?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Older adults with type 2 diabetes have mobility impairment and reduced fitness. This study aimed to test the efficacy of the “Tai Chi for Diabetes” form, developed to address health-related problems in diabetes, including mobility and physical function. Thirty-eight older adults with stable type 2 diabetes were randomized to Tai Chi or sham exercise, twice a week for 16 weeks. Outcomes included gait, balance, musculoskeletal and cardiovascular fitness, self-reported activity and quality of life. Static and dynamic balance index (−5.8 ± 14.2; p = 0.03) and maximal gait speed (6.2 ± 11.6%; p = 0.005) improved over time, with no significant group effects. There were no changes in other measures. Non-specific effects of exercise testing and/or study participation such as outcome expectation, socialization, the Hawthorne effect, or unmeasured changes in health status or compliance with medical treatment may underlie the modest improvements in gait and balance observed in this sham-exercise-controlled trial. This Tai Chi form, although developed specifically for diabetes, may not have been of sufficient intensity, frequency, or duration to effect positive changes in many aspects of physiology or health status relevant to older people with diabetes.
Keywords:
Introduction
Type 2 diabetes has been estimated to affect over 100 million people worldwide and its prevalence is expected to increase to 300 million by 2025 (CitationBjork 2001). The condition is linked to declines in physical and psychosocial health and function (CitationOzdirenç et al 2003; CitationPaschalides et al 2004). Although moderate-to-vigorous intensity aerobic exercise and resistance training have been shown to improve all aspects of insulin resistance syndrome, most adults with type 2 diabetes do not follow recommended physical activity guidelines (CitationMokdad et al 2003), and the high prevalence of obesity and osteoarthritis in this cohort may severely limit participation in many standard forms of exercise. The ancient Chinese martial art of Tai Chi is characterized by slow, smooth movements. Tai Chi has previously been reported to improve balance, rate of falls, aerobic capacity, gait, and osteoarthritis symptoms in older people (CitationWolf et al 1996; CitationHartman et al 2000; CitationTaggart 2002; CitationChristou et al 2003; CitationSong et al 2003; CitationThornton et al 2004; CitationTsang and Hui-Chan 2004). Since older adults with insulin resistance syndrome are at higher risk for mobility disorders, arthritis, sedentariness, impaired aerobic fit-ness, and reduced quality of life compared to healthy adults (CitationLakka et al 2003), it is important to know if such benefits extend to diabetic people as well. A low-impact, low-intensity exercise such as Tai Chi may also address poor adoption of and adherence to typical aerobic exercise due to fear of injury in this population.
The aim of this study was to test the efficacy of an already-developed and widely-advocated Tai Chi program which was designed specifically for people with diabetes (CitationLam 2001), on mobility, physical function, and health-related quality of life in older people with type 2 diabetes. The results of the intervention on insulin resistance/glucose homeostasis and body composition have been reported (CitationTsang et al 2005). In this paper we present the results for the mobility, physical function, and quality of life outcomes, for which it was hypothesized that Tai Chi would improve all measures relative to controls.
Methods
Study design
The study was a single-blind, randomized, sham-exercise-controlled trial with an intention-to-treat design. The study was approved by Human Research Ethics Committee of the Universities of Sydney and New South Wales, Australia, and written informed consent was obtained.
Study population
Thirty-eight sedentary, older subjects with type 2 diabetes were recruited via community advertising. Subject screening included a telephone interview and a medical examination by the study physician. Subjects were eligible if they were ≥50 years of age, sedentary (≤2 exercise sessions/week), ambulatory without assistance, and had stable type 2 diabetes, defined as no change in diabetic medications for at least 3 months prior to study entry. Both aging and type 2 diabetes are related to decline in muscle function and performance (CitationDuckrow et al 1999; CitationOdenheimer et al 1994; CitationRingsberg et al 1999; CitationCarlson 2000; CitationWilley and Fiatarone Singh 2003) hence this ≥50 year age threshold was chosen. Exclusion criteria included cognitive impairment (MMSE ≤24), severe hip or knee arthritis (causing significant pain within 30 seconds of a semi-squat position), current Tai Chi participation, residence in a nursing home, amputation of a limb, severe visual impairment, and any condition that would have precluded the planned exercises in the opinion of the physician screening subjects.
Randomization
Subjects were randomly allocated to the intervention (Tai Chi) or control (sham exercise) groups. Permuted block randomization in blocks of four, stratified by gender was generated by an investigator not otherwise involved with study subjects using a computerized randomization program (CitationDallal 2003). Subjects were randomized following baseline assessment by handing them their group allocation in a sealed opaque envelope. They were blinded to the investigators’ hypotheses regarding which was the active intervention arm.
