Abstract
The association between mean arterial blood pressure (MAP) and hematocrit (Hct) as a surrogate for blood viscosity was investigated in a young (average 20.0±2.3 years), healthy population of 174 men and 442 women. Health status was assessed by clinical examination and serological evaluation. Individuals with severe anemia or hemoconcentration, prior traumas or major surgical intervention, smokers, and pregnant or lactating women were excluded from the study. The MAP/Hct association was positive and significant (P=0.04) for women and negative, albeit not significantly so, for men. The MAP/Hct association was also evaluated in subgroups of the same population with a progressive step-by-step exclusion of: individuals with cholesterol >200 mg/dL; triglycerides >200 mg/dL; body mass index >25 kg/m2; and glucose >100 mg/dL. This consecutively reduced the strength of the positive MAP/Hct association in women, which became negative – although not significantly so – when all anomalously high factors were excluded. The same trend was found in men. Our study indicates that previously reported positive trends in the relationship between the MAP and Hct in the population are not present in a young, healthy population of men or women that excludes individuals with the confounding factors of above normal serological values and BMI.
Introduction
A direct relationship between hypertension, elevated hematocrit (Hct), and blood viscosity was found in studies pioneered by Letcher et al.Citation1 These results were confirmed by findings of the Edinburgh Artery Study, a study that evaluated the blood pressure/viscosity association in 1,592 men and women aged 55–74 years.Citation2 This study concluded that there was evidence of a strong association between blood viscosity and arterial pressure, independently of confounding factors. The same conclusion was reached by the Gubbio Population Study (2,809 men and women aged 25–74 years).Citation3 That study reported a significant independent association between Hct and the prevalence of hypertension and a positive relationship between Hct and blood pressure.
Studies conducted in a populationCitation4 of >100,000 blood donors in the Netherlands reported a positive association between hemoglobin levels and systolic and diastolic blood pressure in adult men and women (49.3±12.5 and 42.4±13.7 years). This study included individuals considered to be healthy with data adjusted for age, body mass index (BMI), mean daily temperature, season, smoking, and antihypertensive drug treatment.
However, studies in populations that can be clinically evaluated tend to show that a significant positive association between MAP and Hct is related to age and/or clinical conditions that may coexist with endothelial dysfunction.Citation5–Citation7 Conversely, healthy controls in these studies tend not to show a positive correlation between MAP and Hct.
Normal endothelial function regulates peripheral vascular resistance due to changes in blood viscosity, by producing the vasodilators nitric oxide and prostacyclin via mechanotransduction in response to flow-induced shear stress on the vascular wall.Citation8 Shear stress at the vessel wall due to blood viscosity, flow, and blood vessel diameter therefore contributes to the autoregulation of blood pressure if the endothelium is responsive and – presumably – healthy.Citation9
In a previous study, we investigated the relationship between MAP and Hct in a healthy population residing in the same locality;Citation10 however, factors that may influence the MAP/Hct trend were not explored. In the present study, we investigated the relationship of MAP versus Hct in a relatively uniform population of younger adults whose health status was determined by clinical interview and anthropometric and serological measurements, with the aim of finding readily measurable variables that affect the MAP/Hct trend.
Methods
The study was carried out in an open population of young adults aged 17–25 years in the city of Durango, Mexico, invited to participate by means of radio and newspaper announcements made by the Universidad Juárez del Estado de Durango. The study was approved by the Ethical Committee of the Universidad Nacional Autónoma de México, México DF, Mexico. Written informed consent was obtained and signed by all participants prior to the investigation. Parents or guardians provided the written consent for minors (individuals under 18 years).
Both females and males who were considered healthy blood donors as determined by the analysis of a written questionnaire, blood pressure measurement not showing hypertension, and the absence of the exclusion criteria, were all included in the study. Individuals were excluded from the study with diagnosis of hemorheological perturbations, such as: severe anemia (blood hemoglobin <10 and 12 g/dL for women and men respectively); hemoconcentration (hemoglobin >18 and 20 g/dL for women and men respectively); traumas or major surgical intervention in the preceding six months; and smoking habits (those who in the previous 6 months consumed at least one cigarette). We additionally excluded subjects with previous or recent diagnosis of diabetes mellitus, cardiovascular diseases, chronic hepatic or renal disease, inflammatory or autoimmune disorders, acute or chronic infectious diseases, cancer, endocrine disorders, as well as pregnant or lactating women.
