Abstract
Background
Anxiety and depression by affecting lifestyle interfere with preventive actions aimed at eliminating or reducing modifiable risk factors for cardiovascular diseases (CVD).
Purpose
The objective of the study was to assess the impact of anxiety and depression on the achievement of therapeutic goals regarding CVD risk factors in patients without a history of atherosclerotic CVD.
Patients and Methods
The study included 200 patients (median age 52.0 [IQR 43.0–60.5] years). Control of the basic risk factors was assessed: blood pressure, BMI, waist circumference, physical activity, smoking status, LDL cholesterol, triglycerides, and blood glucose. The data analysis included a comparison of the number of controlled risk factors and the percentage of subjects who achieved the therapeutic goal for each of the cardiovascular risk factors. The risk of CVD was assessed with SCORE2 and SCORE2-OP. Anxiety and depression were assessed using the Hospital Anxiety and Depression Scale (HADS). On both subscales (HADS Anxiety and HADS Depression), subjects could achieve normal, borderline, and abnormal scores.
Results
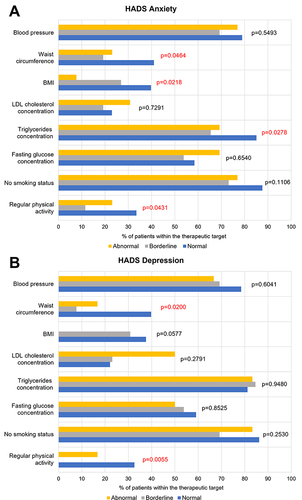
The median number of controlled CVD risk factors was 4.0 (IQR 3.0–5.0), and the median CVD risk assessed with SCORE2 and SCORE2-OP was 3.0% (IQR 1.5–7.0%). Median scores for HADS Anxiety were 3.0 (IQR 2.0–6.0) and for HADS Depression 3.0 (1.0–5.0). Patients with symptoms of anxiety and depression had significantly fewer controlled risk factors (HADS Anxiety p=0.0014; HADS Depression p=0.0304). Among subjects with anxiety and depression, there was a significantly lower percentage of those with a normal waist circumference (HADS Anxiety p=0.0464; HADS Depression p=0.0200) and regular physical activity (HADS Anxiety p=0.0431; HADS Depression p=0.0055). Among subjects with anxiety, there was a significantly lower percentage of those with a normal BMI (p=0.0218) and normal triglyceride concentrations (p=0.0278).
Conclusion
The presence of anxiety and depression may affect the control of CVD risk factors in individuals without a history of atherosclerotic CVD. Assessment of anxiety and depression symptoms should be part of a comprehensive examination of patients with high CVD risk.
Introduction
The classic risk factors for cardiovascular disease (CVD) are mainly related to lifestyle. New research suggests that psychological factors, especially anxiety and depression, are also risk factors for CVD.Citation1–3 Anxiety and depression are among the major mental health disorders in the general population.Citation4,Citation5 Depression is associated with a poorer prognosis and increased healthcare costs in patients with CVD. On average, one in five patients with coronary artery disease or heart failure suffers from depression, and the incidence of depression is at least three times higher than in the general population.Citation6–8
Health behaviors that are risk factors for CVD, including a sedentary lifestyle, inappropriate eating habits, nicotinism, and increased alcohol consumption are common in people with symptoms of anxiety and depression.Citation9 Depression may reduce the motivation and engagement of patients to undertake health-promoting behaviors and take their medication while increasing the likelihood of unhealthy behaviors.Citation10–13 The European Society of Cardiology (ESC) guidelines on CVD prevention pay particular attention to the anxiety and depression in the context of primary prevention.Citation14 The implementation of these recommendations allows for early mental health interventions as part of the comprehensive management of CVD risk factors in the early stages preceding cardiovascular events.Citation5,Citation15–20 In line with these recommendations, we designed a cross-sectional study aimed at assessing the relationship between the occurrence of anxiety and depression symptoms and the fulfillment of therapeutic goals regarding basic cardiovascular risk factors in the group of primary care patients without a history of atherosclerotic cardiovascular disease (ASCVD).
