Abstract
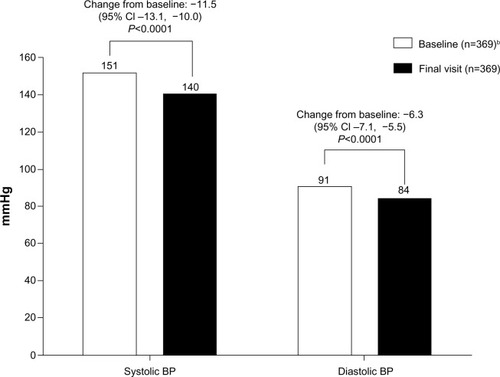
In this retrospective analysis, data pooled from two Phase III/IV open-label Asian studies were used to quantify the additional blood pressure efficacy achieved when titrating amlodipine from 5 mg to 10 mg in mild/moderate hypertensive patients, and compared to data pooled from three Western studies. The primary efficacy end point was the change from baseline in sitting systolic blood pressure (SBP) and diastolic blood pressure (DBP) to the specified time point (4–8 weeks, depending on the trial). For the Asian analysis (n=174), both mean SBP and DBP were significantly decreased at the final visit (SBP −13.3 mmHg, 95% confidence interval [CI] −15.5 to −11.0; DBP −9.2 mmHg, 95% CI −10.6 to −7.8; both P<0.0001). These results were similar to the Western analysis (n=369; SBP −11.5 mmHg, 95% CI −13.1 to −10.0; DBP −6.3, 95% CI −7.1 to −5.5; both P<0.0001). In summary, titration of amlodipine from 5 mg to 10 mg significantly decreased both SBP and DBP in Asian patients with mild-to-moderate hypertension.
Keywords:
Introduction
Hypertension increases the risk of vascular disease, including stroke, myocardial infarction, nephropathy, and retinopathy,Citation1–Citation3 and is a highly prevalent and modifiable risk factor for cardiovascular disease in both economically developed and developing countries. Even small changes in blood pressure have been shown to lower the risk of stroke (by 35%–50%), myocardial infarction (by 20%–25%), and heart failure (by >50%).Citation1,Citation4–Citation7 However, pharmacological intervention is usually required to achieve this.
Calcium-channel blockers (CCBs), including amlodipine, are an effective treatment option for hypertension, as their efficacy is affected neither by age nor ethnicity and because both the risks of cardiovascular events and all-cause mortality are reduced.Citation8 Furthermore, CCBs may have better efficacy for preventing stroke than other classes of antihypertensive agents;Citation7 however, the degree of blood pressure reduction appears to be an important determinant of the size of this treatment effect.Citation8–Citation10 The efficacy of amlodipine for the treatment of hypertension in both normal- and high-cardiovascular-risk hypertensive patients has been demonstrated in multiple large clinical trials,Citation5,Citation11 and CCBs are included in various clinical guidelines as first-line recommendations for hypertension.Citation1,Citation12–Citation14
In the Asia-Pacific region, hypertension may contribute to up to 66% of cardiovascular diseases.Citation15 Research has demonstrated a linear relationship between blood pressure and stroke, and furthermore that the association between blood pressure and stroke is stronger in Asian than Caucasian patients.Citation16,Citation17 Although the efficacy and safety of amlodipine 10 mg has been confirmed in multiple studies,Citation18–Citation21 the option of increasing the amlodipine dose from 5 mg to 10 mg in patients who may benefit from the higher dose has been met with reluctance among some practitioners, especially in Japan, possibly due to concern about adverse events (AEs) (eg, pedal edema) with the 10 mg dose.Citation22
The objective of this study was to quantify the additional blood pressure efficacy achieved when titrating hypertensive Asian patients from amlodipine 5 mg to 10 mg and to compare this with data from Western patients.
