Abstract
Older adults age 65 and over account for a disproportional number of hospital stays and discharges compared to other age groups. The objective of this paper is to describe placement and characteristics of older patients discharged from an acute care for the elderly (ACE) unit. The study sample consists of 1,351 men and women aged 65 years or older that were discharged from the ACE Unit during a 12-month period. The mean number of discharges per month was 109.2 ± 28.4. Most of the subjects were discharged home or home with home health 841, 62.3%. The oldest elderly and patients who had been admitted from long term care institutions or from skilled nursing facilities to the ACE unit were less likely to return to home.
Introduction
Like other industrialized countries, the US population is aging with the group aged 65 years and older expected to double in size within the next 25 years (CitationAdministration on Aging 2005). In 2004, an estimated 35 million non-federal hospital discharges occurred in the US excluding newborns (CitationDeFrances and Podgornik 2004). Older adults age 65 and over account for a disproportional number of hospital stays and discharges compared to other age groups; 44% of the total day care in the hospital and 38% of all hospital discharges for 2004 (CitationDeFrances and Podgornik 2004). Although older adults constitute less than 15% of the population in the US, they utilized close to 50% of hospital expenditures (CitationElixhauser and Yu 2000). After the 4th decade of life the resources estimated per capita health expenditures increase dramatically (CitationWatson 1996).
Older adults face many risks and losses during hospitalization for acute medical illness. Complications can result from the unfamiliar setting, multiple diagnostic tests and procedures, and decreased nutrition and mobility. These may precipitate complications that include deconditioning, falls, delirium, depression, and infection to name a few (CitationLehman et al 2005). One of the challenges when treating the older adult’s acute illness in the hospital is to prevent hospitalization related complications, maintain function, and to plan for a successful discharge to the least restrictive environment.
Factors associated with hospitalization may precipitate a state of irreversible functional decline in a vulnerable older adult (CitationHoenig and Rubenstein 1991; CitationCreditor 1993). This functional decline can produce a cascade of dependency and changes in quality of life. Older adults are more vulnerable to this decline due to changes that may occur with advancing age. In a study of more than 2000 older adults admitted to two teaching hospitals, 35% of the subjects were discharged from the hospital with lower abilities to perform activities of daily living (ADL) than 2 weeks before admission (CitationCovinsky et al 2003). Factors independently associated with risk for decline in ADL function include older age, especially 85 years and older, unsteadiness, malnutrition, cognitive impairment, lower functional status (preadmission), and depression (CitationLamont et al 1983; CitationSager et al 1996; CitationLandefeld 2003). By modification of the hospital environment and promoting physical activity and socialization, the cascade to dependency can be prevented (CitationCreditor 1993).
In response to the growing number older adults with multiple co-morbid conditions and psychosocial problems, hospital units dedicated to the acute care for the elderly (ACE) have been developed across the United States and are growing in popularity. The ACE model specifically addresses the needs of the older adult. A safe, homelike physical environment, patient-family centered care, discharge planning to the least restrictive environment, dedicated staff with expertise in aging, interdisciplinary teamwork, and patient satisfaction are key elements of an ACE Unit (CitationPalmer et al 1994; CitationLehman et al 2005). The ACE Unit is a model of care aimed at minimizing losses experienced by hospitalized older adults while maximizing positive outcomes. The objective of this paper is to describe discharge destination and characteristics of older patients discharged from an ACE unit.
Methods
The study sample consists of 1,351 men and women aged 65 years and older that were hospitalized at the ACE Unit during a 12-month period. The ACE Unit is part of the John Sealy hospital at the University of Texas Medical Branch in Galveston, Texas.
The outcome, discharge destination, was defined as home or home with home health, long-term care institution (LTC) (eg, a nursing home), skilled nursing facility (SNF), other care options (eg, palliative care), or death. For bivariate and multivariate analyses, discharge destination was categorized as home or home with home health (code = 1) versus any other place or death (code = 0).
Independent variables were age, gender, and admission location. Age was used as continuous and categorical variable (years, 65–74, 75–84, and ≥85). Gender was male and female. Admission was defined as home or home with home health, long-term care institution (LTC) (eg, a nursing home), skilled nursing facility (SNF), other care options (eg, palliative care), or unknown.
Chi-square or the t test for bivariate comparisons and logistic regression analysis were used for multivariate comparisons. The significance level (two tailed) was set at P < 0.05. All computer programming and analyses were completed using version 9.1 of the SAS system for Windows (SAS Institute, Cary, NC, USA).
