Abstract
Purpose
Hypertension (HT) can cause renal complications or deterioration of kidney function. HT management is very important because it reduces the severity of illnesses. This study aimed to investigate the relationship between health literacy (HL), self-care behaviors (SCB), and biochemical parameters in hypertensive patients with renal complications.
Methods
A cross-sectional study of 405 hypertensive patients with renal complications among Tai Lue people living in Thailand was conducted using simple random sampling. Face-to-face interviews with questionnaires were used to collect information. Blood pressure (BP) and biochemical parameters, such as fasting blood sugar (FBS) and estimated glomerular filtration rate (eGFR), were measured.
Results
The participants’ mean age was 68.3 years. A significant correlation was found between HL score, SCB score, systolic BP (SBP), diastolic BP (DBP), FBS, and eGFR (p<0.01). Multiple linear regression revealed that eating salty foods was a risk factor for SBP in males and for SBP and DBP in females. Body mass index (BMI) (B = 0.54), sweet food consumption (B = 13.90), and SCB score (B = −0.29) were significantly associated with FBS level (R2 = 17.8%, p<0.05). Employment (B = 2.55), eating bland food (B = 4.07), receiving information from family (B = 3.53), SCB (B= 0.31), and age (B = −0.51) were all significant factors for eGFR (R2 = 35.0%, p<0.05).
Conclusion
HL and SCB levels were associated with the health of hypertensive patients with renal complications in the Tai Lue ethnic community. The significance of organizing health education programs is to emphasize increasing HL to lead to self-care decisions and reduce complications in patients, resulting in improved SCB and quality of life in the future.
Introduction
Untreated or uncontrolled high blood pressure (BP) is an important risk factor for the progression of chronic kidney disease (CKD), leading to morbidity and death.Citation1,Citation2 When the estimated glomerular filtration rate (eGFR) is low, the kidney does not work optimally, and the incidence and severity of HT tend to increase.Citation3 HT prevalence in adults with CKD is 60.0%.Citation3,Citation4 High BP has been identified as a major risk factor for the development of non-communicable diseases such as heart diseases, stroke, and chronic renal failure.Citation4,Citation5 The number of new cases of HT is expected to increase by 29.0% by 2025 to approximately 1.15 billion people.Citation6 HT adversely affects the kidneys and contributes to physical dysfunction among patients, especially in elderly people.Citation7
In Thailand, the death rate from HT was 13.10, 13.15, and 14.20 per 100,000 people in 2017–2019.Citation8 The leading causes of patients with CKD receiving renal replacement therapy in 2020 were HT (42.3%) and diabetes (41.5%).Citation9 Phayao Province is in north Thailand, with diverse ethnicities, cultures, and traditions. Eight ethnic minorities live there: the Hmong, the Mien, the Lisu, the Lu, the Lua, Thai highlanders, Tai Lue, and Thai Northeastern people,Citation10 each with their own culture, language, and way of life. Minority groups have traditional SCB, including using local herbs, performing rituals, and ways of daily cooking.Citation11 Phayao Province is in the top 10 provinces in terms of deaths from HT, reporting a rate of 18.21–24.05 per 100,000 people.Citation12 HT was found to be very high among the Tai Lue ethnic group, especially in people aged 60 years and over (45.48%); 53.37% were patients with CKD stages 1–3 complications, more than other ethnic groups.Citation10 However, hypertension among older adults living in Thai communities can be prevented by self-care behaviors (SCB).Citation13
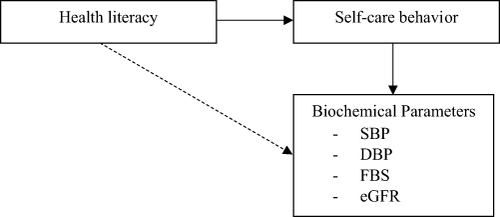
Health literacy (HL) is the ability to obtain the knowledge, skills, and confidence to take action toward health and understand necessary health information and services to make appropriate health decisions.Citation14,Citation15 Individuals with higher education levels or socioeconomic status can have low HL if they struggle to understand and apply health information effectively.Citation15,Citation16 Furthermore, HL is an effective factor in BP control for understanding BP measurements, risk factors and complications, necessary lifestyle changes, and treatment goals.Citation17,Citation18 A previous study found numerous factors associated with SCB in hypertension patients with complications,Citation19 but the association between HL, SCB, and health outcomes is limited. Therefore, this study aimed to investigate the associations of HL, SCB, and blood biological parameters among hypertensive patients with renal complications in elderly Tai Lue people, based on the conceptual framework shown in (). The findings can be used to adjust strategies for increasing knowledge and improving SCBs among hypertensive patients with renal complications in order to reduce disease severity and slow renal deterioration.
