Abstract
Objective
To determine the effectiveness of 8-week group functional balance training classes on balance outcomes in community-dwelling veterans at risk for falls.
Design
Pre-test, post-test using retrospective data.
Setting
VISN 8 Patient Safety Center at James A. Haley Veterans Hospital in Tampa, FL, USA.
Participants
Fifty one community living veterans with mean age of 78 at risk for falls.
Intervention
Participants received a weekly 1-hour functional balance training class for 8 weeks in a small group setting (4–5 participants).
Measurements
Pre and post intervention measures included Berg Balance Scale, Limits of Stability (LOS) and modified Clinical Test of Sensory Interaction on Balance (mCTSIB).
Results
Eighty four percent of the participants completed 5 or more weekly classes. Peripheral neuropathy was the most common risk factor among the participants. There was a significant improvement in the Berg (p < 0.0001) and Composite Reaction Time (p < 0.0004) after the intervention.
Conclusion
An eight week group functional balance training class was safe and effective in improving balance outcomes in a cohort of elderly veterans at risk for falls.
Keywords:
Introduction
A growing body of research supports the link between exercise and fall prevention. A systematic review of this literature (CitationGregg et al 2000), found consistent evidence from a series of prospective and case-control studies linking physical activity with a 20%–40% reduced risk of hip fracture. Balance exercise programs can be effective in improving gait and balance, as well as reducing falls and fall-related injuries (CitationHerwaldt and Pottinger 2003; CitationWolfson et al 1996; CitationTinetti et al 1996).
Further research is needed to gain insight into the underlying mechanisms of different type of exercises and their impact on stability in individuals at risk for falls. Despite thousands of research studies published on patient falls, few studies have focused on the effectiveness of interventions (CitationRubenstein 2004), and fall rates and associated injuries among the elderly continue to rise (CitationCDC 2002). Impaired gait and balance (referred to as impaired stability) is one of the most significant causes and consequences of falls (CitationRobbins et al 1989; CitationAmerican Geriatric Society, British Geriatric Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention 2001; CitationFoster et al 2004).
The purpose of this pre-test, post-test clinical intervention study was to determine the effectiveness of 8-week group functional balance training classes on balance outcomes in community-dwelling veterans conducted at the VISN 8 Patient Safety Center from 2001 to 2004. The objectives of this study were to determine: (1) the diagnostic profile of veterans who participated; (2) class participation rates; (3) the rank order of fall risk factors; and (4) differences in balance measures pre and post participation.
Functional balance training
Functional balance training is a type of exercise that combines muscle strengthening and balance activities with functional gait activities. Regular balance training exercises for a period as short as 9 weeks improved postural control in a study group of persons aged 70–75, as measured by various clinical tests and dynamic posturography, when compared to age-matched control (CitationLedin et al 1991). A 6-week enhanced balance training program consisting of a series of tasks of increasing difficulty which are related to functional balance versus “standard” physical therapy for adults with balance and mobility deficits (CitationSteadman et al 2003) reported positive results in a sample of 199 older adults. We could find no evidence dealing with the dose or duration, of group balance classes.
Study methods
Research design
A pre-test, post test clinical intervention study was conducted over 3 years (2001–2004), using a convenience sample of veterans, that were seen at the VISN 8 Patient Safety Center Falls clinic, found to be at increased risk for falls based on an interdisciplinary fall risk assessment and recommended to participate in an 8-week Group Functional Balance Class.
Clinical intervention
All class sessions began with the warm-up exercises and were conducted using a standing protocol for each session (see describing course content). The specific exercises and patient handouts can be found at http://www.visn8.med.va.gov/patientsafetycenter/fallsTeam.asp The Group Functional Balance Classes incorporated exercises pertaining to lower extremity strengthening, flexibility, coordination, multi-tasking, postural control and gait training. This exercise intervention had a maximum of 5 subjects per class, and was held 1 hour each week, for a total of 8 weeks. The class was taught by a PT with one trained handling assistant for safety reasons. A weekly exercise sheet was given out to participants at the end of each class at which time the therapist demonstrated the home exercises and answered any questions. Participants were provided a course program folder at the beginning of the course, and encouraged to bring the folder to class weekly, so they could take notes, insert new handouts, and show records of their “homework assignments”.