All participants were asked to provide their clinical history. Height, weight, BMI, and blood pressure (criteria of the VII Joint National Committee on Prevention, Detection, and Treatment; High Blood Pressure, National Heart, Lung, and Blood Institute; 2003) were measured at this time.
Hematocrit varies through the day as a function of fluid and food intake, level of exercise, etc. Therefore, to ensure a degree of uniformity of hydration, participants were summoned at 8 am for blood sampling, after 8–12 hours of fasting. Blood pressure was measured first after 5 minutes of resting in the sitting position with an automatic instrument (Omron model BP742, Omron Healthcare, Inc., Bannockburn, IL, USA) three times in the left arm at heart level, at 5-minute intervals and averaged. Glucose, cholesterol, and triglycerides were measured in drawn blood samples with the instrument Accutrend® GCT (Roche Diagnostics GmbH, Mannheim, Germany), which uses a drop of blood obtained from an index finger puncture. Hematocrit and hemoglobin determinations were made by the same method using the instrument HemoCue Hb 201 (HemoCue, Inc., Cypress, CA, USA). These tests were subsequently repeated for individuals who had significant clinical alterations, using standard laboratory analysis techniques.
Statistical analysis
The association between MAP and Hct for the population was evaluated by determining the Spearman’s correlation coefficient of these two variables. The influence of serological factors and BMI upon the MAP/Hct relationship was assessed by the consecutive step-by-step removal of individuals who had values above the normal thresholds for these parameters and reanalyzing the level of association by means of the Spearman’s correlation coefficient, excluding individuals according to the backward-stepwise selection method.Citation11
The order of removal was established by ranking the serological parameters and the BMI above the normal threshold that caused the steepest slope on the MAP/Hct association (ie, produced the strongest effect) when only the individuals with this parameter anomaly were investigated. Individuals with the parameter showing the strongest effect were removed first. Statistical analysis was performed using the GraphPad Prism 5 software (GraphPad Software, Inc., La Jolla, CA, USA). Differences were considered significant when P<0.05.
Results
The study included 616 individuals (442 women and 174 men), aged 17–25 years. The average age was 20.0±2.3 years. The principal characteristics of the population studied are given in .
Table 1 Demographic, anthropometric, and serologic characteristics of the young adult population examined in the municipality of the city of Durango, Mexico
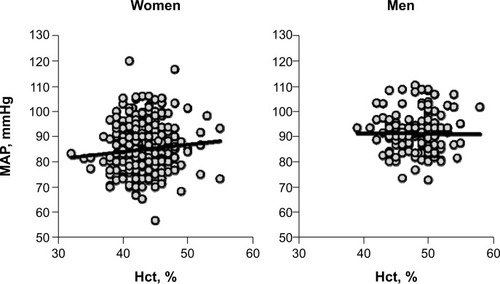
The relationship between MAP and Hct was evaluated for the whole study population separated by sex. Results are presented in showing that the trend of MAP/Hct association is positive and significant for women (P=0.04; r=0.10), and negative – albeit not significant – for men (P=0.91; r=−0.05).
Figure 1 MAP plotted as function of Hct for the study population of individuals described in .
Abbreviations: MAP, mean arterial blood pressure; Hct, hematocrit; BMI, body mass index; n, number.
As shown in , men and women presented variability in parameter values. Some individuals exceeded the normal serological and BMI thresholds. The differences between and men and women in BMI, MAP, glucose, cholesterol, and triglycerides are typical of the Mexican population; these same trends have been previously reported.Citation12 The difference in Hct between men and women is found in all healthy young populations.Citation13
The slope of the MAP/Hct association was evaluated for groups whose individuals had each of their serological and BMI values above the normalcy threshold. This analysis showed that the steepest slope for the MAP/Hct relationship occurred in individuals with cholesterol levels >200 mg/dL; progressively lesser effects were observed in the order of parameters shown in .