Materials and methods
Study design
This was a post hoc, retrospective, pooled analysis. Data from two similarly designed Phase III/IV open-label studies (AML-NY-93-002 and A0531086 [Pfizer data on file]) investigating the safety and efficacy of amlodipine in Asian patients with mild or moderate hypertension were pooled and compared with data pooled from three Western studies (A0531004, A0531044, and A053R0510 [Pfizer data on file]). Eligible patients were male and female, age ≥18 years with mild or moderate hypertension (diastolic blood pressure [DBP] ≥95 to ≤120 mmHg, systolic blood pressure [SBP] >140 to <200 mmHg). The five studies included in this analysis enrolled patients that mirrored actual clinical practice. Namely, they were a mixture of treatment-naïve patients and others who were uncontrolled on prior antihypertensives. All patients remained on stable treatment throughout the study.
Patients received amlodipine at a dose of 5 mg daily for 4–8 weeks, and were then allowed to titrate to 10 mg daily as needed, for an additional 4–8 weeks of treatment. Primary efficacy end points were the change from baseline to final visit in sitting SBP and sitting DBP. Baseline was established prior to titration, ie, after patients had received amlodipine 5 mg daily for 4–8 weeks. Safety end points included assessment of AEs.
Assessments
Efficacy analyses included all patients in the intent-to-treat population who were titrated from 5 mg to 10 mg and had both a baseline and follow-up blood pressure measurement. Safety was assessed by measurement of the frequency of treatment-emergent AEs (all-causality), treatment-emergent serious AEs (all-causality), and AEs resulting in withdrawal from treatment (all-causality). Safety analyses included all patients who were titrated from 5 mg to 10 mg amlodipine.
Statistical analyses
The last observation carried forward was used to impute the end of study blood pressures for those patients who withdrew early. Descriptive statistics were used for quantitative variables and frequency counts by category for qualitative variables. A single-sample t-test was used to test the null hypothesis of no mean change from baseline in blood pressure, along with corresponding 95% confidence interval (CI).
Results
Study population
Of the 174 patients included in the Asian analysis, 69 (40%) were from Japan, with the remaining patients distributed across the People’s Republic of China, Hong Kong, Indonesia, South Korea, the Philippines, Taiwan, and Thailand. Just over half of the patients were male, and the mean age of patients was 55.9 years (). The baseline mean (standard error [SE]) SBP was 149.3 (1.28) mmHg and DBP was 93.0 (0.84) mmHg. For the Western analysis, 206/383 (53.8%) patients were male, the mean age was 59.6 years, and the baseline mean (SE) SBP was 151.4 (0.82) mmHg and DBP was 90.5 (0.48) mmHg ().
Table 1 Baseline characteristics of the pooled Asian and Western populations
Of the 174 patients included in the Asian analysis, 100% were treated and included in the efficacy and safety analyses. A total of 159 (91.4%) patients completed the study, and 15 (8.6%) discontinued. Reasons for discontinuation included AEs (n=9, 5.2%); withdrawal of consent and other (both n=1, 0.6%). For comparison, in the Western studies, 353 of 385 (91.7%) completed the study, and 32 of 385 (8.3%) discontinued due to AEs (24, 6.2%), patient no longer willing to participate (four, 1.0%), other, and protocol violation (both two, 0.5%).
Efficacy
Titration of amlodipine from 5 mg daily to 10 mg daily resulted in a statistically significant decrease in blood pressure. Amlodipine 10 mg lowered SBP by −13.3 mmHg (95% CI −15.5 to −11.0) and DBP by −9.2 mmHg (95% CI −10.6 to −7.8) at the final visit (P<0.0001 for both) (). These results were similar to those of the pooled analysis of three Western studies (SBP −11.5 mmHg, 95% CI −13.1 to −10.0; DBP −6.3 mmHg, 95% CI −7.1 to −5.5; both P<0.0001; ).
Figure 1 Blood pressure of patients titrated from amlodipine 5 mg to 10 mg from the pooled analysis of Asian studies, at baseline and final visit.a
Abbreviation: BP, blood pressure.