Materials and Methods
This study is part of a broader cross-sectional research project on CVD risk factors in the Polish population characterized by high risk of CVD.Citation20–22
Characteristics of the Study Group and Organization of the Study
The study included 200 patients without symptomatic ASCVD, aged 18 to 80 years (median age 52.0 [IQR 43.0–60.5] years) who had been diagnosed 6 to 24 months before study enrolment with at least one of the following conditions: hypertension (ICD10: I10), diabetes (ICD10: E11), or hypercholesterolemia (ICD10: E78), defined according to the ESC guidelines.Citation23–25 Specific inclusion criteria encompassed the inclusion of subjects who began pharmacological treatment for hypertension and/or lipid disorders and/or type 2 diabetes within 6 to 24 months. Exclusion criteria included treatment for any other chronic disease, lack of patient consent, or impossibility of giving informed consent. In patients with diabetes (n=38) CV risk assessment was not performed due to the lack of complete data required for assessment with the use of SCORE2-Diabetes, an algorithm specifically dedicated to this group.Citation26 The characteristics of the study group are presented in .
Table 1 Characteristics of the Study Group
The first stage of patient recruitment involved the analysis of medical digital records in four primary care facilitiesCitation27,Citation28 in three cities between spring 2018 and autumn 2019. Patients meeting the inclusion criteria were identified. The next stage of the study was to invite patients for an individual visit at the study site. Each of the study participants gave their informed consent to participate in the study, in accordance with the principles of Good Clinical Practice and the requirements of the Declaration of Helsinki. The study was approved by the Ethics Committee of Nicolaus Copernicus University in Toruń, Collegium Medicum in Bydgoszcz (study approval reference number KB 586/2017).
The study visit included: measurement of arterial blood pressure, assessment of body mass index (BMI), waist circumference, physical activity history, smoking status, blood sampling for total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), and fasting plasma glucose, as well as anxiety and depression symptom assessment with the use of Hospital Anxiety and Depression Scale (HADS).
Each patient had their arterial blood pressure measured twice in a semi-sitting position using semi-automatic sphygmomanometers. Classification and diagnosis of arterial hypertension were based on the current criteria of the European Society of Cardiology.Citation29
The history of smoking status was verified by assessing the concentration of carbon monoxide in exhaled air with Bedfont Scientific Micro+ Smokerlyzer monitor. A result of >10 ppm was considered indicative of active smoking.
Biochemical blood tests included in the study protocol were performed on fasting venous blood using the Alinity ci-series analyzer (Abbott, Wiesbaden, Germany).
Physical activity was assessed based on patients’ declarations using the question: “Which of the following terms best describes your non-professional activity?” with 4 possible answers: [1] “I do not engage in any physical activity other than professional work”; [2] “Most of the time only light physical activity”; [3] “Intense physical activity at least 20 minutes 1–2 times a week”; [4] “20 minutes of intense physical activity more often than twice a week”. Responses 3 and 4 were considered to be the appropriate level of physical activity.
The following criteria were adopted for risk factor control (the risk factor defined as controlled):
Systolic blood pressure <140 mmHg and diastolic blood pressure <90 mmHg;
BMI 20.0–24.9 kg/m2; however, patients with BMI <20.0 kg/m2 were not included in the analysis of uncontrolled risk factors with regards to BMI (11 patients);
Waist circumference <80 cm for women and <94 cm for men;
Regular physical activity - intense physical activity for 20 minutes or more at least 1–2 times a week;
No smoking status - The declared status of a non-smoker was objectively confirmed by a concentration of carbon monoxide in exhaled air ≤10 ppm;
LDL-C <100 mg/dl (<2.6 mmol/l);
TG <150 mg/dl (<1.7 mmol/l);
Fasting glucose: <100 mg/dl (<5.6 mmol/l).
The number of controlled risk factors, as well as the percentage of subjects whose CVD risk factors were within the therapeutic target range were assessed.
CVD risk was assessed for all patients using Systematic Coronary Risk Evaluation 2 (SCORE2) and Systematic Coronary Risk Evaluation 2 - Older Persons (SCORE2-OP) algorithms, according to the guidelines of the European Society of Cardiology.Citation30,Citation31 The risk assessment was adjusted for Poland as a high-risk country based on the SCORE2 and SCORE2-OP risk regions.Citation30,Citation31 Cardiovascular risk was expressed as a percentage and then defined as low or moderate, high, and very high based on ESC guidelines.
