Abstract
Diabetic macular edema (DME) is a leading cause of vision loss in older Americans. Thermal laser treatment remains the mainstay of treatment for DME. Recently, alternative primary treatments for DME have been evaluated. These treatments include intravitreal injections of steroids as well as pharmaceuticals containing antibodies against vascular endothelial growth factor (VEGF). Surgical treatment has been shown to be appropriate in selected cases. We review the evidence and scientific rationale for various primary treatment options in patients with DME. Regular and timely ophthalmologic evaluation remains crucial to recognition and treatment of macular edema in diabetic patients.
Introduction
Diabetes mellitus affects approximately 20% of American adults over the age of 60, and diabetic retinopathy is a leading cause of blindness in older Americans.Citation1 Diabetic retinopathy is also impacting younger age groups as the incidence of diabetes rises in adolescents and younger adults.Citation2 Diabetic retinopathy is therefore a significant public health problem.Citation1 Because vision loss from diabetic retinopathy is painless and usually gradual in onset, ophthalmologic evaluation is necessary to distinguish diabetic retinopathy from other causes of painless vision loss in diabetic patients, such as cataract and retinal vein occlusion. Furthermore, diabetic retinopathy may be present before vision loss occurs, and progressive retinal damage may be overlooked until the disease is advanced. Early diagnosis and prompt medical intervention are important to prevent avoidable loss of vision.
The incidence of diabetic retinopathy increases with duration of disease,Citation2 and retinopathy occurs more frequently in patients with poorly controlled diabetes. Co-morbid conditions such as hypertension and hypercholesterolemia compound the problem. It is therefore imperative that patients with diabetic retinopathy have appropriate management of both their systemic diseases and their ophthalmic condition.Citation3 A thorough review of medical conditions and medications is important, particularly because diabetic retinopathy may be exacerbated by systemic medications such as glitazones, in which case macular edema may resolve with discontinuation.Citation4
Diabetic retinopathy occurs because the retinal vessels are abnormal, either because they proliferate (proliferative retinopathy) or because the vessels are functionally incompetent and leak fluid and lipid into the retina. Visual impairment occurs when edema affects the central retina or macula (diabetic macular edema, or DME). Macular edema is reversible in the early stages but chronic edema may lead to irreversible changes in the retina. In a large cohort study, diabetics with macular edema had a 50% prevalence of visual impairment and a 20% prevalence of blindness, compared to 16% and 4% respectively in diabetic patients without macular edema.Citation5 and contrast the ophthalmic features of macular edema with a normal retina.
Figure 1a Color photograph of a normal macula. The normal retinal vasculature is visible against a relatively homogeneous background, with the central macula (fovea) demonstrating normal pigmentary differences compared to the surrounding tissues.
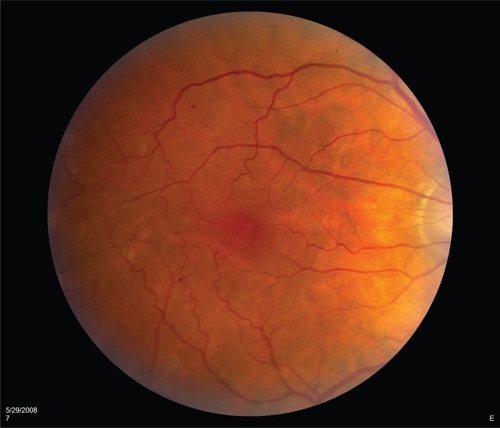
Figure 1b Optical coherence tomography image of a normal macula. The layers of the sensory retina appear homogeneous throughout, with a normal foveal depression.