Interventions
Both groups completed two supervised one-hour sessions each week for 16 weeks. All classes were run by the same investigator extensively trained in both forms of exercise. This same investigator performed the outcome measures also, due to limited staff availability. The Tai Chi group performed the “Tai Chi for Diabetes” exercise (CitationLam 2001), a ‘hybrid’ form of 12 movements from Sun and Yang Tai Chi styles, which utilizes soft, smooth, and subtle movements, with the knees bent in a slight semi-squat position. Each session commenced with specific warm-up exercises for the whole body (10 minutes) and concluded with cool-down exercises (5 minutes). The Tai Chi form was usually performed in its entirety three times each session (45 minutes) and also involved guidance in breathing techniques and visualization. Controls performed sham exercise (calisthenics and gentle stretching), previously shown to have no significant effects on physical or psychological outcomes (CitationPu et al 2001). Most of the exercises were conducted seated, with 5–10 minutes of standing exercises holding onto the back of their chairs. No resistance was used other than opposing gravity, no sustained isometric contractions, prolonged static stretches, or sustained rapid movements were performed, so as to minimize adaptations in the domains of strength, flexibility, and aerobic capacity. Both forms of exercise were presented to the subjects as being potentially beneficial to them, and naming the program, “Move It for Diabetes” assisted in the blinding of the subjects to the hypothesized beneficial exercise mode.
Adverse events
A weekly questionnaire probing possible adverse events (including falls) and all changes in health status was administered in person or by telephone in both groups throughout the trial. A fall was defined as unintentionally coming to rest on the ground, floor or other lower level object (excluding a chair or bed), whether the subject was hurt or not.
Exercise intensity/compliance
Intensity was monitored once for each subject during weeks 14–16. Heart rate was monitored using a Polar heart rate monitor (Polar Electro, OY, Finland) set to record heart rate every 15 minutes throughout the exercise session, as well as at rest and two minutes post-exercise. The average of all exercise heart rates obtained during the session was calculated to estimate average exercise session intensity for each subject. The rating of perceived exertion was measured by the Borg scale (6–20). Rating of perceived exertion was recorded approximately every 15 minutes throughout the exercise session (at the same instance that heart rate was recorded) and averaged for each subject. Compliance to the program was determined as the percentage of sessions attended out of a total of 32 sessions, was calculated using the equation: (number of sessions attended ÷ 32) × 100.
Outcomes
Outcome measures were conducted at baseline (before randomization) and at follow-up (completion of 32 sessions). All measures were performed by the same investigator to maintain consistency in technique across all assessments.
Body composition and nutritional status
Fasting (12 hours) anthropometric measures included height (cm), mass (kg), and waist circumference (cm) using the method described by CitationNorton et al (1996). Fat-free mass (kg), fat mass (kg), and total body fat (%BF) (%) was assessed by bioelectrical impedance analysis (RJL systems, Prizum, BIA-101S, MI, USA) using standardized procedures and calculated using the equation of CitationLukaski et al (1986). All anthropometric measures were assessed in triplicate, and the coefficient of variation (CV) calculated by dividing the standard deviation by the mean.
Physical function
The six-minute walk distance test (CV = 5% (CitationKervio et al 2003)) was administered as described by the American Thoracic Society. For habitual gait speed, the average of two trials was recorded, while the faster of two trials was recorded for maximal gait speed. Using the duplicate measurements for each subject, the CV for habitual gait speed as well as maximal gait speed was calculated. Both habitual and maximal gait speed were measured over a straight path of six meters (as performed previously in other trials (CitationGotlin et al 2000; CitationMenz and Lord 2001), with a preceding acceleration lane of two meters, and a two meter deceleration lane following the six meter path. The six meter path was inconspicuously marked (only the researcher was aware of these markers) so the subjects were unaware that they were actually being timed between those points. The path was marked so subjects believed they were being timed from the start of the acceleration lane, until they passed the ‘finish line’, which was at the end of the deceleration lane. For habitual gait speed, subjects were asked to walk at their own normal, comfortable speed, and were reminded that this was not a test of their fastest walking speed. Subjects were asked to walk as fast as they possibly could, without running, for the test of maximal gait speed.