Methodology
Study Design and Sample Selection
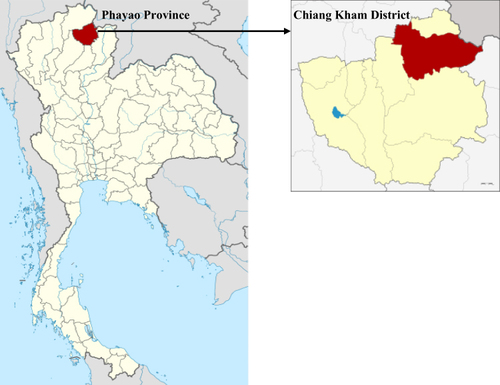
This cross-sectional study was conducted between January and May 2023. Purposive sampling was employed to select a study area in Chiang Kham District, Phayao Province with a population including more than 20% of Tai Lue people (). However, few studies were found using a theoretical concept framework focusing on an ethnic group. Simple sampling using lottery techniques was used to select research sites in ten sub-districts of Chiang Kham District, and five subdistricts were chosen: Yuan, Wiang, Fai Kwang, Nam Wan, and Chiang Ban. The researcher drew lots from the registries of hypertensive patients with kidney disease complications from Chiang Kham Hospital’s HosXP system version 4.0. The sample size calculation used Khazaie’s formula,Citation20 n = [(Zα/2 x σ)/E]² when the population standard deviation (SD) is unknown: n = number of samples, Zα/2 = standard score at 95% confidence level (1.96), σ = SD, and E = acceptable value for tolerance error (σ/10). The number of 385 participants resulted. Adding a 5% to prevent loss of the sample or incomplete data, 405 people participated in the study.
Figure 2 Location of this study area in Chiang Kham District in Phayao, Thailand.
The inclusion criteria were females and males ≥ 60 years, an individual who has been diagnosed with hypertension and renal complications and has had at least one of these features detected for three months, such as albumin excretion rate (AER) > 30 milligrams per day or eGFR < 60 mL/min/1.73 m2Citation9 and registered in the HosXP. system version 4.0 (Secondary care) and HosXP Primary care unit (PCU) Phayao Province for at least 6 months, Tai Lue persons registered by the Highland Health Development Center and the municipality and residing in Chiang Kham District for at least 6 months, able to communicate in the local language, and who signed a written consent form and volunteered to participate. Persons with cognitive impairments, dementia, and blindness were excluded. Prior to conducting the research, an announcement was made to recruit research assistants from each subdistrict. The assistants included a nurse, two public health academics, and three village health volunteers. A meeting was held to clarify the study purpose, the data collection process, techniques for completing the questionnaires, the participants’ rights, privacy, re-checking the data, and related research matters step by step to ensure that everyone understood the process and took the same direction. The researcher translated the official language into the local language for the research assistants to ensure that the questionnaires’ meanings stayed the same. For the data collection process, the researcher liaised with the District Public Health Office, Chiang Kham Hospital, and the Health Promoting Hospital in subdistrict. After obtaining the participants’ written consent, the questionnaires were distributed. The questionnaires were self-administered by literate persons; the research assistant interviewed people who were illiterate face-to-face. The interviews were scheduled at the participant’s home or the subdistrict Health Promoting Hospital between 9:00 a.m. and 5:00 p.m. or when convenient and lasted 20–30 minutes each.