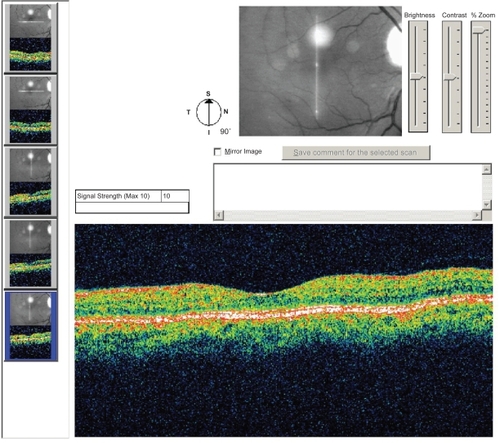
Figure 2a Color photograph of a macula exhibiting diabetic macular edema. Microaneurysms and intra-retinal hemorrhages are visible as red spots. Retinal thickening is visible as a loss of granularity combined with subtle changes in coloration and is best visualized in stereo using slit lamp biomicroscopy. Lipid exudates are visible as yellow streaks or spots, often distributed in a circinate pattern around leaking microaneurysms.
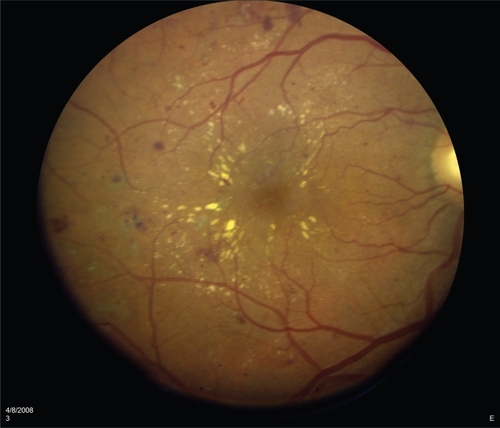
Figure 2b Optical coherence tomography image of a macula exhibiting diabetic macular edema. Thickening of the sensory retina is evident along with typical focal cystoid changes, seen as optically clear cavities within the retina. The foveal depression is lost due to edema.
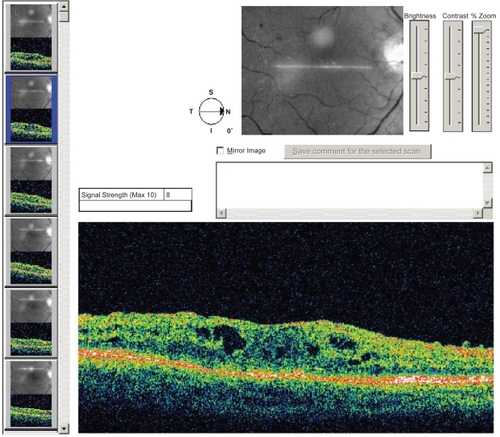
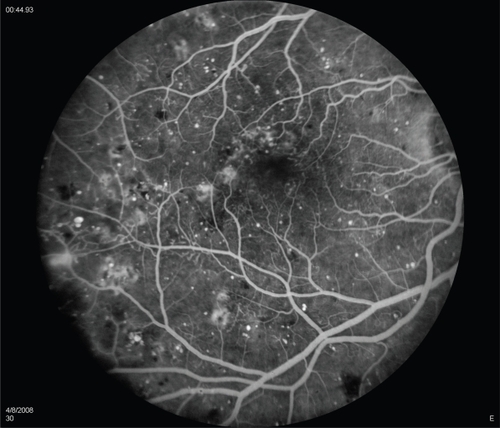
Figure 2c Fluorescein angiography of a macula exhibiting diabetic macular edema. The retinal vascular arcades are visible along with scattered areas of hyperfluorescence throughout the macula, indicating leakage of fluid due to diabetes-induced vascular incompetence.
Thermal laser treatment has been and remains the mainstay for treating macular edema. However, several alternative treatments have emerged over the last few years. Most of these treatments are currently used as second-line therapy for patients with macular edema refractory to thermal laser, but an increasing number of studies have examined first-line use of these alternative therapies. This paper provides an overview of primary treatment options for diabetic macular edema, along with the rationale for each treatment modality.