Symptoms of anxiety and depression were assessed using the Hospital Anxiety and Depression Scale (HADS). The HADS is a standardized and validated tool commonly used to assess symptoms of anxiety and depression.Citation32,Citation33 It consists of 14 questions, with 7 questions assessing symptoms of anxiety (HADS Anxiety) and 7 questions assessing symptoms of depression (HADS Depression). On each of the subscales, the subject can score from 0 to 21 points, with a higher score indicating stronger symptoms of anxiety and depression. For each of the subscales, three score ranges were set to define a normal score (≤7 points), a borderline score indicating moderate symptoms (8 to 10 points), and an abnormal score indicating significant symptoms of anxiety and depression (≥11 points).Citation34
Statistical Analysis
The statistical analysis was carried out using the Statistica 13.0 package (TIBCO Software Inc, California, USA). Continuous variables were presented as means with standard deviations and/or medians with interquartile range. The Shapiro–Wilk test demonstrated a non-normal distribution of the investigated continuous variables. Therefore non-parametric Kruskal–Wallis one-way analysis of variance was used for comparisons between groups. Categorical variables were expressed as the number and the percentage and were compared using the χ2 test. Results were considered significant at p<0.05.
Results
The median number of controlled CVD risk factors was 4.0 (IQR 3.0–5.0), and the median CVD risk assessed with SCORE2 and SCORE2-OP was 3.0% (IQR 1.5–7.0%). Median scores indicating symptoms of anxiety and depression as measured by HADS were 3.0 (IQR 2.0–6.0) for HADS Anxiety and 3.0 (1.0–5.0) for HADS Depression.
The Results of the HADS Anxiety subscale were not observed to differentiate the results in terms of studied parameters (). On the other hand, subjects with an abnormal score in HADS Depression subscale were significantly older (p=0.0450) and had significantly larger waist circumference (p=0.0105), body weight (p=0.0381), and BMI (p=0.0328) ().
Table 2 Comparison of the Studied Parameters Depending on the Level of the HADS Anxiety Subscale Scores
Table 3 Comparison of the Studied Parameters Depending on the Level of the HADS Depression Subscale Scores
The highest risk of CVD assessed with the use of SCORE2 and SCORE2-OP was found in subjects with symptoms of anxiety and depression at a borderline level for both HADS Anxiety (p=0.0072) and HADS Depression (p=0.0177). In turn, patients with symptoms of anxiety and depression (borderline and abnormal levels) in both HADS subscales (HADS Anxiety p=0.0014; HADS Depression p=0.0304) had significantly fewer controlled risk factors ().
Table 4 Total CVD Risk Assessed with the SCORE2 and SCORE2-OP Algorithms and the Number of Adequality Controlled CV Risk Factors According to the Level of Anxiety and Depression Symptoms by the HADS Scale
Analyzing the percentages of subjects achieving control of individual risk factors, it was found that among subjects with symptoms of anxiety and depression, there was a significantly lower percentage of those with a normal waist circumference (HADS Anxiety p=0.0464; HADS Depression p=0.0200) and regular physical activity (HADS Anxiety p=0.0431; HADS Depression p=0.0055). In addition, among subjects with anxiety, there was a significantly lower percentage of those with a normal BMI (p=0.0218) and normal triglyceride concentrations (p=0.0278) ().
Discussion
Depression is one of the best-documented psychosocial factors of poorer prognosis and reduced quality of life of patients with CVD.Citation10,Citation35 The assessment of psychosocial status is considered a necessary element to be observed during the overall diagnosis of the patient.Citation14,Citation22,Citation36 Conditions associated with depression such as disengagement, social isolation, lack of emotional support, and concomitance of fear and anxiety associated with the onset of the disease contribute to neglect in all aspects of life, including a decrease or loss of interest in previously enjoyable activities.Citation37–40 The American Heart Association highlights the impact of mental health and well-being on the occurrence and prognosis of patients with CVD. Attention is drawn to the link between chronic stress, anger, anxiety, depression, pessimism, and an increased risk of CVD.Citation41 Depression itself is associated with increased mortality after MI.Citation42 In one meta-analysis, depression was shown to be associated with both cardiovascular and all-cause mortality in patients after myocardial infarction.Citation43 Similar results were also obtained in a meta-analysis focusing on patients with coronary artery disease.Citation43
To the best of our knowledge, the presented assessment of the relationship between the severity of depression and anxiety symptoms and the risk of CVD is the first such study in individuals without symptomatic ASCVD.
