Abstract
Goals
Recent findings suggest the prevalence of osteoporosis among men is under-recognized. The patient population of the Veterans Health Administration (VA) is predominantly male and many elderly veterans may be at risk of osteoporosis. Given the lack of data on male osteoporosis, we provide initial insight into diagnostic procedures for patients at one VA medical center.
Procedures
A review and descriptive analysis of patients undergoing radiological evaluation for osteoporosis at one VA medical center.
Results
We identified 4,919 patients who had bone mineral density scans from 2001–2004. VA patients receiving bone mineral density scans were commonly white, male, over age 70 and taking medications with potential bone-loss side effects.
Conclusions
While further research is needed, preliminary evidence suggests that the VA screens the most vulnerable age groups in both genders. Heightened awareness among primary care providers of elderly male patients at risk of osteoporosis can lead to early intervention and improved management of this age-related condition.
Introduction
Osteoporosis is a medical condition defined by low bone density and reduced bone strength that increases the risk of fractures. Largely associated with post-menopausal Caucasian women, recent findings suggest the prevalence of osteoporosis among elderly men is under-recognized. The Surgeon General identifies males as a population facing barriers to optimal bone health, stating that 13% of Caucasian men aged 50 and over will have an osteoporotic fracture of the wrist, spine, or hip (CitationDHHS 2004). Research on male osteoporosis is limited with no national guidelines for prevention or treatment expressly for men (CitationBinkley and Krueger 2002; CitationCampion and Maricic 2003; CitationVonderacek and Hasen 2004). Adler has studied osteoporosis in veterans served in pulmonary clinics and using glucocorticoids (CitationAdler and Hochberg 2003; CitationAdler et al 2003), but we are unaware of any studies or internal directives addressing the Veterans Health Administration’s (VA) diagnostic procedures for the wider range of patients who may be at risk of osteoporosis. The purpose of our analysis is to describe patients who have received a radiological evaluation of osteoporosis (ie, those considered high risk) at one VA medical center (VAMC), providing insight into existing diagnosis procedures in a large healthcare system serving a predominantly male population.
Background
Veterans and male osteoporosis
The VA operates the largest integrated healthcare system in the country. There is ample evidence that VA patients are more medically needy than typical patients outside this system (CitationKazis et al 1998; CitationAgha et al 2000; CitationYu et al 2003; CitationDeSalvo et al 2005; CitationSingh et al 2005), and many veterans may have multiple risk factors for osteoporosis. For instance, veterans have higher rates of smoking (CitationVHA PHSHCG 2005) and homeless veterans served by the VA have a myriad of nutritional deficiencies and substance abuse problems (CitationGamache et al 2000; CitationO’Toole et al 2003; CitationNyamathi et al 2004). In addition, 37% of all veterans in the United States are aged 65 and older (CitationCowper et al 2000). The presence of these risk factors suggests significant clinical and financial benefits from early detection of osteoporosis. Nonetheless, several researchers have determined that within the VA attention given to male osteoporosis is inadequate (CitationColon-Emeric et al 2000; CitationRiley et al 2002; CitationAdler and Hochberg 2003).
Indicators for osteoporosis are aimed towards older women (CitationNOF 2005), although there are differences in the presentation of osteoporosis by gender (CitationKamel 2004). Men have approximately 10% greater peak bone mass, are typically older by the onset of osteoporosis, and are less likely to have an associated fracture than women (CitationKamel 2004). When older men do have a hip fracture, they are at greater risk for institutionalization and mortality compared with women (CitationCenter et al 2000; CitationStevens and Olson 2000; CitationDavidson et al 2001; CitationFransen al 2002; CitationBass et al 2007). Due to advances in life expectancy, the number of individuals suffering from osteoporosis and related fractures will likely increase, and so will the economic burden. Lifetime costs for treating a hip fracture from one community-based study were estimated at US$81,300 (CitationBraithwaite et al 2003).
