Abstract
Overactive bladder (OAB) is a prevalent and costly condition that can affect any age group. Typical symptoms include urinary urgency, frequency, incontinence and nocturia. OAB occurs as a result of abnormal contractions of the bladder detrusor muscle caused by the stimulation of certain muscarinic receptors. Therefore, antimuscarinic agents have long been considered the mainstay of pharmacologic treatment for OAB. Currently, there are five such agents approved for the management of OAB in the United States: oxybutynin, tolterodine, trospium, solifenacin and darifenacin. This article summarizes the efficacy, contraindications, precautions, dosing and common side effects of these agents. All available clinical trials on trospium, solifenacin and darifenacin were reviewed to determine its place in therapy.
Introduction
Overactive bladder (OAB) is a clinical condition characterized by urinary urgency with or without incontinence, urinary frequency and nocturia (CitationAbrams 2002; CitationOuslander 2004). Patients with OAB typically present with symptoms of a sudden and compelling need to urinate which is difficult to defer (urgency), involuntary leakage of urine with feelings of urgency (urge urinary incontinence), frequency (≥8 micturitions in 24 hours) and nocturia (≥ one awakening per night to void) (CitationHerbison 2003). In addition, patients with OAB tend to display poor health status, activity restriction, social isolation, depressive symptoms and decreased quality of life (CitationHerbison 2003; CitationStewart 2003; CitationOuslander 2004; CitationChu 2006 and CitationStaskin 2006). OAB affects approximately 17% of the population in the United States. Although incidence increases with advanced age, OAB may affect individuals of all age groups (CitationStewart 2003). In 2000, the direct and indirect expenses associated with OAB were about $12 billion. The burden of diagnosis and treatment contributed to only 0.6% ($78 million) and 23% ($2.8 billion) of the total costs, respectively (CitationHu 2003).
OAB occurs as a result of abnormal and involuntary contractions of the detrusor muscle in the bladder, which is embedded by muscarinic receptors (M2 and M3 subtypes). Stimulation of M2 and M3 receptors by acetylcholine causes bladder contractions that leads to urination (CitationChu 2006 and CitationErdem 2006). Normally, the detrusor muscle remains at rest as the bladder is filled by urine (filling phase). However, it contracts during the filling phase in patients with OAB. Therefore, muscarinic receptor antagonists (antimuscarinic agents) are considered the mainstay of pharmacologic treatment for OAB (CitationErdem 2006).
Pharmacologic options
Muscarinic receptor antagonists inhibit the stimulation of the detrusor muscle by acetylcholine. Unfortunately, these agents are associated with undesirable anticholinergic adverse effects such as dry mouth, constipation, sedation, impaired cognitive function, tachycardia and blurred vision (CitationErdem 2006). In addition, their use is contraindicated in patients with narrow-angle glaucoma, urinary retention and gastric retention. These medications should be given with caution to the elderly, particularly those with gastroesophageal reflux (GERD), constipation, or impaired cognitive function. It is also imperative to monitor patient drug regimens for polypharmacy, potential drug interactions and other drug-related problems (CitationOuslander 2002 and CitationErdem 2006).
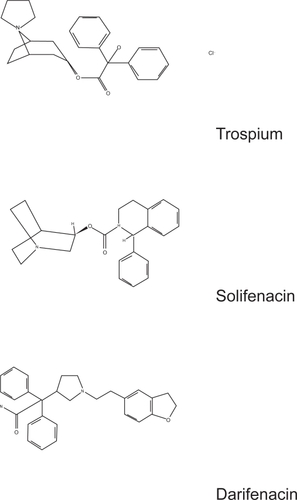
Older antimuscarinic agents used for the management of OAB are oral oxybutynin (Ditropan® and Ditropan XL®, Ortho-McNeil), transdermal oxybutynin (Oxytrol®, Watson Pharmaceuticals) and oral tolterodine (Detrol® and Detrol LA®, Pfizer). In 2004, the United States Food and Drug Administration (FDA) approved three additional antimuscarinic agents for the management of OAB: trospium (Sanctura®, Esprit/Indevus), solifenacin (VESIcare®, Yamanouchi/GlaxoSmithKline), and darifenacin (Enablex®, Novartis).
