Abstract
Apgar score was devised with the aim to standardize the assessment of newborns. It has been used worldwide to evaluate infants’ condition immediately after birth, to determine their need for resuscitation, and to evaluate the effectiveness of resuscitation. Apgar score was never intended for prediction of outcome beyond the immediate postnatal period; however, since low scores correlate with prenatal and perinatal adversities, multiple studies have examined the relation between the value of Apgar score and duration of low (<7) Apgar score and subsequent death or neurologic disability. This article reviews such studies. The author concludes that the overall evidence shows consistent association of low Apgar scores with increased risks of neonatal and infant death and with neurologic disability, including cerebral palsy, epilepsy, and cognitive impairment. Dose-response patterns have been shown for the value of Apgar score and duration of low score and the outcomes of mortality and neurologic disability. The association of Apgar score <7 at five minutes with increased risks of neurologic disability seems to persist many years postnatally. Some corresponding relative risk estimates are large (eg, four to seven for epilepsy or more than 20 for cerebral palsy), while others are modest (eg, 1.33 for impaired cognitive function). The absolute risks, however, are low (<5% in for most neurologic conditions), and majority of surviving babies with low Apgar scores grow up without disability. The low magnitude of absolute risks makes Apgar score a poor clinical predictor of long-term outcome. Nevertheless, the observed associations point to the importance of fetal and perinatal periods for neurodevelopment.
Introduction
Motivated by lack of a method for standardized assessment of newborns, Virginia Apgar, an anesthesiologist at Columbia University Presbyterian Hospital in New York, developed and described, in a classic 1953 paper,Citation1 her scoring system, intended “to predict survival” and “to compare…methods of resuscitation…and perinatal experience across hospitals and obstetric practices.”Citation2 From a list of “objective signs which pertained in any way to the condition of the infant at birth,”Citation1 Dr Apgar selected “five signs, which could be determined easily and without interfering with the care of the infant…A rating of zero, one or two, was given to each sign depending on whether it was absent or present. A score of ten indicated a baby in the best possible condition” ().Citation1
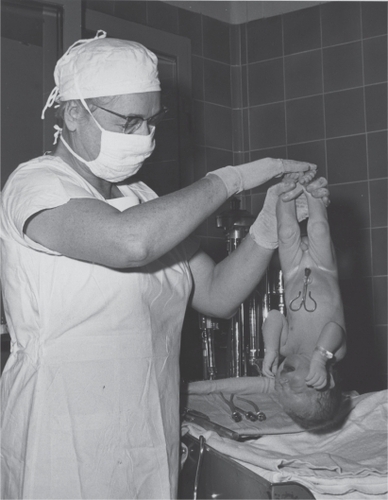
Figure 1 Dr Virginia Apgar holds a newborn baby upside-down to test its reflex irritability – one of the five Apgar score items (1959). Copyright © 2009. Reproduced with permission. Series 6 of the L. Stanley James Papers (MS 0782) in the Mount Holyoke College Archives and Special Collections. Available from: http://mtholyoke.cdmhost.com/u?/p1030coll8,3155.
The five signs of the Apgar score are heart rate, respiratory effort, muscle tone, reflex irritability, and color. The current rating guidelines by the American College of Obstetrician and GynecologistsCitation3 are given in (the guidelines have changed little since the original description of the score).Citation1 In the two reports following the score description, Dr Apgar provided further refinement, observation, and advice regarding its use.Citation2,Citation4 She also presented evidence that Apgar score did in fact measure condition at birth, noting, for example, the inverse association between the value of the score and rates of neonatal death.Citation1,Citation4
Table 1 Components of the Apgar score and scoring guidelinesCitation3
Apgar score was quickly adopted for use worldwide, becoming “common currency”Citation5 among perinatologists. The score was initially measured at one minute after birth. A second measurement, at five minutes of age, was subsequently added, and it has been used to assist in judging the effectiveness of resuscitation, if initiated in response to a low one-minute score.Citation2 Thus, with the exception of a small proportion of infants whose resuscitation begins seconds after birth, one-minute Apgar score reflects a natural condition at one minute after both head and feet emerge from the birth canal. The five-minute Apgar score reflects response to resuscitation among infants in whom it was initiated. Most, but not all, infants with a low one-minute score reach a five-minute score in the 7–10 range.Citation6 If an infant does not improve sufficiently after five minutes, Apgar score may be continuously measured (for up to 25 minutes postpartum) to assess the effectiveness of continuing resuscitation.