Risk factors for males are known and many apply to both genders (see ). Diseases and medical conditions which may cause osteoporosis include endocrine (such as thyroid disease), gastrointestinal (malabsorption issues with Vitamin D and calcium), chronic renal failure, malignancy, systemic mastocytosis, and idiopathic hypercalciuria (CitationCompston 2001; CitationNOF 2005). Glucocorticoids and other medications such as anticonvulsants, methotrexate, excessive thyroid hormone, cyclosporine A, antiandrogens, heparin, and cholestyramine can result in decreased bone density (CitationCompston 2001; CitationNOF 2005; CitationSaad 2005; CitationShahinian et al 2005; CitationTrant and Holbert 2006) .
Table 1 General risk factors for osteoporosis in men
Bone density scans
Several types of machines can measure bone density: only those used at the VAMC analyzed are included here. Dual-energy X-ray absorptiometry (DXA) scans are the standard for bone mineral density measurement and are used primarily for prefracture diagnosis of osteoporosis (CitationACOG 2004). With the use of X-rays, a two-dimensional image is generated, permitting the caluculation of bone mineral density (CitationWahner and Fogelman 1994). A central DXA is used for sites on the axial skeleton (eg, spine, femoral neck, hip) whereas a peripheral DXA is for the appendicular skeleton (eg, wrist, heel). DXAs expose patients to low levels of radiation and administration is typically uncomplicated, but there are some disadvantages. Classifications are site-dependent: a patient may have a healthy spine measurement, but an osteoporotic hip. DXA machines have no universal calibration system so results may differ depending on the actual machine used. Machines cannot identify an unsatisfactory scan acquisition due to operator error, insufficient scan speed or patient movement. A quantitative computed tomography (CT) may also be used to measure bone density in the spine using a conventional tomgraphy unit (CitationTrand and Holbert 2006). Unlike a DXA machine which is used only for bone mineral density measurement, clinics that have CT units can use these machines for diagnosing multiple conditions. However, CT results do not always correspond well with a DXA and patients are exposed to higher levels of raditaion. Definitive data pertaining to the effectiveness of any screening and subsequent treatment for osteoporosis is lacking (CitationKern et al 2005; CitationRaisz 2005), despite the widespread use of scans. The cost to the VAMC for administering each DXA scan in 2004 was US$189.34; CT scans cost US$130.16 (CitationVHA 2005).
Data source and methods
The sample for this study was drawn from one of the nation’s busiest VAMCs, located in the state with the largest number of elderly veterans (CitationCowper et al 2000). The VAMC encompasses one hospital, three regional outpatient clinics, and five smaller community-based outpatient clinics. Of the nine facilities, only the hospital has a DXA machine (a Lunar DPX-1Q; Lunar, Madison, Wisconsin, USA). The outpatient clinics use an axial CT bone density scan or refer patients to the hospital. The data were assembled from local the Veterans Health Information Systems and Technology Architecture (VistA), which is an integrated system of software applications assisting with patient healthcare and management at VA facilities (CitationVIReC 2004). Each VAMC maintains its own VistA which contains administrative and some clinical information such as patients’ medical and healthcare utilization histories, demographics, practitioner information, diagnoses, and procedures (CitationVIReC 2004). All patients treated at VA medical centers are included in the files which are updated during office visits or as part of administrative processes.
