Abstract
Guidewire loss is a rare complication of central venous catheterization. A 65-year-old male was hospitalized in a high-dependency unit for exacerbation of chronic obstructive pulmonary disease, pneumonia, erythrocytosis, and clinical signs of heart failure. Upon admission, after an unsuccessful right jugular approach, a left jugular central venous catheter was placed. The next day, chest radiography revealed the catheter located in the left parasternal region, with suspected retention of the guidewire, visually confirmed by the presence of its proximal end inside the catheter. The left parasternal location of the catheter and the typical projection of the guidewire in the coronary sinus, later confirmed by echocardiography, raised suspicion of a persistent left superior vena cava (PLSVC). Agitated saline injected into the left antecubital vein confirmed bubble entry from the coronary sinus into the right atrium. After clamping the guidewire, the catheter was carefully retrieved along with the guidewire without any complications. This is the first reported case of guidewire retention in PLSVC and coronary sinus. It underscores the potential causes of guidewire loss and advocates preventive measures to avoid this potentially fatal complication.
Introduction
Placement of a central venous catheter (CVC) is a common procedure in the intensive care unit (ICU) that is required for the administration of fluids, medications, parenteral nutrition, central venous pressure monitoring, and blood sampling. The Seldinger technique, introduced in 1953, simplifies catheter placement over the guidewire.Citation1 Controlling the proximal end of the guidewire is a fundamental step before CVC advancement over the guidewire. Possible complications related to the guidewire include kinking, intravascular looping, rupture with wire embolisation, and rarely guidewire loss.Citation2 Retention of the guidewire can cause dysrhythmia, vascular damage, thrombosis, embolism, and cardiac perforation with tamponade and death.Citation3 Although this complication is generally recognised intraoperatively, it can be discovered up to several months after the procedure.Citation4 In this paper, the authors present the first reported case of unrecognized loss of guidewire in the right atrium through the persistent left superior vena cava (PLSVC) and coronary sinus. The guidewire was clamped to the catheter and cautiously retrieved without any complications.
Case Presentation
A 65-year-old man with a history of chronic obstructive pulmonary disease (COPD) was admitted to a high-dependency unit (HDU) because of respiratory insufficiency. Analyses of arterial blood gases revealed hypercapnic respiratory insufficiency and respiratory acidosis. Biochemistry showed increased NT-proBNP levels in the context of heart failure, a complete blood count showed a COPD-related elevation in hemoglobin and hematocrit levels, and coagulation parameters were abnormal due to secondary liver failure. A focused ultrasound examination revealed a right-sided pleural effusion with possible right lung consolidation and bilaterally visible B-lines, suggestive of heart failure. Echocardiography demonstrated normal systolic function with grade II diastolic dysfunction of the left ventricle, pulmonary hypertension, and mildly reduced right ventricular systolic function (TAPSE 13 mm).
The patient’s exacerbation of COPD with pneumonia was treated with noninvasive ventilation and conventional medical therapy (bronchodilators, corticosteroids, and antibiotics). Heart failure volume overload was treated cautiously with low-dose diuretic therapy to prevent further increase in hematocrit level. Pleurocentesis was required due to a right-sided pleural effusion with respiratory insufficiency, and 1400 mL of pleural fluid was evacuated. Right heart failure and pulmonary hypertension were greatly aggravated by polycythemia; therefore, therapeutic phlebotomy was indicated. Central venous catheterization was planned because of the limited peripheral venous access. After an unsuccessful attempt to access the right jugular vein, a left jugular CVC (triple lumen, 7 Fr, 20 cm; Biometrix) was successfully placed using the landmark technique by an internal medicine specialist with prior experience. The procedure was performed without complications, although the operator was distracted by another emergency in the ward. The nurse noticed a slow flow from the distal lumen during the initial 400 mL of therapeutic phlebotomy, which was reported to the operator, but no further action was taken.
