Abstract
Background
To report a case of peripheral polypoidal choroidal vasculopathy (PCV) which was treated successfully.
Methods
Interventional case report. Best-corrected visual acuity measurements (BCVA), slit-lamp examination, fundus biomicroscopy, fluorescein angiography (FFA), and indocyanine green angiography (ICGA) were performed at baseline examination and during the follow-up period. The patient underwent ICGA-guided argon laser to treat the active polyps.
Results
An 82-year-old Caucasian man presented complaining of sudden deterioration of peripheral vision in his left eye (LE). His previous ocular history was associated with advanced age-related macular degeneration (AMD) involving both eyes (BE). Fundus examination revealed macular scars in BE and a large hemorrhagic pigment epithelial detachment (PED) temporal to the macula in the LE. ICGA revealed active polyps at the margins of the PED. The patient underwent ICGA-guided argon laser to treat the active polyps. Six months post-laser, the patient regained his peripheral vision with resolution of the hemorrhagic PED and remains stable until now, one year after treatment.
Conclusions
Appropriate treatment and regular follow-up is important in patients with PCV and peripheral lesions even if central vision is lost.
Introduction
Idiopathic polypoidal choroidal vasculopathy (PCV) is an exudative disorder of the macula. Although its pathogenesis remains unclear, it is generally thought to be an inner choroidal vascular abnormalityCitation1 which usually emanates from the posterior poleCitation1 or less commonly from the peripheral retina.Citation2 We report a case of PCV in the peripheral fundus in a patient with bilateral end-stage age-related macular degeneration (AMD) treated successfully.
Figure 1 A) Color fundus picture of the right eye of our patient showing a macular scar. B) Color-mosaic fundus picture of the left eye (LE) before treatment showing a macular scar and a large hemorrhagic pigment epithelial detachment (PED) temporal to the fovea resembling a choroidal melanoma. C) Late phase of fluorescein angiography of the LE showing hyperfluorescence due to staining of fibrotic tissue at the fovea and hypofluorescence due to masking of the hemorrhagic PED temporal to the fovea. D) Mid phase of Indocyanine green angiography showing hypofluorescence due to the PED with two hot spots at the margins (white arrows).
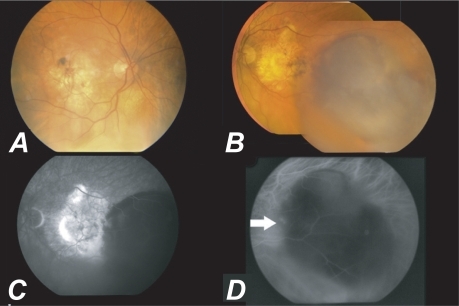
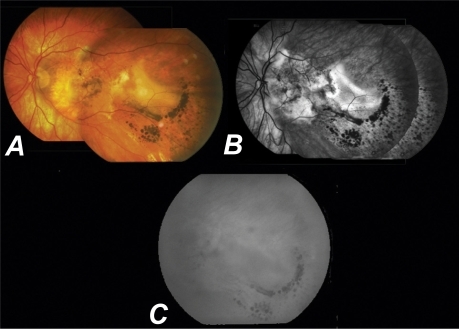
Figure 2 A) Color-mosaic fundus picture of the left eye (LE) six months post-ICGA-guided argon laser showing a macular scar and almost complete resolution of the hemorrhagic pigment epithelial detachment (PED) temporal to the fovea. The appearance remained stable for another six months. B) Late phase of FFA of the LE resolution of the PED temporal to the fovea with hyperfluorescence due to staining of the fibrotic tissue. C) Late phase of ICGA at the same time showing the area corresponding to the PED with no active hot spots.