Particularly noteworthy is the greater severity of anxiety and depression symptoms going together with poorer control of risk factors. This appears to be supported by reports by some authors suggesting that anxiety and depression may be associated with a lower quality of life and less commitment towards the care for health.Citation10,Citation35,Citation38–40 Depression may decrease the motivation and engagement of cardiac patients to undertake health-promoting behaviors such as caring for diet, physical activity, and taking medicationCitation11 and at the same time increase the likelihood of unhealthy behaviors.Citation10 It is worth noting that a higher risk of CVD as measured by SCORE2 and SCORE2-OP was found in subjects with symptoms of anxiety and depression in both HADS subscales. In turn, patients with symptoms of anxiety and depression had significantly fewer effectively controlled risk factors.
In addition, more severe symptoms of depression in people of older age, with larger waist circumference, body weight, and BMI strongly suggest a causal relationship between these risk factors in individuals without clinically evident ASCVD. Such a two-way relationship with respect to modifiable risk factors was previously observed in people with confirmed CVD.Citation44–46 For many years now, we have seen the aging of the population and an increase in the incidence of chronic diseases, including cardiovascular diseases and mental disorders. Geriatric patients with diagnosed depressive disorders have a higher risk of CVD, and at the same time, CVD may be associated with a higher risk of depression.Citation44–46 Our results complement these observations in the group of people without clinically evident ASCVD.
Clinically important is the frequent co-occurrence of classic CVD risk factors with obesity.Citation47–50 In addition, in our analysis, people with higher severity of anxiety and depression were less likely to achieve the therapeutic goal regarding physical activity. As Sin et alCitation51 show, depression and anxiety are associated with lower adherence to pharmacotherapy and difficulties in maintaining healthy behaviors and self-control. Dietary care and the resulting opportunities to reduce eg lipid levels (including triglycerides shown to be statistically significant in our analysis) are one of the basic components of adherence assessment, apart from the assessment of completeness of pharmacotherapy, physical activity, and self-control.Citation52–54
The INTERHEART and INTERSTROKE studies have shown that 9 and 10 risk factors, respectively, account for more than 90% of the incidence of heart attack and stroke. Effective control of these risk factors (lowering blood pressure and glucose levels to correct values, implementation of lipid-lowering therapy) has been demonstrated to reduce subsequent morbidity and mortality.Citation55 Identification of risk factors and actions to achieve therapeutic goals in primary prevention are key to reducing the incidence of CVD. It appears that the assessment of anxiety and depression symptoms should complement a comprehensive risk assessment also in people without clinically evident CVD.
Given the practical implications of our study, to help people at increased risk of CVD, we suggest a comprehensive approach involving psychological and health interventions. Behavioral therapy, psychological support, and programs promoting a healthy lifestyle can improve risk factor control.Citation5–7 Health education, altering eating habits, and increasing physical activity are key elements to improving health.Citation9,Citation12–14,Citation24
Limitations of the study include a relatively small number of included patients and a lack of long-term follow-up. An important limitation of the study is also the adopted imprecise definitions of physical activity. Another limitation of the study is the wide age range of participants. The influence of age on the incidence of CVD risk factors is obvious. Older patients tend to have a higher risk of CVD and a higher incidence of depression and anxiety symptoms. In elderly people, depression and anxiety often co-exist with other chronic diseases, making it more difficult to control CVD risk factors.Citation1,Citation3,Citation8 Younger people, on the other hand, may experience other stressors, such as work and social pressure, which also affect mental and physical health.Citation2,Citation4
The lack of complete data to perform the SCORE2-Diabetes algorithm in diabetic patients is another limitation of the study. One of the limitations of this study is the absence of instrumental screening for asymptomatic CVD. Therefore our patients, even if asymptomatic, could present atherosclerotic lesions.Citation56 However, it should be noted that the objective of the study was not to diagnose atherosclerotic disease in patients without CVD symptoms.