Oxybutynin and tolterodine
Oxybutynin is a relatively nonselective antimuscarinic agent which has been used for the management of OAB for over 30 years (CitationProduct Information 2004a; CitationStaskin 2006). Three formulations are available: an immediate-release (IR) tablet taken twice daily (Ditropan®, Ortho-McNeil), an extended-release (ER) tablet taken once daily (Ditropan XL®, Ortho-McNeil), and a transdermal patch applied twice weekly (Oxytrol®, Watson Pharmaceuticals) (CitationAbramovicz et al 2001, CitationAbramovicz et al 2003).
Tolterodine is a competitive muscarinic receptor antagonist which gained FDA approval for the treatment of OAB in 1998. Two formulations are available: an IR capsule taken twice daily (Detrol®, Pfizer) and an ER capsule taken once daily (Detrol LA®, Pfizer).
Oxybutynin and tolterodine have been commonly associated with adverse effects such as dry mouth, constipation, headache, dyspepsia, and dry eyes. Cognitive impairment, tachycardia and urinary retention may also occur. (CitationAbramovicz et al 2001, CitationAbramovicz et al 2003). The ER formulations of these agents have shown to be better tolerated, particularly with respect to dry mouth, and more effective than the respective IR- formulations.
Oxybutynin and tolterodine have demonstrated their efficacy in the management of OAB in multiple placebo-controlled studies (CitationAbramovicz et al 2003; CitationProduct Information 2004a, Citation2005). Here we summarize four major trials that directly compare these two agents.
The Overactive Bladder: Judging Effective Control and Treatment (OBJECT) study was a prospective, randomized, double-blind, parallel-group study that compared the efficacy and tolerability of oxybutynin-ER (10 mg once daily) to tolterodine-IR (2 mg twice daily). A total of 378 patients were treated with one of the agents for 12 weeks. About 88% (332 patients) completed the study. Results showed that oxybutynin-ER was significantly more effective than tolterodine-IR in weekly urge incontinence (p = 0.03), total incontinence (p = 0.02) and micturition frequency episodes (p = 0.02). However, both agents significantly improved symptoms of OAB from baseline as evaluated by the 3 outcomes measures (p < 0.001). Adverse events were similar among all patients, with dry mouth being reported most commonly (28.1% oxybutynin-ER group, 33.2% tolterodine-IR group) (CitationAppell et al 2001).
The Overactive Bladder: Performance of Extended-Release Agents (OPERA) trial was a 12-week double-blind study which randomized 790 women with OAB to receive either oxybutynin-ER 10 mg once daily or tolterodine-ER 4 mg once daily. At 12 weeks, results showed similar improvements in weekly urge urinary incontinence for both groups as well as a significantly greater reduction in micturition frequency in the oxybutynin-ER group (p = 0.003). A greater percentage of women in the oxybutynin-ER group reported no episodes of urinary incontinence as compared to those in the tolterodine-ER group (23% vs 16.8%, p = 0.03). Tolerability was similar among all women, with the exception of dry mouth which was more commonly reported in the oxybutynin-ER group (p = 0.02) (CitationKiokno et al 2003).
The Antimuscarinic Clinical Effectiveness Trial (ACET) consisted of two identically designed open-label trials that randomized 1,289 participants with OAB to receive tolterodine-ER 2 mg or 4 mg once daily, or oxybutynin-ER 5 mg or 10 mg once daily for 8 weeks. At the end of the trial, more patients in the tolterodine-ER groups reported an improvement in their bladder condition (60% tolterodine-ER 2 mg group, 70% tolterodine-ER 4 mg group, 59% oxybutynin-ER 5 mg group, and 60% oxybutynin-ER 10 mg group; p < 0.01 vs oxybutynin-ER 10 mg). Furthermore, the response to therapy was greater in patients whose perception of bladder symptoms were moderate to severe at the beginning of the trial. In terms of adverse effects, dose-dependent dry mouth was most commonly reported in both groups, but a lower severity was reported in the tolterodine-ER group (CitationSussman et al 2002).