Table 1 Functional balance class content
. outlines class content over the 8 week period.
The space accommodated a large set of parallel bars and multiple chairs. Warm-up exercises were performed in a seated position with the participants’ chairs being set-up in a “U” shape around the instructor and facilitators. The majority of the standing exercises were performed around the parallel bars (each participant should have ample room to stand and move without touching each other). Chairs were positioned behind each patient to allow them to sit and rest immediately if necessary. Equipment required for each class was listed on each handout. Typically, this equipment consisted of devices which were readily available in a therapy department. Patients were advised to exercise at their “own level” and “listen to their body”. They were encouraged to sit (chair located behind them) at any time during the class to rest if necessary and advised to inform a staff member immediately if they experience any form of distress.
The 8-week curriculum consisted of 8 critical balance elements essential for safe performance of ADLs. These elements progressively increase in difficulty over the 8 week period with increased class time allotted to elements which are more complex and potentially harder for subjects to master. Class begins with an emphasis on core stability exercises in standing and rapidly progresses through various levels of mobility and center of gravity control over the 8 weeks; ultimately ending with multi-tasking and complex movement coordination skills. Protective postural responses, anticipatory postural mechanisms and ability to respond to various environmental conditions (manipulation of surface and vision) are trained throughout the entire 8-week session.
Subjects/sample
A retrospective chart review of patients that participated in the 8 week Group Functional Balance course were reviewed for the period of 2001–2004. Subject were referred for the course if they were cognitively intact, able to stand unsupported for a minimum of 10 minutes, had fair to good rehab potential demonstrated on Falls Clinic Functional Assessment, were willing to participate and attempt to attend all 8 class sessions, and medically cleared for moderate level exercise. A total of fifty one patients consented to participate in the Group Functional Balance Class.
Measures
The measures completed pre and post intervention included Berg Balance Scale (CitationBerg et al 1989), Limits of Stability (LOS) (CitationClark and Rose 2001) and modified Clinical Test of Sensory Interaction on Balance (mCTSIB) (CitationShumway-Cook and Horak 1986).
Berg balance scale
The Berg Balance Scale is a commonly used clinical measure to evaluate performance during various balance activities. The scale consists of 14 common daily balance tasks. Administration requires only minimal basic equipment and takes approximately 15 minutes. All 14 sub-tests are scored on a 5-point ordinal scale based on the subject’s ability to perform the requested task safely and in a timely manner. Sub-test scores are summed to achieve a total score ranging from 0 to 56 with higher scores indicating better performance. The Berg Balance Scale has established psychometric properties including a Cronbach alpha value for internal consistency of 0.96 and inter-rater reliability values ranging from 0.71 to 0.99 (CitationBerg et al 1989). Concurrent validity as a measure of balance has been determined in comparison with the POMA balance subscale (Pearson r = 0. 91) and the Timed Up and Go (Pearson r = −0.76) (CitationBerg et al 1992).
Limits of stability (LOS)
This test allows for the analysis of a subject’s ability to voluntarily move their center of gravity to their limits of stability in the eight cardinal and diagonal directions. Outcomes include: reaction time, sway velocity, directional control, endpoint excursion and maximum excursion. Endpoint excursion and maximum excursion are calculated as percentages of the subjects theoretical 100% limit of stability that is a function of their height. The LOS takes 10 minutes to administer and retest reliability has been shown to be good to excellent (CitationWigglesworth et al 1996).
Modified clinical test of sensory interaction on balance (mCTSIB)
The mCTSIB protocol consists of four separate conditions, of increasing difficulty, performed with the subject in a quiet upright stance. They are 1) firm surface with eyes open, 2) firm surface with eyes closed, 3) foam surface with eyes open and 4) foam surface with eyes closed. Each sub-test lasts 30 seconds and is repeated 3 times. The combination of these sub-tests can document the presence of sensory dysfunction and provide objective analysis of the patient’s functional balance control by quantifying postural sway velocity during the four sensory conditions (http://www.onbalance.com/neurocom/protocols/motorImpairment/los.aspx).