Thermal laser
Thermal laser is the most established primary treatment for diabetic macular edema. Laser treatment is delivered at a slit lamp using a contact lens on the cornea. Since the sensory retina is transparent, the laser energy is absorbed by vascular structures within the retina or by the pigmented epithelium immediately behind the sensory retina. Focal laser spots may be applied to microaneurysms in order to stop leakage of fluid. A grid pattern of laser spots also may be applied lightly to the pigmented epithelium in areas of more diffuse edema. The pigmented epithelium functions as a pump to remove fluid from the retina, and stimulation with laser spots is thought to stimulate pump function and thereby decrease retinal edema.Citation6
The Early Treatment of Diabetic Retinopathy Study (ETDRS), a large randomized controlled trial completed in 1985, demonstrated that prompt laser treatment of the macula reduced the frequency of vision loss by 50% in diabetic patients with macular edema compared to untreated control subjects.Citation3 In addition, almost half of the patients with poor vision initially demonstrated some improved vision at three years of follow-up. Patients typically need more than one laser treatment and long term follow-up is needed so that recurrent edema can be managed in a timely manner.
Steroids
Diabetic macular edema is caused by a cascade of vascular permeability factors that include the production of interleukin-6 (IL-6) and vascular endothelial growth factor (VEGF). IL-6 and VEGF are present in higher concentrations in eyes with diabetic retinopathy and steroid administration reduces the concentration of these factors with concurrent clinical improvement of macular edema.Citation7,Citation8
There are two ways to deliver steroids into the vitreous cavity. The first is by direct injection into the vitreous cavity (intravitreal injection); triamcinolone is the most frequently used steroid for this purpose. In a recent prospective randomized study of more than 100 patients, intravitreal injection of triamcinolone improved visual acuity and decreased retinal thickness compared to baseline, and neither endpoint was significantly different compared to macular laser treatment alone or laser combined with triamcinolone.Citation9 These findings suggest that triamcinolone treats DME at least as well as laser alone over six months of follow-up, although some patients in the study had received previous laser treatment.Citation9 Intravitreal triamcinolone has also been successfully combined with macular laser treatment as the initial therapy for diabetic macular edema.Citation10,Citation11 In addition, numerous studies have shown that intravitreal steroids reduce macular edema in cases that are refractory to laser treatment, although visual acuity does not consistently improve in these cases, probably due to permanent damage to retinal photoreceptors by chronic edema.Citation12,Citation13
Side effects of intravitreal steroids include accelerated development of cataracts as well as elevated intraocular pressure that may lead to glaucomatous damage to the optic nerve. These complications may require surgical correction.Citation12
A second way to deliver intravitreal steroids is by sustained-release steroid implants. The Posurdex implant (Dexamethasone Posterior Segment Drug Delivery System; Allergan Inc, Irvine, CA, USA) releases dexamethasone into the vitreous cavity for up to six months, while the Retisert implant (fluocinolone acetonide intravitreal implant; Bausch and Lomb Inc, Rochester, NY, USA) releases fluocinolone acetonide. Both implants have been shown to improve vision in patients with diabetic macular edema, but both are relatively expensive and carry side effects similar to intravitreal triamcinolone injections.Citation13
Anti-VEGF therapies
Since VEGF contributes to the development of macular edema, attention has recently focused on intravitreal injections of anti-VEGF antibodies. Antibodies delivered by intravitreal injection bind to VEGF and thereby decrease downstream effects on vascular leakage. Anti-VEGF antibodies were first used to treat patients with exudative age-related macular degeneration (AMD) with dramatic beneficial results. Because of these benefits, anti-VEGF antibodies are now being evaluated in the treatment of macular edema.
Three drugs are currently in use. Bevacizumab (Avastin; Genentech, San Francisco, CA) was approved by the FDA for intravenous use in cancer patients. This drug has been used off-label as an intravitreal injection, first for AMD, and subsequently for a variety of other ocular diseases including macular edema.Citation14 Ranibizumab (Lucentis; Genentech, San Francisco, CA) is FDA-approved for intravitreal injection in patients with AMD, and has been used off-label for other ocular diseases including diabetic macular edema.Citation15 Pegaptanib (Macugen; OSI Pharmaceuticals, Melville, NY) was FDA-approved for intravitreal injection in patients with AMD before the advent of ranibizumab and bevacizumab. Pegaptanib has fallen out of favor for use in AMD patients but has been studied in patients with diabetic macular edema.