Another study compared the efficacy and safety of the transdermal oxybutynin to oral tolterodine-ER and placebo in the treatment of OAB. This 12-week, double-blind study randomized 361 patients to receive twice weekly transdermal oxybutynin (3.9 mg/day), tolterodine-ER 4 mg once daily, or placebo after withdrawal of previous treatments. At the end of the study, significant reductions in the number of daily incontinence episodes (median change of −3 in the transdermal oxybutynin group, and −3 in the tolterodine-ER group vs −2 in the placebo group; p < 0.05), increases in the average void volume (median change of 24 mL and 29 mL vs 5.5 mL; p < 0.01), and improved quality of life based on questionnaire answers were observed. The most commonly reported adverse effects in the transdermal oxybutynin group were application site pruritus (14% vs 4% placebo) and erythema (8.3% vs 1.7% placebo). The incidence of dry mouth in this groups was 4.1% as compared to 7.3% in the tolterodine-ER group and 1.7% in the placebo group (p < 0.05) (CitationDmochowski et al 2003).
Trospium
In May 2004, trospium (Sanctura®, Esprit/Indevus) gained FDA approval for the management of OAB (CitationProduct Information 2004c). Trospium is a quaternary ammonium compound that has antimuscarinic properties (). Trospium has high water solubility, low oral bioavailability and thus poor penetration into the central nervous system (CNS). These characteristics explain its lesser pronounced CNS side effects when compared to oxybutynin, a tertiary amine (CitationTodorova et al 2001). compares its pharmacokinetics to that of other agents for the management of OAB. The recommended dose is 20 mg twice daily at least 1 hour before meals or administered on an empty stomach. The dosage should be reduced to 20 mg once daily in patients with creatinine clearance (CrCl) <30 mL/min or patients ≥75 years of age (CitationProduct Information 2004c).
Table 1 Pharmacokinetics of antimuscarinic agents approved for overactive bladder
The efficacy of trospium was evaluated in two multicenter, double-blind, randomized, placebo-controlled, 12-week studies (CitationProduct Information 2004c; CitationZinner et al 2004; CitationRudy et al 2006a). Entry criteria required that patients have urge or mixed incontinence (with a predominance of urge), urge incontinence episodes of ≥7 per week, and >70 micturitions per week. The efficacy outcomes included improvement in urinary frequency, urge incontinence and urinary void volume. Of the 591 patients who received trospium, 249 (42%) were ≥65 years of age and 89 (15%) were ≥75 years of age (CitationProduct Information 2004c).
In one study, 262 patients received trospium 20 mg twice daily and 261 patients received placebo for 12 weeks () (CitationZinner et al 2004). The majority of patients were Caucasian (85%) and female (74%) ranging in age between 21 and 90 years. The mean change from baseline in urinary frequency was −1.3 in the patients who received placebo and −2.4 in those who received trospium (p < 0.001). The mean change from baseline in urge incontinence episodes per week was −13.9 for the placebo group and −15.4 for the trospium group (p = 0.012). The mean change from baseline in urinary void volume was +7.7 mL in patients who received placebo and +32.1 mL in those who received trospium (p <0.001). About 8.8% of those in trospium group and 5.7% of placebo group discontinued from the study due to adverse events.
Table 2 Efficacy of trospium in the management of overactive bladder (CitationProduct Information 2004c)
In another study, a total of 329 patients received trospium 20 mg twice daily and 329 patients received placebo for 12 weeks () (CitationRudy et al 2006a). The majority of patients were Caucasian (88%) and female (82%) ranging in age between 19 and 94 years. The mean change from baseline in urinary frequency was −1.8 in the patients who received placebo and −2.7 in those who received trospium (p < 0.001). The mean change from baseline in urge incontinence episodes per week was −12.1 for the placebo group and −16.1 for the trospium group (p < 0.001). The mean change in urinary void volume was +9.4 mL in patients who received placebo and +35.6 mL in those who received trospium (p < 0.001). Efficacy of trospium could be seen within 7 days of therapy (CitationRudy et al 2006b).
Dry mouth and constipation were reported in 20% and 10% of patients in the clinical trials, respectively. Other adverse events reported were headache (4%), fatigue (2%), dyspepsia (1%), and flatulence (1%). Drug interactions may occur when coadministing trospium with drugs that are renally eliminated by active tubular secretion (digoxin, procainamide, pancuronium, morphine, vancomycin, metformin, and tenofovir). Due to competition in renal elimination, serum concentration of trospium and/or the coadministered drug can increase (CitationProduct Information 2004c).