In order to reduce the ‘noise’ from the partially subjective nature of the scoring (eg, the “color” component) Dr. Apgar suggested categorizing her score as low (0–3), intermediate (4–6), and normal (7–10).Citation3 The categories were defined based on the observed neonatal mortality patterns. Because very small proportion of newborns have Apgar scores in the 0–3 range, research studies often examine outcomes among infants with low and intermediate scores combined (<7). Therefore, unless specified otherwise, the term ‘low Apgar score’ in this review will refer to a score < 7.
Risk factors for low Apgar scores include abnormalities of gestational length and prenatal growth; congenital malformations; as well as health, demographic, and socioeconomic characteristics of the parentsCitation7,Citation8 (). In developed countries, about 1% of newborns have Apgar score < 7 at five minutes. The reported specific prevalences for year 2000 are 0.7% in DenmarkCitation9 and 1.4% in the United States.Citation10 The lower proportion of infants with scores < 7 in Scandinavia may reflect social and ethnic homogeneity, combined with uniform access to obstetric care. In Sweden, an increase in the prevalence of five-minute Apgar scores < 7 was reported between 1992 and 1997; explanations offered for the rise included increasing prevalence of multiple births, growing immigrant population, and more frequent use of epidural anesthesia.Citation11 Higher prevalence of Apgar scores < 7 is reported for developing countries (eg, 2.8% in Uganda),Citation12 indicating that the distribution of low Apgar score in the population may in fact reflect level of available obstetric care, economic situation, or nutrition.
Table 2 Risk factors for low Apgar scores
Apgar score was never intended to be a predictor of long-term outcome. Nevertheless, its correlation with many maternal and fetal signs of prenatal and intrapartum adversities () has been repeatedly noted. Since some of these traits (such as prematurity) increase the risk neurologic disability, many studies have examined the association of Apgar score with neurologic sequelae. The goal of this article is to provide overview of evidence regarding the association of Apgar scores with mortality and neurologic disability. This review is restricted to evidence from developed countries.
Methods
Between January 1st, 1999 and February 20, 2009, there were 1070 English-language MEDLINE-listed publications with abstracts containing the term ‘Apgar score’ in title or abstract. From these articles and those found by the related-article and manual searches, I primarily selected reports examining association of the Apgar score with mortality and/or neurologic disability published in the last 10 years. This period was chosen because it was judged be relevant to current obstetric practices. I also, however, included studies published before 1999, if they exemplified initial efforts to address an association.Citation4,Citation6,Citation13–Citation15 This review covers 17 studies,Citation4,Citation6,Citation9,Citation11,Citation13–Citation26 examining the outcome of mortality (N = 6)Citation4,Citation6,Citation14,Citation16–Citation18 and/or neurologic disability (N = 14).Citation9,Citation11,Citation13–Citation15,Citation17,Citation19–Citation26
Results
Apgar score and mortality