Data Collection Instruments and Procedure
The quantitative data collection tools were developed from a literature review and previous research. The researcher adapted the interview questionnairesCitation22 for use in rural areas and different ethnic groups, using a conceptual framework based on HL development.Citation23 The questionnaire comprised three parts: 1) sociodemographic information (age, gender, education, income, occupation, health status, BMI, food consumption, smoking, alcohol drinking, HT, and access to health services); 2) HL divided into six components, namely (i) ability to access information on HT and health services, (ii) HT knowledge (on pathogenesis, causes and symptoms, complications, risk behaviors, and abnormal conditions), (iii) health communication (communication about HT, requesting help, and interactions among family members, friends, or patients, village health volunteers, health staff, and people in the community), (iv) the ability to make informed decisions about HT and its prevention, and (v) health management and behavioral modification for HT prevention, focusing on daily self-reminders, competencies and skills for HT prevention and control, unhealthy food consumption and control, exercise, medication, stress management, and observation of any abnormalities or changes in the disease. The last component (vi) was on media literacy on health information, including questions focused on decision-making on reliable sources of information, healthy products, and preventive practice for HT. Part 2 contained 6 questions per section, totaling 36 items. The characteristic of the questions were multiple choices, namely Yes, Not Sure, and No. The scoring criterion was, if correct equals to 1 point and if wrong equals to 0 points. The total score ranged from 0–36 points, and they were divided into 3 levels: critical literacy level (≥ 28 points), interactive literacy level (21–27 points), and functional literacy level (scores ≤ 20 points). Part 3 of the questionnaire focused on SCB in HT prevention:Citation22 food consumption (10 items, not including food taste), medication (10 items), exercise (10 items), and stress management and relaxation (10 items), totaling 40 items. The questions were measured with a three-level rating scale never practiced, rarely practiced (1–3 times/week), and regularly practiced (4–7 times/week), divided into 3 levels: high scores ≥ 80% (≥ 96 points), moderate scores between 60% and 79% (73–95 points) and low scores < 60% (≤ 72 points). Before using the questionnaires in the field, a try out was performed on 30 elderly people who had similar characteristics to those in the study. HL precision of Kuder-Richardson Formula: KR20 = 0.88. And for SCB questionnaire, the reliability was analyzed using Cronbach’s alpha coefficient which was 0.87.
Biochemical Parameters
The participants’ blood samples were taken. They were prepared for a day, with holding water and food for at least 12 hours after 8:00 p.m. before arriving for blood collection at 7:00 a.m. the next morning. Medical technicians or professional nurses took 5 cc of blood from the patients and transported it to Chiang Kham Hospital’s lab room. The blood biological indicators included fasting blood sugar (FBS) and eGFR, which was computed from creatinine using the CKD-EPI Equation.Citation9 Systolic BP (SBP) and diastolic BP (DBP) were measured using an automatic blood pressure measurement device.
Statistical Analyses
Data were analyzed by SPSS Version 17 (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± SD for normally distributed data. Categorical variables are expressed as numerals (percentages). The Pearson correlation coefficient (r) was used to investigate relationships between variables such as HL, SCB, SBP, DBP, and chemical indicators (FBS and eGFR). Multiple linear regression using the stepwise method was used to identify factors such as general characteristics and self-care behavior that are associated with SBP, DBP, FBS, and eGFR in hypertensive patients with renal complications. The level of statistical significance was set at 0.05.