Muscle performance
Keiser pneumatic-resistance training equipment modified with K400 software (Keiser Corporation, Keiser, 11–5416, Fresno, CA) was used to measure bilateral knee extensor strength (1 repetition-maximum, 1RM), peak power (the best trial recorded after explosively lifting loads of 40%, 50%, 60%, 70%, 80%, and 90% 1RM), and endurance (number of repetitions at 90% baseline 1RM). For all muscle performance tests, both legs were tested together. Range of motion was limited to 90 degrees, and the concentric phase of the movement was assessed. Subjects were required to lift the loads with good form, only to their full range of motion, which was determined by asking them to lift a minimum load as high as they could by extending their knees. One trial was permitted for each test, and an attempt was made to achieve 1RM within ten repetitions. To determine 1RM, subjects were given 1–2 minutes rest between each repetition, and the load was increased with each repetition performed with good form until failure was reached in approximately 10 repetitions. Failure was reached when the subject could not lift the weight through their full range of motion on at least two attempts, at least 90 seconds apart. For the power test, subjects were instructed to, “Lift the weight as fast and explosively as you can – like a bullet out of a gun. Then slowly lower it back down.” Before the endurance test, subjects were asked to, “Slowly lift the weight and lower it down – 3 seconds up, 3 seconds down, until I ask you to stop.” This test was terminated once they could no longer lift the load to their full range of motion in good form, or if they paused between any two repetitions for one second or longer.
Balance
Six tests of static balance and postural control were measured on a Chattecx Balance System (Balance System Dynamic, Chattecx, 1014, Chattanooga, TN): anterior-posterior sliding (of the platform) with eyes open and closed; anterior-posterior tilting (of the platform) with eyes open and closed; and 1-legged stance (platform stationary) with eyes open and closed. The order of these conditions were presented to the subjects at random, using the computerized randomization program. Subjects were not told which test to expect next, the only information given to them was whether to stand on one or both legs, with their eyes open or closed. Maximum anterior-posterior and medio-lateral sway amplitude and stance time (up to 30 seconds) were recorded for each condition. The use of the Chattecx Balance System has been widely used in previous studies as a tool for measuring static and dynamic balance (CitationDickstein and Dvir 1993; CitationFife and Baloh 1993; CitationLevine et al 1996; CitationRingsberg et al 1999; CitationBennell and Hinman 2005). A balance index was derived as a summary score by summating all anterior-posterior and medio-lateral sway measures and time results respectively, to simplify the interpretation of relationships with the 18 balance variables, by allowing us to observe overall balance with a single variable. This method has been previously described and validated to be sensitive to changes during an exercise intervention (CitationOrr et al 2006). The balance index equation was as follows:
A lower balance index reflected less sway, and longer stance duration, hence better balance. From the results obtained from this test, unilateral stance duration was also observed in isolation, to compare any changes to results from previous Tai Chi studies which have utilised single-leg stance as a test of balance (CitationHartman et al 2000; CitationSong et al 2003).
Dynamic balance was assessed with the tandem walk test administered over a straight path of 3 meters. The duration of the faster of two trials and the number of mistakes made were recorded and summated to give a tandem walk score.
Health status and psychosocial function
Health status was obtained from self-report, physician exam, and medical records review. Cognitive function was determined by Mini-mental State Examination (MMSE) (CitationFolstein et al 1975), and habitual physical activity levels over the previous seven days were assessed using the Physical Activity Scale for the Elderly (PASE) (CitationWashburn et al 1993). Health-related quality of life, determined by the Short Form 36 Health Survey questionnaire (SF36), was comprised of 8 subscale scores (CitationWare et al 1993, 2000). Attitude towards diabetes was obtained from the Diabetes integration scale (ATT19) (CitationWelch et al 1996). All questionnaires were interviewer-administered.
Sample size
Sample size was estimated from studies of aerobic and resistance training effects on HbA1c in type 2 diabetes (CitationBoule et al 2001; CitationCastaneda et al 2002), as this was the primary outcome of the study (CitationTsang et al 2005). A decrease in HbA1c of 1% (absolute change) and a standard deviation of 1% was estimated. Setting the power (1-beta) at 0.8, and an alpha value of 0.05, total sample size required was estimated as 34 (CitationBuchner et al 1997). We estimated a dropout rate of 15%; thus the sample size was increased to 39. This sample size was also large enough to test for outcomes reported here: being appropriate for detecting an increase in leg extensor strength of 78.1 ± 45.8 N (effect size = 1.86); and for observing increases in duration of unilateral stance with eyes closed of 7.5 ± 7.8 s (effect size = 1.03), based on previous reports on Tai Chi in the literature (CitationChristou et al 2003; CitationSong et al 2003).
