Abstract
Objective:
To evaluate the predictive values of the expression of factor VIII, CD-34, p53, bcl-2, and DNA ploidy regarding the response to chemoradiation of squamous cell carcinoma of the esophagus.
Design:
Retrospective analysis of pretreatment biopsies with immunohistochemistry and flow cytometry. The results were correlated to tumor response (complete vs. noncomplete) following chemoradiation with three cycles of 5-FU and cisplatin combined with 40–64 Gy of radiation.
Subjects:
44 consecutive patients with squamous cell carcinoma of the esophagus treated with chemoradiation with a curative intent from 1992–2000.
Main outcome measures:
Treatment response.
Results:
No correlations were found between the expressions of p53, bcl-2, or DNA ploidy and tumor response to chemoradiation. A positive correlation was found between factor VIII expression and a complete tumor response (p = 0.0357). However the other marker for angiogenesis, CD-34, showed a negative correlation (p = 0.0493). Both markers indicate blood vessel density meaning that, in this study, many vessels indicated a favorable response if measured with factor VIII, but a poor response if measured with CD-34.
Conclusion:
It is not possible to predict tumor response to our chemoradiation protocol through the analysis of pretreatment expression of p53, bcl-2 or DNA ploidy in biopsy specimens. In spite of significant correlations between complete tumor responses and the expressions of the markers for angiogenesis this significance may be questionable since one of the two markers, factor VIII had a positive and the other,CD-34, a negative correlation to tumor response.
Introduction
Esophageal cancer has a well known poor prognosis.Citation1–Citation3 The 5-year survival has been in the order of 5%–10% following surgery or radiotherapy. These poor results have stimulated the development of new treatment techniques including more radical surgical procedures.Citation4,Citation5
However, at least in the Western countries, esophageal cancer is mostly diagnosed at a late disseminated stage. Then locoregional treatments such as surgery and/or radiotherapy are insufficient to cure the patients. In this situation it is rational to include a systemic treatment, ie, chemotherapy into the protocols.
Results of chemotherapy have been poor until the last decade when a number of different series of concomitant chemoradiotherapy, mostly including cisplatinum, have shown promising results with complete response rates above 40%.Citation6–Citation10.
However these chemoradiotherapy protocols, often in neoadjuvant settings, are followed by rather high morbidity and treatment-related mortality.Citation11 It would therefore be of interest to be able to predict which patient is a responder and which is not before the administration of the treatment. It would then be possible to exclude nonresponders from a potentially harmful treatment.
In this study microbiologic markers have been evaluated in two groups of patients, responders and nonresponders, treated according to the same chemoradiotherapy protocol.
Angioneogenesis in tumor tissue has been studied, since it is known that good oxygenation of tumor cells enhances the radiosensitivity and improves the delivery of cytotoxic agents.Citation12,Citation13 A high microvessel density with an improved circulation enhances this crucial oxygenation. It is however also known that angioneogenesis may be a limiting factor regarding tumor growth and possibly also regarding the tendency to metastasize.Citation14,Citation15 Accordingly a pronounced angioneogenesis may both act as an adjunct to chemoradiotherapy and at the same time be a marker of poor prognosis regarding tumor biology. We have investigated pretreatment microvessel density within tumors expressed through factor VIII and CD-34 and correlated the results to tumor response after chemoradiation.
Apoptosis, or programmed cell death, is a physiological mechanism regulating homeostasis in both normal and tumor tissue by the elimination of unnecessary cells.Citation16 Failure of tumor cells to undergo apoptosis can result in uncontrolled accumulation of cells. It is known that apoptosis can be induced by chemotherapuetic agents and radiationCitation17 and by oncogenes such as bcl-2 and p53.Citation18.Citation19 Like a neoplasm with fully established tumor cell necrosis, a carcinoma with a high incidence of apoptotic nuclei of the neoplastic parenchymal cell carcinoma is looked upon as a neoplasm with a bad prognosis for the patient, requiring particular types of therapy. P53 expression has been correlated to survival in carcinoma of the breast,Citation20 colon,Citation21 stomach,Citation22 and lung,Citation23 while the prognostic value of p53 in esophageal cancer remains more uncertain.Citation24,Citation25 Mutations of the tumor suppression antigen p53 are among the most commonly detected genetic abnormalities in human neoplasia in general and in squamous cell carcinomas in particular. The results of an immunohistochemistry (IHC) analysis of p53 can govern both the therapy and the prognosis of the patient′s carcinoma. It is however a rather well established fact that the simple finding of an IHC overexpression of some kind, does not yet in itself become a good predictor of the subsequent course of the patient’s neoplastic disease. It is neither decisive for the choice of therapy. We have studied the correlation between tumor response and bcl-2 and p53.
