Abstract
Crohn’s disease is a chronic inflammatory disease that can affect any part of the gastrointestinal tract. Classically the disease has a predilection for the distal small bowel and colon and presents with dominant symptoms of abdominal pain and diarrhea. This case report describes a 38-year-old woman with Crohn’s disease who presented with odynophagia. Direct visualization of the oropharynx revealed a large serpiginous Crohn’s disease ulcer. A precipitous drop in hemoglobin prompted a series of gastroenterologic investigations that confirmed both ileal and oropharyngeal Crohn’s disease. This manuscript describes the presentation of oropharyngeal Crohn’s and reviews previous reports and management options.
Introduction
Crohn’s disease involves chronic inflammation of the mucosal tissues that may advance to fissuring ulcers, sinus tracts, submucosal fibrosis, transmural lymphoid infiltrates and serositis, affecting any part of the alimentary tract.Citation1,Citation2 The etiology of Crohn’s disease remains to be elucidated, however, it likely occurs as a consequence of luminal antigens [microbial and/or dietary] triggering an uncontrolled mucosal and systemic inflammatory response in a genetically predisposed individual.Citation3,Citation4 While the peak age of onset is between 15 and 25 years of age, individuals can be of any age at the time of disease onset. Typical symptom presentation includes abdominal cramping, diarrhea, weight loss, and anemia. The diagnosis of Crohn’s disease requires a combination of endoscopic and histological evaluations to differentiate it from other forms of chronic gastrointestinal inflammation.Citation2
Crohn’s disease is most common in the distal small bowel and colon. At the time of presentation, 80% of patients have small bowel disease (predominantly distal ileum), 50% have ileocolitis, and only 20% have disease limited to the large bowel.Citation5 Rarely does Crohn’s disease present with symptoms localized to the oropharynx or upper-gastrointestinal tract.Citation5
Case presentation
A 38-year-old female presented to her family doctor with a 2-week history of throat pain, odynophagia, and an associated 5.4 kg weight loss. She noted a history of frequent oral “canker sores”. Throat swabs were negative for infectious etiologies and there was no improvement with two separate courses of antimicrobials. There were no genital ulcers or eye symptoms noted by the patient and none on examination. When the throat pain and odynophagia progressed to the point of significantly limiting oral intake the woman was admitted to the otolaryngology specialty service for further investigation and treatment. Direct visualization of the oral pharynx revealed a large 2 cm, serpiginous ulcerating lesion proximal to the pyriform fossae. Given the fact that the patient was a one pack per day smoker, the diagnosis of a primary malignant lesion was entertained.
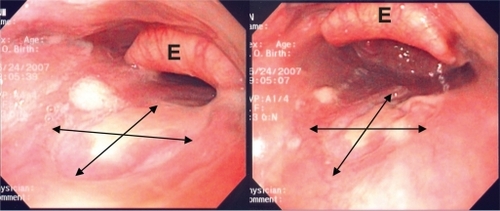
Before a biopsy of the lesion could be arranged a drop in the patient’s hemoglobin from 112 g/L to 65 g/L occurred over a 36-hour interval. The patient noted some increase in bowel frequency and bright red blood mixed with the feces. Consultation to the Gastroenterology Service was initiated and a esophago-gastro-duodenoscopy revealed a normal esophagus, stomach, and proximal duodenum with no obvious upper gastrointestinal source to account for the anemia. Colonoscopy demonstrated a normal peri-anal region, rectum, and colon; however, on intubation into the terminal ileum, there were several long, discrete deep ulcers and exudate (). Histologic analysis confirmed Crohn’s disease. With this finding of Crohn’s disease in the terminal ileum the esophago-gastro-duodenoscopy was repeated with the aim of carefully inspecting the oropharynx for evidence or oropharyngeal Crohn’s disease. A large (2 × 2 cm), irregular, non-bleeding ulcer was seen in the oropharynx, consistent in size and location with the one identified during direct visualization ( and ). Histologic analysis of the oropharyngeal ulcer confirmed Crohn’s disease. On retrospective questioning the patient recalled a 3-year history of intermittent diarrhea (5–6 bowel movements per day) with intermittent blood in the stool, and associated abdominal cramping and occasional vomiting. The patient’s mother had a history of ulcerative colitis. There was no other family history of inflammatory bowel disease.
Figure 1 Endoscopic view of the terminal ileum with evidence of large deep serpiginous mucosal ulceration (double headed arrows).
