Abstract
Patients with mantle cell lymphoma (MCL) have a poor prognosis; consequently, new therapeutic approaches, such as rapamycin and its derivates, mammalian target of rapamycin (mTOR) inhibitors, are warranted. Temsirolimus (also known as CCI-779), a dihydroester of rapamycin, in MCL cell lines inhibited mTOR, downregulated p21 and v-Raf, and induced autophagy. The first clinical trial in MCL patients was performed using 250 mg of temsirolimus weekly for 6–12 cycles. The overall response rate was 38%; the median time to progression was 6.5 months, median overall survival was 12 months, and the median duration of response was 6.9 months. At lower dose (25 mg/week), the overall response rate was 41%, median overall survival was 14 months, and time to progression was 6 months. In another trial, 162 patients were randomly assigned to receive temsirolimus at 2 different doses (175 mg/week for 3 weeks, then 75 mg or 25 mg/week) or a treatment chosen by the investigator among the most frequently adopted single agents for treatment of relapsed MCL. Patients treated with 175/75 mg of temsirolimus had significantly higher response rates and longer progression-free survival than those treated with investigator’s choice therapy. These data support the use of mTOR inhibitors for the treatment of MCL, probably in combination with other agents, such as antiangiogenic drugs or histone acetylase inhibitors.
Keywords:
Mantle cell lymphoma
Mantle cell lymphoma (MCL), which accounts for approximately 6% of all non-Hodgkin lymphomas, represents the subtype where mammalian target of rapamycin (mTOR) inhibitors appear as more promising compounds in its treatment. The interest in application of these drugs to treat MCL has grown as it has been demonstrated that cyclin D1, overexpressed in this histotype of lymphoma, is an important downstream target of the mTOR signaling pathway.
Nevertheless, it has been reported that mTOR inhibitors inactivate other genes associated with the pathogenesis of MCL, such as vascular endothelial growth factor (VEGF), Ras, Raf, extracellular regulated kinase (ERK), and nuclear factor-kappa B. Moreover, the interest in this class of compounds has increased as more effective therapeutic strategies are required for MCL treatment, which has been demonstrated by the low response and survival rates observed in MCL patients treated with this drug.
Indeed, notwithstanding the most recent and effective therapeutic approaches adopted, the clinical evolution of most patients with MCL is still aggressive, with median overall survival not exceeding 3–4 years.Citation1 Given the poor complete remission rates achieved with conventional regimens, chemotherapy combinations have been investigated to improve the outcomes: one of these regimens is the hyper-CVAD (fractionated cyclophosphamide, vincristine, doxorubicin, dexamethasone, alternating with high-doses methotrexate and cytarabine). This regimen, associated with the anti-CD20 monoclonal antibody rituximab, has shown good efficacy and tolerability in MCL, offering high response rates and 3-year failure-free survival and overall survival of 64% and 82%, respectively.Citation2 Analogously, rituximab combined with cyclophosphamide, adriamycin, vincristine and prednisone (R-CHOP) has been shown to be significantly superior to CHOP in overall response rate (94% vs 75%) and time to treatment failure (21 vs 14 months), with acceptable toxicity.Citation3 In conclusion, the responses to second-line treatments of about 30% of patients affected by MCL relapse are still not fully satisfactory: rituximab associated with fludarabine, cyclophosphamide, and