Studies have consistently shown an inverse relation between the value of Apgar score and neonatal mortality (death within 28 days of life).Citation4,Citation6,Citation14,Citation16,Citation17 The lower the value of Apgar score Citation6,Citation14,Citation16,Citation17 and the longer the durationCitation6,Citation14 of a low score, the greater the proportion of infants dying neonatally. An early report on > 17,000 infants showed that five-minute Apgar score had a stronger association with neonatal mortality than one-minute Apgar score.Citation6 A recent study of > 150,000 malformation-free singleton infants in the USA reported an inverse association between the value of five-minute Apgar score and the incidence of neonatal death. Among infants born preterm (before 37 weeks’ gestation), the risks of neonatal death per 1000 live births were 315, 72, and 6, for those with five-minute Apgar scores 0–3, 4–6, and 7–10, respectively; among term infants (born at 37 weeks’ gestation or later), the corresponding estimates were 244, 9, and 0.2 per 1000 live births. Among term infants in that study, the relative risk (RR) of neonatal death associated with five-minute Apgar score of 0–3 was RR = 1460 (95% confidence interval [CI]: 835–2555). This estimate was eight times greater than the relative risk associated with umbilical-artery pH ≤ 7.0, leading to the conclusion that a five-minute Apgar score < 4 is a better predictor of neonatal death than fetal acidosis among term infants.Citation16 A recent report of a Norwegian registry-based study of term, non-low birth weight (non-LBW, birth weight ≥2500 g) infants estimated risks of neonatal death at 16.4%, 2.3%, and 0.05% among newborns with five-minute Apgar scores of 0–3, 4–6, and 7–10, respectively.Citation17 The study also demonstrated the effect of prolonged Apgar score < 7 on mortality. Compared with infants whose Apgar score was 7–10 at both one and five minutes, the relative risk of neonatal death among infants with one-minute Apgar score 0–3 decreased from 642 (95% CI: 442–934) to 70 (95% CI: 43–114) to 6 (95% CI: 1–24), depending on whether the five-minute score remained in the 0–3 range at five minutes, or rose to the 4–6, or 7–10 level.Citation17 Based on the recent evidence, relative risk for neonatal death associated with five-minute Apgar score 0–3 vs 7–10 ranges from 442 to > 2500 among term infants.Citation16,Citation17
There are also reports of association between Apgar score and longer-term mortality. In a 1981 US study, the reported infant mortality (risk of death within the first year of life) among non-LBW infants with five-minute Apgar scores 0–3 was 15.5%; infant mortality was 5.7% among newborns with five-minute Apgar scores of 4–6; and it was 1.0% among newborns with scores 7–10.Citation14 The estimates were higher for LBW infants and those with prolonged low Apgar scores (59% if a score 0–3 persisted for 20 minutes).Citation14 In Norway, infant mortality among non-LBW children with Apgar scores 0–3, 4–6 and 7–10 at five minutes was 19.2%, 2.7%, and 0.3%. The estimated risks of death in the first eight years of life were 3.0%, 0.4%, and 0.2% for the three Apgar score categories listed above.Citation17
The outcome is poor among the rare infants successfully resuscitated after having Apgar score of 0 that lasts for ten minutes. A review of eight studies, together reporting on 94 such infants, found that 78 of them died within hours or days of birth, while majority of the survivors had severe disability (eg, spastic quadriparesis).Citation18
Apgar score and neurologic disability
summarizes findings of studies reporting relative measures of association between five-minute Apgar scores and neurologic disability.