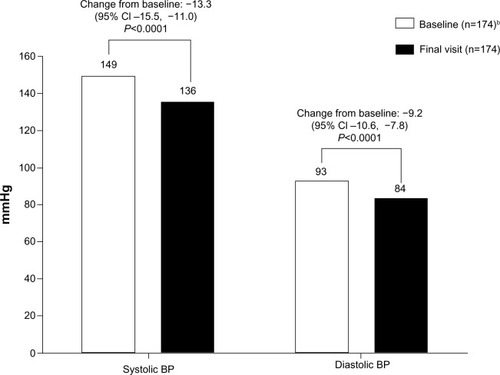
Figure 2 Blood pressure of patients titrated from amlodipine 5 mg to 10 mg from the pooled analysis of Western studies, at baseline and final visit.a
Abbreviation: BP, blood pressure.
Safety
A total of 65 of 174 (37.4%) Asian patients experienced 142 AEs (), of which infections 14.9% (26), musculoskeletal 12.6% (22), gastrointestinal 9.8% (17), and general disorders 9.8% (17) were the most commonly reported postbaseline. Peripheral edema occurred in eleven of 174 (6.3%) patients. Serious AEs were reported by four patients (one cardiac disorder, 0.6%; three neoplasms, 1.7%). Treatment was withdrawn from nine patients due to an AE. Of the AEs that led to treatment withdrawal, neoplasms (n=3, 1.7%), general disorders (n=2, 1.1%), and nervous system disorders (n=2, 1.1%) occurred in one or more patients; cardiac disorders, gastrointestinal disorders, infections and investigations, each occurred in one patient. None of the patients discontinued treatment due to peripheral edema.
Table 2 Incidence of adverse events for the pooled Asian and Western populations
For comparison, in the Western studies, 100 of 385 (26.0%) patients experienced 174 AEs (). Peripheral edema occurred in 35 of 385 (9.1%) patients. Serious AEs were reported by two patients (cardiac disorder, n=1, 0.3%; infections and infestations, n=1, 0.3%; and nervous system disorders, n=2, 0.5%). Treatment was withdrawn from 14 patients due to an AE. Of the AEs that led to treatment withdrawal, general disorders (n=10, 2.6%); musculoskeletal and connective tissue disorders (n=3, 0.8%); nervous system disorders (n=3, 0.8%); psychiatric disorders (n=2, 0.5%), respiratory, thoracic, and mediastinal (n=2, 0.5%), skin and subcutaneous tissue (n=2, 0.5%), and vascular disorders (n=2, 0.5%) occurred in two or more patients. Nine (2.3%) patients discontinued treatment due to peripheral edema.
Discussion
Although the need for effective management of blood pressure is well understood, adherence to antihypertensive treatment and blood pressure control continues to be a challenging international health goal.Citation23 In recent guidelines, eg, those produced by the European Society of Hypertension/European Society of Cardiology,Citation24 CCBs, such as amlodipine, are recommended as first-line antihypertensive agents.