mitoxantrone (R-FCM) offered only 29% of complete remission;Citation4 radioimmunotherapy resulted in 30% of complete responses, with median event-free survival of 6 months and median overall survival of 21 months.Citation5 Moreover, an objective response was achieved in 45% of patients receiving bortezomib, with median progression-free survival of only 6 months.Citation6 Fifty-three percent of patients responded well to lenalidomide, with a median duration of response of 13.7 months and median progression-free survival of 5.6 months.Citation7,Citation8
Targeting mTOR pathway
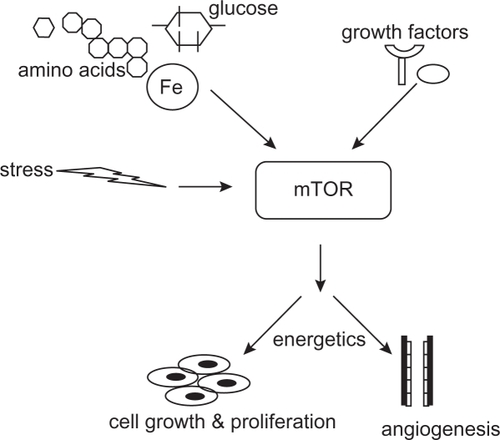
In the mid-1970s, a strain of Streptomyces hygroscopicus, producing a compound with potent antifungal activity, was isolated from the soil samples collected from the Rapa Nui Island in the South Pacific.Citation9 From the geographical origin, the purified antibiotic was named “rapamycin.”Citation10 In addition to antifungal activity, rapamycin was found to inhibit immune responses in mammals by depressing lymphocyte proliferation and to exert a cytostatic activity in several in vitro and in vivo cancer models.Citation11 In the 1990s, rapamycin was found to exert its activities by an evolutionarily conserved pathway that integrates signals from growth factors, nutrients, and energy status. The activation of mTOR pathway signifies a decision point that takes into account the availability of materials required for cell growth (amino acids, glucose, and energy) and the growth-regulating signals (hormones and growth factors). Thus, the cells are protected from outside signals to grow and still proliferate when nutrients and energy inside are not sufficient ().Citation12
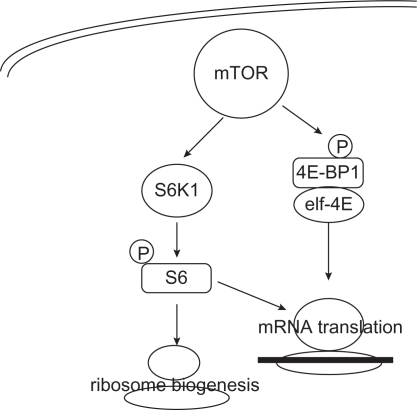
Figure 1 mTOR as central regulator of the cell nutrition and growth. Conditions outside of the cell, such as nutrient and energy levels, growth factors, hormones, and stressful conditions, control the mTOR activation. After activation, mTOR stimulates cell growth, increases angiogenesis, and responds to bioenergetics necessities.
The human MTOR gene (GeneID: 2475) maps to chromosome 1p36.2 and encodes a 289-kDa protein containing a kinase catalytic domain, 20 HEAT (Huntington elongation factor 1A-protein phosphatase) repeats, an autoinhibitory repressor domain, and the FRB domain, responsible for interaction with FKBP12, a cofactor and transporter for rapamycin.Citation13,Citation14
The mTOR protein participates in 2 signaling complexes: mTORC1 and mTORC2. mTORC1, which is sensitive to rapamycin, includes mTOR, Raptor (regulatory-associated-protein of mTOR), and GβL (G protein β-subunit-like protein). This complex reacts with signals that originate from growth factors, energy status, nutrient availability, hypoxia, reactive oxygen species, deoxyribonucleic acid (DNA) damage, and osmotic condition of environment.Citation15 mTORC1 is activated by numerous upstream signalling pathways, including PI3K/Akt, Ras/MAPK, and Bcr-Abl1, whereas the negative regulators are phosphatase and tensin homolog (PTEN), LKB1, and the heterodimer TSC1 (tuberous sclerosis complex 1 or amartin)/TSC2 (tuberous sclerosis complex 2 or tuberin)Citation16 (). Activated AktCitation17 and Ras-Raf-ERK pathways phosphorylate TSC1/TSC2, leaving the Rheb protein GTP-bound and capable of interacting with and activating mTOR.Citation18
Figure 2 mTOR upstream pathway. Amino acid, glucose levels, growth factors, and genes, such as Bcr-Abl and Ras, induce activation of the PI3K/Akt pathway and consequently of the mTOR. The Akt pathway is inhibited by PTEN and LKB1 through the TSC1–TSC2 complex.