Table 3 Studies examining the relation between five-minute Apgar score and neurologic disability
Cerebral palsy
Cerebral palsy was one of the first outcomes studied in relation to Apgar score. Nelson and Ellenberg, in the landmark study of 49,000 infants born in twelve US teaching hospitals, examined risk of cerebral palsy within the first seven years of life according to value of Apgar scores and duration of low scores.Citation14 The pattern was similar to that observed for mortality, with lower score values and prolonged duration of low scores conferring increasingly greater risk of cerebral palsy. Among non-LBW infants with an Apgar score < 4 lasting one minute or less, the risk of cerebral palsy within first seven years of life was 0.7%, increasing to 0.9%, 4.7%, 9.1% and 57.1% if the score < 4 persisted for 5, 10, 15, or 20 minutes (as compared with the background risk of 0.2%). A similarly clear monotone increase was lacking among the LBW infants. This was attributed to high neonatal mortality among LBW infants with low Apgar scores.Citation14 Among 87 infants who survived after having Apgar score 0–3 lasting ten minutes or longer and who were free of cerebral palsy, eight were reported to have other handicaps (eg, hearing impairment, mild mental retardation) before age 7.Citation14
In Norway, the reported risks of cerebral palsy in the first eight years of life among infants with Apgar scores 0–3, 4–6, and 7–10 at five minutes were 6.8%, 2.7%, and 0.09%, respectively.Citation17 The relative risk of cerebral palsy decreased in relation to whether Apgar scores 0–3 at one minute remained in that range (RR = 145; 95% CI: 85–248), or achieved by five minutes in the 4–6 range (RR = 57; 95% CI: 38–86) or the 7–10 range (RR = 17; 95% CI: 9–32). Comparisons were relative to infants with Apgar scores 7–10 at both one and five minutes. Similar patterns were observed for other neurodevelopmental outcomes ().Citation17 Comparable findings regarding cerebral palsy were reported in a large registry-based case-control study in Sweden ().Citation22
Epilepsy and seizures
In a registry-based cohort study of > 130,000 singletons born in 1978–2001 in one Danish county, Apgar score < 7 at five minutes was associated with an increased risk of epilepsy hospitalization in the first 12 years of life (RR = 2.4; 95% CI: 1.5–3.8).Citation21 Using data from the same period, but including all births in Denmark (> 1.5 million), another group of investigators assessed risk of in- and outpatient epilepsy diagnosis in relation to one- and five-minute Apgar score and their combination. There were up to 25 years of follow-up for each newborn.Citation9 The study showed a dose-response pattern of association between Apgar score at five minutes and long-term risk of epilepsy. Relative risk estimates (95% CI) were 1.45 (1.35–1.56); 1.89 (1.72–2.07); 2.44 (2.13–2.78); 4.22 (3.78–4.72); and 7.14 (95% CI: 5.79–8.81), respectively, among infants whose five-minute Apgar scores were nine, eight, seven, 4–6, or 1–3, relative to infants with a five-minute score of ten. The magnitude and pattern of association remained essentially unaffected by excluding outpatient epilepsy cases or by considering epilepsy risk only among those without congenital malformation or cerebral palsy. The relative effects were weaker for preterm births, probably because of the high background risk in that group.Citation9 The absolute risks of epilepsy, however, remained comparatively low even in the lowest five-minute Apgar score category (incidence rate, 628 per 100,000).Citation9 Both Danish studies showed stronger association of low Apgar score with epilepsy diagnosed in the first year of life.Citation9,Citation21
An earlier study using data from Swedish population registry reported and association between Apgar score < 7 at five minutes and risk of epilepsy in term, nonmalformed infants.Citation11 Because the length of follow-up is not stated and it is not clear how variable follow-up was addressed, the estimates of association of Apgar score with epilepsy are hard to interpret. The study reports prevalence of (presumably neonatal) seizures of 6.4% for term infants with five-minute Apgar score < 7 as compared with the prevalence of 0.09% among infants with scores in 7–10 range (relative risk = 71; 95% CI: 64–74).Citation11 Finally, in a relatively small Norwegian study, the prevalences of neonatal seizures corresponding to five-minute Apgar scores 0–3, 4–6, and 7–10 were, respectively, 11.6%, 4.7%, and 0.3% among infants free of birth defects or major neurologic impairment at birth.Citation19 The same study reported inverse relation between five-minute Apgar score and proportion of newborns needing ventilator treatments of having feeding difficulties.Citation19
Cognitive function