The efficacy of amlodipine monotherapy in reducing blood pressure is well established in a number of populations, including patients aged ≥65 years,Citation25 pediatric patients,Citation26 patients treated at primary and also specialized care centers,Citation27 and patients of different ethnic origin.Citation28 The results of a meta-analysis suggest that CCBs have better efficacy for preventing stroke than other classes of antihypertensive agents.Citation7 Another meta-analysis determined that this benefit of CCBs extended to reduction in the risk for cardiovascular death, major cardiovascular events, and heart failure.Citation8 For patients who receive amlodipine, the size of the reduction in risk of stroke is largely dependent on the magnitude of the reduction in blood pressure achieved.Citation9 In particular, the association between blood pressure and stroke is known to be stronger in Asian than Caucasian patients.Citation16,Citation17 Furthermore, other research suggests that in addition to its antihypertensive-related effect, amlodipine has a blood pressure-independent beneficial effect on stroke risk;Citation9,Citation10 administration of amlodipine may lead to enhanced endothelial nitric oxide production, inhibition of smooth-muscle cell proliferation, and antioxidant activity: effects not characteristic of some of the other CCBs.Citation29,Citation30 Recent evidence also suggests amlodipine lowers levels of highly sensitive cardiac troponin – which is associated with cardiovascular disease, mortality, and heart failure – to a greater extent than the combination of losartan and hydrochlorothiazide.Citation31
There is a significant association between disrupted diurnal variations in blood pressure and cardiovascular disease. Nondippers with diminished nocturnal blood pressure fall, and risers with higher nocturnal blood pressure than daytime blood pressure are associated with target-organ damage and subsequent cardiovascular events.Citation32,Citation33 In addition, exaggerated morning surge is an independent predictor of cardiovascular events.Citation34,Citation35 Amlodipine maintains blood pressure in patients with diurnal variations in blood pressure, eg, it attenuates morning surge in blood pressure in hypertensive individuals.Citation36 A once-daily dose of long-acting amlodipine can control ambulatory blood pressure throughout a 24-hour period in elderly uncomplicated hypertensive patients with different nighttime blood pressure dipping.Citation37 The ALPHABET study demonstrated that the effects of high-dose (10 mg) amlodipine on clinic, home, and ambulatory blood pressure control, and brain natriuretic peptide reduction were similar to the combination of losartan and hydrochlorothiazide.Citation38 Furthermore, amlodipine may have additional protective benefits in not reducing nocturnal blood pressure to the extent that it accelerates brain ischemia in some hypertensive patients with marked nocturnal blood pressure reduction.Citation39,Citation40
In this retrospective post hoc analysis, the titration of amlodipine from 5 mg to 10 mg daily significantly decreased both SBP and DBP in Asian patients with mild-to-moderate hypertension. Amlodipine 10 mg lowered SBP by −13.3 mmHg (95% CI −15.5 to −11.0) and DBP by −9.2 mmHg (95% CI −10.6 to −7.8) at the final visit (P<0.0001 for both). Not only were the results from this analysis similar to those of the pooled analysis of three Western studies, they also provide support for other studies that have also shown the benefits of titrating from amlodipine 5 mg to 10 mg in hypertensive Asian patients. In the Amlodipine Cohort Study by Internet-Based Research for Evaluation of Efficacy (ACHIEVE), Kario et alCitation20 reported that in poorly controlled hypertensive Japanese patients, titration from amlodipine 5 mg to 10 mg daily significantly reduced both home and clinic blood pressure. Furthermore, these reductions seemed to be more pronounced among patients with higher baseline blood pressure than in those with lower baseline blood pressure values. In another study, Uno et alCitation21 compared the efficacy and tolerability of amlodipine 5 mg and 10 mg in Japanese hypertensive patients, and found that amlodipine 10 mg resulted in greater reductions in blood pressure versus amlodipine 5 mg. These blood pressure reductions were also shown to be significantly correlated with reductions in both hypertensive cardiac overload and renal damage (measured by brain natriuretic peptide and microalbuminuria levels, respectively). The wealth of studies reporting not only the dangers of sustained hypertension on the risk of cardiovascular events but also the benefits of uptitration to amlodipine 10 mg in reducing elevated blood pressure highlights the importance of encouraging this strategy in prescribing patterns.
Overall, more AEs were reported in the Asian population than in the Western population (37% versus 26%). In particular, AEs of nasopharyngitis, back pain, diabetes mellitus, and flushing were all four times more common in the Asian population versus the Western population. Whereas it is well documented that diabetes is more prevalent in Asian subjects, the reason for the higher incidences of nasopharyngitis, back pain, and flushing reported in Asian subjects in this analysis is unknown. A possible explanation for the higher incidence of nasopharyngitis observed in Asian versus Western patients is that it has been reported that the Asians are more susceptible to catching colds than those from any other region;Citation41 however, literature to support this theory is currently limited, and further research is required.