Conclusion
The presence of anxiety and depression may affect the achievement of therapeutic goals in terms of controlling the basic CVD risk factors in individuals without a history of atherosclerotic CVD. Therefore, assessment of anxiety and depression symptoms should be part of a comprehensive examination not only of patients with CVD but also those with high CVD risk.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors express their gratitude to the medical facilities: Nasz Rodzinny sp. Z o.o. in Bydgoszcz, NZOZ Salus in Bydgoszcz, Provincial Polyclinical Hospital with Outpatient Clinics in Toruń, and MEJAMED Family Physician Clinic in Łódź for their help in recruiting patients for the study. Part of this paper and abstract of this paper was presented at the Association of Cardiovascular Nursing and Allied Professions (ACNAP) 2023 Congress name ‘Relationship of the occurrence of self-reported anxiety and depression symptoms and achievement of cardiovascular risk factors controlas’ a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in European Journal of Cardiovascular Nursing name ‘Relationship of the occurrence of self-reported anxiety and depression symptoms and achievement of cardiovascular risk factors control’: https://doi.org/10.1093/eurjcn/zvad064.021.
References
- Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. AJHYPE. 2015;28(11):1295–1302. doi:10.1093/ajh/hpv047
- Walli-Attaei M, Rosengren A, Rangarajan S, et al. Metabolic, behavioural, and psychosocial risk factors and cardiovascular disease in women compared with men in 21 high-income, middle-income, and low-income countries: an analysis of the PURE study. Lancet. 2022;400(10355):811–821. doi:10.1016/S0140-6736(22)01441-6
- Silverman AL, Herzog AA, Silverman DI. Hearts and minds: stress, anxiety, and depression: unsung risk factors for cardiovascular disease. Cardio Rev. 2019;27(4):202–207. doi:10.1097/CRD.0000000000000228
- Javaid SF, Hashim IJ, Hashim MJ, Stip E, Samad MA, Ahbabi AA. Epidemiology of anxiety disorders: global burden and sociodemographic associations. Middle East Curr Psyc. 2023;30(1):44. doi:10.1186/s43045-023-00315-3
- Herrman H, Kieling C, McGorry P, Horton R, Sargent J, Patel V. Reducing the global burden of depression: a Lancet–World Psychiatric Association Commission. Lancet. 2019;393(10189):e42–e43. doi:10.1016/S0140-6736(18)32408-5
- Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. The prevalence and persistence of depression and anxiety following myocardial infarction. British J Health Psycho. 2002;7(1):11–21. doi:10.1348/135910702169321
- Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the heart and soul study. JAMA. 2003;290(2):215. doi:10.1001/jama.290.2.215
- Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in Heart Failure. J American Coll Cardio. 2006;48(8):1527–1537. doi:10.1016/j.jacc.2006.06.055
- Velten J, Lavallee KL, Scholten S, et al. Lifestyle choices and mental health: a representative population survey. BMC Psychol. 2014;2(1):58. doi:10.1186/s40359-014-0055-y
- Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large scale meta analysis of 3211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16(2):163–180. doi:10.1002/wps.20420
- Holvast F, Wouters H, Hek K, et al. Non-adherence to cardiovascular drugs in older patients with depression: a population-based cohort study. Int J Cardiol. 2019;274:366–371. doi:10.1016/j.ijcard.2018.08.100
- Bremner J, Moazzami K, Wittbrodt M, et al. Diet, stress and mental health. Nutrients. 2020;12(8):2428. doi:10.3390/nu12082428
- Ljungberg T, Bondza E, Lethin C. Evidence of the importance of dietary habits regarding depressive symptoms and depression. IJERPH. 2020;17(5):1616. doi:10.3390/ijerph17051616