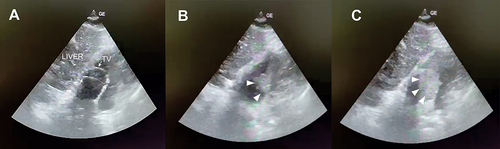
Twenty hours after CVC placement, chest radiography confirmed the presence of right-sided bronchopneumonia. The radiologist described the left parasternal location of the CVC and suspected a retained guidewire with an end-loop in the right atrium (). Visual inspection of the CVC revealed that the proximal end of the guidewire was in the distal lumen, which was immediately clamped to prevent further displacement. Due to the left parasternal location of the catheter with a typical guidewire position in the coronary sinus, PLSVC was suspected. Echocardiography revealed a dilated coronary sinus (17 mm) with a hyperechoic linear echo of the guidewire (). PLSVC was diagnosed by agitated saline injection (bubble test) through the left antebrachial vein with visual confirmation of bubble entrance from the coronary sinus ostium on the interatrial septum (). The CVC with the clamped guidewire was slowly removed from the patient without any complications.
Figure 1 Chest radiograph showing the left parasternal location of the central venous catheter (CVC) with a guidewire retained in the right atrium through the PLSVC and the coronary sinus (brightness and contrast changed for better visualisation of the guidewire).
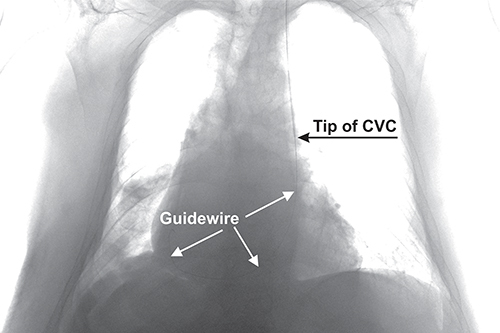
Figure 2 Transthoracic echocardiography (“shortened“ apical 4-chamber view in supine) shows a visibly dilated coronary sinus (CS) with the guidewire inside.
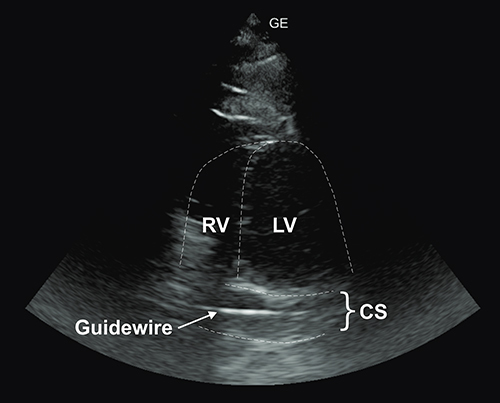
Figure 3 Focused echocardiography of the right atrium during a bubble test (subcostal 4-chamber view). (A) Focus on the right atrium with visualization of the terminal part of the guidewire (arrow). The dotted line indicates the out-of-plane part of the guidewire leading toward the ostium of the coronary sinus on the interatrial septum (asterisk) prior to the agitated saline injection; (B) Visual confirmation of early bubble entrance into the right atrium (arrowheads); (C) Late phase of bubble entry into the right atrium (arrowheads).
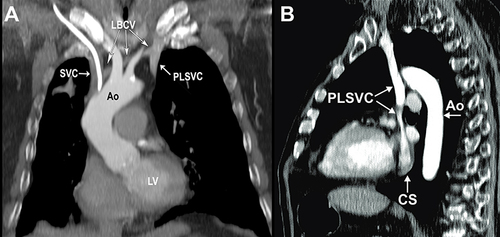
The patient was transferred to the general ICU for mechanical ventilation on the fourth day of hospitalisation after experiencing respiratory distress. Contrast-enhanced computed tomography of the thorax was performed during hospitalization in the ICU after consulting with the pulmonologist, that confirmed PLSVC with drainage to the coronary sinus with a small-diameter left brachiocephalic vein connecting the PLSVC and the right superior vena cava (SVC) (). The patient was extubated on the fifth day of hospitalisation and was transferred to the pulmonology ward with respiratory and cardiac stabilisation and improvement in laboratory results.
Figure 4 Contrast-enhanced computed tomography of the thorax. (A) Coronal view shows the proximal part of the PLSVC with a minor LBCV connecting to the SVC (note the central vein catheter within the SVC): (B) Sagittal view shows the inflow of the PLSVC into the coronary sinus.