Results
Participant and Variables
Of the 405 participants, over half were female (64.0%), and the average age was 68.29 years (SD= 6.82, Min.-Max. = 60–94). Most participants (75.6%) were educated, had adequate income (66.7%), and worked (58.3%). Regarding food consumption, many (44.4%) ate bland food, followed by salty food (39.8%). They smoked cigarettes (8.9%) and drank alcohol (28.1%). Almost all received information from public health officers (93.1%), followed by village health volunteers, family, radio/television/announcements, and the internet/online media (82.5%, 46.7%, 30.9%, and 20.2%, respectively). In health terms, nearly half (45.7%) had a normal BMI, and 28.6% had obesity (mean =23.20, SD =3.34, Min.-Max. = 15.26–35.04). Considering HL levels, almost half had a functional literacy level (41.5%), followed by a critical literacy level (30.4%), and an interactive literacy level (28.1%) (mean 22.46, SD 6.15, range 5–33). In terms of SCB, the participants’ scores were moderate (37.5%), high (32.3%), and low (30.2%) (mean =86.17, SD =15.48, Min.-Max. = 59–115). More than half had normal (65.2%) (<140 mmHg) SBP levels, with 34.8% having abnormal levels (mean =133.46, SD =13.09, Min.-Max. = 91–184). Most DBP levels were normal (87.9%) (<90 mmHg) followed by abnormal (12.1%) (mean= 78.35, SD =8.69, Min.-Max. = 54–103). In terms of blood biological parameters, more than half had eGFR at stage 2 (66.2%), followed by stage 1 (21.7%), stage 3 (11.9%), and stage 4 (0.2%) (mean =77.19, SD= 14.04, Min.-Max. = 27.47–99.16). Nearly 15% had abnormal FBS (14.8%) (≥ 110 mg/dL) (mean =96.99, SD = 17.34, Min.-Max. = 70–195) ().
Table 1 The Level of Health Literacy, Self-Care Behaviors, and Blood Biological Parameters Among Participants (n=405)
Correlation Between Research Variables
The relationship between the HL score and the six HL components was statistically significant (p<0.01) (). The Pearson correlation coefficients were highest (r = 0.648) between the communication and decision-making domains. shows the relationship between all the study variables: HL, SCB, SBP, DBP, FBS, and eGFR. The total HL score was significantly correlated with the SCB score (r = 0.858), SBP (r = −0.420), DBP (r = −0.199), FBS (r = −0.251), and eGFR (r = 0.487). The SCB score was significantly correlated with SBP (r = −0.486), DBP (r = −0.225), FBS (r = −0.318), and eGFR (r = 0.504).
Table 2 Pearson Correlation Coefficients (r) Between Each Domain of Health Literacy Among Participants
Table 3 Pearson Correlation Coefficients (r) Between Health Literacy, Self-Care Behaviors, Blood Pressure, FBS, and eGFR Among Participants
Factors Associated with Clinical Indicators
shows the factors associated with BP levels, separately by sex, in hyper-tensive patients with renal complications using multiple linear regression. In the males, eating salty food (B = 6.21) and the SCB score (B = −0.31) were significant factors for the SBP level (R2 = 31.7%, p<0.05), but only the SCB score (B = −0.15) was a significant factor for the DBP level (R2 = 6.6%, p < 0.05). In the females, eating salty food (B = 4.87), receiving information from village health volunteers (B = −6.87), receiving information from radio/television/ announcements (B = −3.58), and the SCB score (B = −0.21) were all significant factors for the SBP level (R2 = 26.3%, p<0.05), whereas BMI (β = 3.21) and eating salty food (B = 0.39) were significant factors for the DBP level (R2 = 5.6%, p<0.05). The FBS level was significantly related to BMI (B = 0.54), sweet food consumption (B = 13.90), and SCB score (B = −0.29), accounting for 35.0% of the variance in FBS (). The protective factors for eGFR included employment (B = 2.55), eating bland food (B = 4.07), receiving information from family (B = 3.53), and SCB (B = 0.31), while age (B = −0.51) was a risk factor (R2 = 35.0%, p<0.05).