Data collection
One member of the falls clinic team completed record review. Data were extracted from the Falls Clinic Consult Note (demographics, age, co-morbidities, falls risk factors) and Group Functional Balance Class Notes for each patient (balance outcomes). The data were recorded onto a customized Access database.
Data analysis
Descriptive statistics and Paired t-test were used for the analysis.
Results
The age of the participants ranged from 43 to 90 years, with an average age of 77.9 years (SD: 7.2 years) and median age of 80.
Most commonly identified fall risk factors
Data were extracted from the fall clinic notes as to the risk factors that were contributing to falls. The most common risk factors were presence of peripheral neuropathy and centrally-acting medications. Since majority of patient has multiple risk factors identified, only top three fall risk factors were extracted from the Falls Clinic Consult Note ().
Table 2 Rank order of fall risk factors
Frequency of subject participation
Forty seven percent of participants attended at least 5 functional balance classes, 22% attended 7 and 33% attended all 8 classes.
Balance outcomes
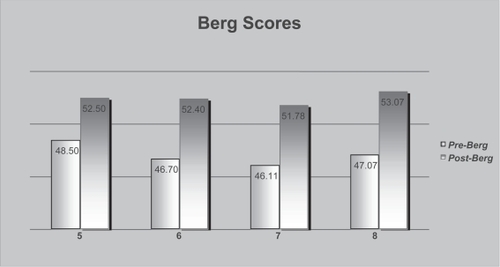
Patients made gains in balance in all measures. Increases in scores for post-intervention Berg Balance Scale are presented in . Mean Berg score increased from 46.8 to 52.5 on average. Participants also showed improvements in Limits of Stability Test (LOS) (See .) LOS composite Reaction Time (RT) and composite movement velocity (MVL) showed trends toward improvement while LOS composite end point excursion (EPE), maximum excursion (MXE) and directional control (DCL) all were significantly improved when compared to baseline.
Table 3 Berg balance scores
Table 4 Limits of stability test
Scores on mCTSIB measures also demonstrated improvement represented by a decrease in the mean center of gravity (COG) sway velocity. As shown in , the lower the number post intervention indicates a trend towards the reduction of sway for all testing conditions. Significant improvement was measured in the composite mean center of gravity sway velocity indicating improvement in balance post intervention (2.50 degrees/sec to 2.20 degrees/sec).
Table 5 Modified clinic test for sensory interaction in balance (mCTSIB) results
Functional balance scores by frequency of class participation
A total of 33 participants attended both first and last class. We wanted to explore if there was an optimal dose of the intervention and tried to analyze results by dividing participants based on the number of classes attended (4–6 classes vs. 7–8). Using a paired t-test statistically significant pre-post changes were found in Berg (p < .0001) and Composite Reaction Time (p < .0004) for both participants that attended 4–6 and those that attended 7–8 classes when compared to baseline, but none within the groups so, in conclusion, no difference in improvement was found between individuals that participated in 4–6 classes vs. 7–8 classes.
Results are shown in .
We also looked at the subgroup of participants with the most common risk factor—peripheral neuropathy and found statistically significant improvement in pre-post measures in Berg score (46.26 [SD 3.03] to 52.74 [SD 2.70]) (p < 0.0001), LOS composite EPE (p < 0.006), composite MXE (p < 0.001), and composite DCL (p < 0.0005) and MCT composite mean COG sway velocity 2.33 (SD 0.78) to 1.94 (SD 0.66) (p < 0.038).
Discussion
We wanted to provide some preliminary data on dose and intensity of exercise interventions in elderly at risk for falls. We found statistically significant improvement in balance outcomes as a result of an 8 week group functional balance training class. We also demonstrated the feasibility of a group functional balance intervention and safety in elderly at risk for falls. Treating individuals in small groups rather then on a 1:1 basis is also a more economical way of providing treatment. Our study has a number of limitations. It was retrospective and we did not do post-intervention testing on the subjects that dropped out, so we do not know if they were any different then the subjects that finished the intervention. We found improvement (and no difference) in balance outcomes in both patients that participated in 4–6 classes or 7–8 classes since our sample size was probably too small to find a difference. Also we did not measure the amount of time patients spent at home doing exercises on their own which could have confounded the outcomes although that would have been a bigger problem if we did not find the difference in balance measures. We did not track falls but used balance outcomes as a marker of fall risk. In addition, we noticed that our participants benefited form the social interactions (based on their feedback) before, during and after the classes but we did not formally measure their psychosocial wellbeing in this study or how it affected the participation rates.