DNA ploidy is known to indicate prognosis in squamous cell carcinoma of the esophagus through the detection of aneuploid peaks in flow cytometric analysis.Citation26 We have investigated the pretreatment DNA ploidy and then correlated this analysis to the response to chemoradiation therapy.
Patients and methods
Patients
Forty-four patients were recruited from a consecutive group of patients, who had received planned preoperative or fulldose chemoradiation for squamous cell carcinoma of the esophagus during 1992–2000. The patients were separated into two groups depending on response to oncological therapy (complete response [CR] vs non-CR). See for details.
Table 1 Patient and tumor characteristics
Eligibility criteria for the study included histologically confirmed squamous cell carcinoma of the esophagus without signs of distant metastases, ie tumor stage T1-4, N0-1, M0 according to the International Union against Cancer.Citation27 The patients had to have a functional performance status of ≤2 according to the World Health Organization (WHO) classification and they should not suffer from any other condition that could be worsened by the planned treatment such as serious heart (ie, heart failure or angina) or kidney disorders. Hematological and renal function test parameters had to be normal (leucocytes ≥3.0 × 109/L, platelets ≥100 × 109/L, cr-EDTA clearence >65 mL/min). There should not be a history of other squamous cell malignancy prior to entry nor should there be any history of any type of malignant tumor during the last five years before inclusion. Before entry into the study the patients were investigated with spirometry, electrocardiogram, barium esophagogram, chest X-ray, computed tomography (CT) scan of the chest and upper abdomen, abdominal and endoscopic ultrasound (EUS), esophagoscopy with biopsies, and finally bronchoscopy, if the tumor was located at or above the carina. Patients with intraluminal airway growth were excluded. The results of these pretreatment investigations were evaluated by a surgeon and an oncologist to find out if the patients were fit for the planned treatment.
Surgical treatment
Before starting the treatment the patients were stratified as primarily resectable or unresectable by the surgeon and the oncologist. This stratification was repeated after the primary chemoradiation treatment, when a new CT scan and EUS (if available) were performed. The standard surgical technique was an Ivor Lewis procedure with a gastric pull-up or with a colon interponate as the esophageal substitute.
Oncological treatment
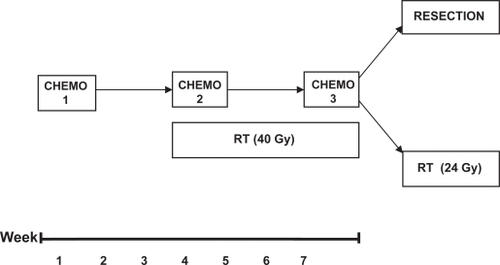
The protocolCitation6 included three five-day courses of cisplatinum (100 mg/m2 on the first day of each course) and 5-fluorouracil (a continuous 120-hour infusion on day 1 through 5 of each course with 750 mg/m2 administered on each day of treatment) with a two-week rest between the treatments. Radiation was administered daily on weekdays from the first day of the second course of chemotherapy up to a preoperative dose of 40 Gy or through a full dose treatment of 64 Gy. The radiation treatment (preoperative or full dose) was decided on before the treatment started. The daily fractionation was 2 Gy (see ).
When no tumors were found postoperatively after histopathological examination the responses were classified as pathological CR. Patients not operated on were evaluated with clinical methods (X-ray of the esophagus, endoscopy, CT scans and, when available, EUS). Responses were classified as clinically CR, when no manifestations of malignancy could be found with clinical techniques. All other tumors, not classified as complete responses, were grouped together as incomplete responses (non-CR) regardless of degree of response.