We performed a search of VistA by extracting all files from the financial year (October 1st–September 30th) 2000–2004 for patients receiving any of three procedures defined by common procedure terminology (CPT) codes 76070 (axial CT bone density scan), 76075 (axial skeleton study DXA) or 76076 (peripheral study DXA). Screening males with a DXA machine began late in 2000; therefore, our period of measurement is 2001–2004. Descriptive statistics of scan recipients and time trends were examined by select demographics, primary and secondary diagnoses, and the utilization of potential bone-loss drugs. Descriptive statistics include counts, percentages, and chi-square statistics testing whether the composition of the scan population remained constant over time. Analyses were conducted with SAS 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
Demographics
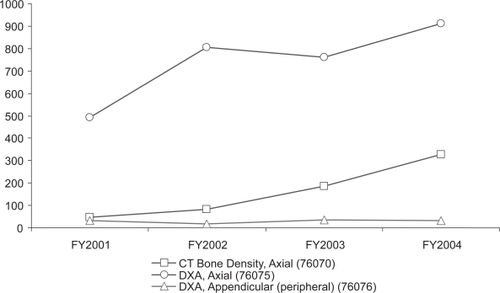
We identified 4,919 patients who had 6,743 scans. The total number of all scans rose by approximately 5% annually from 2001 to 2003, with a 14% jump in 2004. Peripheral DXA scans remained a very small proportion of total scans, as seen in . Comparing the two axial skeleton procedures, the trend from 2001–2004 shows a significant increase (p < 0.001) of CT scans for both males () and females. Fifty-five percent (3,730) of the scans over the four year time period were given to men. Whereas the total number of scans given to women decreased, the share of scans performed for male patients increased from 37% in 2001 to 66% in 2004, a statistically significant change in the gender composition (p < 0.001).
Table 2 Annual scan procedures (CPT codes) by gender
Figure 1 Bone mineral density scans for males, 2001–2004.
Abbreviations: CT, computed tomography; DXA, dual-energy X-ray absorptiometry, FY, financial year.
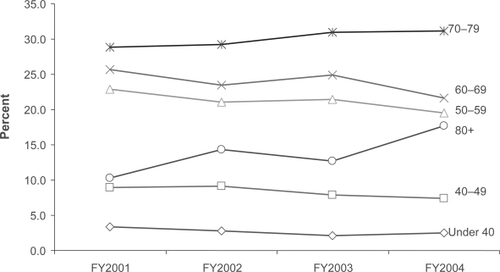
The four year annual average confirmed that men in the age group 70–79 received the most scans (). Over half (54%) of male scans were given to those between the ages of 60 and 79. In contrast, the largest group of females was in the 50–59 range, accounting for 36% of scans over the four year span. For women, this age group constantly composed the largest proportion of scans. For men the most consistent and significant growth in scans was for the aged 80 and over group (). Age distribution changed significantly over time for both genders (p < 0.001).
Table 3 Age distribution (percentages)* by gender of scan recipients by first and last year of study, including four year annual average
Figure 2 Trends for male scan recipients by age, 2001–2004.
Abbreviations: FY, financial year.
Since there was little change in the sample by race, we report the annual average from 2001–2004. The majority (74%) of male scan recipients were identified as non-Hispanic whites. An average of 18% of male scan recipients did not have a specified race recorded, as is the case for VA records in general. Five percent were black. Numbers in the remaining categories (American Indian/Alaskan Native, Asian, and Hispanic) were too small to report. The race distribution of females was similar, with a larger percentage (24%) of unknown race.
Common diagnoses
We report the four years combined of diagnoses information since there was no change over time in the types of diagnoses for scan recipients during their inpatient stay or clinic visit. There was little variation by gender in the primary admitting diagnoses for inpatients who received bone density scans. Most inpatients were seen for either multiple or orthopedic rehabilitation, or aftercare from surgery. Older patients had a higher frequency of heart disease. Hyperlipidemia was the common secondary diagnosis for both genders in most age groups (hypertension is the most frequent secondary diagnosis of all VA patients, regardless of primary admitting diagnosis). Primary diagnoses in the outpatient setting were exclusively for counseling.
While not among the most common diagnoses, a sizable portion of male patients screened had spinal cord injury. In 2003, these patients composed 11% of all those receiving bone density scans. Since every spinal cord injury patient had a positive diagnosis, it became routine practice became to treat most spinal cord injury patients for osteoporosis, reducing—and eventually eliminating—the scans ordered by the Spinal Cord Injury Clinic service.
