Abstract
To find out clues to differentiate between polymyalgia rheumatica (PMR) and other diseases that mimic PMR. We studied Japanese patients with PMR (n = 7), pseudogout (n = 1), remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome (n = 1), and post-infectious polyarthritis (n = 1). The distribution of inflammation in patients was evaluated using a gallium-67 scintigraphy. We measured serum C-reactive protein (CRP), matrix metalloproteinase-3 (MMP-3), and vascular endothelial growth factor (VEGF) in patients before and after treatment. Further, we compared the clinical course of PMR with that of other diseases that mimic PMR. Patients with pseudogout, RS3PE syndrome, post-infectious polyarthritis manifested similar changes in scintigraphic findings and serum CRP, MMP-3, and VEGF levels to PMR before the treatment. A significant reduction in serum CRP levels at one week after use of nonsteroidal anti-inflammatory drugs (NSAIDs) is a good clue to differentiate pseudogout and post-infectious polyarthritis from PMR. Chondrocalcinosis in the radiographs of joints is also effective to differentiate pseudogout from PMR. A small reduction of CRP levels after NSAIDs use and promptly ameliorated CRP and symptoms by a low-dose steroid therapy, which was commonly observed in patients with PMR, were also found in a patient with RS3PE syndrome. Pitting edema of the back of hands and gallium uptake in metacarpophalangeal (MCP) joints were useful to differentiate RS3PE syndrome from PMR. In conclusion, pseudogout, RS3PE syndrome, post-infectious polyarthritis should be included in the spectrum of diseases mimicking PMR. A promptly decreased serum CRP level by NSAIDs is a good clue to differentiate pseudogout and post-infectious polyarthritis from PMR. Pitting edema of the back of hands and symmetric gallium uptake in MCP joints are characteristic for RS3PE syndrome.
Introduction
Polymyalgia rheumatica (PMR) is an inflammatory rheumatic disease in elderly people. It is a common indication for a long term treatment with steroid in patients based in the community. Although the cause of PMR is largely unknown, the presence of articular synovitis in PMR has been proven by synovial biopsy.Citation1 Recently, we have reported that symmetrical gallium-67 uptake in the shoulders and elevated serum matrix metal-loproteinase-3 (MMP-3) and vascular endothelial growth factor (VEGF) levels as the markers for synovitis in patients with PMR.Citation2 Although bilateral aching and stiffness of shoulders and pelvic girdle of acute or subacute onset are very characteristic for PMR, several other diseases can be present with similar symptoms. Here, we studied a gallium scintigraphic findings, and serum C-reactive protein (CRP), MMP-3 and VEGF levels in patients with diseases that mimic PMR. Further, we discuss clues to differentiate between PMR and other diseases that mimic PMR.
Methods
We studied Japanese patients with PMR (n = 7), pseudogout (n = 1), remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome (n = 1), and post-infectious polyarthritis (n = 1). Diagnosis for PMR had been done using the Hunder’s criteria.Citation3 The distribution of inflammation in patients was evaluated using a gallium-67 scintigraphy whole body scan before the treatment. We measured serum CRP, MMP-3, and VEGF levels as the markers for a synovial inflammation before and after the treatment.Citation4,Citation5 Serum CRP and MMP-3 concentrations were measured by polyclonal antibody-based (Dade Behring, Marburg, Germany) and monoclonal antibody-based (Daiichi Fine Chemical, Co., Ltd., Toyama, Japan) latex agglutination method, respectively. Serum concentrations of VEGF165 (major form of VEGF) were analyzed by enzyme linked immunosorbent assay (ELISA; VEGF165, R&D Systems, Inc, Minneapolis, MN, USA).