It has been reported that some practitioners in Asia, particularly Japan, are reluctant to prescribe a higher dose of amlodipine, perhaps due to concerns about an increased incidence of pedal edema with the 10 mg dose.Citation22 Of the 174 patients included in this pooled analysis, peripheral edema occurred in eleven patients (6.3%). Furthermore, there were no treatment discontinuations as a result of peripheral edema, demonstrating that despite concerns, the increased dose of amlodipine is not associated with a worsened safety signal.
In summary, in this retrospective post hoc analysis, the titration of amlodipine from 5 mg to 10 mg daily significantly decreased both SBP and DBP in Asian patients with mild-to-moderate hypertension. The findings of this analysis support the uptitration of amlodipine from 5 mg to 10 mg in order to reduce blood pressure in Asian patients with hypertension.
Disclosure
This analysis was funded by Pfizer Inc. Jeffery Robbins and Barrett W Jeffers are employees of Pfizer Inc. Kazuomi Kario reports no specific funding in relation to this research and has no conflicts of interest to disclose on this paper. Editorial support was provided by Helen Jones, PhD, and Michelle Jenvey, PhD, of Engage Scientific and funded by Pfizer Inc.
References
- ChobanianAVBakrisGLBlackHRSeventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureHypertension20034261206125214656957
- VasanRSLarsonMGLeipEPImpact of high-normal blood pressure on the risk of cardiovascular diseaseN Engl J Med2001345181291129711794147
- LewingtonSClarkeRQizilbashNPetoRCollinsRAge-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiesLancet200236093491903191312493255
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research GroupMajor outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT)JAMA2002288232998300712479764
- DahlöfBSeverPSPoulterNRPrevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trialLancet2005366948989590616154016
- OgiharaTNakaoKFukuiTEffects of candesartan compared with amlodipine in hypertensive patients with high cardiovascular risks: candesartan antihypertensive survival evaluation in Japan trialHypertension200851239339818172059
- LawMRMorrisJKWaldNJUse of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studiesBMJ2009338b166519454737
- CostanzoPPerrone-FilardiPPetrettaMCalcium channel blockers and cardiovascular outcomes: a meta-analysis of 175,634 patientsJ Hypertens20092761136115119451836
- TakagiHUmemotoTRevisiting evidence of blood pressure-dependent and independent effects of amlodipine on the risk of strokeJ Clin Hypertens (Greenwich)2011131078178221974768
- WangJGLiYFranklinSSSafarMPrevention of stroke and myocardial infarction by amlodipine and angiotensin receptor blockers: a quantitative overviewHypertension200750118118817502490
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research GroupMajor outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)JAMA2002288232981299712479763
- DaskalopoulouSSKhanNAQuinnRRThe 2012 Canadian hypertension education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapyCan J Cardiol201228327028722595447
- ManciaGLaurentSAgabiti-RoseiEReappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force documentBlood Press200918630834720001654
- WangJGKarioKLauTUse of dihydropyridine calcium channel blockers in the management of hypertension in Eastern Asians: a scientific statement from the Asian Pacific Heart AssociationHypertens Res201134442343021228778
- MartiniukALLeeCMLawesCMHypertension: its prevalence and population-attributable fraction for mortality from cardiovascular disease in the Asia-Pacific regionJ Hypertens2007251737917143176
- LawesCMRodgersABennettDABlood pressure and cardiovascular disease in the Asia Pacific regionJ Hypertens200321470771612658016
- PerkovicVHuxleyRWuYPrabhakaranDMacMahonSThe burden of blood pressure-related disease: a neglected priority for global healthHypertension200750699199717954719
