, erythropoietin deficiency results in normochromic normocytic anemia that occurs early in DN, often prior to the decline in renal function.Citation33 Therefore, the RBC count in normochromic normocytic anemia may provide some indication of damage to the cells and vascular architecture of the renal tubulointerstitium associated with DN that may be apparent before demonstrable changes in renal function.Citation34 Anemia in early DN is also induced by a poor response of erythropoietin to low hemoglobin levels as a result of impaired sensing mechanisms associated with autonomic DN.Citation35
In addition, higher values of RDW reflect greater variation in the distribution of RBC volumes. Higher RDW values are associated with increased risk for cardiovascular disease and nephropathy in adult patients with diabetes.Citation36,Citation37 Increased RDW was associated with decreased RBC deformability, which can impair blood flow through the microcirculation.Citation38 RBC deformability plays a role, as elevated RDW is associated with increased inflammation and decreased levels of antioxidants.Citation39 Moreover RDW is elevated in conditions of ineffective red cell production (eg, iron deficiency, anemia of chronic disease, B12 or folate deficiency) and increased red cell destruction (eg, hemolysis).Citation40
These results suggest that RBC count is a potential candidate to improve further our ability to identify patients at high risk of developing microvascular complications and institute appropriate preventive measures. The work described here may motivate further studies in comparisons of RBC concentration and microcirculation using Doppler perfusion imaging or laser speckle perfusion imaging for the investigation of tissue microcirculation.Citation41 The present findings are limited in their ability to eliminate causal relationships between RBC count and microvascular complications in T2DM. Further prospective population-based studies are needed to investigate the mechanisms in order to answer these questions.
In conclusion, a decreased RBC count is associated with microvascular complications in Chinese patients with T2DM. It indicated that lower RBC counts may be related to RBC membrane protein alterations, a decrease in hemoglobin levels, and erythropoietin deficiency.
Disclosure
The authors report no conflicts of interest in this work.
References
- HinnenDThe role of the kidney in hyperglycemia: a new therapeutic target in type 2 diabetes mellitusJ Cardiovasc Nurs201328215716522343215
- ChoiSKGalánMKassanMPartykaMTrebakMMatrouguiKPoly(ADP-ribose) polymerase 1 inhibition improves coronary arteriole function in type 2 diabetes mellitusHypertension20125951060106822454481
- JindalSGuptaSGuptaRPlatelet indices in diabetes mellitus: indicators of diabetic microvascular complicationsHematology2011162868921418738
- TongPCLeeKFSoWYWhite blood cell count is associated with macro- and microvascular complications in Chinese patients with type 2 diabetesDiabetes Care200427121622214693992
- StamlerJVaccaroONeatonJDWentworthDDiabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention TrialDiabetes Care19931624344448432214
- HoareEMBarnesAJDormandyJAAbnormal blood viscosity in diabetes mellitus and retinopathyBiorheology19761312125938738
- SchwartzRSMadsenJWRybickiACNagelRLOxidation of spectrin and deformability defects in diabetic erythrocytesDiabetes19914067017082040386
- ChoYIMooneyMPChoDJHemorheological disorders in diabetes mellitusJ Diabetes Sci Technol2008261130113819885302
- AssociationCDGuideline for the diagnosis and treatment of type 2 diabetes in China (2010 edition)Chin J Diabetes2012201S1S36
- PetropoulosIKMargetisPIAntonelouMHStructural alterations of the erythrocyte membrane proteins in diabetic retinopathyGraefes Arch Clin Exp Ophthalmol200724581179118817219119
- MillerJAGravalleseEBunnHFNonenzymatic glycosylation of erythrocyte membrane proteins. Relevance to diabetesJ Clin Invest19806548969017358849
- BabaYKaiMSetoyamaSOtsujiSThe lower levels of erythrocyte surface electric charge in diabetes mellitusClin Chim Acta1978841–2247249639309
- MazzantiLFaloiaERabiniRADiabetes mellitus induces red blood cell plasma membrane alterations possibly affecting the aging processClin Biochem199225141461312917
- MegeJLCapoCBenolielAMBongrandPUse of cell contour analysis to evaluate the affinity between macrophages and glutaraldehyde-treated erythrocytesBiophys J19875221771863117125