Table 4 SCB and Other Factors Associated with BP Level Among Participants Using Stepwise Linear Regression, Separately by Sex
Table 5 SCB and Other Factors Associated with FBS and eGFR Among Participants Using Stepwise Linear Regression
Discussion
HL Correlated with SCB and Biochemical Parameters
The findings of the research revealed associations between HL, SCB, and blood biological parameters such as BP, FBS, and eGFR among hypertensive patients with renal complications who were elderly Tai Lue people residing in rural northern Thailand. The participants’ eGFR was mostly stage 2 (66.2%), abnormal FBS was low (14.8%), and almost half had a functional literacy level. When the six HL components were classified, the scores for ability to assess knowledge about HT and health services and cognitive skills were low and moderate, respectively.
HL scores were statistically significantly correlated with SCB, SBP, DBP, FBS, and eGFR. The HL items with low scores were information on HT and its complications: uncontrolled BP, HT leading to kidney failure, and a BP of 140/90 mmHg considered normal. This aligns with a systematic review that found that low HL is a major risk factor for poor BP control, leading to adverse health outcomes.Citation24 Interactive HL, which was the lowest in this study, refers to cognitive and social skills to actively participate in everyday situations and make informed choices to improve healthy behaviors.Citation25 Knowledge of HT was significantly associated with SCB (eg, weight control and medication intake), in line with research in Iran.Citation26 Some studies also indicate that patients with high knowledge of diabetes are 1.85 times more likely to achieve glycemic control goals than patients with low knowledge of diabetes.Citation27 Consistent with a previous study in northern Thailand, HL was statistically significantly associated with FBS and HbA1C.Citation28
Almost half the participants had moderate SCB scores. Considering the questionnaire’s individual items, the participants had poor food consumption behavior, in particular adding high amounts of seasoning (eg, salt, fish sauce, soy sauce) when cooking, eating food containing monosodium glutamate and high-sodium foods (eg, salted fish, fermented fish, rotten beans, and pickled mustard, a local food). Previous research indicates that most SCBs are moderate to low, which can be explained by social, cultural, and self-management factors, folk medicine treatment, self-medication by buying from a drugstore, beliefs and traditional treatment, and lifestyles being risk factors affecting SCB.Citation29 This aligns with a study in Ethiopia that showed an overall level of self-care of 53.1%.Citation30 Several studies have indicated that differences in patients’ SCBs are due to factors such as HL levels and/or self-care attitudes.Citation31,Citation32
SCB and Other Factors Associated with Biochemical Parameters
Analyzing the relationship of variables, eating salty foods and SCB were associated with SBP levels in the males, while eating salty foods, receiving information from health volunteer and radio/TV/announcements, and SCB were associated with SBP levels in the females. SCB is a cost-effective tool in health management and preventing HT and its complications.Citation30–32 People with uncontrolled BP have been found to be twice as likely to have poor self-management as people with high BP (p=0.003) and poor social support; both are independent predictors of poor SCB.Citation30 Also, SCBs were correlated with DBP levels in the males. BMI, eating salty foods, and SCB were statistically correlated with DBP levels in the females. Previous studies suggest differences may relate to differences in populations, livelihoods, cultures, economic status, and health facility access.Citation30 Consistent with a study by Irwan, food consumption in Southeast Asia continues to be closely affected by culture in terms of saltiness, oiliness, and using coconut milk in cooking.Citation33 Some studies suggest that females are at increased risk of DBP and likelier to have health complications compared to males.Citation34 BMI, salt intake, and smoking are associated with SCB and statistically significantly affect BP.Citation33,Citation35 The long-term effects of uncontrolled BP may increase the incidence of CKD.Citation36
We found that BMI, sweet food consumption, and SCB had statistically significant relationships with FBS with 17.8% variance. The participants had poor food consumption behaviors, which can be explained by the uniqueness of the Tai Lue community in term of indigenous food, a traditional way of life, and culture; they lack awareness to make the right food choices, resulting in poor dietary and health behaviors.Citation11 Similar to a study among ethnic northern Thais, the study participants mostly had moderate and low SCB scores; increased BMI was significantly associated with SCB and affected FBS.Citation29 This study’s results are similar to those of research in India that reported that 62.9% of respondents’ SCB level were unfavorable, influenced by negative perceptions of health status (odds ratio = −2.8).Citation37
Age, occupation, eating bland food, receiving information from family and SCB were significantly associated with eGFR with 35.0% variance. The results are similar to a previous study that described SCB as the ability to take care of oneself and perform necessary activities to achieve, maintain, or promote optimal health; self-care is individuals’ ability to deal with illness, disability, economic status, and access to health information from various sources.Citation38 Diet is one of the main management modalities for alleviating metabolic disorders and renal function deterioration.Citation38,Citation39 A study in Taiwan concluded that age and a BMI < 24 kg/m2 were significantly associated with CKD patients’ self-care,Citation39 and other research found that SCB and disease awareness in patients with CKD are closely related.Citation38,Citation40 Therefore, good SCB is one of the best ways to alleviate the adverse outcomes associated with CKD.