In 1975, a positive correlation was first reported between Apgar score at one minute and mean Bayley mental and motor scores in children at the age of eight months.Citation13 More recently, using data from parents’ questionnaires and national reports of disability benefits in Norway, five-minute Apgar scores < 7, and particularly five-minute Apgar scores < 4, in combination with symptoms of neonatal encephalopathy, were shown to be associated with increased risks of minor motor impairments, attention-deficit hyperactivity disorder-related diagnoses, and with visual impairment. There appeared to have been little association between Apgar score < 7 and the examined impairments in the absence of neonatal encephalopathy symptoms, although the relevant data were sparse.Citation19
Evidence regarding adult intelligence quotient (IQ) in relation to Apgar scores comes from studies based on linkage of birth data with results of routine IQ testing at conscription.Citation15,Citation25,Citation26 The first such study failed to find an association between Apgar score and adult cognitive function.Citation15 A low overall prevalence of low (<85) IQ scores reported in that study (7% instead of 15% expected given the distribution of IQ scores in the population) is an indication of possible selection bias, whereby conscripts with cognitive impairment may have been exempt from the routine IQ testing.Citation15 A study of Danish male draftees examined neurologic outcomes and army rejection rates among men who were exempt from IQ testing.Citation26 Apgar score < 7 at five minutes was associated with a four-fold increased risk of a neurologic disability in both exempt and non-exempt men and with six-fold risk of neurologic disability that led to army exemption. There was a modest association between five-minute Apgar score < 7 and prevalence of IQ scores in the bottom quartile (prevalence ratio = 1.33 compared with five-minute Apgar score of 10, ).Citation26 In the largest study to date (>170,000 Swedish conscripts), the increase in the risk of low cognitive function associated with five-minute Apgar score <7 (vs 7–10) was nearly identical (odds ratio = 1.35) despite different types of IQ tests used to measure cognitive function.Citation25 The study showed little association between briefly (<5 minutes) low Apgar score and subsequent cognitive performance.Citation25 Reported mean decrease in IQ associated with Apgar score < 7 at five minutes amounts to one-tenth of one standard deviation, ranging from 1.2 to 1.8 IQ points.Citation24–Citation26
Other neurologic outcomes
A recent case-control study reported a three-fold increase in risk of infantile autism associated with five-minute Apgar score < 7.Citation20 In addition there is evidence suggesting association of low Apgar scores with neonatal auditory impairment.Citation23
Discussion
Most studies consistently show that low Apgar scores, particularly when prolonged, are associated with greater risk of neonatal death and with subsequently diagnosed neurologic disability.
Low Apgar score is associated with correlates of brain damage, such as hypoxic–ischemic encephalopathy (HIE) and acidemia (pH < 7.0 of the umbilical-cord blood). Reported prevalence of HIE from a recent study was 70%, 14%, and 0% among term, malformation-free infants with five-minute Apgar score 0–3, 4–6, and 7–10, respectively.Citation27 Acidemia reportedly occurs in about 38% of term infants with five-minute Apgar scores <7.Citation28 Acidemia may be indicative of hypoxia, which in turn could lead to HIE. HIE may cause neurologic dysfunction in term newborns,Citation29,Citation30 and it accounts for about 20% of cerebral palsy cases.Citation31 Severe HIE is associated with up to 75% infant mortality.Citation32 The co-occurrence of low Apgar scores with markers of hypoxia and with HIE is one possible mechanism underlying its association with death and neurologic disability.
Neurologic disability develops by a number of mechanisms, some of which involve HIE, but many still unknown. A low value of Apgar score may reflect the action of different sets of prenatal or perinatal factors that either cause neurologic morbidity or are markers of increased susceptibility.Citation21 Furthermore, common causes that underlie infant’s failure to respond to resuscitation and its poor long-term neurologic prognosis could also partially account for the observed associations. There are likely to be individual differences with respect to the amount of asphyxia required to produce appreciable brain damage in survivors with low Apgar scores.Citation14
Although relative risks reported for the associations between low Apgar scores and risks of neurologic disability are rather large, the corresponding absolute risks are low. Furthermore, majority of children with clinical disability do not have a history of a low Apgar score.Citation3,Citation14 This is hardly surprising given that there is imperfect correlation between low Apgar scores and conditions that predispose to neurologic damage, such as HIE. These conditions, in turn, imperfectly correlate with subsequent neurologic morbidity,Citation33,Citation34 further contributing to the dilution of the observed associations.