Biopsy procedure
The biopsies obtained during endoscopies were paraffin-embedded and formaldehyde-fixed. These procedures were performed at the time of diagnosis. Hence no patients had received any anticancer treatment prior to the biopsy procedure.
A minimum of three macroscopically representative biopsies were sampled from gross tumor tissue through an endoscope (various Olympus video gastroscopes) with biopsy graspers (Olympus FB-24K®).
Laboratory methods
Factor VIII, CD-34, p53 and bcl-2 were all analyzed according to standard immunohisto-chemistry methods utilizing the avidin biotinylated immunoperoxidase-staining technique (Hsu 28). The reason why factor VIII and CD34 were chosen as IHC markers for angiogenesis was the fact that among the antisera raised against endothelial cells available in our laboratory, these were found to be those which in pilot studies showed themselves to give the histotechnically most optimal results.
A standardized procedure for cutting out specimens from the large resection material for subsequent light microscopy was applied. Particular attention was paid to visualize the free borders of the specimen. This was performed by marking them with India ink.
The sections were deparaffinated in xylene and rehydrated in ethanol and distilled water. Antigen retrieval was performed through pressure boiling for two minutes in 10 mM citrate buffer (factor VIII, CD-34, p-53, and bcl-2) and through digestion with proteinase K (DAKO, code 2019) (factor VIII). They were then immunostained (see for primary antibodies) and endogenous peroxidase activity was blocked with hydrogen peroxide before exposure to biotinylated secondary linking antibody, avidin-biotinylated enzyme complex, diaminobenzidine (DAB) as chromogen and hematoxylin as counterstain.
Table 2 Primary antibodies used during immunohistochemistry
Two independent experienced histopathologists (SF, UF) then evaluated the specimens. They did not know the clinical outcome of the individual patients.
The evaluations were performed in light microscopy in 400 × magnification fields. All tumor tissue was evaluated, excluding the stroma. An average figure from each section was calculated.
Factor VIII
The number of microvessels in each field was calculated. Stains were counted as microvessels when they were not associated with the muscular bundles of arteries or arteriole. A lumen was not necessary for a positive count. Vessels in and along the borders of tumor tissue were counted.
CD-34
CD-34 was calculated in the same way as factor VIII.
Bcl-2
One or more stained cells in a biopsy were regarded as a positive case. The evaluation was performed at both 100 × and 400 × magnification.
P-53
More than 50% positively stained cells out of the total were regarded as a positive case. The evaluation was performed at both 100 × and 400 × magnification.
DNA
The utilized procedure in the analysis of DNA-ploidy was flow cytometry. This analysis was only performed with specimens from the first consecutive 28 patients due to technical difficulties.
Statistical considerations
The continuing variables have been analyzed with logistic regression and divided into different categories according to different value cut-offs. The category variables have been analyzed in cross tables with Fisher’s test and the Chi-squared test.
Ethical considerations
The study was approved by the ethics committee at the Karolinska Institute in Stockholm. All living patients gave their informed consent to take part in the study.
Results
Oncological therapy
Twenty-three patients had complete responses (the CR group), while the other 21 patients (the non-CR group) showed poorer responses (partial responses or less). See for details. In accordance with other studiesCitation6 response to chemoradiation was correlated to initial tumor stage (p < 0.05).
Table 3 Responses and survival following therapy
All 44 patients received ≥40 Gy of radiation and three courses of chemotherapy. Four patients, two from each group, received full dose radiation.
Surgery
Thirty-five of the 44 patients were operated on (80%). Five patients did not receive any operation due to a high location in the esophagus. High tumors were not resected to avoid mutilating laryngectomies. Two patients were not operated on because of local overgrowth on adjacent organs. Finally two patients, initially planned for surgery, were not operated due to poor health following oncologic treatment. In the non-CR group of patients three cases of unexpected advanced tumor growth was found during operation and therefore only explorations were performed. Eighteen of the 23 patients (78%) in the CR group had resections compared to 14 of 21 patients (67%) in the non-CR group. See for details.