Discussion
The Seldinger technique is commonly used for CVC placement. Following venipuncture, a metal guidewire is introduced through the needle and a catheter is railed into the vein over the guidewire. Complications associated with CVC are dependent on operator experience and technique used (landmark vs. ultrasound-guided) with a prevalence of 0.3–3% and include pneumothorax, arterial puncture and laceration, hematoma, hemothorax, nerve injury, air embolism, infection, and thrombosis.Citation5 Although protocols like RaCeVa (Rapid Central Vein Assessment) and SIC (Safe Insertion of Centrally Inserted Central Catheters) have been proposed to enhance the efficacy and safety of central vein catheterization, guidewire loss remains a significant issue that has not been mitigated by the implementation of these new protocols.Citation3,Citation6,Citation7
Guidewire loss is a very rare complication of central venous catheterization (CVC), typically considered a “never event”, but it still occurs at a frequency of 0.05%.Citation3 Complete loss of the guidewire is usually asymptomatic, as observed in this case, but can lead to fatal complications, such as cardiac tamponade, blood vessel perforation, and dysrhythmia.Citation8 The retained guidewire is usually detected during a procedure, but there have been cases where a diagnosis was discovered incidentally several months later during routine radiology diagnostics.Citation9 Possible signs that guide the recognition of guidewire retention include slow backflow from the distal tip or resistance to injection, a missing guidewire after the procedure, or radiological suspicion during radiology diagnostics.Citation10,Citation11 Although a nurse in this case alerted the operator of slow backflow, the operator was not aware of the potential sign of guidewire retention.
In scenarios of guidewire loss using the left jugular or subclavian approach in the presence of PLSVC, the guidewire may migrate toward the coronary sinus and the right atrium. PLSVC is the most common thoracic venous anomaly, with a prevalence of 0.5–2% in the general population and up to 10% in patients with congenital heart disease.Citation12 Typically, PLSVC is usually found as an accessory left SVC connected to the right SVC via the left brachiocephalic vein, but in a minority of cases, it presents as an isolated left SVC. In almost 90% of patients, PLSVC is drained into the right atrium without any hemodynamic significance; however, in 8–10% of cases, it can be drained into the left atrium directly or through the pulmonary vein, leading to a considerable right-to-left shunt and potential paradoxical embolization, including air or thromboemboli, especially during peripheral or central venous cannulation or drug therapy administration.Citation13
Guidewire loss in coronary sinus or CVC placement in PLSVC can result in severe complications such as arrhythmia, angina, cardiogenic shock, and cardiac arrest. Despite these risks, PLSVC does not hinder the successful implantation of a pacemaker, ICD, or CRT leads.Citation14,Citation15 Moreover, there are numerous documented reports of successful and uneventful dialysis procedures, as well as numerous chemotherapy administration protocols using CVC inside PLSVC.Citation16,Citation17 However, it is our perspective that if PLSVC has been previously diagnosed, it should only be considered as an alternative vascular access when other sites have failed. In such cases, preprocedural diagnostic evaluation (MSCT venography) must be performed to exclude left atrial drainage to prevent systemic embolism and ensure the presence of the right SVC to prevent SVC syndrome in the event of isolated PLSVC thrombosis. Preprocedural signs that may raise concern for a PLSVC include a dilated left external jugular vein or a dilated coronary sinus observed on echocardiography. These findings should be confirmed with a bubble test using agitated saline injected into the left cubital vein.Citation18
Recognising and removing the retained guidewire as soon as possible is essential. Long-term retention of the guidewire (several years) may cause vascular injury during the removal of the guidewire due to its neointimalization.Citation19 In the case of partial guidewire loss, as presented in this case, where the guidewire is accessible for clamping, it is recommended to clamp a guidewire and retrieve it with a catheter. In the scenario of complete loss of the guidewire, the endovascular approach using a vascular snare under radiographic control is the method of choice.Citation20 The endovascular approach has a high success rate (90%), and the surgical approach is reserved in cases of percutaneous failure or inaccessibility of this method.Citation21