- Visseren FLJ, Mach F, Smulders YM, et al. ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–3337. doi:10.1093/eurheartj/ehab484
- Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365–1372. doi:10.1093/eurheartj/eht462
- Harshfield EL, Pennells L, Schwartz JE, et al. Association between depressive symptoms and incident cardiovascular diseases. JAMA. 2020;324(23):2396. doi:10.1001/jama.2020.23068
- Balog P, Falger PRJ, Szabó G, Rafael B, Székely A, Konkolÿ Thege B. Are vital exhaustion and depression independent risk factors for cardiovascular disease morbidity? Health Psychol. 2017;36(8):740–748. doi:10.1037/hea0000495
- Michas G, Karvelas G, Trikas A. Cardiovascular disease in Greece; the latest evidence on risk factors. Hellenic J Cardio. 2019;60(5):271–275. doi:10.1016/j.hjc.2018.09.006
- Seldenrijk A, Vogelzangs N, Batelaan NM, Wieman I, van Schaik DJF, Penninx BJWH. Depression, anxiety and 6-year risk of cardiovascular disease. J Psychosom Res. 2015;78(2):123–129. doi:10.1016/j.jpsychores.2014.10.007
- Kubica A, Michalski P, Kasprzak M, et al. Two different approaches to assess adherence to medication in Polish cohort of the EUROASPIRE V registry. Med Res J. 2022;7(2):108–113. doi:10.5603/MRJ.a2022.0015
- Ratajczak J, Kubica A, Michalski P, et al. Determinants of lipid parameters in patients without diagnosed cardiovascular disease—results of the polish arm of the EUROASPIRE V survey. JCM. 2023;12(7):2738. doi:10.3390/jcm12072738
- Kubica A, Pietrzykowski Ł, Michalski P, et al. The occurrence of cardiovascular risk factors and functioning in chronic illness in the Polish population of EUROASPIRE V. Cardiol J. 2022. doi:10.5603/CJ.a2022.0102
- Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37(39):2999–3058. doi:10.1093/eurheartj/ehw272
- Piepoli MF, Hoes AW, Agewall S, et al. European Guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts)developed with the special contribution of the European Association for cardiovascular prevention & rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. doi:10.1093/eurheartj/ehw106
- Perk J, De Backer G, Gohlke H, et al.; Authors/Task Force Members. European guidelines on cardiovascular disease prevention in clinical practice (version 2012): the fifth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) *developed with the special contribution of the European Association for cardiovascular prevention & rehabilitation (EACPR). Eur Heart J. 2012;33(13):1635–1701. doi:10.1093/eurheartj/ehs092.
- Pennells L, Kaptoge S, Østergaard HB, et al.; SCORE2-Diabetes Working Group and the ESC Cardiovascular Risk Collaboration. SCORE2-Diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in Europe. Eur Heart J. 2023;44(28):2544–2556. doi:10.1093/eurheartj/ehad260.
- Sowada C, Sagan A, Kowalska-Bobko I Maresso, A. Poland: health system summary. Poland: Health System Summary (Copenhagen: WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies). 2022p. 3, 10.
- Lechowski Ł, Jasion A. Spatial Accessibility of Primary Health Care in Rural Areas in Poland. IJERPH. 2021;18(17):9282. doi:10.3390/ijerph18179282
- Galiè N, Humbert M, Vachiery JL, et al. ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European society of cardiology (esc) and the European respiratory society (ers)endorsed by: Association for European paediatric and congenital cardiology (aepc), international society for heart and lung transplantation (ISHLT). Eur Heart J. 2016;37(1):67–119. doi:10.1093/eurheartj/ehv317
- Hageman S, Pennells L, Ojeda F, et al.; SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–2454. doi:10.1093/eurheartj/ehab309.
- De Vries TI, Cooney MT, Selmer RM, et al.; SCORE2-OP working group and ESC Cardiovascular risk collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J. 2021;42(25):2455–2467. doi:10.1093/eurheartj/ehab312.