Results
Patients with PMR
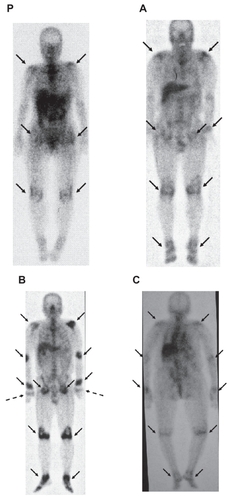
Case P is a 64-year-old woman with PMR (). Symmetrical and bilateral gallium uptake in shoulders, pelvic girdle, and knees were observed. Age of all patients with PMR were over 50 years (). Serum CRP (normal range, <0.3 mg/dL), MMP-3 (normal range, <115 ng/ml), and VEGF (normal range, 17.3–59.7 pg/ml) levels were significantly elevated in patients with PMR before the treatment (). Rheumatic factor (RF), antinuclear antibody (ANA), myeloperoxidase-antineutrophil cytoplasmic antibody (MPO-ANCA), and proteinase-3 (PR3)-ANCA were negative in all PMR patients. Daily administration of 20 mg corticosteroid ameliorated symptoms and significantly decreased serum CRP and VEGF levels (). Although a statistically significant difference between values before and after the treatment was not observed, corticosteroid increased serum MMP-3 levels. Nonsteroidal anti-inflammatory drugs (NSAIDs) did not ameliorate patients’ symptoms and serum CRP levels ().
Table 1 Age, serum CRP, MMP-3, VEGF levels before and after the treatment in patients with PMR, pseudogout, RS3PE syndrome, and post-infectious polyarthritis
Table 2 Changes in serum CRP levels after one week’s treatment using NSAIDs in patients with PMR, pseudogout, RS3PE syndrome, and post-infectious polyarthritis
Figure 1 Gallium-67 scintigraphic findings of patients with polymyalgia rheumatica (P), pseudogout A), remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome B), and post-infectious polyarthritis C). A–C corresponds to case A–C in , respectively. Arrows indicate a gallium uptake. Dotted arrows indicate a gallium uptake in metacarpophalangeal joints in a patient in RS3PE syndrome.
Case A
An 83-year-old man was admitted via emergency room complaining of fever and polyarthralgia, including bilateral wrists, knees, and hip joints. His body temperature was 38.1 °C. Physical examination showed swelling of wrists, knees, and hip joints. Laboratory evaluation on admission was notable for a CRP level of 24.3 mg/dl, and RF, ANA, MPO-ANCA, and PR3-ANCA were negative. Serum MMP-3 and VEGF levels were elevated before the treatment (). His clinical and biochemical characteristics, and symmetrical and bilateral gallium uptake in shoulders, pelvic girdle, knees, and ankles, suggested the presence of PMR (). However, the radiographs of the wrist (), knee (), and hip () showed chondrocalcinosis. Arthrocentesis on the right knee was performed. Calcium pyrophosphate dihydrate crystals were detected in the joint fluid, suggesting that this patient was having pseudogout. Loxoprofen (180 mg/day), NSAIDs, promptly ameliorated his symptoms and decreased serum CRP level (1.2 mg/dl at seven days after the treatment started) (), and also decreased serum MMP-3 and VEGF levels.
Case B
A 65-year-old man was diagnosed as having deep venous thrombosis (DVT) because of edema and pain in lower extremities by a family physician, and was referred to the department of cardiology. The cardiologist found no evidence of DVT and elevated serum CRP level, and then this patient was referred and admitted to our department. He complained of fever, polyarthralgia, and pitting edema in bilateral hands and legs. A gallium-67 scintigraphy revealed symmetrical uptake in shoulders, elbows, wrists, pelvic girdle, knees, and ankles (). In contrast to PMR, a symmetrical gallium uptake in MCP joints was observed. Serum MMP-3 and VEGF levels were significantly elevated (), and RF, ANA, MPO-ANCA, and PR3-ANCA were negative. He was finally diagnosed as having RS3PE syndrome. NSAIDs did not ameliorate patient’s symptoms and serum CRP, however, a low dose of steroid (daily use of 20 mg prednisolone) was very effective in relieving his symptoms and decreasing serum CRP level. Pitting edema on the back of hands and symmetric gallium uptake in MCP joints are characteristic for RS3PE syndrome.