Table 4 Delivered treatment
Angiogenetic markers in CR vs non-CR groups
Factor VIII
A statistically significant difference was found between responders and nonresponders regarding vessel density in tumor tissue expressed as mean numbers of vessels stained for factor VIII/field of vision (p = 0.0357).
CD-34
A weak negative correlation (p = 0.0493) was found when the vessel density was calculated with the CD-34 method as opposed to the results of the factor VIII evaluations.
Apoptosis
Bcl-2
Seven patients in the CR group had positive stains for bcl-2 as did five patients in the non-CR group. All other patients were negative. As a consequence no significant difference was found between the two groups regarding bcl expression.
P-53
No significant differences were found between responders and nonresponders regarding p-53 expression (p = 0.895).
DNA-ploidy
DNA
Most of the 28 analyzed tumors were aneuploid (n = 25). Two tumors in the CR group (n = 14) of patients were tetraploid, as was one of the tumors in the non-CR group (n = 14). Hence no difference in DNA-ploidy was found between the groups.
Discussion
Tumor angiogenesis has been shown to relate to survival in a number of different tumors including squamous cell carcinoma of the esophagus.Citation29 The same relation has also been shown regarding the expression of p-53Citation25 and apoptosis through bcl-2.Citation30
A few investigators have adressed the same issue as in our study, ie, to find predictors of tumor response to demanding oncological therapy. The rationale is to make it possible to avoid the often serious side effects of a demanding and, in the case of the non responders, ineffective treatment.
Imdahl and colleaguesCitation31 found a better response to chemoradiation in tumors with a high proliferation rate determined by MIB-1 immunohistology, but no such correlation was found in their series investigating tumor response and apoptosis. Seitz and colleaguesCitation32 found correlations between clinical response (endoscopy with biopsies two to three weeks after chemoradiation) and lack of p53 overexpression. DNA ploidy (flow cytometry) and cell proliferation (Ki67) was not correlated to tumor response. Ressiot and colleagues, on the other hand, found overexpression of Ki67 to be an independent factor for complete response in esophageal cancer.Citation33 Sarbia and colleaguesCitation34 found that the expression of cyklin D1 was correlated to a poor response to radiochemotherapy but this correlation was not found in overall survival. The same authors have also investigated bcl-2 and p53 in radiochemotherapy treated patients without finding a significant correlation to tumor response.Citation35
Shimada and colleagues found a correlation between low angiogenetic activity, expressed through low serum vascular endothelial growth factor levels, and a good tumor response in squamous cell carcinoma of the esophagus.Citation36 This finding was supported by the study by Imdahl.Citation37
COX-2 displays antiapoptotic functions related to angiogenesis or blocking of bcl-2 action. Takatori and colleagues found that COX-2 mRNA expression in tumor biopsies was closely related to chemoradiotherapy effectiveness in esophageal squamous cell carcinoma.Citation38
In our study correlations between angiogenesis and tumor response were found. There were no correlations between apoptosis (bcl-2), p-53 expression or DNA ploidy and the response to chemoradiation. Shimada did not find any correlation between p-53 and tumor response either,Citation39 but these results were challenged by earlier studies by RibieroCitation40 and Yang.Citation41 One major problem with the results of our study was that the two markers of angiogenesis, factor VIII and CD-34 were correlated to response, but not in the same way. Factor VIII had a significant positive correlation at the 5% level with a p-value of 0.0357 whereas CD-34 had a slight significant negative correlation with a p-value of 0.0493. One explanation for this lack of correlation may be the fact that VIII also is known to be a marker of lymphangiogenesis.
Squamous cell carcinomas of the esophagus have an intratumoral heterogeneity that may influence the representativeness of the biopsies harvested. It has been shown that heterogeneity is less pronounced in different parts of the same tumor compared with samples from different tumors.Citation42 It is therefore unlikely that our method of sampling can explain the results.
The method of pressure cooking to achieve antigen retrieval during the IHC process is sensible and it has to be performed with caution. However the fact that both positive and negative stains were found after pressure cooking and that the controls utilized were colored as expected supports the accuracy of the method.