- Stern AF. The Hospital Anxiety and Depression Scale. Occup Med. 2014;64(5):393–394. doi:10.1093/occmed/kqu024
- De Smedt D, Clays E, Doyle F, et al. Validity and reliability of three commonly used quality of life measures in a large European population of coronary heart disease patients. Int J Cardiol. 2013;167(5):2294–2299. doi:10.1016/j.ijcard.2012.06.025
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
- Kim JM, Stewart R, Lee YS, et al. Effect of escitalopram vs placebo treatment for depression on long-term cardiac outcomes in patients with acute coronary syndrome: a randomized clinical trial. JAMA. 2018;320(4):350–358. doi:10.1001/jama.2018.9422
- Buszko K, Pietrzykowski Ł, Michalski P, et al. Validation of the Functioning in Chronic Illness Scale (FCIS). Med Res J. 2018;3(2):63–69. doi:10.5603/MRJ.2018.0011
- Chen ML, Chang HK, Yeh CH. Anxiety and depression in Taiwanese cancer patients with and without pain. J Adv Nurs. 2000;32(4):944–951. doi:10.1046/j.1365-2648.2000.t01-1-01560.x
- Bunker SJ, Colquhoun DM, Esler MD, et al. “Stress” and coronary heart disease: psychosocial risk factors. Med J Aust. 2003;178(6):272–276. doi:10.5694/j.1326-5377.2003.tb05193.x
- Jha MK, Qamar A, Vaduganathan M, Charney DS, Murrough JW. Screening and management of depression in patients with cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73(14):1827–1845. doi:10.1016/j.jacc.2019.01.041
- Vongmany J, Hickman LD, Lewis J, Newton PJ, Phillips JL. Anxiety in chronic heart failure and the risk of increased hospitalisations and mortality: a systematic review. Eur J Cardiovasc Nurs. 2016;15(7):478–485. doi:10.1177/1474515116635923
- Levine GN, Cohen BE, Commodore-Mensah Y, et al. Psychological health, well-being, and the mind-heart-body connection: a scientific statement from the American heart Association. Circulation. 2021;143(10). doi:10.1161/CIR.0000000000000947
- Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270(15):1819–1825. doi:10.1001/jama.1993.03510150053029
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802–813. doi:10.1097/01.psy.0000146332.53619.b2
- Novak Sarotar B, Lainscak M. Psychocardiology in the elderly. Wien Klin Wochenschr. 2016;128(Suppl 7):474–479. doi:10.1007/s00508-016-1139-x
- Eschweiler GW. Diagnostics and multimodal treatment of depression in old age: new developments. Z Gerontol Geriatr. 2017;50(2):99–105. doi:10.1007/s00391-016-1174-2
- Palmiero P, Zito A, Maiello M, et al. Primary prevention of cardiovascular risk in octogenarians by risk factors control. CHYR. 2019;15(2):78–84. doi:10.2174/1573402115666190211160811
- Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24(1):18–33. doi:10.1038/s41380-018-0017-5
- Kapfhammer HP. The relationship between depression, anxiety and heart disease - A psychosomatic challenge. Psychiatry Danub. 2011;23(4):412–424.
- Kent LK, Shapiro PA. Depression and related psychological factors in heart disease. Harv Rev Psychiatry. 2009;17(6):377–388. doi:10.3109/10673220903463333
- Marazziti D, Rutigliano G, Baroni S, Landi P, Dell’Osso L. Metabolic syndrome and major depression. CNS Spectr. 2014;19(4):293–304. doi:10.1017/S1092852913000667
- Sin NL, Kumar AD, Gehi AK, Whooley MA. Direction of association between depressive symptoms and lifestyle behaviors in patients with coronary heart disease: the heart and soul study. Ann Behav Med. 2016;50(4):523–532. doi:10.1007/s12160-016-9777-9
- Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment: clinical applications. JAMA. 2002;288(22):2880–2883. doi:10.1001/jama.288.22.2880
- Sabaté E. World Health Organization. editor. Adherence to Long-Term Therapies: evidence for Action. World Health Organization. 2003;1:1.
- Kubica A, Kasprzak M, Obońska K, et al. Discrepancies in assessment of adherence to antiplatelet treatment after myocardial infarction. Pharmacology. 2015;95(1–2):50–58. doi:10.1159/000371392
- Teo KK, Rafiq T. Cardiovascular risk factors and prevention: a perspective from developing countries. Cana J Cardiol. 2021;37(5):733–743. doi:10.1016/j.cjca.2021.02.009
- Martelli E, Enea I, Zamboni M, et al. Focus on the most common paucisymptomatic vasculopathic population, from diagnosis to secondary prevention of complications. Diagnostics. 2023;13(14):2356. doi:10.3390/diagnostics13142356