Medication use
shows the percentage of scan recipients who either had a prescription for or received intravenously any of the medications listed above as damaging to the skeleton (glucocorticoids, excessive thyroid hormones, anticonvulsants, methotrexate, cyclosporine A, anti-androgens, heparin, and cholestyramine). Data on dosage or duration was not available for analysis. Steroids were the most common drug for both genders. One quarter of male scan patients and 20% of females had a prescription for Gabapentin. Levothyoxine had a much larger share of female patients. From 2001–2004, the proportion of males with these prescriptions converged to the level observed in females, approximately 55%, which had remained relatively stable with no statistically significant change (p = 0.18; data not shown).
Table 4 Scan patients (%)* receiving drugs with potential bone-loss side effects 2001–2004
Discussion
By 2004, the large VAMC examined here had concentrated the delivery of bone density scans in the hospital setting, though approximately one quarter was performed at outpatient clinics. While the hospital utilized a DXA machine, the outpatient clinics used CT scans. Almost all the growth in CT scans was accounted for by one outpatient clinic. Why scans were increasing at that site could not be determined. The decrease in the number of axial DXA scans from 2002 to 2003 may have been influenced by the policy of the Spinal Cord Injury Clinic to no longer send its patients for DXA scans. The low frequency of peripheral DXAs reflects appropriate standard of care since these scans are not used for diagnosis.
The composition of the scan population did not remain constant over the years examined. By 2004, the typical patient receiving a bone mineral density scan in this VAMC was male. There is no clear explanation for the increase in male scans. New primary providers (who order scans) may have been hired, provider behavior may have changed, or access may have been easier for male patients beginning in 2000 when the DXA machine was moved from the Women’s Clinic to Radiology due to space constraints. Male scan patients were significantly older by 2004 than in 2001, and older than women receiving scans. Conversely, the average age for women decreased over the four year span, though two-thirds of women scanned still were post-menopausal. This supports the view that osteoporosis manifests later in men than women and suggests that the VA screens the most vulnerable age groups in both genders. The decrease in scans ordered from the Spinal Cord Injury Clinic whose patients tend to be younger may also have contributed to the age shift. Generalizations from analysis of the race variable are problematic due to the large proportion of missing values, but at least 74% of male and 67% of female scan recipients were Caucasian. These Caucasian majorities may reflect the VA patient population served at this particular VAMC (predominantly white), or show awareness by clinicians regarding the heightened risk for this racial group.
Primary and secondary diagnoses of scan recipients did not appear different from what is expected in the general elderly patient population. Rehabilitation, aftercare from surgery, counseling, hypertension, and hyperlipidemia were common. High-risk conditions such as thyroid disease or metastatic prostate cancer were unevenly distributed.
VA clinicians are monitoring patients using drugs with potential bone-loss side effects. The most common medications taken by scan patients were steroids. While short-term steroid use causes little concern, steroid-induced osteoporosis can develop in patients whose usage extends beyond 3 months (CitationVan Staa et al 2000). The second largest medication group was anticonvulsants. Some anticonvulsant use is accounted for by the uniqueness of this scan population: approximately half of the spinal cord injury patients take gabapentin. There is disagreement as to the association of this newer anticonvulsant with osteoporosis (CitationPack and Morrell 2001; CitationAsconape 2002), but we included gabapentin as it is in the class of drugs historically associated with potential bone loss. Levothyoxine had a larger share of female patients, explained by the higher frequency of thyroid problems in women. As with steroids, data on duration and dosage of thyroid medication to determine if use were “excessive” would have been useful. Over the four year time span, the percent of men receiving scans who were taking the aforementioned drugs fell and by 2004 mirrored that of women. The reasons for this convergence may be coincidental or due to systematic change in physician practice (ie, fewer male patients were prescribed these medications, or fewer male patients given these medications were being screened). We were unable to determine which was more likely. It is important to note that these pharmaceutical records may be incomplete for patients who also seek care outside the VA.