Among preterm infants, low values of some Apgar score components (eg, reflex irritability, muscle tone, respiratory effort) reflect physiological prematurity rather than newborn compromise.Citation35,Citation36 Therefore, the degree of correlation between low Apgar scores and potential markers of brain damage is weaker in preterm than in term infants. For example, the shorter the gestation, the weaker the correlation appears to be between low Apgar score and acidosis (ie, larger proportions of preterm babies have low Apgar scores without evidence of acidosis).Citation37 Similarly, relative risks of abnormal clinical findings associated with low Apgar scores in the first hours of life appear to be decreasing with decreasing gestational age.Citation36 Preterm infants are at greater risk of adverse outcome regardless of Apgar score. Thus, the de-coupling of low Apgar score from signs of potential neurologic damage among preterm infants may explain weaker associations between low Apgar scores and risk of neurologic disability.Citation9,Citation14 At the same time, stronger association of low Apgar score with adverse outcome among term infants may be viewed as a strength, rather than a limitation, of Apgar score, since in term babies, Apgar score may indicate vulnerabilities that are not known or apparent.
Apgar score is a reliable index of a newborn’s condition immediately after birth, particularly in guiding decisions regarding resuscitation and in predicting neonatal death.Citation16 The associations of low Apgar scores with neurologic disability have been shown with sufficient consistency, but the low associated absolute risks do not warrant use of low Apgar score to predict long-term neurologic prospects for individual infants. Rather, the associations may be taken as evidence of the potential biologic mechanisms that link prenatal and perinatal events with neurodevelopment.
Search strategy
I searched Medline for English language articles with abstracts, published from January 1st, 1999 to February 20, 2009, using the term ‘Apgar score’ in the title or abstract. I examined Medline-provided related articles, and also manually searched references of published papers.
Acknowledgements
I am grateful to Dr. Lars Pedersen and to Prof. Henrik Toft Sørensen for insightful comments on material related to this article. The author reports no conflicts of interest in this work.
References
- ApgarVA proposal for a new method of evaluation of the newborn infantCurr Res Anesth Analg19533226026713083014
- ApgarVThe newborn (Apgar) scoring system. Reflections and advicePediatr Clin North Am19661336456505946299
- ACOG Committee OpinionNumber 333, May 2006 (replaces No. 174, July 1996): The Apgar scoreObstet Gynecol200610751209121216648434
- ApgarVHoladayDAJamesLSWeisbrotIMBerrienCEvaluation of the newborn infant; second reportJAMA195816819851988
- CrawfordJSDaviesPPearsonJFSignificance of the individual components of the Apgar scoreBr J Anaesth19734521481584704065
- DrageJSKennedyCSchwarzBKThe Apgar score as an index of neonatal mortality: a report from the Collaborative Study of Cerebral PalsyObstet Gynecol19642422223014199529
- OddDEDoylePGunnellDLewisGWhitelawARasmussenFRisk of low Apgar score and socioeconomic position: a study of Swedish male birthsActa Paediatr20089791275128018489620
- SunYVestergaardMZhuJLMadsenKMOlsenJPaternal age and Apgar scores of newborn infantsEpidemiology200617447347416755265
- SunYVestergaardMPedersenCBChristensenJOlsenJApgar scores and long-term risk of epilepsyEpidemiology200617329630116570027
- Centers for Disease ControlTable 1–28. Live births by 5-minute Apgar score and Age of mother, according to race and hispanic origin of mother: Total of 48 reporting states and the district of Columbia, 2000. Accessed February 9, 2009. Available from: http://www.cdc.gov/nchs/data/statab/t001x28.pdf
- Thorngren-JerneckKHerbstALow 5-minute Apgar score: a population-based register study of 1 million term birthsObstet Gynecol2001981657011430958