Prior studies have identified numerous factors that contribute to guidewire retention. These include patient-related factors (such as obesity, coagulopathy, and non-cooperation), operator-related factors (including inattention, lack of experience, inadequate supervision, fatigue, distractions, and work interruptions), and procedural circumstances (such as urgency, lack of ultrasound guidance, and poor guidewire design). Despite improvements in institutional security protocols and standards, the use of anesthesia in uncooperative patients, and the implementation of ultrasound guidance, guidewire retention still occurs in the healthcare system.Citation3 Contrary to previous reports, the observational study by Kassis et al on 24 guidewire retention incidents found that most cases occurred in non-obese, non-coagulopathic patients during regular shift hours, in the jugular vein position, using ultrasound by attending physicians with preprocedural sedation in non-emergent settings. This suggests that despite improved security protocols and technological advancements in CVC placement, such as the use of ultrasound, human error remains a significant factor. In an observational study of 73 guidewire retention incidents, human factors were identified as the cause in 34.4% of cases. These factors included inadequate training, lack of experience, insufficient supervision, failure to visually assess the guidewire after the procedure, operator distraction or urgency, lack of situational awareness, and failure to recognize foreign objects on postprocedural chest X-rays.Citation22 We believe that operator distraction during the procedure, as was present in our scenario, is an important risk factor that significantly impacts situational awareness. At last, postprocedural chest X-ray serves as the last safety measure for detecting unintentional guidewire retention and should be mandatory as suggested by the American Society of Anesthesiologists Task Force.Citation21 It is also essential to communicate with the radiologist after ordering a diagnostic procedure to ensure that, in addition to ruling out pneumothorax and localizing the catheter tip, guidewire retention is also excluded. In this scenario, after operator interrogation, post-procedural chest radiography was omitted due to his presumption that the left jugular approach carried a negligible risk of iatrogenic pneumothorax, overlooking the possibility of catheter malposition, congenital venous anomaly as later diagnosed, or guidewire retention. We believe that using an ultrasound-guided technique during the initial right jugular approach could increase the likelihood of successful central venous catheter (CVC) placement, thereby preventing the inadvertent placement of a CVC in PLSVC during a subsequent left jugular attempt.
In light of the aforementioned safety concerns, we recommend several steps to prevent guidewire loss. First, recognizing guidewire loss as a potential complication increases situational awareness. Training and education should emphasize the importance of controlling the proximal end of the guidewire and preventing excessive advancement. Having another person monitor the procedure is beneficial, especially in case of distractions due to emergencies. Implementing a checklist and requiring visual confirmation of guidewire removal by two individuals are mandatory practices. A postprocedural chest X-ray is essential to exclude pneumothorax, verify the tip location, and detect any foreign objects, such as a guidewire. Promoting a safety culture and minimizing potential distractions are crucial for the safe performance of CVC procedures.
Conclusion
Guidewire loss is a rare but preventable complication of CVC procedures. Rapid recognition and removal are essential to reduce potentially lethal complications. Promoting a safety culture, including continuous guidewire control, active surveillance by another team member, visual confirmation of guidewire removal, the use of checklists, and mandatory postprocedural chest X-rays, can reduce the incidence of this complication. Additionally, using ultrasound and favoring the right-sided approach (jugular and subclavian) can prevent the potential cannulation of PLSVC in the presence of this venous anomaly.
Consent for Publication
Informed consent for the publication of the details and images included in this manuscript was obtained from the patient whose clinical case is described in this report. In accordance with institutional policy, obtaining approval for publication was deemed unnecessary.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
The authors are most grateful to Ante Mandić and Edin Begić for their assistance with text proofreading and editorial suggestions.