Future directions
Our group functional balance intervention needs to be further tested in a prospective trial with falls as a primary outcome rather than balance measures to see if our intervention is effective in reducing fall risk as well as looking at cost-effectiveness of group vs. individual treatment. Further studies are needed to address the most effective dose and intensity of exercise in elderly individuals at risk for falls and testing exercise intervention in specific populations of individuals at risk for falls like peripheral neuropathy, osteoarthritis, Parkinson’s disease, etc.
Focusing on a homogeneous patient populations would distinguish unique gait and balance deficits that contribute to impaired stability and mobility risk, as well as to better understand unique responses to treatment that are clouded when diverse patients are aggregated (CitationKing and Tinetti 1996; CitationNelson and Quigley 2002).
References
- American Geriatric Society, British Geriatric Society, and The American Academy of Orthopaedic Surgeons Panel on Falls Prevention2001Guideline For the Prevention of Falls in Older PersonsJAGS49664672
- BergKWood-DauphineeSWilliamsJIGaytonD1989Measuring balance scale: Reliability assessment with an elderly populationArchives of Physical Medicine and Rehabilitation73107310801444775
- BergKOWood-DauphineeSLWilliamsJIMakiB1992Measuring balance in the elderly: validation of an instrumentCan J Public Health Jul–Aug83 Suppl2S7111468055
- BergKOWood-DauphineeSLWilliamsJIGaytonD1989Measuring balance in the elderly: preliminary development of an instrumentPhysiotherapy Canada41304311
- Centers for Disease Control (CDC)2002Injury Fact Book-2001–2002’US Government Printing OfficeAtlanta, GA
- ClarkSRoseDJ2001Evaluation of dynamic balance among community-dwelling older adult fallers: a generalizability study of the limits of stability testArchives of Physical Medicine and Rehabilitation824687411295006
- FosterEHillegassLJPhillipsSL2004Demonstration program: An interdisciplinary approach at a Falls and Mobility ClinicAnnals of Long Term Care1252732
- GreggEWPereiraMACaspersenCJ2000Physical activity, falls, and fractures among older adults: A review of the epidemiologic evidenceJAGS4888393
- HerwaldtLPottingerJ2003Preventing falls in the elderlyJAGS5111751177
- KingMBTinettME1996A multifactorial approach to reducing injurious fallsClinics in Geriatric Medicine124745598890114
- LedinTKronheadACMollerCMollerMOdkvistLMOlssonB1991Effects of balance training in elderly evaluated by clinical tests and dynamic posturographyJ Vestib Res12129381670146
- NelsonAQuigleyP2002Research Agenda on Risk and Prevention of Falls: 2002–2007, VISN 8Patient Safety Center of InquiryTampa, FL
- RobbinsASRubensteinLZJosephsonKRSchulmanBLOsterweilDFineG1989Predictors of falls among elderly people: Results of two population based studiesArchives of Internal Medicine1491628332742437
- RubensteinL2004Joseph T. Freeman Award Lecture. Comprehensive geriatric assessment: from miracle to realityJournal of Gerontology: Medical Sciences59A54737
- Shumway-CookAHorakFB1986Assessing the influence of sensory interaction on balance: suggestions from the fieldPhysical Therapy661548503763708
- SteadmanJDonaldsonNKalraL2003A randomized controlled trial of an enhanced balance training program to improve mobility and reduce falls in elderly patientsJAGS51684752
- TinettiMEMcAvayGClausE1996Does multiple risk factor reduction explain the reduction in fall rate in the Yale FICSIT trial?American Journal of Epidemiology1444389998712196
- WigglesworthJKDayhoffNESuhrheinrich1996The reliability of four measures of postural control using the Smart Balance MasterJ American Coll Sports Med29S113
- WolfsonLWhippleRDerbyCJudgeJKingMAmermanPSchmidtJSmyersD1996Balance and strength training in older adults: Intervention gains and Tai Chi maintenanceJ Am Geriatr Soc444985068617896