Results
illustrates the characteristics of the study population. The sample consists of 1,351 subjects with a mean age of 80.2 (± 7.8); 516 (38.2%) were men, and 835 (61.8%) were women. About a third of all subjects were 85 years and older. Women were slightly older at 80.9 ± 7.9 compared to men at 79.1 ± 7.4, and the difference was significant (p < 0.0001). The same trend was seen when age was used as a categorical variable, where women aged 85 and older had an increased percentage compared to men (p < 0.0001). Subjects (737 or 54.5%) were usually admitted from home or home with home health. The mean numbers of discharges per month was 109.2 ± 28.4. Women had an increased mean number of discharges per month compared to men (p < 0.0001). Most of the subjects were discharged to home or home with home health 841 (62.3%) after the hospitalization at the ACE unit.
Table 1 Characteristics of study population, older persons aged 65 and over
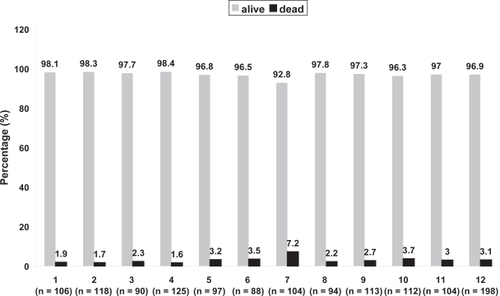
illustrates the subjects who were discharged from the ACE Unit during a 12-month period. It shows a range of discharges from 85 (6th month) to 198 (12th month). It also shows that the death rate range was from 1.6% (4th month, 2 deaths among 125 who were discharged) to 7.2% (7th month, 7 deaths among 104 who were discharged).
illustrates bivariate comparisons between discharge categories. It shows that patients who are discharged to home are more likely to be younger than patients who are discharged to other places or more likely to die (p = 0.0002). There are not gender differences between patients who are discharged to home and patients who are discharged to other places or died. Patients who are discharged to home are more likely to have a history of being admitted from home (p < 0.0001).
Table 2 Bivariate comparisons between discharge categories by selected characteristics
Patients who died (n = 39) had increased age (81.4 ± 9.6) when compared to patients who were alive (n = 1,312; 80.2 ± 7.7, p = 0.0425). Women who died (n = 21, mean = 85.8 ± 9.2) were significantly older than men who died (n = 18, mean = 76.3 ± 7.4, p = 0.0012).
illustrates the predictors of discharge to home in the ACE unit. Patients aged 75–84 (p = 0.0124) and 85 years and over (p = 0.0022) were less likely to return to home than patients aged 65–74. Gender was not a predictor of discharge to home. Finally, patients admitted from nursing homes (p < 0.0001), skilled nursing facilities (p < .0001) or other places (p = 0.0007) were less likely to be discharged to home compared to patients that were admitted from home.
Table 3 Predictors of discharge to home from the ACE UnitTable Footnotea
Discussion
Those over the age of 75 years and patients who had been admitted from long term care institutions or from skilled nursing facilities to the ACE unit were less likely to return to home. About 38% of our sample was not discharged to home, which is higher than the national data. The CitationAgency for Health Care Quality Research (1999) data shows that 23% of hospital patients aged 65 and older were discharged to another institution, and 11.6% are discharged with home care. This discrepancy could be secondary that our study sample was older and more likely to be in poorer health with more disability.
In a randomized evaluation, CitationLandefeld and colleagues (1995) demonstrated that Acute Care for Elders unit improved several outcomes of hospitalization at discharge including function, ability to walk, symptoms of depression, and reduced nursing home placement. ADL function improved from admission to discharge in 34% of patients in the ACE unit vs. 24% of patients receiving usual care (p = 0.009) and only 16% of patients in the ACE unit had a worsening in ADL function from admission to discharge as compared to 21% of patients with usual care.
Another randomized trial by CitationCounsell and colleagues (2000) demonstrated benefits in several processes of care such as reductions in prescription of high-risk medicines, restraints used, and days to discharge planning. Unfortunately, several studies on ACE units have not shown a significant reduction in mortality or hospital costs as compared to usual care (CitationLandefeld et al 1995; CitationCounsell et al 2000).