Finally it has to be noted that the group of patients was relatively small which may influence the results. However it must be concluded that no major differences can be found regarding apoptosis, p-53 or DNA ploidy if a CR group is compared with a non-CR group in chemoradiation of squamous cell carcinoma of the esophagus. Neither can it be concluded that angiogenesis is a predictor of therapeutic success with the chemoradiation protocol used, since the two markers of angiogenesis show diverse correlations. An unknown procedure related, or biologically determined factor may be responsible for this. It has however to be noted that other studies, as demonstrated above, do not show unequivocal results.
Disclosure
The authors report no conflicts of interest.
References
- EarlamRCunha-MeloJREsophageal squamous cell carcinoma I: A critical review of surgeryBr J Surg1980673813906155968
- EarlamRCunha-MeloJREsophageal squamous cell carcinoma: II. A critical review of radiotherapyBr J Surg198067451461
- MüllerJMErasmiHSteltznerMZierenUPichlmaierHSurgical therapy of esophageal carcinomaBr J Surg1990778458572203505
- LerutTDeLeynPCoosemansWVan RaemdonckDScheysILe SaffreESurgical strategies in esophageal carcinoma with emphasis on radical lymphadenectomyAnn Surg199221655835901444650
- AkiyamaHTsurumaruMUdagawaHKajiyamaYRadical lymph node dissection for cancer of the thoracic esophagusAnn Surg199422033643728092902
- StockeldDTennvallJWageniusGA Swedish study of chemoradiation in squamous cell carcinoma of the esophagusActa Oncol200140556657311669327
- FagerbergJStockeldDLewensohnRCombined treatment modalities in esophageal cancer. Should chemotherapy be included?Acta Oncol19943344394508018378
- ForastiereAHeitmillerRLeeD-JIntensive chemoradiation followed by esophagectomy for squamous cell and adenocarcinoma of the esophagusCancer J Sci Am199731441529161779
- ForastiereAAOrringerMBPerez-TamayoCConcurrent chemotherapy and radiation therapy followed by transhiatal esophagectomy for local-regional cancer of the esophagusJ Clin Oncol199081191272295902
- StahlMWilkeHFinkUCombined preoperative chemotherapy and radiotherapy in patients with locally advanced esophageal cancer: Interim analysis of a phase II trialJ Clin Oncol1996148298378622031
- GanemGDubrayBRaoulYConcomitant chemoradiotherapy followed, where feasible, by surgery for cancer of the esophagusJ Clin Oncol19971527017119053496
- TannockIFOxygen diffusion and the distribution of cellular radio-sensitivity in tumoursBr J Radiol1972455155245067983
- VaupelPKalinowskiFOkunieffPBlood flow, oxygen and nutrient supply and metabolic microenvironment of human tumours: a reviewCancer Res198949644964652684393
- FolkmanJWhat is the evidence that tumors are angiogenesis dependent?J Natl Cancer Inst199082461688381
- LiottaLKleinermannJSaidelGQuantitative relationships of intravascular tumor cells, tumor vessels, and pulmonary metastases following tumor implantationCancer Res19743499710044841969
- WyllieAHKerrJFRCurrierARCell death: the significance of apoptosisInt Rev Cytol1980682513067014501
- IjiriKPottenCSResponse of intestinal cells of differing topographical and hierarchical status to ten cytotoxic drugs and five sources of radiationBr J Cancer1983471751856824565
- HockenberyDNunesGMilliamCSchreiberRDKorsmeyerSJBcl-2 is an inner mitochondrial membrane protein that blocks programmed cell deathNature19903483343482250705
- FujiwaraTGrimmEAMukhopadhyayTCaiDWOwen-SchaubLBRothJAA retroviral wild-type p53 expression vector penetrates human lung cancer spheroids and inhibits growth by inducing apoptosisCancer Res199353412941338395976
- ThorADMooreDHIIEdgertonSMAccumulation of p53 tumor supressor gene protein; an independent marker of prognosis in breast cancersJ Natl Cancer Inst1992848458551317462