Statistical methods
Statistical analyses were performed using Statview, version 5.0 (SAS Institute, Cary, NC). Data collected from subjects who did not complete all training sessions were included in all analyses, as per the intention-to-treat design. All data were visually inspected for normality of distribution. Non-normal data were log-transformed. Baseline values are reported as mean ± standard deviation; and non-normally distributed data reported as median (range). Changes over time in outcome measures are reported as mean ± 95% confidence interval (95% CI). At baseline, groups were compared using t tests of continuous variables and by Chi square tests for categorical data. Repeated measures analysis of variance was used to analyze change over time and the main effect of group assignment. Additional analyses of covariance (ANCOVA) models were constructed to include potential confounders for outcomes of interest. Variables that were different between groups at baseline and potentially related to the outcome of interest were used as covariates in ANCOVA models. Between group (relative) effect sizes (ES) for study outcomes were calculated as:
A p value of <0.05 was accepted as statistically significant.
Results
Participant flow
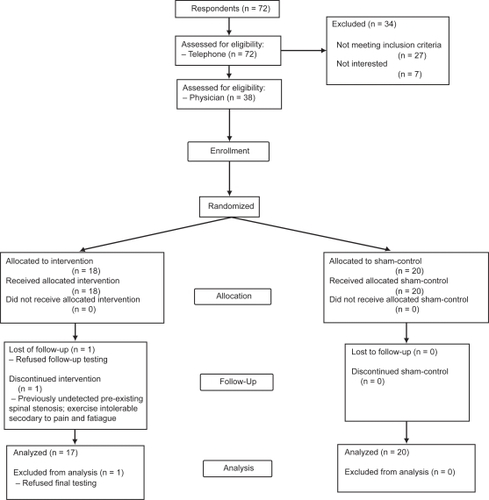
Recruitment and enrolment of 38 subjects occurred from March to July, 2004 (). Eighteen subjects were randomized to the Tai Chi group, and twenty were randomly allocated to the sham control group.
Participant characteristics
Baseline participant characteristics are shown in , and . The cohort had a mean age of 65 ± 8 years, and had been diagnosed with type 2 diabetes for 8.5 (0–50) years. Based on the National Cholesterol Education Program (NCEP) guidelines 23.7% of participants were overweight, and an additional 63.1% were obese, with only 13.2% presenting with a BMI within the normal range. Calculated CV’s for height and weight were 0.06% and 0.07% respectively. The subjects had many co-morbidities, primarily osteoarthritis, hypertension, dyslipidemia, and coronary artery disease (). In the cohort, 81.6% displayed metabolic syndrome, as defined by CitationNCEP (2002), and 40% had one or more diabetic complications (peripheral vascular disease, neuropathy, nephropathy, or retinopathy). Pharmacologic treatment (7.4 ± 4.0 medications per day) consisted of antihypertensives other than diuretics (76.3% of subjects), oral hypoglycemics (68.4%), primarily metformin (63.2%), hypocholesterolemics (55.3%), anti-inflammatories (31.6%), and diuretics (21.1%). Insulin was used by 9% of subjects, and 18.4% were not taking any medications for their diabetes.
Table 1 Baseline demographics and health status
Table 2 Baseline nutritional status
Table 3 Baseline and follow-up outcomes
Compared to controls, subjects randomized to Tai Chi had greater total body and central fat (measured via waist circumference (CV = 0.13%)) estimates (p = 0.03), higher cognitive scores, lower social function, and lower self-reported recreational and work-related activity, (, and ). Overall in our cohort, men reported more physical activity than women (PASE score 170.2 [95%CI: 88.6–251.8] in men vs. 111.2 [95%CI: 88.8–133.6] in women) (f = 4.6, p = 0.04), and had lower %BF (34.3 [95%CI: 26.7–41.9] in men vs. 41.5 [95%CI: 39.0–44.0] in women) (f = 6.3, p = 0.02).
Compliance
The median number of weeks taken to complete the trial (up to 32 sessions) was 16 (0.3–21.4) weeks. There was one dropout in the Tai Chi group (at week 4) who refused follow-up testing due to illness and difficulty with transport. The median attendance rate was 100 (6–100)% and 100 (0–100)% in Tai Chi and controls respectively (p = 0.7), inclusive of this dropout. Seventy-six percent of subjects completed >80% of the scheduled classes. Reasons for non-compliance included other commitments, moving away, and transport issues.
Adverse events
One subject (with pre-existing spinal stenosis) in the Tai Chi group found the exercise intolerable secondary to pain and fatigue, and did not attend after session 1. This condition was not symptomatic during the screening or baseline assessment, hence was not detected before randomization. Only the body composition and questionnaire data was included in the analyses for this subject, due to inability to perform any physical tests at follow-up.