- RogersMEWilliamsDTNiththyananthanRRamplingMWHeslopKEJohnstonDGDecrease in erythrocyte glycophorin sialic acid content is associated with increased erythrocyte aggregation in human diabetesClin Sci (Lond)19928233093131312416
- McMillanDEUtterbackNGWujekJJEffect of anionic amphophiles on erythrocyte propertiesAnn N Y Acad Sci19834166336416587820
- HuangYXWuZJMehrishiJHuman red blood cell aging: correlative changes in surface charge and cell propertiesJ Cell Mol Med201115122634264221435169
- VinkHWieringaPASpaanJAEvidence that cell surface charge reduction modifies capillary red cell velocity-flux relationships in hamster cremaster muscleJ Physiol1995489Pt 11932018583403
- KamenevaMVAntakiJFBorovetzHSMechanisms of red blood cell trauma in assisted circulation. Rheologic similarities of red blood cell transformations due to natural aging and mechanical stressASAIO J1995413M457M4608573845
- IdeguchiHEffects of abnormal Hb on red cell membranesRinsho Byori1999473:232237 Japanese10228388
- BudakYDemirciHAkdoganMYavuzDErytrocyte membrane anionic charge in type 2 diabetic patients with retinopathyBMC Ophthalmol200441415473902
- D’AmicoDJDiseases of the retinaN Engl J Med19943312951068208273
- ZwaalRFSchroitAJPathophysiologic implications of membrane phospholipid asymmetry in blood cellsBlood1997894112111329028933
- KimelbergHKDifferential distribution of liposome-entrapped [3H] methotrexate and labelled lipids after intravenous injection in a primateBiochim Biophys Acta19764484531550823974
- KannoHCritical role of phosphatidylserine in hemolysis due to red blood cell enzyme/membrane defectsNihon Rinsho2008663461468 Japanese18330023
- NeidlingerNALarkinSKBhagatAVictorinoGPKuypersFAHydrolysis of phosphatidylserine-exposing red blood cells by secretory phospholipase A2 generates lysophosphatidic acid and results in vascular dysfunctionJ Biol Chem2006281277578116278219
- MiyamotoMSasakawaSOzawaTKawaguchiHOhtsukaYMechanisms of blood coagulation induced by latex particles and the roles of blood cellsBiomaterials19901163853882207226
- KeaneWFBrennerBMde ZeeuwDThe risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: the RENAAL studyKidney Int20036341499150712631367
- ThomasMCAnemia in diabetes: marker or mediator of microvascular disease?Nat Clin Pract Nephrol200731203017183259
- DeicherRHörlWHAnaemia as a risk factor for the progression of chronic kidney diseaseCurr Opin Nephrol Hypertens200312213914312589173
- FineLGBandyopadhayDNormanJTIs there a common mechanism for the progression of different types of renal diseases other than proteinuria? Towards the unifying theme of chronic hypoxiaKidney Int Suppl200075S22S2610828757
- GrunwaldJERivaCESinclairSHBruckerAJPetrigBLLaser Doppler velocimetry study of retinal circulation in diabetes mellitusArch Ophthalmol198610479919962942132
- KimMKBaekKHLimDJErythropoietin response to anemia and its association with autonomic neuropathy in type 2 diabetic patients without advanced renal failureJ Diabetes Complications2010242909519303331
- ThomasMTsalamandrisCMacIsaacRJerumsGAnaemia in diabetes: an emerging complication of microvascular diseaseCurr Diabetes Rev20051110712618220587
- McGillJBBellDSAnemia and the role of erythropoietin in diabetesJ Diabetes Complications200620426227216798479
- TonelliMSacksFArnoldMRelation between red blood cell distribution width and cardiovascular event rate in people with coronary diseaseCirculation2008117216316818172029
- MalandrinoNWuWCTaveiraTHWhitlatchHBSmithRJAssociation between red blood cell distribution width and macrovascular and microvascular complications in diabetesDiabetologia201255122623522002006
- PatelKVMohantyJGKanapuruBHesdorfferCErshlerWBRifkindJMAssociation of the red cell distribution width with red blood cell deformabilityAdv Exp Medicine Biol2013765211216
- SembaRDPatelKVFerrucciLSerum antioxidants and inflammation predict red cell distribution width in older women: the Women’s Health and Aging Study IClin Nutr201029560060420334961
- AllenLAFelkerGMMehraMRValidation and potential mechanisms of red cell distribution width as a prognostic marker in heart failureJ Card Fail201016323023820206898
- O’DohertyJMcNamaraPClancyNTEnfieldJGLeahyMJComparison of instruments for investigation of microcirculatory blood flow and red blood cell concentrationJ Biomedical Opt2009143034025