- FogariRMugelliniADerosaGEfficacy and tolerability of candesartan cilexetil/hydrochlorothiazide and amlodipine in patients with poorly controlled mild-to-moderate essential hypertensionJRAAS20078313914417907102
- NissenSETuzcuEMLibbyPEffect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trialJAMA2004292182217222515536108
- KarioKOdawaraMKimuraKNodeKNearly half of uncontrolled hypertensive patients could be controlled by high-dose titration of amlodipine in the clinical setting: the ACHIEVE studyCurr Hypertens Rev20117102110
- UnoHIshikawaJHoshideSEffects of strict blood pressure control by a long-acting calcium channel blocker on brain natriuretic peptide and urinary albumin excretion rate in Japanese hypertensive patientsHypertens Res200831588789618712044
- WeirMRIncidence of pedal edema formation with dihydropyridine calcium channel blockers: issues and practical significanceJ Clin Hypertens (Greenwich)20035533033514564133
- ChockalingamACampbellNRFodorJGWorldwide epidemic of hypertensionCan J Cardiol200622755355516755308
- ManciaGFagardRNarkiewiczK2013 ESH/ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)J Hypertens20133171281135723817082
- LangdonCTreatment of hypertension in patients ≥65 years of age: experience with amlodipineClin Ther200022121473148211192138
- TallianKBNahataMCTurmanMAMahanJDHayesJRMentserMIEfficacy of amlodipine in pediatric patients with hypertensionPediatr Nephrol199913430431010454779
- ValcárcelYJiménezRHernándezVArísteguiRGilAEfficacy and safety of amlodipine: a comparative study of hypertensive patients treated at primary- and specialised-care centresClin Drug Investig2006263125133
- SowunmiAWalkerOSalakoLAAmlodipine as monotherapy in hypertensive Africans: clinical efficacy and safety studiesAfr J Med Med Sci199625321321610457792
- JorgensenBSimonsenSEndresenKRestenosis and clinical outcome in patients treated with amlodipine after angioplasty: results from the Coronary Angioplasty Amlodipine Restenosis Study (CAPARES)J Am Coll Cardiol200035359259910716459
- MasonRPMechanisms of plaque stabilization for the dihydropyridine calcium channel blocker amlodipine: review of the evidenceAtherosclerosis2002165219119912417269
- HoshideSFukutomiMEguchiKWatanabeTKabutoyaTKarioKChange in high-sensitive cardiac troponin T on hypertensive treatmentClin Exp Hypertens2013351404422631049
- KarioKMatsuoTKobayashiHImiyaMMatsuoMShimadaKNocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippersHypertension19962711301358591875
- KarioKPickeringTGMatsuoTHoshideSSchwartzJEShimadaKStroke prognosis and abnormal nocturnal blood pressure falls in older hypertensivesHypertension200138485285711641298
- KarioKPickeringTGUmedaYMorning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective studyCirculation2003107101401140612642361
- KarioKMorning surge in blood pressure and cardiovascular risk: evidence and perspectivesHypertension201056576577320937968
- IshimitsuTMinamiJKawanoYNumabeATakishitaSMatsuokaHAmlodipine, a long-acting calcium channel blocker, attenuates morning blood pressure rise in hypertensive patientsClin Exp Pharmacol Physiol199926750050410405773
- EguchiKKarioKShimadaKEffects of long-acting ACE inhibitor (temocapril) and long-acting Ca channel blocker (amlodipine) on 24-h ambulatory BP in elderly hypertensive patientsJ Hum Hypertens200115964364811550111
- FukutomiMHoshideSEguchiKWatanabeTShimadaKKarioKDifferential effects of strict blood pressure lowering by losartan/hydrochlorothiazide combination therapy and high-dose amlodipine monotherapy on microalbuminuria: the ALPHABET studyJ Am Soc Hypertens201261738222054782
- IshikawaJHoshideSEguchiKIshikawaSShimadaKKarioKNighttime home blood pressure and the risk of hypertensive target organ damageHypertension201260492192822892810
- KarioKShimadaKDifferential effects of amlodipine on ambulatory blood pressure in elderly hypertensive patients with different nocturnal reductions in blood pressureAm J Hypertens19971032612689056682
- NielsenHeadaches, colds and backache – most common health complaints: Nielsen Global Survey2007 Available from: http://nz.nielsen.com/news/OTC_Aug07.shtmlAccessed July 29, 2013