Over the 16 weeks 0 (0–2) falls per person were reported in Tai Chi, and 0 (0–2) in controls (p = 0.2).
Exercise intensity
Proficiency was achieved in 6–12 sessions in the Tai Chi group, and 1–2 sessions in controls, as determined subjectively by the instructor. The average HR during Tai Chi sessions was 83.3 [95% CI: 76.3–90.3] beats/min, and 81.0 [95% CI: 75.5–86.5] beats/min during control sessions (p = 0.5). The mean Borg scale rating of perceived exertion was 11 [95% CI: 10–12] and 10 [95% CI: 9–11] for Tai Chi and controls respectively (p = 0.3).
Physical performance
Modest, significant improvements over time were seen in maximal gait speed (CV = 2.09%) in both groups (6.6 [95%CI: 1.5–11.7]% in Tai Chi, and 5.9 [95%CI: −0.1–11.9]% in controls; f = 9.2, p = 0.005; between group ES = 0.18)). Similarly, significant improvements were observed in the balance index (−3.9 [95%CI: −11.5–3.7] in Tai Chi vs. −7.4 [95%CI: −13.7–1.1] in. controls; f = 5.4, p = 0.03; between group ES = 0.3). There were no significant differences between groups () or group effects in ANCOVA models adjusted for baseline group differences (%BF, PASE score, MMSE, and baseline values of maximal gait speed or balance index).
No significant changes over time or between groups were observed in the other physical performance measures (six-minute walk distance, tandem walk, single-leg stance duration, muscle strength, power, and endurance, or habitual gait speed (CV = 3.16%)) ().
Habitual physical activity level
There was a significant group effect in physical activity score, with an increase in habitual physical activity of 18 [95%CI: −7.4–43.4] units in the Tai Chi group, and decrease of 35 [95%CI: −58.4–11.6] units in controls (f = 9.96, p = 0.003; between group ES = 0.35). However, after adjusting for baseline differences in potential confounders (PASE score, %BF, and social function), the difference in physical activity level between groups was no longer significant (p = 0.2).
Quality of life
A significant group effect was observed in Social Function sub-scale score, with Tai Chi improving their score by 6.6 [95% CI: −7.3–20.5] and controls worsening by 14.2 [95% CI: −28.1–0.3] (f = 4.6, p = 0.04; between group ES = 0.24), but this group difference was attenuated and no longer significant after change in social function was adjusted for %BF, and physical activity levels (f = 3.7, p = 0.07). None of the other domains measured in the SF36, or ATT19 score were significantly changed after the intervention over time or between groups.
Discussion
Habitual gait speed and a summary static/dynamic balance index improved similarly and significantly in both Tai Chi and control groups after 16 weeks. There was a tendency for Tai Chi practice to be associated with improvement in habitual activity level and Social Function relative to sham-exercise participation, but these trends did not lead to differential benefits in terms of physical function or mobility. Neither the “Tai Chi for Diabetes” form nor sham exercise improved muscle function, endurance capacity, cognition, or other aspects of health-related quality of life in older sedentary adults with type 2 diabetes. The strength of this study compared to some previous investigations lies in the use of a sham exercise rather than non-treatment control condition and the randomized design and intention-to-treat analysis.
It is possible that the modest improvements in balance over time represented a learning effect, as repeated trials were not given at baseline, rather than a specific result of exercise. Tai Chi involves the practice of shifting to the limits of stability (thus training someone to increase sway), whereas the balance index penalizes those who sway when perturbed. Several previous Tai Chi trials have measured static balance improvements with the one-legged stance duration test (CitationHartman et al 2000; CitationSong et al 2003), which is one small component of our balance index measure. However, when we examined only the static stance time in isolation, there was neither improvement over time nor effect of group assignment. The lack of improvement in the tandem walk test after the intervention was unexpected, as it was thought that the heel-down-first action of the feet and weight-shifting in the Tai Chi form was somewhat similar to that required in the tandem walk test, and may have therefore been transferable between the two. The speed of movement, and distance between the feet however are different between Tai Chi and tandem walking, which may explain the lack of improvement in this measure which required both speed and accuracy. No other controlled trial of Tai Chi has tested dynamic balance with the tandem walk test, or the exact balance platform measure we employed, thus preventing direct comparisons to balance outcomes in other studies. However, the Atlanta FICSIT study (CitationWolf et al 1993) also reported no improvement in computerized balance platform testing after a Tai Chi form found effective for fall prevention. As in our testing paradigms, the FICSIT subjects were penalized for swaying, suggesting that this mode of testing is insufficiently sensitive to the kinds of balance improvements targeted by the practice of Tai Chi.