Additional information
Funding
References
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography: a new technique. Acta Radiol. 1953;39(5):368–376. doi:10.3109/00016925309136722
- Sarkar PK, Mubarak K. A lost guidewire. Indian J Crit Care Med. 2014;18(7):481–482. doi:10.4103/0972-5229.136085
- Kassis N, Alkukhun L, Kravitz K, et al. Patient, operator, and procedural characteristics of guidewire retention as a complication of vascular catheter insertion. Crit Care Explor. 2023;5(1):e0834. doi:10.1097/cce.0000000000000834
- Auweiler M, Kampe S, Zähringer M, et al. The human error: delayed diagnosis of intravascular loss of guidewires for central venous catheterization. J Clin Anesth. 2005;17(7):562–564. doi:10.1016/j.jclinane.2004.11.007
- Teja B, Bosch NA, Diep C, et al. Complication rates of central venous catheters: a systematic review and meta-analysis. JAMA Intern Med. 2024;184(5):474–482. doi:10.1001/jamainternmed.2023.8232
- Brescia F, Pittiruti M, Ostroff M, Spencer TR, Dawson RB. The SIC protocol: a seven-step strategy to minimize complications potentially related to the insertion of centrally inserted central catheters. J Vasc Access. 2023;24(2):185–190. doi:10.1177/11297298211036002
- Spencer TR, Pittiruti M. Rapid Central Vein Assessment (RaCeVA): a systematic, standardized approach for ultrasound assessment before central venous catheterization. J Vasc Access. 2019;20(3):239–249. doi:10.1177/1129729818804718
- Khasawneh FA, Smalligan RD. Guidewire-related complications during central venous catheter placement: a case report and review of the literature. Case Rep Critical Care. 2011;2011.
- Osailan A, De Queiroz Siqueira M, Bouvet L, Chassard D. Lost venous access guidewire identified by its late cervical protrusion: case report. A a Pract. 2022;16(2):e01565. doi:10.1213/xaa.0000000000001565
- Amit A, Jyotsna S, Kumar Kasyap V. Retention of guidewire: a rare but avoidable complication of central venous catheterization. case report. journal of Comprehensive Pediatrics. 2016;7(1):e33238. doi:10.17795/compreped-33238
- Shih AF, Sankey C. Incidental discovery of retained triple lumen catheter guidewire. J Gen Intern Med. 2017;32(3):361–362. doi:10.1007/s11606-016-3798-8
- Edwards J. Thoracic venous anomalies. Arch Pathol. 1950;49:514–537.
- Azizova A, Onder O, Arslan S, Ardali S, Hazirolan T. Persistent left superior vena cava: clinical importance and differential diagnoses. Insights Imaging. 2020;11(1):110. doi:10.1186/s13244-020-00906-2
- Adavidoaei CG, Haba AM, Costache II, et al. Cardiac implantable electronic devices in different anatomical types of persistent left superior vena cava: case series and brief review of the literature. Diagnostics. 2022;12(11):2596.
- Ghazzal B, Sabayon D, Kiani S, et al. Cardiac implantable electronic devices in patients with persistent left superior vena cava-A single center experience. J Cardiovasc Electrophysiol. 2020;31(5):1175–1181. doi:10.1111/jce.14460
- Wang X, Yang Y. Analysis of six cancer patients with persistent left superior vena cava identified during central venous access device placement via an intracavitary electrocardiogram. J Vasc Access. 2021;11297298211045576. doi:10.1177/11297298211045576
- Piedade A, Domingues P, Natário A, Barreto C, Parreira L. Persistent left superior vena cava: rare location of hemodialysis catheter. Cureus. 2023;15(2):e35579. doi:10.7759/cureus.35579
- Mandolfo S, Maggio M, Bucci R, et al. Contrast echocardiographic and persistent left superior vena cava. J Vasc Access. 2017;18(3):e30. doi:10.5301/jva.5000633
- Van Doninck J, Maleux G, Coppens S, Moke L. Case report of a guide wire loss and migration after central venous access. J Clin Anesth. 2015;27(5):406–410. doi:10.1016/j.jclinane.2015.04.005
- Egglin TK, Dickey KW, Rosenblatt M, Pollak JS. Retrieval of intravascular foreign bodies: experience in 32 cases. AJR. 1995;164(5):1259–1264. doi:10.2214/ajr.164.5.7717243
- Apfelbaum JL, Rupp SM, Tung A, et al. Practice guidelines for central venous access 2020: an updated report by the American society of anesthesiologists task force on central venous access. Anesthesiology. 2020;132(1):8–43. doi:10.1097/aln.0000000000002864
- Steelman VM, Thenuwara K, Shaw C, Shine L. Unintentionally retained guidewires: a descriptive study of 73 sentinel events. Jt Comm J Qual Patient Saf. 2019;45(2):81–90. doi:10.1016/j.jcjq.2018.08.003