Solifenacin
Solifenacin (VESIcare®, Yamanouchi/GlaxoSmithKline) is a muscarinic blocker for the management of OAB. It is a competitive, selective M1 and M3 receptor antagonist. In animal studies, the selectivity of solifenacin for the bladder over the salivary glands was greater than that of tolterodine, oxybutynin, darifenacin or atropine (CitationSimpson et al 2005). The starting dosage is 5 mg daily with or without food, and may be titrated to 10 mg daily as tolerated. A maximum daily dose of 5 mg is recommended in patients with CrCl <30 mL/min, with Child-Pugh B hepatic impairment, or receiving potent cytochrome P450 enzyme (CYP) 3A4 inhibitors, such as ketoconazole (CitationProduct Information 2004d).
Four 12-week, double-blind, randomized, placebo-controlled, parallel group, multicenter clinical trials evaluated the efficacy and safety of solifenacin for the management of OAB (CitationGittelman et al 2003; CitationCardozo et al 2004; CitationChapple et al 2004; CitationHaab et al 2005). All patients were required to have symptoms of OAB for ≥3 months. These studies involved 3027 patients (1811 on solifenacin and 1216 on placebo), and approximately 90% of these patients completed the studies. The majority of patients were Caucasian (93%) and female (80%) with a mean age of 58 years. At 12-weeks, the mean reduction in the number of micturitions per 24 hours was greater with solifenacin 5 mg (−2.3; p < 0.001) and solifenacin 10 mg (−2.7; p < 0.001) as compared to placebo (−1.4). The mean reduction in the number of daily incontinence episodes was greater with solifenacin 5 mg (−1.5; p < 0.001) and solifenacin 10 mg (−1.8; p < 0.001) as compared to placebo (−1.1). The mean increase in the volume voided per micturition was significantly greater with solifenacin 5 mg (+32.3 mL; p < 0.001) and solifenacin 10 mg (+42.5 mL; p < 0.001) compared to placebo (+8.5 mL). Similar safety and effectiveness were observed between older (623 patients ≥65 years and 189 patients ≥75 years) and younger patients (CitationProduct Information 2004d). reports the major results from four individual 12-week clinical trials.
Table 3 Efficacy of solifenacin in the management of overactive bladder (CitationProduct Information 2004d)
Solifenacin demonstrated similar efficacy when compared to tolterodine-IR 2 mg twice daily in a randomized, double-blind, 12-week trial (CitationChapple et al 2004). Compared to baseline, the mean change in number of urgency episodes per 24 hours were: −1.41 (placebo); −2.85 (solifenacin 5 mg); −3.07 (solifenacin 10 mg) and −2.05 (tolterodine-IR). The changes in episodes of incontinence were: −0.76 (placebo), −1.42 (solifenacin 5 mg), −1.45 (solifenacin 10 mg) and −1.14 (tolterodine-IR). The mean number of voids in 24 hours were: −1.20 (placebo), −2.19 (solifenacin 5 mg), −2.61 (solifenacin 10 mg), and −1.88 (tolterodine-IR). The mean volume voided per micturition was significantly higher with all three active treatments (48 to 41 mL). The most common side effects reported were dry mouth (solifenacin 14%–21%, tolterodine-IR 19%), constipation (solifenacin 7%–8%, tolterodine-IR 3%) and blurred vision (solifenacin 4%–6%, tolterodine-IR 2%). In another study, solifenacin showed greater efficacy to tolterodine-ER 4 mg once daily in decreasing urgency episodes, incontinence, and pad usage and increasing the volume voided per micturition (CitationChapple et al 2005). More patients in the solifenacin group reported improvements in perception of bladder symptoms.
The long-term efficacy and safety of solifenacin were demonstrated in a 52-week study (12-week phase III study followed by a 40-week open-label extension study) (CitationHaab et al 2005). Eighty-one percent of 1637 patients completed the study with 4.7% of patients discontinuing treatment due to adverse events. Improvements in OAB symptoms were noted for all patients for up to 52 weeks of treatment. Patient satisfaction with solifenacin tolerability and efficacy was high at 85% and 74%, respectively. Solifenacin also significantly improved the quality of life in patients with OAB symptoms after 12 weeks of treatment, with further improvements during long-term administration up to 1 year (CitationHaab et al 2005; CitationKelleher et al 2005).