There are several limitations of our study in addition to those explained above. This research describes patients at one VAMC, so results may not necessarily be generalized to national patient populations. In addition, some patients may have been receiving care outside the VA, so some patient-level data may be absent. Complete information on lifestyle behaviors, such as smoking, was lacking. We did not have information on which clinics or providers ordered the scans, nor the test results. Finally, our results are suspect to the general shortcomings of using a chiefly administrative database.
Conclusions
The large VAMC examined here averaged 1,900 bone mineral density scans annually by 2004. In general, VA patients receiving bone mineral density scans are white, male, over age 70, and taking medications with potential bone-loss side effects. This is a different group from the female patient population usually screened for osteoporosis outside the VA. Our findings suggest that VA diagnostic procedures target high-risk patients in their population of primarily elderly males, indicating appropriate resource utilization. The larger question is how much of the high-risk patient population is screened.
Osteoporosis is a serious health issue that is not confined to elderly women. Fortunately osteoporosis is largely preventable and treatable. Primary care providers may help elderly male patients better manage osteoporosis through early detection. Performing bone density scans in men at risk for osteoporosis can facilitate timely treatment and may reduce the incidence of debilitating, costly fractures.
Acknowledgements
This research was supported by the Department of Veterans Affairs, Veterans Health Administration at the James A Haley VAMC’s Patient Safety Center of Inquiry in Tampa, Florida. The views expressed are the authors’ own and do not necessarily represent those of the Department of Veterans Affairs. The research was approved by the local Institutional Review Board. The authors wish to thank Dustin French, PhD and Jeff Harrow, MD, PhD for helpful comments and suggestions.
References
- AdlerRAHochbergMC2003Suggested guidelines for evaluation and treatment of glucocortic-induced osteoporosis for the Department of Veterans AffairsArch Intern Med16326192414638562
- AdlerRAFunkhouserHLPetkovVI2003Osteoporosis in pulmonary clinic patients: does point-of-care screening predict central dual-energy X-ray absorptiometry?Chest12320121812796183
- AghaZLofgrenRPVanRuiswykJV2000Are patients at the Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource useArch Intern Med16032525711088086
- [ACOG] American College of Obstetricians and Gynecologists2004Osteoporosis: ACOG Practice Bulletin No. 50Obstet Gynecol130203216
- AsconapeJJ2002Some common issues in the use of antiepileptic drugsSemin Neurol22273912170391
- BassEFrenchDDBradhamDDRubensteinLZ2007Risk-adjusted mortality rates of elderly veterans with hip fracturesAnn EpidemiolIn press.
- BinkleyNKruegerD2002Osteoporosis in menWMJ101283212152513
- BraithwaiteRSNanandaFWongJB2003Estimating hip fracture morbidity, mortality and costsJ Am Geriatr Soc513647012588580
- CampionJMMaricicMJ2003Osteoporosis in menAm Fam Physician6715212612722852
- CenterJRNguyenTVSambrookPN2000Hormonal and biochemical parameters and osteoporotic fractures in elderly menJ Bone Miner Res1514051110893691
- Colon-EmericCYballeLSloaneR2000Expert physician recommendations and current practice patterns for evaluating and treating men with osteoporotic hip fractureJ Am Geriatr Soc4812616311037013
- CompstonJ2001Secondary causes of osteoporosis in menCalcif Tissue Int69193511730248
- CowperDYuWKubalJD2000VA Health Care Atlas FY 2000. Rehabilitation Outcomes Research Center. [online]. Accessed January 20, 2006. URL: http://www1.va.gov/rorc/products.cfm