It is unlikely that a ceiling effect on the balance index explains the lack of group differences.
In another recent study by CitationOrr et al (2006) we have reported improvements in balance index in healthy older adults, of similar age to this cohort, after power training. The subjects in the present study had poorer balance scores at baseline (a mean balance index of 110.8), compared to the mean score of 89.4 by those in the study by CitationOrr et al (2006), suggesting that these diabetic subjects had sufficient impairments in balance to respond to a balance-enhancing intervention.
The smaller than expected improvements in balance in our Tai Chi group may also be related to their co-morbidities, in addition to the methodological issues discussed above. Almost all of our subjects were overweight or obese (86.8%) and 89% had osteoarthritis, both of which likely impaired their ability to perform the proper weight-shifting or semi-squat position that was intended during Tai Chi. The low exercise HR observed (83.3bpm compared to 116bpm in a previous study (CitationLan et al 1998)) may also be attributed to these factors, though CitationJin (1989) also noted similar HR’s in beginners of Tai Chi when practicing in the morning and evening (87.4bpm and 94.1bpm respectively). The BMI of our cohort was greater than that of patients with osteoarthritis who had BMI’s within the normal range, (CitationSong et al 2003). Those subjects demonstrated a significant improvement in one-legged stance duration after Tai Chi training, in contrast to the overweight-to-obese subjects in CitationHartman et al (2000) and the present study, both of which found no significant change in balance measures compared to controls. It would be of interest for future studies to directly compare balance adaptations to Tai Chi between overweight and normal weight or sarcopenic individuals to identify characteristics of high responders.
Muscle function did not improve in either group in our study. Previous Tai Chi studies have reported significant improvements in isokinetic and isometric knee extensor strength ranging from 13.5%–46.2% after 12–52 weeks of training in older adults with no previous Tai Chi experience (CitationLan et al 1998; CitationLan et al 2000; CitationChristou et al 2003; CitationChoi et al 2005). Six months of Tai Chi practice 3–4 times per week improved the endurance ratio of the knee extensors by 9.6%–18.8% in healthy, community-dwelling adults (CitationLan et al 2000), whereas no change in endurance was observed in our study. The frequency of training in these studies ranged from 3–7 sessions per week (though requested daily home practice was not monitored in these studies), which may explain why we saw only a non-significant 12.9% improvement in strength, and no significant changes in muscle power or endurance after Tai Chi. As noted, most of our subjects also presented with osteoarthritis, and therefore maintained a higher stance during Tai Chi practice to avoid exacerbation of their condition, thus possibly not providing their knee extensors a large enough stimulus to promote strengthening of the muscles at an angle which would contribute to a knee extensor one repetition maximum (performed from 90 degrees of flexion through full extension). It is also possible that the benefits of the isometric contractions of Tai Chi were not reflected in the dynamic strength tests we used, due to specificity of training adaptations.
Small but significant improvements were seen in maximal gait speed in both groups, though based on the relative ES’s calculated, our study may have been underpowered to identify between group differences in maximal gait speed. The gait speed tests were performed twice at baseline and follow-up however, so learning is unlikely to be the mechanism of benefit. We had hypothesized that only the Tai Chi group would improve their gait velocity, but it is possible that changes in other unmeasured factors such as self-efficacy, depression, or arthritis symptoms explained these improvements in both groups. Several other studies have also reported no benefits of Tai Chi on gait speed or walking endurance. CitationWolf et al (1996) found that 15 weeks of Tai Chi training decreased the distance walked in 12 minutes, perhaps due to the emphasis on slow movements during the Tai Chi training. Neither CitationWolfson et al (1996) nor CitationHartman et al (2000) found significant changes in habitual gait speed, similar to our results. Compared to age and gender norms for gait speed (CitationBohannon 1997), our cohort had slightly slower habitual and maximal gait speed at baseline than age-matched peers, suggesting some degree of gait impairment. However it is possible that our subjects, selected for diabetes rather than frailty, mobility disorders, or falls risk, did not have sufficient impairment in habitual gait to improve this outcome, whereas the more stressful maximal gait speed test allowed room for improvement.
Limitations in this study include the non-blinded assessment of outcomes, lack of specificity of outcomes for the physiological characteristics of this form of Tai Chi, and the intervention intensity, duration and frequency. Isometric as well as dynamic strength measures in future studies may shed light on the specific adaptations in muscle function attributable to Tai Chi. Reduction in stride-to-stride gait variability, which has been shown to be predictive of falls (CitationHausdorff et al 2001) may be more likely to improve after Tai Chi than simple measures of habitual velocity. A more frequent Tai Chi intervention (3–4 times a week) should be considered to allow for further progression in the intensity of performance (for example, lowering the stance as the subject is able). The use of a chair or bar for support during initial training of the stances and foot/leg movements may be considered. Additionally, it is possible that more time spent guiding the internalization of the exercises would improve physical and psychosocial function to a greater degree.