Table 2 Thresholds defining the upper limit of parameters for the normal population
This information was used to reevaluate the MAP/Hct relationship in groups in which individuals with values above the threshold for a given parameter were progressively removed from the respective group, in the order shown in , obtaining the results shown in and .
Table 3 Women
Table 4 Men
The net effect of this treatment of the data was the nonsignificant lowering of the value of m (slope) ( and ) in the association between MAP and Hct. Excluding women with abnormally high cholesterol caused their positive MAP/Hct association to become not statistically significant, changing the P-value from 0.04–0.14. The subsequent exclusion of women with high triglycerides yielded P=0.90 for the MAP/Hct association. Further step-by-step removal of individuals with above threshold values of BMI and glucose caused the trend to become negative (but not significant). Applying the procedure to the data from men caused the negative slope of the MAP/Hct association to become progressively steeper, ie, with a numerically greater negative slope m, although without reaching significance.
Discussion
The principal result of this study is that – in a young healthy population, with normal serological parameters and BMI – the relationship between MAP and Hct for men and women shows a nonsignificant negative trend. This result is different from that found in several studies of older populations showing positive and significant trends.Citation2,Citation3 We also show that excluding healthy women who present serological parameters beyond the threshold of normalcy reduces the strength (ie, the slope and the significance) of the association between MAP and Hct, which becomes negative although not significant when the confounding factors are removed.
In the case of men, the MAP/Hct association is negative but not significant for the whole population; removing individuals with anomalous parameter values reduces the slope and the strength of the association. However, this reduction is not significant.
The path taken to investigate the effect of above threshold serological parameters and BMI on the MAP/Hct association is somewhat arbitrary since it does not account for the incidence of occurrence (ie, proportion of individuals) of the abnormalities in the population. The significant result is that there is no MAP/Hct association in a population that has normal serological data and BMI, and that – in the tested population – only 9% of women and 22% of men could be considered normal, according to the chosen criteria.
The proportion of males with no BMI or serology abnormalities was 28.7% versus 38.7% for women, a difference due to the incidence of overweight and obesity in men (46.6% versus 28.5%).
Blood viscosity is primarily determined by Hct, being a nonlinear function of this parameter.Citation13,Citation14 However, the relationship between blood viscosity and Hct for the normal range of variability of Hct in the population can be considered linear,Citation10 which facilitates the study of the MAP/blood viscosity relationship in large populations, where the measurement of blood viscosity could be substituted with the measurement of Hct.
In our study, we used Hct as a surrogate for blood viscosity, an assumption that may not be accurate in older individuals who may show altered plasma composition, particularly concerning fibrinogen and other rheological abnormalities, such as decreased red blood cell flexibility.Citation15 Although we did not evaluate blood fibrinogen, this assumption should be accurate for the population studied, given its age and health.Citation16
Blood viscosity is one of the determinants of peripheral vascular resistanceCitation17 and, hence, in a circulatory system consisting of rigid tubes increasing blood viscosity increases vascular resistance, according to the Hagen–Poiseuille law. Supporting experimental data on the effect of blood viscosity on MAP originate with the classical studies of Richardson and GuytonCitation18 and those of Messmer et al.Citation19 However, the Hct changes studied were significantly greater than those associated with the variability of Hct in the normal population.
Experimental studies on changes of Hct in the range of variability of the normal population yield different results. Martini et alCitation20,Citation21 showed in awake animals that acutely increasing blood viscosity above normal by about 10% through altering isovolemic hemoconcentration significantly lowered the MAP and increased the cardiac output. It should be noted that these are acute responses that may not extrapolate to chronic conditions. However, these changes of blood pressure lasting several hours do not appear to be regulated by baroreceptor responses.
The control of peripheral vascular resistance in the normal organism independently from the activity of the central nervous system is linked to mechanotransduction, via shear stress at the blood vessel wall that governs the production of vasodilators.Citation22,Citation23 Shear stress is in part determined by blood viscosity,Citation24,Citation25 which can have two opposing effects on peripheral vascular resistance. Namely, it can have a direct effect due to simple hemodynamic hindrance and a second, opposite effect due to the response to vasodilator release.