Limitations and Recommendations
This study has several limitations. First, the participants were ethnic Tai Lue people residing in Chiang Kham District, Phayao Province; therefore, our findings cannot be representative of other populations across the country, highlighting the need for caution in interpreting the effects of study results in diverse populations. Second, this cross-sectional study could not draw causal conclusions but only link the relationships among HL, SCB, BP levels, and blood biological parameters. Third, reporting bias cannot be eliminated. Although the study tool was adapted from previous research and the questionnaire was tested for validity and reliability, the results may not be able to verify causal relationships among HL, SCB, BP level and chemical indicators because the context is different, and there may be discrepancies from the interviews in which the participants did not provide truthful information. Because the researcher is on the local public health team, future studies should focus on other factors associated with HT such as duration of illness, amount of drug used per day, albuminuria, and history of NSAID or steroid use and include the use of herbal medicines and dietary supplements. Prospective and randomized studies are required to confirm whether the cross-sectional findings can be translated into clinically useful interventions. A qualitative study of healthcare teams should be conducted on interventions to encourage patient involvement in health behaviors that help slow the progression of CKD and improve the quality of life among Tai Lue people.
Conclusion
HL was associated with SCB, which may have an impact on BP levels, FBS, and eGFR control in elderly hypertensive patients with renal complications. These data can be used to improve renal function and develop a care plan for patients with high BP, such as improving HL by emphasizing access to accurate and reliable disease information, communicating, and making informed decisions about healthcare options to avoid complications. Furthermore, self-management skills programs that enable patients to address dietary choices, weight control, social support, and other relevant personal factors will result in positive health outcomes and help delay the progression of kidney deterioration.
Ethical Approval and Information Consent
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the University of Phayao Human Ethics Committee, Thailand (UP-HEC 1.3/004/66 approved 15 December 2022). The trial was registered participants gave a written informed consent prior to data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors also express their deepest gratitude to all participants for their contribution to the study.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study will be available upon reasonable request from the first author. Email: [email protected]
Additional information
Funding
References
- Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D. Predictors of new-onset kidney disease in a community-based population. JAMA. 2004;291(7):844–850. doi:10.1001/jama.291.7.844
- Bidani AK, Griffin KA. Pathophysiology of hypertensive renal damage: implications for therapy. Hypertension. 2004;44(5):595–601. doi:10.1161/01.HYP.0000145180.38707.84
- Muntner P, Anderson A, Charleston J, et al. Chronic Renal Insufficiency Cohort (CRIC) study investigators. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2010;55(3):441–451. doi:10.1053/j.ajkd.2009.09.014
- Ravera M, Noberasco G, Weiss U, et al. CKD awareness and blood pressure control in the primary care hypertensive population. Am J Kidney Dis. 2011;57(1):71–77. doi:10.1053/j.ajkd.2010.08.022
- Hamrahian SM, Falkner B. Hypertension in chronic kidney disease. Adv Exp Med Biol. 2017;956:307–325.