Two prospective randomized controlled trials recently demonstrated greater improvements in visual acuity, albeit with just trhee months follow-up, in patients receiving intravitreal bevacizumab compared to controls receiving laser treatment.Citation16,Citation17 Bevacizumab has also produced improvements in visual acuity and retinal thickness in patients who are refractory to initial laser treatment.Citation18,Citation19 The initial results are promising but follow up is limited. Long-term follow-up may help to establish the utility of intravitreal bevacizumab for diabetic macular edema, as well as determine the regimen of treatment to maintain vision and prevent recurrence.
Data regarding ranibizumab for diabetic macular edema is more limited, likely due to the high price of ranibizumab compared to bevacizumab. Two small prospective studies demonstrated maintenance or improvement of vision in patients treated primarily with ranibizumab.Citation20,Citation21
Pegaptanib was shown in a Phase II randomized controlled trial to decrease vision loss and increase vision gain compared to a sham medication, with a decreased need for subsequent photocoagulation.Citation22 However, pegaptanib was not directly compared to thermal laser in this study.
Side effects of intravitreal anti-VEGF injections are rare and include retinal detachments, which are most likely due to the injection procedure itself rather than the pharmaceutical compound (the risk of retinal detachment is common to other intravitreal injections such as triamcinolone). Similarly, endophthalmitis is a rare complication of intravitreal injection and is likely related to the injection itself rather than specific pharmaceutical characteristics.Citation23 Intravitreal bevacizumab and ranibizumab do not result in significant elevations of intraocular pressure nor have they been shown to accelerate cataract formation to any appreciable degree.
Vitrectomy
Pars plana vitrectomy is a surgical procedure in which the vitreous gel is removed from the eye. Some cases of diabetic macular edema are associated with vitreous traction on the retina. Vitrectomy has been shown in several studies to improve vision in patients with traction-associated macular edema.Citation24,Citation25 Vitrectomy has also been studied in patients without a tractional component, with mixed results.Citation26–Citation28
Conclusion
Early detection of diabetic retinopathy and prompt treatment of macular edema are important for preserving vision in the diabetic patient. Thermal laser is the mainstay of treatment for diabetic macular edema, and strong evidence supports the use of laser treatment to decrease progressive vision loss. Diabetic eye disease is a major cause of vision loss in working age American adults, resulting in hundreds of millions of dollars in direct and indirect medical expenses each year.Citation29 Intravitreal steroid and anti-VEGF injections may be used in lieu of or in combination with thermal laser to limit vision loss and in some cases improve vision. However, data on the long term results for these newer modalities is limited. The next few years may see a shift in the primary therapy of macular edema as more data become available about the efficacy of intravitreal steroids and anti-VEGF antibodies.
Disclosure
The authors report no conflicts of interest in this work.