- DavidsonCWWilkinsonTJSainsburyR2001Hip fracture and mortality: can we do better?N Z Med J1143293111548098
- [DHHS] Department of Health and Human Services, Public Health Service, Office of the Surgeon General2004Bone Health and Osteoporosis: a Report of the Surgeon GeneralWashington, DCUS Government Printing Office
- DeSalvoKBFanVSMcDonell2005Predicting mortality and health-care utilization with a single questionHealth Serv Res1012344616033502
- FransenMWoodwardMNortonR2002Excess mortality or institutionalization after hip fracture: men are at greater risk than womenJ Am Geriatr Soc506859011982669
- GamacheGRosenheckRATesslerR2000Factors predicting choice of provider among homeless veterans with mental illnessPsychiatr Serv511024810913456
- KamelHK2004Osteoporosis in the aging maleAnnals of Long-Term Care12405
- KazisLERenXSLeeA1998Health-related quality of life in patients servered by the Department of Veteran Affairs: results from the Veterans Health StudyArch Intern Med158626329521227
- KernLMPoweNRLevineMA2005Association between screening for osteoporosis and the incidence of hip fractureAnn Intern Med1421738115684205
- [NOF] National Osteoporosis Foundation2005Prevention: Who’s at risk? [online]. Accessed January 20, 2006. URL: http://www.nof.org/diseasefacts.htm
- NyamathiASandsHPattatucci-AragonA2004Perception of health status by homeless US veteransFam Community Health27657414724503
- O’TooleTPConde-MartelAGibbonJL2003Health care of homeless veteransJ Gen Intern Med189293314687279
- PackAMMorrellMJ2001Adverse effects of antiepileptic drugs on bone structure: epidemiology, mechanisms and therapeutic implicationsCNS Drugs56334211524035
- RaiszLG2005Screening for osteoporosisN Engl L Med35316471
- RileyRLCarnesMLGudmundssonA2002Outcomes and secondary prevention strategies for male hip fracturesAnn Pharmacother36172311816248
- SaadF2005Bone loss in prostate cancer: evaluation, treatment and preventionCan J Urol12Suppl 171615780171
- SinghJABorowskySJNugentS2005Health-related quality of life, functional impairment and healthcare utilization by veterans: veterans’ quality of life studyJ Am Geriatr Soc531081315667386
- ShahinianVBKuoYFFreemanJL2005Risk of fracture after androgen deprivation for prostate cancerN Engl J Med3521546415647578
- StevensJAOlsonS2000Reducing falls and resulting hip fractures among older womenMMWR4931215580729
- TrantJHolbertBL2006Bone mineral testing: an updateFederal Practitioner23427
- Van StaaTPLeufkensHGAbenhaimL2000Use of oral corticosteroids and risk of fracturesJ Bone Miner Res15993100010841167
- [VHA] Veterans Health Administration, VSSC, DSS/NDE2005Radiology workload and procedure cost by DSS intermediate product (IP) Number [online]. Accessed April 10, 2006. URL: http://klfmenu.med.VHA.gov/dssreports/ndereports/ancillary.htm
- [VIReC] Veterans Administration Information Resource Center2004Veterans Health Information Systems and Technology Architecture (VistA) [online]. Accessed November 8, 2005. URL: http://VHAww.virec.research.med.VHA.gov/DataSourcesName/VISTA/VISTA.htm
- [VHA PHSHCG] VHA Public Health Strategic Health Care Group2005Smoking and Tobacco Use Cessation Program [online]. Accessed January 20, 2006. URL: http://vhaaidsinfo.cio.med.VHA.gov/smoking/TOC.htm
- VonderacekSFHasenLB2004Current approaches to the management of osteoporosis in menAm J Health Syst Pharm6118011115462251
- WahnerHWFogelmanI1994The evaluation of osteoporosis: dual energy X-ray absorptiometry in clinical practiceLondon, EnglandMartin Dunitz
- YuWRaveloAWagnerTH2003Prevalence and costs of chronic conditions in the VHA health care systemMed Care Res Rev60S146S167S15095551