In conclusion, twice-weekly, supervised participation in a Tai Chi program utilizing the “Tai Chi for Diabetes” form for 16 weeks or a sham exercise class both improved maximal gait speed and overall balance modestly, perhaps due to non-specific effects of study participation or learning effects. However, habitual gait speed, muscle strength, static balance, walking endurance, and self-reported physical function or mental health did not improve in older sedentary adults with type 2 diabetes. Our results should not be extrapolated to cohorts differing significantly from ours in terms of health status, age, or obesity. Tai Chi may be an appropriate exercise to explore further in relation to its potential benefits for individuals who may be reluctant to participate in some traditional exercise modalities due to physical and/or psychological characteristics. Tai Chi forms vary widely, as does ability to master complex movements, and thus generalizations of benefits observed between different Tai Chi forms or between different cohorts should not be assumed without empirical evidence of benefit.
Financial disclosure
This study was supported by the School of Exercise and Sport Science, University of Sydney, $700 AUD. Blood tests and collection tubes were supplied by our sponsor, Douglass Hanly Moir Pathology.
There were no conflicts of interest and the results of the present study do not constitute endorsement of the product by the authors: T Tsang, R Orr, E Comino, and MF Singh. Author P Lam was the creator of the “Tai Chi for Diabetes” form and producer of its video, and is also the founder of the business, Tai Chi Productions, which distributes these videos and similar products and services.
Acknowledgements
The authors would like to express their gratitude to their sponsor, Douglass Hanly Moir Pathology for all their assistance and generosity; to Keiser Sports Health Inc for their donation of K400 Electronics for pneumatic resistance machines; and to the subjects for their dedication and commitment to the study. This study was funded by the School of Exercise and Sport Science, University of Sydney, Australia.
References
- BennellKLHinmanRS2005Effect of experimentally induced knee pain on standing balance in healthy older individualsRheumatology443788115572391
- BjorkS2001The cost of diabetes and diabetes careDiabetes Research & Clinical Practice54Suppl 1S13811580964
- BohannonRW1997Comfortable and maximum walking speed of adults aged 20–79 years: Reference values and determinantsAge & Ageing261599143432
- BouleNGHaddadEKennyGP2001Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: A meta-analysis of controlled clinical trialsJournal of the American Medical Association28612182711559268
- BuchnerAFaulFErdfelderE1997University of Trier, Trier, Germany.
- CarlsonJE2000CME article: Role of physical activity in the prevention of disability for older personsClinical Geriatrics8
- CastanedaCLayneJEMunoz-OriansL2002A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetesDiabetes Care2523354112453982
- ChoBLScarpaceDAlexanderNB2004Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adultsJ Am Geriatr Soc5211687315209657
- ChoiJHMoonJSSongR2005Effects of Sun-style Tai Chi exercise on physical fitness and fall prevention in fall-prone older adultsJournal of Advanced Nursing51150715963186
- ChristouEAYangYRosengrenKS2003Taiji training improves knee extensor strength and force control in older adultsJ Gerontol A Biol Sci Med Sci58763612902537
- DallalGE2003Randomization.com [online]. Accessed on March 15, 2004. URL:http://www.randomization.com
- DicksteinRDvirZ1993Quantitative evaluation of stance balance performance in the clinic using a novel measurement devicePhysiotherapy Canada45102810126337
- DuckrowRBAbu-HasaballahKWhippleR1999Stance perturbation-evoked potentials in old people with poor gait and balanceClinical Neurophysiology11020263210616107
- FifeTDBalohRW1993Disequilibrium of unknown cause in older peopleAnnals of Neurology346947028239563
- FolsteinMFolsteinSMcHughP1975“Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJournal of Psychiatric Research12189981202204
- GotlinRSShermanALSierraN2000Measurement of brake response time after right anterior cruciate ligament reconstructionArchives of Physical Medicine & Rehabilitation81201410668775
- HartmanCAManosTMWinterC2000Effects of T’ai Chi training on function and quality of life indicators in older adults with osteoarthritisJournal of the American Geriatrics Society481553911129742
- HausdorffJMRiosDAEdelbergHK2001Gait variability and fall risk in community-living older adults: a 1-year prospective studyArchives of Physical Medicine & Rehabilitation821050611494184