- Ondoa-OnamaCTumwineJKImmediate outcome of babies with low Apgar score in Mulago Hospital, UgandaEast Afr Med J2003801222912755238
- SerunianSABromanSHRelationship of Apgar scores and Bayley mental and motor scoresChild Dev19754636987001157607
- NelsonKBEllenbergJHApgar scores as predictors of chronic neurologic disabilityPediatrics19816836447243507
- SeidmanDSPazILaorAGaleRStevensonDKDanonYLApgar scores and cognitive performance at 17 years of ageObstet Gynecol19917768758782030860
- CaseyBMMcIntireDDLevenoKJThe continuing value of the Apgar score for the assessment of newborn infantsN Engl J Med2001344746747111172187
- MosterDLieRTIrgensLMBjerkedalTMarkestadTThe association of Apgar score with subsequent death and cerebral palsy: A population-based study in term infantsJ Pediatr2001138679880311391319
- HarringtonDJRedmanCWMouldenMGreenwoodCEThe long-term outcome in surviving infants with Apgar zero at 10 minutes: a systematic review of the literature and hospital-based cohortAm J Obstet Gynecol20071965463e46146517466703
- MosterDLieRTMarkestadTJoint association of Apgar scores and early neonatal symptoms with minor disabilities at school ageArch Dis Child Fetal Neonatal Ed2002861F16F2111815542
- HultmanCMSparenPCnattingiusSPerinatal risk factors for infantile autismEpidemiology200213441742312094096
- EhrensteinVSørensenHTPedersenLLarsenHHolsteenVRothmanKJApgar score and hospitalization for epilepsy in childhood: a registry-based cohort studyBMC Public Health2006612316451724
- Thorngren-JerneckKHerbstAPerinatal factors associated with cerebral palsy in children born in SwedenObstet Gynecol200610861499150517138786
- JiangZDWilkinsonARNeonatal auditory function and depressed Apgar score: correlation of brainstem auditory response with Apgar scoreActa Paediatr200695121556156017129961
- LawlorDANajmanJMBattyGDO’CallaghanMJWilliamsGMBorWEarly life predictors of childhood intelligence: findings from the Mater-University study of pregnancy and its outcomesPaediatr Perinat Epidemiol200620214816216466433
- OddDERasmussenFGunnellDLewisGWhitelawAA cohort study of low Apgar scores and cognitive outcomesArch Dis Child Fetal Neonatal Ed2008932F115F12017916594
- EhrensteinVPedersenLGrijotaMNielsenGLRothmanKJSørensenHTAssociation of Apgar score at five minutes with long-term neurologic disability and cognitive function in a prevalence study of Danish conscriptsBMC Pregnancy Childbirth2009911419341459
- HoganLIngemarssonIThorngren-JerneckKHerbstAHow often is a low 5-min Apgar score in term newborns due to asphyxia?Eur J Obstet Gynecol Reprod Biol2007130216917516621222
- LocatelliAIncertiMGhidiniAGrecoMVillaEPaterliniGFactors associated with umbilical artery acidemia in term infants with low Apgar scores at 5 minEur J Obstet Gynecol Reprod Biol2008139214615018316156
- FerrieroDMNeonatal brain injuryN Engl J Med2004351191985199515525724
- ShalakLPerlmanJMHypoxic-ischemic brain injury in the term infant-current conceptsEarly Hum Dev200480212514115500993
- PerlmanJMIntrapartum Hypoxic-Ischemic Cerebral Injury and Subsequent Cerebral Palsy: Medicolegal IssuesPediatrics19979968518599164779
- SimonNPLong-term neurodevelopmental outcome of asphyxiated newbornsClin Perinatol199926376777810494478
- GrahamEMRuisKAHartmanALNorthingtonFJFoxHEA systematic review of the role of intrapartum hypoxia-ischemia in the causation of neonatal encephalopathyAm J Obstet Gynecol2008199658759519084096
- PerlmanJMIntrapartum asphyxia and cerebral palsy: is there a link?Clin Perinatol200633233535316765728
- CatlinEACarpenterMWBrannBStThe Apgar score revisited: influence of gestational ageJ Pediatr198610958658683772665
- WeinbergerBAnwarMHegyiTHiattMKoonsAPanethNAntecedents and neonatal consequences of low Apgar scores in preterm newborns: a population studyArch Pediatr Adolesc Med2000154329430010710031
- GoldenbergRLHuddlestonJFNelsonKGApgar scores and umbilical arterial pH in preterm newborn infantsAm J Obstet Gynecol198414966516546742047