Transitional care is essential for persons with complex care needs and includes the sending and the receiving aspects of the transfer (CitationColeman and Boult 2003). Older adults, especially those with complex care, frequently need transitions across different sites of care. For example, transfers from SNFs back to acute care hospitals within 30 days are estimated near 20% (CitationKramer et al 2000). There are many adverse effects of poorly executed transitions for patients that are potentially preventable (CitationColeman and Boult 2003).
The healthcare team on the ACE unit utilizes an interdisciplinary team model approach to care especially in the discharge planning process. The team is typically composed of several disciplines including physicians, nurses, physical therapists, occupational therapists, dietitians, pharmacists, social workers and others. This team model has been described for acute care and in other levels and types of care such as palliative care (CitationMcCallin 2001; CitationCooper and Fishman 2003). Integration of roles is a feature of the interdisciplinary team. Effective care of older patients routinely combines the efforts of different disciplines.
Our study is not without limitations. We do not have information available about functional limitations or diseases that may affect discharge destination. Also, we have a high number of unknown admission places that prevent us from making definitive conclusions. However, our study suggests that admission characteristics may influence discharge destination in older patients. Further studies of this type of hospital unit (specializing in care of the elderly) should include additional patient characteristics (eg, functional status and social support). These are needed to determine other potential predictors for discharge disposition.
Acknowledgements
Dr Amador’s work is supported by the Geriatric Academic Career Award 1 K01 HP 00056-01 by the Bureau of Health Professions.
References
- Administration on Aging 2005 [online]Accessed July 28, 2006. URL: http://www.aoa.gov/PROF/Statistics/profile/2005/4.asp
- Agency for Health Care Quality Research HCUPnetOutcomes by patient and hospital characteristics for all discharges 1999 [online]Accessed July 28, 2006. URL: http://www.hcup.ahrq.gov/HCUPnet.asp
- ColemanEABoultC2003The American Geriatrics Society Health Care Systems Committee. Improving the quality of transitional care for persons with complex care needsJ Am Geriatr Soc51556712657079
- CounsellSRHolderCMLiebenauerLL2000Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: A randomized controlled trial of Acute Care for Elders (ACE) in a community hospitalJ Am Geriatr Soc4815728111129745
- CooperBSFishmanE2003The interdisciplinary team in the management of chronic conditions: Has its time come?Baltimore, MDPartnership for Solutions, Johns Hopkins University119
- CovinskyKEPalmerRMFortinskyRH2003Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with ageJ Am Geriatr Soc J514518
- CreditorMC1993Hazards of Hospitalization of the ElderlyAnn Intern Med118219238417639
- DeFrancesCJPodgornikMN2004National Hospital Discharge SurveyAdv Data. 2006 May4371119
- ElixhauserAYuKSteinerC2000Hospitalization in the United States, 1997 AHRQ Publication No 00-0031, HCUP Fact Book No 1Rockville, MDAgency for Healthcare Research and Quality
- HoenigHMRubensteinLZ1991Hospital-associated deconditioning and dysfunctionJ Am Geriatr Soc3922021991956
- KramerAEilertsenTLinM2000Effects of nurse staffing on hospital transfer quality measures for new admissionsHealth Care Financing AdministrationAppropriateness of Minimum Nurse Staffing Ratios for Nursing HomesBaltimore, MDHealth Care Financing Administration9.19.22
- LamontCTSampsonSMatthiasR1983The outcome of hospitalization for acute illness in the elderlyJ Am Geriatr Soc3128286841857
- LandefeldCSPalmerRMKresevicDM1995A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patientsN Engl J Med3321338447715644
- LandefeldCS2003Improving health care for older personsAnn Intern Med139421412965969
- LehmanCTylerSAmadorLF2005Care of the patient with dementia in the acute care setting: The birth of the ACE Unit. Chapter in: Care of the hospitalized person with dementiaSpringer
- McCallinA2001Interdisciplinary practice-a matter of teamwork: An integrated literature reviewJ Clin Nurs104192811822488
- PalmerRMLandefeldCSKresevicD1994A medical unit for the acute care of the elderlyJ Am Geriatr Soc42545528176151
- SagerMARudbergMAJalaluddinM1996Hospital admission risk profile (HARP): Identifying older patients at risk for functional decline following acute medical illness and hospitalizationJ Am Geriatr Soc4425178600192
- Watson Wyatt Worldwide1996From baby boom to elder boom: providing health care for an aging population