Evidence for lack of association between MAP and blood viscosity
Our results support the concept that increased Hct does not lead to an increased MAP in the young, healthy population. Furthermore, our present and previous studies indicate that the association may be negative, with increased Hct leading to lower MAP. Therefore, it is of interest to briefly analyze the results of previous studies in terms of the characteristics of the populations tested.
The relationship between blood viscosity and MAP was studied in a healthy population of 84 men and 65 women (30.6±8.0 years) from the city of Durango. The trend of association with MAP/viscosity was negative but not significant for women; there was a negative linear correlation (r=0.22; P=0.03) for men.Citation10
The study of de Simone et alCitation26 showed that systolic blood pressure and blood viscosity were negatively correlated in the Native Americans who participated in the Strong Heart Study (P<0.01).Citation26 Conversely, Paul et alCitation27 showed that hypertension and anemia, and therefore decreased blood viscosity, were positively correlated. A group of 646 young male office workers (age range, 18–41 years; 28.3±5.6) in Tokyo, Japan, was investigated using multiple regression analysis of systolic (SBP) and diastolic blood pressure (DBP) using Hct, age, BMI, and drinking and smoking habits as independent variables. The results showed that Hct was a significant independent variable for DBP (P<0.001) but not for SBP.Citation28 This association can be interpreted to be representative of a normal endothelial autoregulation of peripheral vascular resistance.Citation29
A study of healthy subjects selected from participants in a campaign of prevention of cardiovascular disease (n=103) in Catanzaro, Italy, showed that the only variables that were significantly positively associated were SBP and age, and DBP and Hct.Citation30
The effect of aging on endothelial function is evident in women that pass from pre- to postmenopause.Citation31 Salazar Vázquez et alCitation32 analyzed the distribution of MAP and Hct in a population of pre- and postmenopause women from the city of Durango, Mexico. In this study, healthy nonsmoking premenopausal women (n=85) showed a nonsignificant negative correlation (P=0.5) between MAP and Hct, while menopausal women (n=92) presented a positive correlation (P<0.01). Women aged >60 years in the city of Stockholm, Sweden, (n=2,189) showed an identical MAP/Hct trend to that of menopausal women in Durango.Citation32
The study of de Simone et alCitation33 found a significant independent relation between SBP, DBP, MAP, and blood viscosity (measured over a range of shear rates) as well as Hct (r=0.17–0.23; all P<0.05) in a cohort of normotensive members of the employed population in New York City.Citation34 The study included apparently normal men and women who were 27–75 years old.
Adaptation to altitude increases Hct and MAPCitation35, the increase in MAP preceding the increase in Hct; however, the prolonged residence at high altitude lowers MAP relative to that of sea level residents.Citation36–Citation38 The decrease of MAP with altitude is attributed to the relaxation of the vascular smooth muscle, increased collateral circulation, increased vascularization,Citation39 higher red blood cell and hemoglobin levels, hypocaloric stress, and respiratory ailments.Citation40,Citation41
However, the hypothesis that this may be due to increased mechanotransduction caused by increased Hct and blood viscosity appears to have not been considered. In general, children and young adults of populations that adapt to altitude by increasing Hct have comparatively lower MAP than similarly aged populations at sea level.
A common trend in these studies is that the MAP/Hct association is positive in conditions where the organism has some form of dysfunction; it is not significant in healthy persons.
Conclusion
Our results show that, in normal healthy males and females, MAP is not elevated when Hct is higher than the norm if the serological parameters and the BMI do not exceed the normalcy thresholds. Most studies in the literature that report a positive and significant association between MAP and Hct include older individuals. Values of plasma glucose, cholesterol, and triglycerides exceeding the normal threshold are related to increased blood pressure. Hence, it is not surprising that the exclusion of these individuals lowers the strength of the MAP/Hct association. A mechanism that may in part explain the lack of MAP/Hct association for normal individuals is the increase of shear stress at the blood vessel wall interface due to increased viscosity, which – according to the mechanisms of endothelial biochemical mechanotransduction – increases the release of vasodilators by the endothelium, an effect not present with endothelial dysfunction.Citation8
Our results indicate that the increase in Hct in healthy young individuals is not related to the increase of MAP.