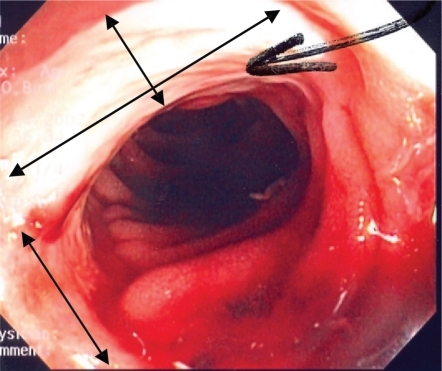
Figure 2 Endoscopic view of the oropharynx showing the 2 × 2 cm ulcer. Double-headed arrows outline the inner diameter of the ulcer. E, epiglottis.
Following the patient’s endoscopic examinations and diagnosis of Crohn’s disease, treatment was initiated with methylprednisolone 40 mg intravenously every 12 hours and azathioprine 150 mg po daily. Following 3 days of intravenous steroid treatment the patient had significantly improved, noting cessation of her diarrhea and rectal bleeding as well as marked improvement of her throat pain and odynophagia. After 5 days the patient was ingesting a regular diet and the intravenous steroid treatment was changed to oral prednisone. The woman was discharged home on a tapering dose of prednisone (initially 40 mg daily, and tapering over 16 weeks to zero) and azathioprine 150 mg daily.
The patient remained in clinical remission on maintenance azathioprine 150 mg per day for 8 months at which point she began having recurrence of throat pain and odynophagia. Symptoms of abdominal pain and diarrhea were not a feature of the relapse. Endoscopic examination revealed recurrence of the oropharyngeal ulceration. Infliximab, 5 mg/kg, was initiated at week 0 and 2. Within 6 days after the fist infusion there was almost complete resolution of the oral symptoms. Infliximab every 8 weeks as scheduled therapy and azathioprine 150 mg per day were continued as maintenance therapy.
Discussion
The first case report of oropharyngeal Crohn’s disease was described in 1969 (6). Since then, it is estimated that only 0.5% to 20% of Crohn’s disease patients will have some oropharyngeal involvement of Crohn’s disease with perhaps a higher incidence in children.Citation7,Citation8 Oral findings in Crohn’s disease are most commonly intermittent shallow aphthous ulcers, but much less commonly include mucogingivitis, mucosal tags, lip swelling, and pyostomatitis vegetans (ulceration with mucosal and gingival pustules). Large oropharyngeal ulcers, as seen in this case, are rarely described.Citation8 The differential diagnosis of oropharyngeal ulceration extends beyond inflammatory bowel diseases to include infectious (tuberculosis, toxoplasmosis, syphilis), infiltrative (sarcoid), inflammatory (Behçet’s), caustic, and neoplastic (lymphoma, squamous cell carcinoma) etiologies.Citation9
The partiality of Crohn’s disease for one region of the gastrointestinal tract versus another is not completely understood. Compromised oral mucosal integrity secondary to reduced circulating salivary IgA levels has been postulated as a pathogenic mechanism in oral Crohn’s disease.Citation1 Another separate hypothesis involves a hypersensitive cellular and/or humoral immune response to oral antigens in Crohn’s patients with altered immune regulation.Citation9
Proximal and oropharyngeal gastrointestinal tract Crohn’s disease is difficult to diagnose and carries its own prognostic and treatment implications. Thorough history-taking, direct visualization, and tissue biopsy are all important steps in establishing the diagnosis.Citation1 In this regard, a systematic evaluation of the mouth by physicians or dentists is an important step in the diagnostic process.Citation7 Gastroscopy by experienced gastroenterologists will identify oropharyngeal Crohn’s disease in only 50% of patients.Citation8 This low identification rate is attributed to the limited examination of the oro-and hypo-pharynx by endoscopists during intubation of the esophagus. Indeed, the initial gastroscopy performed in this patient did not identify the oropharyngeal ulcer. Only after the colonos-copy had identified terminal ileal Crohn’s disease did a repeat gastroscopy and careful visualization of the oropharyngeal region confirm the Crohn’s oropharyngeal ulcer.
Conflicting data exists on the frequency of granulomas seen on biopsy in oral Crohn’s disease lesions. Ramzan et al found the proportion of oral lesions attributable to Crohn’s disease having granulomas on biopsy to be less than 10%.Citation10 Conversely, Ganesh et al found 75% of patients in their sample to have granulomas.Citation7 There were no granulomas in the biopsies obtained from this patient.