Common side effects reported were dry mouth (11%, 28%), constipation (5%, 13%), blurred vision (4%, 5%), and dyspepsia (1%, 4%) for solifenacin 5 mg and solifenacin 10 mg, respectively (CitationProduct Information 2004d). Patients should be advised to contact their physician if they experience severe abdominal pain or become constipated for 3 or more days. Drug Interactions must be monitored between solifenacin and potent CYP3A4 inhibitors (eg, ketoconazole, itraconazole, ritonavir, nelfinavir, clarithromycin, and nefazodone).
Darifenacin
In December 2004, darifenacin (Enablex®, Novartis), another muscarinic receptor antagonist, was approved for the management of OAB (CitationProduct Information 2004b). It has a greater affinity for the bladder-specific M3 receptor. The recommended starting dose is 7.5 mg once daily with or without food. After two weeks of therapy, the dose may be increased to 15 mg once daily if tolerated. The maximum daily dose of 7.5 mg is recommended in patients with moderate hepatic impairment or in those taking potent CYP3A4 inhibitors (eg, ketoconazole, itraconazole, ritonavir, nelfinavir, clarithromycin, and nefazodone) concomitantly. Darifenacin should be administered with caution to patients with severe hepatic impairment. Patients should swallow the whole tablets without chewing, crushing or dividing.
Four randomized, double-blind, placebo-controlled, multicenter, 12-week studies evaluated the efficacy and safety of darifenacin (CitationHaab et al 2004; CitationSteers et al 2005; CitationChapple et al 2005; CitationHill et al 2006). The majority of patients were white (94%) and female (84%), with a mean age of 58 years (range: 19 to 93 years). All patients had ≥8 micturitions and ≥1 episode of urinary urgency per day and ≥5 episodes of urge urinary incontinence per week for at least six months. A significant decrease in weekly urge incontinence from baseline was observed in all four studies. Reductions in weekly incontinence were observed within the first 2 weeks in patients treated with darifenacin. reports the major results from four individual 12-week clinical trials (CitationProduct Information 2004b).
Table 4 Efficacy of darifenacin in the management of overactive bladder (CitationProduct Information 2004b)
An analysis of pooled data from three phase III, multicenter, double-blind, 12-week clinical trials (n = 1059 adults, 85% women) confirmed the efficacy and safety of darifenacin in OAB. Darifenacin reduced the number of weekly incontinence episodes by 8.8 (median) at 7.5 mg, and 10.6 (median) at 15 mg (both p < 0.01 versus placebo). Darifenacin also reduced the frequency and severity of urgency, voiding frequency, and number of significant leaks, and increased bladder capacity (CitationChapple et al 2005).
Darifenacin provides comparable efficacy with improved tolerability when compared to oxybutynin. A double-blind study randomized 76 adults with OAB to receive 2 weeks each of darifenacin 15 and 30 mg once daily, oxybutynin 5 mg three times daily and placebo, in random sequence at 10-day intervals. Darifenacin and oxybutynin significantly reduced incontinence episodes, and the number/severity of urgency episodes (all p <0.05 vs placebo). Improvements in symptoms with darifenacin were dose-dependent. Dry mouth occurred in 13%, 34% and 36% in the darifenacin 15 mg, 30 mg and oxybutynin groups, respectively. Constipation occurred more commonly in darifenacin groups, 10%, 21% and 8%, respectively. Patients reported blurred vision or dizziness with oxybutynin only (3% and 2%, respectively) (CitationZinner et al 2005).
In all fixed-dose phase III studies combined, 3.3% of patients treated with darifenacin discontinued due to adverse events versus 2.6% in placebo. Dry mouth and constipation were the leading causes of treatment discontinuation. The most common adverse effects associated with darifenacin 7.5 mg and 15 mg, respectively, were: dry mouth (20%, 35%), constipation (15%, 21%), dyspepsia (3%, 8%), urinary tract infection (5%, 5%) and abdominal pain (2%, 4%). Darifenacin is extensively metabolized by CYP2D6 and CYP3A4. Daily coadministration of darifenacin 30 mg with a potent CYP2D6 inhibitor (eg, paroxetine) can lead to a 33% increase of darifenacin drug exposure at steady state (CitationProduct Information 2004b).