Case C
An 89-year-old woman was admitted to the department of ophthalmology due to left intraocular inflammation, and her left eyeball was extracted. At the fourth day after eyeball extraction, she had fever (39.2 °C), and her serum CRP level was elevated (14.5 mg/dl). Antibiotic therapy was started, but, antibiotic did not decrease her body temperature and serum CRP level (12.1 mg/dl at the fifth day after the beginning of antibiotic therapy), and she was referred and admitted to our department. She complained of fever and polyarthralgia. Serum RF, ANA, MPO-ANCA, and PR3-ANCA were negative. Symmetrical gallium uptake in shoulders, elbows, wrists, knees, and ankles in a gallium-67 scintigraphy () and elevated serum MMP-3 and VEGF levels () suggested the presence of PMR. We stopped use of antibiotics and started to use loxoprofen (60–120 mg/day), NSAIDs. Loxoprofen promptly ameliorated her symptoms and decreased serum CRP level (1.3 mg/dl at the seventh day after the treatment started). Her clinical course suggested that she was having post-infectious polyarthritis due to intraocular inflammation.
Discussion
PMR is a common disease in the elderly. In the United Kingdom, age-adjusted incidence of diagnosed PMR was reported to have increased by 35% between 1990 and 2001.Citation6 However, it is not clear whether this suggests a true increase, increased recognition, or overdiagnosis of PMR. There is considerable uncertainty related to diagnosis in patients with PMR.Citation7
Recently, developing classification criteria for PMR has been reported.Citation8 Most survey respondents agreed on the importance of seven core criteria. These were 1) age ≥ 50 years, 2) duration ≥2 weeks, 3) bilateral shoulder and/or pelvic girdle aching, 4) duration of morning stiffness >45 min, 5) elevated erythrocyte sedimentation rate, 6) elevated CRP, and 7) rapid steroid response. All other core criteria except rapid steroid response were observed in patients with pseudogout and post-infectious polyarthritis, and all core criteria were observed in a patient with RS3PE syndrome, suggesting that this newly developed classification cannot distinguish pseudogout, post-infectious polyarthritis, and RS3PE syndrome from PMR.
Clinical and biochemical characteristics for PMR that we newly found were shown in . Patients with pseudogout, RS3PE syndrome, post-infectious polyarthritis manifested similar changes in scintigraphic findings and serum CRP, MMP-3, and VEGF to PMR. A good response to NSAIDs is an effective clue to differentiate pseudogout and post-infectious polyarthritis from PMR.Citation9,Citation10 An abnormality (chondrocalcinosis) in the radiographs of joints is also effective to differentiate pseudogout from PMR. Serum CRP level (24.3 mg/dl) in our patient (Case A) with pseudogout was quite high. A Korean female patient of calcium pyrophosphate dihydrate crystal deposition disease (CPDD) presenting as an acute polyarthritis also showed significantly elevated serum CRP levels (18.8 mg/dl).Citation11 However, it is too difficult to differentiate CPDD and CPDD + PMR from PMR, especially in elderly patients.Citation12 Therefore, we cannot completely deny a possible existence of an additional inflammatory condition including PMR in Case A.