Acknowledgments
This work was supported by a grant FOMIX (Fondo mixto: combined funding) CONACYT (Consejo Nacional de Ciencia y Technología: National Counsel for Science and Technology) clave 66638, México; BY Salazar Vázquez, principal investigator.
Disclosure
The authors report no conflicts of interest in this work.
References
- LetcherRLChienSPickeringTGSealeyJELaraghJHDirect relationship between blood pressure and blood viscosity in normal and hypertensive subjects. Role of fibrinogen and concentrationAm J Med1981706119512027234890
- FowkesFGLoweGDRumleyALennieSESmithFBDonnanPTThe relationship between blood viscosity and blood pressure in a random sample of the population aged 55 to 74 yearsEur Heart J19931455976018508852
- CirilloMLaurenziMTrevisanMStamlerJHematocrit, blood pressure, and hypertension. The Gubbio Population StudyHypertension19922033193261516951
- AtsmaFVeldhuizenIde KortWvan KraaijMPasker-de JongPDeinumJHemoglobin level is positively associated with blood pressure in a large cohort of healthy individualsHypertension201260493694122949533
- Romero-CorralASert-KuniyoshiFHSierra-JohnsonJModest visceral fat gain causes endothelial dysfunction in healthy humansJ Am Coll Cardiol201056866266620705223
- KregelKCZhangHJAn integrated view of oxidative stress in aging: basic mechanisms, functional effects, and pathological considerationsAm J Physiol Regul Integr Comp Physiol20072921R18R3616917020
- ArcaroGCrettiABalzanoSInsulin causes endothelial dysfunction in humans: sites and mechanismsCirculation2002105557658211827922
- MartiniJCabralesPTsaiAGIntagliettaMMechanotransduction and the homeostatic significance of maintaining blood viscosity in hypotension, hypertension and haemorrhageJ Intern Med2006259436437216594904
- SriramKSalazar VázquezBYTsaiAGCabralesPIntagliettaMTartakovskyDMAutoregulation and mechanotransduction control the arteriolar response to small changes in hematocritAm J Physiol Heart Circ Physiol20123039H1096H110622923620
- VázquezBYBlood pressure and blood viscosity are not correlated in normal healthy subjectsVasc Health Risk Manag201281622272069
- MotulskyHMultiple regressionIntuitive Biostatistics, A Nonmathematical Guide to Statistical Thinking3rd edNew York, NYOxford University Press2013341356
- SternMPRosenthalMHaffnerSMHazudaHPFrancoLJSex difference in the effects of sociocultural status on diabetes and cardiovascular risk factors in Mexican Americans. The San Antonio Heart StudyAm J Epidemiology19841206834851
- KamenevaMVWatachMJBorovetzHSGender difference in rheologic properties of blood and risk of cardiovascular diseasesClin Hemorheol Microcirc1999213–435736310711771
- PirofskyBThe determination of blood viscosity in man by a method based on Poiseuille’s lawJ Clin Invest195332429229813052686
- BaskurtOKMeiselmanHJBlood rheology and hemodynamicsSemin Thromb Hemost200329543545014631543
- DrenosFMillerGJHumphriesSEIncrease of plasma fibrinogen levels and variability with age in a sample of middle aged healthy menAnn Hum Genet200771Pt 1435316999842
- BaskurtOKYalcinOMeiselmanHJHemorheology and vascular control mechanismsClin Hemorheol Microcirc2004303–416917815258340
- RichardsonTQGuytonACEffects of polycythemia and anemia on cardiac output and other circulatory factorsAm J Physiol195919711671170
- MessmerKSunder-PlassmannLKlövekornWPHolperKCirculatory significance of hemodilution: rheological changes and limitationsAdvances in MicrocirculationHardersH(Hamburg). S. Karger AGBasel, Switzerland1972177