Similar to other anticholinergic drugs, all newer agents for the management of OAB (trospium, solifenacin and darifenacin) are contraindicated in patients with urinary retention, gastric retention, or uncontrolled narrow-angle glaucoma (CitationProduct Information 2004b). Use these agents cautiously in patients with clinically significant bladder outflow obstruction, ulcerative colitis, intestinal atony, gastrointestinal obstructive disorders, myasthenia gravis, narrow-angle glaucoma, and moderate/severe hepatic dysfunction. Patients should be informed of possible anticholinergic side effects, such as heat prostration (fever and heat stroke due to decreased sweating in hot environment), dry mouth, constipation, dry eyes, urinary retention, dizziness and blurred vision. Use these agents only if the potential benefits outweigh the risks associated with therapy (CitationProduct Information 2004b).
Summary
Antimuscarinic agents are the mainstay of pharmacologic treatment of OAB. Currently available drugs indicated for the treatment of OAB with symptoms of urge urinary incontinence, urgency and frequency are: oxybutynin, tolterodine, trospium, solifenacin and darifenacin. All of these agents have demonstrated efficacy and safety in placebo-controlled clinical trials. Additionally, they have similar contraindications, precautions and side effect profiles (dry mouth, constipation and other anticholinergic effects). Management of urinary symptoms associated with OAB should be individualized based on patient renal/hepatic function, medical conditions and concurrent medication use. Dosing convenience and drug cost should be considered to promote patient compliance (). Anticholinergic side effects should be monitor closely, especially in the elderly and those who take other anticholinergic agents concomitantly. Ideally, patient medication regimen should be reviewed periodically for therapeutic efficacy, drug toxicity, clinical significant drug interactions and other drug-related problems.
Table 5 Considerations for individualizing therapy for overactive bladder (CitationProduct Information 2004a, Citation2004b, Citation2004c, Citation2004d)
References
- AbramowiczM2001Detrol LA and Ditropan XL for overactive bladderMed Letter43289
- AbramowiczM2003Oxybutynin transdermal (Oxytrol) for overactive bladderMed Letter45389
- AbramsPCardozoLFallM2002The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence SocietyNeurourol Urodyn211677811857671
- AppellRASandPDmochowskiR2001Prospective randomized controlled trial of extended-release oxybutynin chloride and tolterodine tartrate in the treatment of overactive bladder: results of the OBJECT studyMayo Clin Proc763586311322350
- CardozoLLisecMMillardR2004Randomized, double-blind placebo controlled trial of the once daily antimuscarinic agent solifenacin succinate in patients with overactive bladderJ Urol17219192415540755
- ChappleCRRechbergerTAl-ShukriS2004Randomized, double-blind placebo- and tolterodine-controlled trial of the once-daily anti-muscarinic agent solifenacin in patients with symptomatic overactive bladderBJU Int9333031014764127
- ChappleCRSteersWNortonP2005A pooled analysis of three phase III studies to investigate the efficacy, tolerability and safety of darifenacin, a muscarinic M3 selective receptor antagonist, in the treatment of overactive bladderBJU Int957993100115839920
- ChappleCRMartine-GarciaRSelvaggiL2005A comparison of the efficacy and tolerability of solifenacin succinate and extended release tolterodine at treating overactive bladder syndrome; results of the STAR trialEur Urol484647015990220
- ChuFMDmochowskiR2006Pathophysiology of overactive bladderAm J Med1193S8S
- DioknoACAppellRASandPK2003Prospective, randomized, double-blind study of the efficacy and tolerability of the extended-release formulations of oxybutynin and tolterodine for overactive bladder: results of the OPERA trialMayo Clin Proc786879512934777