Table 3 Clinical and biochemical characteristics for polymyalgia rheumatic
A significant difference in gallium scintigraphic findings in RS3PE syndrome as compared with PMR was the presence of gallium uptake in both MCP joints. However, symmetrical gallium uptake was observed in shoulders and pelvic girdle, showing the similar scintigraphic findings to PMR. RS3PE syndrome is a very rare inflammatory arthritis.Citation13 The features of this syndrome are bilateral pitting edema of both hands, sudden onset of polyarthritis, age > 50 years old, seronegative for RF.Citation14 Mild to moderate synovitis of the joints and an association of VEGF with the pathogenesis have been observed in RS3PE syndrome as well as PMR.Citation5,Citation15,Citation16 Elevated serum CRP, MMP-3 and VEGF levels, a bad response to NSAIDs, and rapid steroid response, were observed in our patient with RS3PE syndrome as well as patients with PMR. Pitting edema of the back of hands and symmetric gallium uptake in MCP joints are characteristic for RS3PE syndrome. As neoplasm are common in RS3PE syndrome, but not in PMR. Follow-up evaluation has been suggested to be necessary to observe for the possible occurrence of associated neoplasms.Citation17
In conclusion, pseudogout, RS3PE syndrome, post-infectious polyarthritis should be included in the spectrum of diseases mimicking PMR. A good response to NSAIDs is a good clue to differentiate pseudogout and post-infectious polyarthritis from PMR. Pitting edema of the back of hands and symmetric gallium uptake in MCP joints are characteristic for RS3PE syndrome.
Disclosures
The authors report no conflicts of interest in this work.
References
- SalvaraniCHunderGGMusculoskeletal manifestations in a population-based cohort of patients with giant cell arteritisArthritis Rheum1999421259126610366120
- YanaiHFurutaniNItoKYoshidaHTadaNScintigraphic findings and serum matrix metalloproteinase 3 and vascular endothelial growth factor levels in patients with polymyalgia rheumaticaThe Open General and Internal Medicine Journal200935357
- ChuangTYHunderGGIlstrupDMKurlandLTPolymyalgia rheumatica: a 10-year epidemiologic and clinical studyAnn Intern Med1982976726806982645
- RibbensCMartin y PorrasMFranchimontNIncreased matrix metalloproteinase-3 serum levels in rheumatic diseases: relationship with synovitis and steroid treatmentAnn Rheum Dis20026116116611796404
- MeliconiRPulsatelliLDolzaniPVascular endothelial growth factor production in polymyalgia rheumaticaArthritis Rheum2000432472248011083270
- SmeethLCookCHallAJIncidence of diagnosed polymyalgia rheumatica and temporal arteritis in the United Kingdom, 1990–200Ann Rheum Dis2006651093109816414971
- DasguptaBHutchingsAMattesonELPolymyalgia rheumatica: the mess we are now in and what we need to do about itArthritis Rheum20065551852016874793
- DasguptaBSalvaraniCSchirmerMDeveloping classification criteria for polymyalgia rheumatica: comparison of views from an expert panel and wider surveyJ Rheumatol20083527027718050370
- PeterselDLSigalLHReactive arthritisInfect Dis Clin North Am20051986388316297737
- AnnounNGuernePATreating difficult crystal pyrophosphate dihydrate deposition diseaseCurr Rheumatol Rep20081022823418638432
- SongJSLeeYHKimSSParkWA case of calcium pyrophosphate dihydrate crystal deposition disease presenting as an acute polyarthritisJ Korean Med Sci20021742342512068153
- Pego-ReigosaJMRodriguez-RodriguezMHurtado-HernandezZCalcium pyrophosphate deposition disease mimicking polymyalgia rheumatica: a prospective followup study of predictive factors for this condition in patients presenting with polymyalgia symptomsArthritis Rheum20055393193816342107
- McCartyDJO’DuffyJDPearsonLHunterJBRemitting seronegative symmetrical synovitis with pitting edema. RS3PE syndromeJAMA1985254276327674057484
- OliveAdel BlancoJPonsMVaqueroMTenaXThe clinical spectrum of remitting seronegative symmetrical synovitis with pitting edema. The Catalan Group for the Study of RS3PEJ Rheumatol1997243333369034993
- PulsatelliLDolzaniPSilvestriTSynovial expression of vasoactive intestinal peptide in polymyalgia rheumaticaClin Exp Rheumatol20062456256617181926
- ArimaKOriguchiTTamaiMRS3PE syndrome presenting as vascular endothelial growth factor associated disorderAnn Rheum Dis2005641653165516227418
- TriplettLMPfisterAKThe clinical entity of remitting seronegative synovitis with pitting edema (RS3PE syndrome)W V Med J20019730230411828677