- MartiniJCarpentierBNegreteACFrangosJAIntagliettaMParadoxical hypotension following increased hematocrit and blood viscosityAm J Physiol Heart Circ Physiol20052895H2136H214316006543
- MartiniJTsaiAGCabralesPJohnsonPCIntagliettaMIncreased cardiac output and microvascular blood flow during mild hemoconcentration in hamster window modelAm J Physiol Heart Circ Physiol20062911H310H31716489106
- FrangosJAEskinSGMcIntireLVIvesCLFlow effects on prostacyclin production in cultured human endothelial cellsScience19852274693147714793883488
- YalcinOUlkerPYavuzerUMeiselmanHJBaskurtOKNitric oxide generation by endothelial cells exposed to shear stress in glass tubes perfused with red blood cell suspensions: role of aggregationAm J Physiol Heart Circ Physiol20082945H2098H210518326799
- MelkumyantsAMBalashovSAKhayutinVMEndothelium dependent control of arterial diameter by blood viscosityCardiovasc Res19892397417472611812
- SmieskoVLangDJJohnsonPCDilator response of rat mesenteric arcading arterioles to increased blood flowAm J Physiol19892576 Pt 2H1958H19652603980
- de SimoneGDevereuxRBChinaliMBestLGLeeETWeltyTKStrong Heart Study InvestigatorsAssociation of blood pressure with blood viscosity in american indians. The Strong Heart StudyHypertension200545462563015699438
- PaulBWilfredNCWoodmanRDepasqualeCPrevalence and correlates of anaemia in essential hypertensionClin Exp Pharmacol Physiol200835121461146418759858
- NishikidoNKobayashiTKashiwazakiHHematocrit correlates with blood pressure in young male office workersInd Health1999371768110052303
- BrettSERitterJMChowienczykPJDiastolic blood pressure changes during exercise positively correlate with serum cholesterol and insulin resistanceCirculation2000101661161510673252
- IraceCCaralloCScavelliFLopreteAMeranteVGnassoALack of association between systolic blood pressure and blood viscosity in normotensive healthy subjectsClin Hemorheol Microcirc2012511354122240365
- MaturanaMAIrigoyenMCSpritzerPMMenopause, estrogens, and endothelial dysfunction: current conceptsClinics (Sao Paulo)2007621778617334553
- VázquezBYVázquezMAIntagliettaMde FaireUFagrellBCabralesPHematocrit and mean arterial blood pressure in pre- and postmenopause womenVasc Health Risk Manag20095248348819554088
- de SimoneGDevereuxRBChienSAldermanMHAtlasSALaraghJHRelation of blood viscosity to demographic and physiologic variables and to cardiovascular risk factors in apparently normal adultsCirculation19908111071172297818
- HammondIWDevereuxRBAldermanMHLaraghJHRelation of blood pressure and body build to left ventricular mass in normotensive and hypertensive employed adultsJ Am Coll Cardiol198812499610043417996
- Zubieta-CallejaGRPaulevPEZubieta-CallejaLZubieta-CastilloGAltitude adaptation through hematocrit changesJ Physiol Pharmacol200758Suppl 5(Pt 2)81181818204195
- CahillERowanSCSandsMThe pathophysiological basis of chronic hypoxic pulmonary hypertension in the mouse: vasoconstrictor and structural mechanisms contribute equallyExp Physiol201297679680622366565
- HannaJMClimate, altitude, and blood pressureHum Biol199971455358210453102
- TripathyVGuptaRBlood pressure variation among Tibetans at different altitudesAnn Hum Biol200734447048317620154
- León-VelardeFSanchezJBigardAXBrunetALestyCMongeCHigh altitude tissue adaptation in Andean coots: capillarity, fibre area, fibre type and enzymatic activities of skeletal muscleJ Comp Physiol B1993163152588459054
- WolfelEESellandMAMazzeoRSReevesJTSystemic hypertension at 4,300 m is related to sympathoadrenal activityJ Appl Physiol (1985)1994764164316508045844
- RuizLPeñalozaDAltitude and hypertensionMayo Clin Proc1977527442445875468