- SunXFCarstensenJMZhangHPrognostic significance of cytoplasmatic p53 oncoprotein in colorectal adenocarcinomaLancet1992340136913731360088
- MartinHMFilipeMIMorrisRWLaneDPSilvestreFP53 expression and prognosis in gastric carcinomaInt J Cancer1992508598621555884
- QuinlanDCDavidsonAGSummersCLWardenHEDoshiHMAccumulation of p53 protein correlates with a poor prognosis in human lung cancerCancer Res199252482848311324796
- SarbiaMPorschenRBorchardFHorstmannOWillersRGabbertHEP53 protein expression and prognosis in squamous cell carcinoma of the esophagusCancer1994748221822237922972
- MongesGMSeitzJFGiovanniMFGouvernetJMTorrenteMAHassounJAPrognostic value of p53 protein expression in squamous cell carcinoma of the esophagusCancer Detect Prev199620163678907205
- DokiYShiozakiHTaharaHPrognostic value of DNA ploidy in squamous cell carcinoma of esophagus. Analyzed with improved flow cytometric measurementCancer1993726181318188364859
- HermanekDSobinLHUICC: TNM classification of malignant tumors4th edRev 2BerlinSpringer Verlag1992
- HsuSMRaineLFangerHUse of avidin-biotin-peroxidase complex (ABC) in immunoperoxidase techniques. A comparison between ABC and unlabeled antibody (PAP) proceduresJ Histochem Cytochem1981295775806166661
- TanigawaNMatsumuraMAmayaHKitaokaAShimomatsuyaTLuCMuraokaRTanakaTTumor vascularity correlates with the prognosis of patients with esophageal squamous cell carcinomaCancer19977922202259010094
- ShibataHMatsubaraOApoptosis as an independent prognostic indicator in squamous cell carcinoma of the esophagusPathol Int200151749850311472561
- ImdahlAJenknerJIhlingCRuckauerKFarthmannEHIs MIB-1 proliferation index a predictor for response to neoadjuvant therapy in patients with esophageal cancer?Am J Surg2000179651452011004343
- SeitzJFPerrierHMongesGGiovanniMGouvernetJMultivariate analysis of the prognostic and predictive factors of response to concomitant radiochemotherapy in epidermoid cancers of the esophagus. Value of immunodetection of protein p53Gastroenterol Clin Biol19951954654747589997
- RessiotEDahanLLiprandiAPredictive factors of the response to chemoradiotherapy in esophageal cancerGastroenterol Clin Biol2008326–756757718555630
- SarbiaMStahlMFinkUPrognostic significance of cyklin D1 in esophageal squamous cell carcinoma patients treated with surgery alone or combined therapy modalitiesInt J Cancer1999 1984186919988238
- SarbiaMStahlMFinkUWillersRSeeberSGabbertHEExpression of apoptosis-regulating proteins and outcome of esophageal cancer patients treated by combined therapy modalitiesClin Cancer Res1998412299129979865911
- ShimadaHTakedaANabeyaYClinical significance of serum vascular endothelial growth factor in esophageal squamous cell carcinomaCancer200192366366911505413
- ImdahlABognarGSchulte-MontingJPredictive factors for response to neoadjuvant therapy in patients with oesophageal cancerEur J Cardiothoracic Surg200221657663
- TakatoriHNatsugoeSOkomuraHMatsumotoMIshigamiSOwakiTAikouTPredictive value of COX-2 for the effect of chemoradiotherapy on esophageal squamous cell carcinomaOncol Rep200513469770115756444
- ShimadaHHoshinoTOkazumiSExpression of angiogenetic factors predict response to chemoradiotherapy and prognosis of oesophageal squamous cell carcinomaBr J Cancer20028655255711870536
- RibieroUJrFinkelsteinSDSafatle-RibieroAVP53 sequence analysis predicts treatment response and outcome of patients with esophageal carcinomaCancer1998837189655287
- YangBRiceTWAdelsteinDJRybickiLAGoldblumJROver-expression of p53 protein associates decreased response to chemoradiotherapy in patients with esophageal carcinomaMod Pathol19991225125610102609
- PorschenRClassenSPiontekMBorchardFVascularization of carcinomas of the esophagus and its correlation with tumor proliferationCancer Res1994545875918275498