- World Health Organization. World health statistics; 2014. Available from: https://apps.who.int/iris/bitstream/handle/10665/112738. Accessed Jul 1, 2022.
- Kithas PA, Supiano MA. Hypertension and chronic kidney disease in the elderly. Adv Chronic Kidney Dis. 2010;17(4):341–347. doi:10.1053/j.ackd.2010.04.003
- Non-communicable disease control division, department of disease control, ministry of public health Thailand: number and rate of hypertension and chronic kidney disease data. Available from: http://www.thaincd.com/2016/media-detail.php?id=14287&tid=&gid=1-015-005. Accessed July 1, 2023.
- The nephrology society of Thailand: Thailand renal replacement therapy year; 2020. Available from: https://www.trtregistry.org. Accessed July 1, 2022.
- Health data center Phayao province Thailand: non-communicable diseases data; 2020. Available: https://pyo.hdc.moph.go.th/hdc/main/index.php. Accessed July 1, 2022.
- Boonyathee S, Ong-Artborirak P, Seangpraw K, et al. Level of hemoglobin A1c, and quality of life among agricultural workers of various ethnicities in Thai border communities. Front Med. 2022;9:796955. doi:10.3389/fmed.2022.796955
- Department of Disease Control, Ministry of public Thailand: number and rate of non-communicable diseases data; 2020 Available from: http://www.thaincd.com/2016/media-detail.php?id=13865&tid=&gid=1-015-005. Accessed July 1, 2022.
- Boonyathee S, Seangpraw K, Ong-Artborirak P, et al. Effects of a social support family caregiver training program on changing blood pressure and lipid levels among elderly at risk of hypertension in a northern Thai community. PLoS One. 2021;16(11):e0259697. doi:10.1371/journal.pone.0259697
- Nielsen-Bohlman L, Panzer AM, Kindig DA; Institute of Medicine (US). Committee on Health Literacy. In: Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press (US); 2004.
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi:10.7326/0003-4819-155-2-201107190-00005
- Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(3):30–54. doi:10.1080/10810730.2011.604391
- Gaffari-Fam S, Babazadeh T, Oliaei S, Behboodi L, Daemi A. Adherence to a health literacy and healthy lifestyle with improved blood pressure control in Iran. Patient Prefer Adherence. 2020;14:499–506. doi:10.2147/PPA.S244820
- Halladay JR, Donahue KE, Cené CW, et al. The association of health literacy and blood pressure reduction in a cohort of patients with hypertension: the heart healthy lenoir trial. Patient Educ Couns. 2017;100(3):542–549. doi:10.1016/j.pec.2016.10.015
- Pahria T, Nugroho C, Yani DI. Factors influencing self-care behaviors in hypertension patients with complications. Vasc Health Risk Manag. 2022;18:463–471. doi:10.2147/VHRM.S366811
- Khazanie R. Statistics in a World of Applications. New York: Harper Collins; 1966.
- NordNordWest. Locator map of Phayao Province, Thailand. Available from: https://upload.wikimedia.org/wikipedia/commons/3/37/Thailand_Phayao_locator_map.svg. Accessed January 1, 2024.
- Division of Health Education. Department of health service support ministry of public health Thailand: health literacy assessment tools and guidelines; 2020. Available from: http://www.hed.go.th/.Accessed July 1, 2022.