Case presentation
An 82-year-old Caucasian man presented in our department complaining of sudden deterioration of peripheral vision in his left eye (LE). His previous ocular history was associated with advanced AMD involving both eyes. Best-corrected visual acuity (BCVA) was counting fingers in both eyes. The anterior segments and intraocular pressures were within normal limits in both eyes. Fundus examination revealed scar formation involving the center of the fovea bilaterally. In addition, a large hemorrhagic pigment epithelial detachment (PED) was detected temporal to the macula in the LE
Indocyanine green angiography (ICGA) disclosed the presence of actively leaking polypoidal vessels at the margins of the PED. The diagnosis of peripheral idiopathic PCV in a patient with advance AMD was made. After informed consent was obtained, ICGA-guided argon laser photocoagulation was applied. Six months post-laser, the hemorrhagic PED was resolved. One year later, the patient remains stable and his peripheral vision has significantly improved.
Discussion
In 1990, idiopathic PCV was first described by Yannuzzi and colleaguesCitation1 as a vascular disorder originating from the choroidal circulation. This disorder has been recognized increasingly in recent years as a distinct clinical entity separate from AMD. The pathogenesis of PCV remains unclear. Recent genetic research has shown that PCV and AMD share common genetic factorsCitation3 which may suggest that although PCV and wet AMD have different clinical characteristics, they may share same similar pathophysiologic aspects. In support of the latter, Lafaut and colleaguesCitation4 reported the possible coexistence of AMD and PCV in the same patient histopathologically.
Patients with end-stage AMD, characterized from the development of fibrotic tissue in the fovea, experience a significant loss of central vision. Peripheral retina is rarely affected allowing the patient to maintain some quality in their peripheral or side vision. Modifying the patient’s environment and using available low vision devices and aids, AMD patients can continue to maintain their lifestyle and independence.
Choroidal vascular lesions of PCV are more preferable found in the posterior pole of the retina,Citation4 although further evidence suggests that the lesion could also be found in the peripheral retina up to 63%.Citation3,Citation5
We report a case of peripheral PCV in a male patient with advanced bilateral AMD affecting severely both foveal areas. The initial complain of the patient was deterioration of peripheral vision in addition to the already affected central vision. Such a clinical situation may impair significantly the quality of life of the patient and needs to be promptly identified, diagnosed and treated in order to preserve, in the best possible way, the peripheral vision of the patient.
Currently there are many therapeutics options for PCV. Photodynamic therapy alone or combined with anti-vascular endothelial growth factor treatment showed promising results.Citation6 However, use of a conventional argon laser achieved up to 78% clinical or angiographic resolution of maculopathy for extrafoveal polyps.Citation7 When PCV lesions accompany PED, the lesions are usually located at the margins of PED.Citation8 In our case, ICGA-guided argon laser photocoagulation was selected, since central vision was impaired due to foveal scars and the polyp lesions were extrafoveal and at the margins of the PED.
In our case, treatment with ICGA-guided argon laser photocoagulation was beneficial and resolved the hemorrhagic PED, preserving the peripheral vision of the patient. Appropriate treatment and regular follow-up is important in patients with PCV even if central vision is lost.
Disclosure
The authors report no conflicts of interest or financial support in this work.
References
- YannuzziLASorensonJSpaideRFLipsonBIdiopathic polypoidal choroidal vasculopathy (IPCV)Retina199010181693009
- YannuzziLANogueiraFBSpaideRFIdiopathic polypoidal choroidal vasculopathy: a peripheral lesionArch Ophthalmol199811633823839514497
- KondoNHondaSIshibashiKTsukaharaYNegiALOC387715/HTRA1 variants in polypoidal choroidal vasculopathy and age-related macular degeneration in a Japanese populationAm J Ophthalmol2007144460861217692272
- LafautBAAisenbreySVan den BroeckeCBartz-SchmidtKUHeimannKPolypoidal choroidal vasculopathy pattern in age-related macular degeneration: a clinicopathologic correlationRetina200020665065411131419
- CackettPWongDYeoIA classification system for polypoidal choroidal vasculopathyRetina200929218719118827731
- GomiFTanoYPolypoidal choroidal vasculopthy and treatmentsCurr Opin Ophthalmol200819320821218408495
- LeeMWYeoIWongDAngCLArgon laser photocoagulation for the treatment of polypoidal choroidal vasculopathyEye200923114514817721502
- TsujikawaASasaharaMOtaniAPigment epithelial detachment in polypoidal choroidal vasculopathyAm J Ophthalmol2007143110211117101112