References
- Centers for Disease Control and PreventionNational Diabetes Fact Sheet: General information and national estimates on diabetes in the United States, 2005Atlanta, GACenter for Disease Control2005
- EppensMCCraigMECusumanoJPrevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetesDiabetes Care2006291300130616732012
- Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research groupArch Ophthalmol1985103179618062866759
- LiazosEBroadbentDMBeareNKumarNSpontaneous resolution of diabetic macular oedema after discontinuation of thiazolidenedionesDiabet Med20082586086218644073
- MossSEKleinRKleinBEThe 14-year incidence of visual loss in a diabetic populationOphthalmology199810599810039627648
- BandelloFLanzettaPMenchiniUWhen and how to do a grid laser for diabetic macular edemaDoc Ophthalmol19999741541910896358
- AdamisAPMillerJWBernalMTIncreased vascular endothelial growth factor levels in the vitreous of eyes with proliferative diabetic retinopathyAm J Ophthalmol19941184454507943121
- BrooksHLJrCaballeroSJrNewellCKVitreous levels of vascular endothelial growth factor and stromal-derived factor 1 in patients with diabetic retinopathy and cystoid macular edema before and after intraocular injection of triamcinoloneArch Ophthalmol20041221801180715596583
- LamDSChanCKMohamedSIntravitreal triamcinolone plus sequential grid laser versus triamcinolone or laser alone for treating diabetic macular edema: six-month outcomesOphthalmology20071142162216717459479
- CelliniMPazzagliaAZampariniELeonettiPCamposECIntravitreal vs subtenon triamcinolone acetonide for the treatment of diabetic cystoid macular edemaBMC Ophthalmol20088518366650
- ShimuraMNakazawaTYasudaKShionoTNishidaKPretreatment of posterior subtenon injection of triamcinolone acetonide has beneficial effects for grid pattern photocoagulation against diffuse diabetic macular oedemaBr J Ophthalmol20079144945417077114
- Vasconcelos-SantosDVNehemyPGSchachatAPNehemyMBSecondary ocular hypertension after intravitreal injection of 4 mg of triamcinolone acetonide: incidence and risk factorsRetina20082857358018398360
- FurlaniBAMeyerCHRodriguesEBEmerging pharmacotherapies for diabetic macular edemaExpert Opin Emerg Drugs20071259160317979601
- HurwitzHFehrenbacherLNovotnyWBevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancerN Engl J Med20043502335234215175435
- RosenfeldPJMoshfeghiAAPuliafitoCAOptical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degenerationOphthalmic Surg Lasers Imaging20053633133516156152
- ScottIUEdwardsARBeckRWA phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edemaOphthalmology20071141860186717698196
- SoheilianMRamezaniABijanzadehBIntravitreal bevacizumab (avastin) injection alone or combined with triamcinolone versus macular photocoagulation as primary treatment of diabetic macular edemaRetina2007271187119518046223
- HaritoglouCKookDNeubauerAIntravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edemaRetina200626999100517151486
- KumarASinhaSIntravitreal bevacizumab (Avastin) treatment of diffuse diabetic macular edema in an Indian populationIndian J Ophthalmol20075545145517951903
- ChunDWHeierJSToppingTMDukerJSBankertJMA pilot study of multiple intravitreal injections of ranibizumab in patients with center-involving clinically significant diabetic macular edemaOphthalmology20061131706171217011952
- NguyenQDTatlipinarSShahSMVascular endothelial growth factor is a critical stimulus for diabetic macular edemaAm J Ophthalmol200614296196917046701
- CunninghamETJrAdamisAPAltaweelMA phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edemaOphthalmology20051121747175716154196
- JonasJBSpandauUHSchlichtenbredeFShort-term complications of intravitreal injections of triamcinolone and bevacizumabEye20082259059118292795
- GandorferAMessmerEMUlbigMWKampikAResolution of diabetic macular edema after surgical removal of the posterior hyaloid and the inner limiting membraneRetina20002012613310783944
- HarbourJWSmiddyWEFlynnHWJrRubsamenPEVitrectomy for diabetic macular edema associated with a thickened and taut posterior hyaloid membraneAm J Ophthalmol19961214054138604734
- FigueroaMSContrerasINovalSSurgical and anatomical outcomes of pars plana vitrectomy for diffuse nontractional diabetic macular edemaRetina20082842042618327133
- PatelJIHykinPGSchadtMLuongVFitzkeFGregorZJPars plana vitrectomy with and without peeling of the inner limiting membrane for diabetic macular edemaRetina20062651316395132
- YanyaliAHorozogluFCelikENohutcuAFLong-term outcomes of pars plana vitrectomy with internal limiting membrane removal in diabetic macular edemaRetina20072755756617558316
- HoganPDallTNikolovPEconomic costs of diabetes in the US in 2002Diabetes Care20032691793212610059