- Nutbeam D. health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–267. doi:10.1093/heapro/15.3.259
- Du S, Zhou Y, Fu C, Wang Y, Du X, Xie R. Health literacy and health outcomes in hypertension: an integrative review. Int J Nurs Sci. 2018;5(3):301–309. doi:10.1016/j.ijnss.2018.06.001
- Marciano L, Camerini AL, Schulz PJ. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. J Gen Intern Med. 2019;34(6):1007–1017. doi:10.1007/s11606-019-04832-y
- Larki A, Tahmasebi R, Reisi M. Factors Predicting self-care behaviors among low health literacy hypertensive patients based on health belief model in Bushehr District, South of Iran. Int J Hypertens. 2018;2018(1):1–7. doi:10.1155/2018/9752736
- Tefera YG, Gebresillassie BM, Emiru YK, et al. Diabetic health literacy and its association with glycemic control among adult patients with type 2 diabetes mellitus attending the outpatient clinic of a university hospital in Ethiopia. PLoS One. 2020;15(4):e0231291. doi:10.1371/journal.pone.0231291
- Ong-Artborirak P, Seangpraw K, Boonyathee S, et al. Health literacy, self-efficacy, self-care behaviors, and glycemic control among older adults with type 2 diabetes mellitus: a cross-sectional study in Thai communities. BMC Geriatr. 2023;23:297. doi:10.1186/s12877-023-04010-0
- Mafu C, Seangpraw K, Ong-Artborirak P, et al. Self-care behaviors and lipid profiles among an ethnic minority adult population in Thai Rural communities. Open Public Health J. 2023;16:1–9. doi:10.2174/18749445-v16-e230403-2022-173
- Melaku T, Bayisa B, Fekeremaryam H, et al. Self-care practice among adult hypertensive patients at ambulatory clinic of tertiary teaching Hospital in Ethiopia: a cross-sectional study. J Pharm Policy Pract. 2022;15:15–23.
- RobatSarpooshi D, Mahdizadeh M, Alizadeh Siuki H, Haddadi M, Robatsarpooshi H, Peyman N. The relationship between health literacy level and self-care behaviors in patients with diabetes. Patient Relat Outcome Meas. 2020;11:129–135. doi:10.2147/PROM.S243678
- Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27(3):393–404. doi:10.1177/014572170102700309
- Irwan AM, Potempa K, Abikusno N, Syahrul S. self-care management for hypertension in southeast Asia: a scoping review. J Multidiscip Healthc. 2022;15:2015–2032. doi:10.2147/JMDH.S367638
- Ji H, Kim A, Ebinger JE, et al. Sex differences in blood pressure trajectories over the life course. JAMA Cardiol. 2020;5(3):19–26. doi:10.1001/jamacardio.2019.5306
- George KM, Maillard P, Gilsanz P, et al. Association of early adulthood hypertension and blood pressure change with late-life neuroimaging Biomarkers. JAMA Netw Open. 2023;6(4):e236431. doi:10.1001/jamanetworkopen.2023.6431
- Wan EYF, Yu EY, Chin WY, Fong DYT, Choi EPH, Lam CLK. Association of blood pressure and risk of cardiovascular and chronic kidney disease in Hong Kong hypertensive patients. Hypertension. 2019;74(10):331–340. doi:10.1161/HYPERTENSIONAHA.119.13123
- Dasgupta A. Socially embedded preferences, environmental externalities, and reproductive rights. Popul Dev Rev. 2017;43(3):405–441. doi:10.1111/padr.12090
- Tsai YC, Wang SL, Tsai HJ, et al. The interaction between self-care behavior and disease knowledge on the decline in renal function in chronic kidney disease. Sci Rep. 2021;11(1):401. doi:10.1038/s41598-020-79873-z
- Wang Y, Chen T, Gan W, et al. Association among high blood pressure health literacy, social support and health-related quality of life among a community population with hypertension: a community-based cross-sectional study in China. BMJ Open. 2022;12(6):e057495. doi:10.1136/bmjopen-2021-057495
- Schrauben SJ, Cavanaugh KL, Fagerlin A, et al. The relationship of disease-specific knowledge and health literacy with the uptake of self-care behaviors in CKD. Kidney Int Rep. 2019;5(1):48–57. doi:10.1016/j.ekir.2019.10.004