Successful treatment of oropharyngeal Crohn’s disease has been achieved, in isolated case studies by laser therapy and nutrition, however, pharmacologic therapy remains the mainstay. It is estimated that less than 25% of oropharyngeal Crohn’s disease resolve spontaneously.Citation11 In a single case report, laser therapy achieved a successful outcome in treating an isolated oral Crohn’s lesion.Citation12 A variety of pharmacologic agents have been investigated for the treatment of oral Crohn’s disease and remain the mainstay of therapy. Turchi et al illustrated the success of corticosteroid induced remission followed by mesalamine maintenance therapy with no relapse after 6 months.Citation1 Infliximab is a chimeric monoclonal antibody against tissue necrosis factor alpha (TNF-alpha) that has an established role in the initiationCitation13 and maintenanceCitation14 of remission in moderate to severe fistulizing and non-fistulizing Crohn’s disease.Citation15,Citation16 Oral Crohn’s lesions resistant to mesalamine and corticosteroid therapy have been described to respond to infliximab therapy with significant symptom improvement seen with the initial infusion.Citation11,Citation17 Thalidomide is an oral immunomodulatory and anti-angiogenic medication that has been shown to completely resolve oral granulomatous lesions, including oral Crohn’s disease in cases refractory to other immunomodulatory agents such as azathioprine.Citation18 However, the high incidence of dose-dependent and dose-independent adverse effects has limited its use.
In summary, oropharyngeal Crohn’s disease presents a diagnostic and therapeutic challenge to clinicians. The lesions of oropharyngeal Crohn’s disease are frequently missed at the time of endoscopy, resulting in delay of diagnosis, and the associated odynophagia often leads to limited oral intake and subsequent weight loss. Indirect laryngoscopy can provide initial identification of the oral ulcerations, and in the absence of neoplasia on biopsy, a careful search for luminal Crohn’s disease should be undertaken. The oropharyngeal Crohn’s disease in this patient had an initial response to corticosteroids and azathioprine, however the response could not be maintained despite azathioprine therapy. Infliximab therapy rapidly induced and maintained a second response.
Disclosures
None of the authors have conflicts of interest to disclose.
References
- TurchiRMSorianoHRodgersGLTb or not TB:Crohn’s disease presenting with tonsillar granulomasOtolaryngol Head Neck Surg20061345283016500459
- YantissRKOdzeRDPitfalls in the interpretation of nonneoplastic mucosal biopsies in inflammatory bowel diseaseAm J Gastroenterol200710289090417324129
- BaumgartDCSandbornWJInflammatory bowel disease:clinical aspects and established and evolving therapiesLancet200736916415717499606
- FedorakRNMadsenKLProbiotics and the management of inflammatory bowel diseaseInflamm Bowel Dis2004102869915290926
- BradleyPJFerlitoADevaneyKORinaldoACrohn’s disease manifesting in the head and neckActa Otolaryngol20041242374115141749
- DudeneyTPCrohn’s disease of the mouthProc R Soc Med19696212375363108
- PittockSDrummBFlemingPThe oral cavity in Crohn’s diseaseJ Pediatr20011387677111343060
- HartySFlemingPRowlandMA prospective study of the oral manifestations of Crohn’s diseaseClin Gastroenterol Hepatol200538869116234026
- JohnsonDACattauELJHancockJEPrimary Crohn’s disease of the oropharynxEar Nose Throat J19856453464064986
- RamzanNNLeightonJAHeighRIShapiroMSClinical significance of granuloma in Crohn’s diseaseInflamm Bowel Dis200281687311979136
- MahadevanUSandbornWJInfliximab for the treatment of orofacial Crohn’s diseaseInflamm Bowel Dis20017384211233659
- GillerJPVinciguerraMHellerAKunkenFRKahnETreatment of gingival Crohn’s disease with laser therapyNY State Dent J199763325 [PMID:9188263].
- TarganSRHanauerSBvan DeventerSJMayerLPresentDHBraakmanTDeWoodyKLSchaibleTFRutgeertsPJA short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn’s disease. Crohn’s Disease cA2 Study GroupN Engl J Med1997151029359321530
- HanauerSBFeaganBGLichtensteinGRMayerLFSchreiberSColombelJFMaintenance infliximab for Crohn’s disease:the ACCENT I randomised trialLancet200235993171541912047962
- CardosoHNunesACCarneiroFTavarela VelosoFSuccessful infliximab therapy for oral Crohn’s diseaseInflamm Bowel Dis2006123378 [PMID:16633058].16633058
- StainesKSGreenRFelixDHThe management of fistulizing oral Crohn’s disease with infliximabJ Oral Pathol Med200736444617617840
- OttavianiFSchindlerACapaccioPPetroneMBianchiPGNew therapy for orolaryngeal manifestations of Crohn’s diseaseAnn Otol Rhinol Laryngol200311237912537056
- HegartyAHodgsonTPorterSThalidomide for the treatment of recalcitrant oral Crohn’s disease and orofacial granulomatosisOral Surg Oral Med Oral Pathol Oral Radiol Endod2003955768512738949