- DmochowskiRRSandPKZinnerNR2003Comparative efficacy and safety of transdermal oxybutynin and oral tolterodine versus placebo in previously treated patients with urge and mixed urinary incontinenceUrology622374212893326
- ErdemNChuFM2006Management of overactive bladder and urge urinary incontinence in the elderly patientAm J Med11929S36S
- GittelmanMChuFMKlimbergI2003Two randomized, double-blind, placebo-controlled, parallel-group, fixed-dose, multicenter studies assess the efficacy and safety of daily oral administration of 10 mg YM905 versus placebo in male and female subjects with overactive bladderJ Urol169349
- HaabFStewartLDwyerP2004Darifenacin, an M3 selective receptor antagonist, is an effective and well-tolerated once-daily treatment for overactive bladderEur Urol454420915041104
- HaabFCardozoLChappleC2005Solifenacin Study Group. Long-term open-label solifenacin treatment associated with persistence with therapy in patients with overactive bladder syndromeEur Urol473768415716204
- HerbisonPHay-SmithJEllisG2003Effectiveness of anticholinergic drugs compared with placebo in the treatment of overactive bladderBMJ326841412702614
- HillSKhullarVWyndaeleJJ2006Dose response with darifenacin, a novel once-daily M3 selective receptor antagonist for the treatment of overactive bladder: results of a fixed dose studyInt Urogynecol J Pelvic Floor Dysfunct1732394715999217
- HuTWWagnerTHBentkoverJD2003Estimated economic costs of overactive bladder in the United StatesUrology611123812809878
- KelleherCJCardozoLChappleCR2005Improved quality of life in patients with overactive bladder symptoms treated with solifenacinBJU Int9581515638900
- OuslanderJG2002Geriatric considerations in the diagnosis and management of overactive bladderUrology6050512493354
- OuslanderJG2004Management of overactive bladderN Engl J Med3507869914973214
- Product Information2004a Ditropan XL®, oxybutynin chloride extended-release tablets. Ortho-McNeil Pharmaceutical, Inc., New Jersey, USA.
- Product Information2004b Enablex®, darifenacin. Novartis Pharmaceuticals Corporation, New Jersey, USA.
- Product Information2004c Sanctura®, trospium. Esprit, New Jersey, USA.
- Product Information2004d VESIcare®, solifenacin. Yamanouchi Pharma America, Inc. and GlaxoSmithKline, Oklahoma & New Jersey, USA.
- Product Information2005 Detrol LA®, tolterodine tartrate extended-release capsules. Pfizer Inc., New York, USA.
- RizackMA2005Solifenacin and darifenacin for overactive bladderMed Letter47234
- RudyDClineKHarrisR2006Multicenter phase III trial studying trospium chloride in patients with overactive bladderUrology672758016461077
- RudyDClineKHarrisR2006Time to onset of improvement in symptoms of overactive bladder using antimuscarinic treatmentBJU Int97540616469022
- SimpsonDWagstaffAJ2005Solifenacin in overactive bladder syndromeDrugs Aging221061916363887
- StaskinDRMacDiarmidSA2006Pharmacologic management of overactive bladder: practical options for the primary care physicianAm J Med11924S8S
- StaskinDRMacDiarmidSAUsing anticholinergics to treat overactive bladder: the issue of treatment tolerabilityAm J Med20061199S15S
- SteersWCorcosJFooteJ2005An investigation of dose titration with darifenacin, an M3-selective receptor antagonistBJU Int95580615705084
- StewartWFVan RooyenJBCundiffGW2003Prevalence and burden of overactive bladder in the United StatesWorld J Urol203273612811491
- SussmanDGarelyA2002Treatment of overactive bladder with once-daily extended-release tolterodine or oxybutynin: the antimuscarinic clinical effectiveness trial (ACET)Curr Med Res Opin181778412201616
- TodorovaAVonderheid-GuthBDimpfelW2001Effects of tolterodine, trospium chloride, and oxybutynin on the central nervous systemJ Clin Pharmacol416364411402632
- ZinnerNGittelmanMHarrisR2004SussetJKanelosAAuerbachSTrospium chloride improves overactive bladder symptoms: a multicenter phase III trialJ Urol1712311515126811
- ZinnerNTuttleJMarksL2005Efficacy and tolerability of darifenacin, a muscarinic M3 selective receptor antagonist (M3 SRA), compared with oxybutynin in the treatment of patients with overactive bladderWorld J Urol232485216096831