- JinP1989Changes in heart rate, noradrenaline, cortisol and mood during Tai ChiJournal of Psychosomatic Research331972062724196
- KervioGCarreFVilleNS2003Reliability and intensity of the six-minute walk test in healthy elderly subjectsMedicine & Science in Sports & Exercise351697412544651
- LakkaTALaaksonenDELakkaHM2003Sedentary lifestyle, poor cardiorespiratory fitness, and the metabolic syndromeMedicine & Science in Sports & Exercise3512798612900679
- LamP2001East Action VideosTai Chi ProductionsNarwee
- LanCLaiJSChenSY199812-month Tai Chi training in the elderly: Its effect on health fitnessMedicine & Science in Sports & Exercise30345519526879
- LanCLaiJSChenSY2000Tai Chi Chuan to improve muscular strength and endurance in elderly individuals: A pilot studyArchives of Physical Medicine & Rehabilitation81604710807099
- LevineDWhittleMWBeachJA1996Test-retest reliability of the Chattecx balance system in the patient with hemiplegiaJournal of Rehabilitation Research & Development3336448868416
- LukaskiHCBolonchukWWHallCB1986Validation of tetrapolar bioelectrical impedance method to assess human body compositionJournal of Applied Physiology601327323700310
- MenzHBLordSR2001Foot pain impairs balance and functional ability in community-dwelling older peopleJournal of the American Podiatric Medical Association91222911359885
- MokdadAFordEBowmanB2003Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001Journal of the American Medical Association28976912503980
- NCEP2002National Heart, Lung, and Blood Institute
- NortonKWhittinghamNCarterL1996NortonKOldsTAnthropometricaUNSW PressSydney2575
- OdenheimerGFunkensteinHHBeckettL1994Comparison of neurologic changes in ‘successfully aging’ persons vs the total aging populationArchives of Neurology51573808198468
- OrrRde VosNJSinghNA2006Power training improves balance in healthy older adultsJournal of Gerontology A Biological Science Medical Sciences61A7885
- OzdirençMBiberogluSOzcanA2003Evaluation of physical fitness in patients with type 2 diabetes mellitusDiabetes Research in Clinical Practice601716
- PaschalidesCWeardenAJDunkerleyR2004The associations of anxiety, depression and personal illness representations with glycaemic control and health-related quality of life in patients with type 2 diabetes mellitus5755764
- PuCTJohnsonMTForman2001The effects of high-intensity strength training on skeletal muscle and exercise performance in older women with heart failure: A randomized controlled trialJournal of Applied Physiology9023415011356801
- RingsbergKGerdhemPJohanssonJ1999Is there a relationship between balance, gait performance and muscular strength in 75-year-old women?Age & Ageing282899310475866
- SongRLeeEOLamP2003Effects of Tai Chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trialJournal of Rheumatology3020394412966613
- TaggartHM2002Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older womenApplied Nursing Research152354212444582
- ThorntonEWSykesKSTangWK2004Health benefits of Tai Chi exercise: improved balance and blood pressure in middle-aged womenHealth Promotion International1933814976170
- TsangTOrrRLamP2005Health benefits of Tai Chi for older adults with type 2 diabetesJournal of the American Geriatrics Society: 2005 Annual Scientific Meeting Abstract Book53S1745
- TsangWWHui-ChanCW2004Effect of 4- and 8-wk intensive Tai Chi training on balance control in the elderlyMedicine & Science in Sports & Exercise366485715064593
- WareJEJrSnowKKKosinskiM1993, 2000SF-36 health survey: Manual & interpretation guideQualityMetric IncorporatedLincoln, RI
- WashburnRASmithKWJetteAM1993The physical activity scale for the elderly (PASE): development and evaluationJournal of Clinical Epidemiology46153628437031
- WelchGBeeneyLJDunnSM1996The development of the diabetes integration scale: A psychometric study of the ATT39Multivariate Experimental Clinical Research117588
- WilleyKFiatarone SinghM2003Battling insulin resistance in elderly obese people with type 2 diabetes - bring on the heavy weightsDiabetes Care261580158812716822
- WolfSBarnhartHKutnerN1996Reducing frailty and falls in older persons: An investigation of Tai Chi and computerized balance trainingJournal of the American Geriatrics Society44489978617895
- WolfSLKutnerNGGreenRC1993The Atlanta FICSIT study: Two exercise interventions to reduce frailty in eldersJournal of the American Geriatrics Society41329328440859
- WolfsonLWhippleRDerbyC1996Balance and strength training in older adults: Intervention gains and Tai Chi maintenanceJournal of the American Geriatrics Society444985068617896