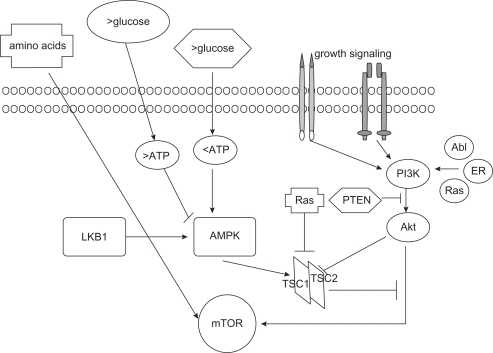
The activity of PI3K is countered by PTEN; loss of PTEN has been reported in several solid tumors and lymphomas and seems to correlate with sensitivity to rapamycin derivatives.Citation19
mTORC2 complex, rapamycin insensitive, contains mTOR, GβL, Rictor (rapamycin-independent companion of mTOR), and mSIN1 (mammalian stress-activated protein kinase interacting protein 1).Citation20 It is believed that various growth factors contribute to mTORC2 activation. This complex regulates cytoskeleton organization and activates Akt, thus representing a further important level of self-regulation of the mTOR pathway.Citation21
Upon activation, mTOR facilitates cell cycle progression from G1 to S phase by phosphorylation of p70S6 kinase (p70S6K) and 4E-binding protein 1 (4E-BP1). p70S6K phosphorylates and activates S6, a ribosomal subunit involved in initiating translation of 5′ terminal oligopyrimidine tract-containing mRNA encoding components of the protein synthesis machinery. The mTOR-mediated phosphorylation of 4E-BP1 diminishes the stability of the 4E-BP1/eIF4E complex and facilitates the eIF4E action, enhancing translation of several mRNAs, such as cyclin D1, c-myc, hypoxia-inducible factor 1α (HIF1α), ornithine decarboxylase, VEGF, fibroblast growth factor, and ribosomal proteins ().Citation22,Citation23
mTOR inhibitors in hematological malignancies
Rapamycin (sirolimus) was the first mTOR inhibitor used in clinical practice;Citation24 more recently, several rapamycin analogs have been tested in clinical trials for solid and hematological malignancies: temsirolimus (CCI-779; Wyeth Pharmaceuticals, Madison, New Jersey, USA), everolimus (RAD001; Novartis, Basel, Switzerland), and deforolimus (MK-8669, AP23573; Merck and Ariad Pharmaceuticals, Cambridge, Massachusetts, USA).
Because mTOR is important for cell proliferation in several hematological malignancies, mTOR inhibitors have been used either as single drugs or in combination with conventional chemotherapeutic agents or monoclonal antibodies in acute/chronic lymphocytic or myeloid leukemia, multiple myeloma, myelodysplastic syndromes, and lymphomas. mTOR inhibitors have been shown to be also effective against acute lymphoblastic leukemia, even when combined with methotrexate, anthracyclines, etoposide, or corticosteroids.Citation24–Citation27
Rapamycin restored sensitivity to steroid-resistant cellsCitation28 and to tyrosine kinase inhibitors in resistant patients with chronic myeloid leukemia.Citation29 In acute myeloid leukemia, where Akt is activated, phosphorylation of p70S6K and 4EBP-1 is significantly inhibited by everolimus, especially when combined with Ara-C.Citation30 Also in myelodysplastic syndromes, activation of the Akt/mTOR pathway in high-risk patients was described.Citation31
The PI3K/Akt pathway is frequently activated in multiple myeloma, where mTOR inhibitors were effective.Citation32,Citation33 In a phase II trial, 16 patients with relapsed refractory multiple myeloma received 25 mg of intravenous temsirolimus weekly until progression, with overall response rate of 38% and median time to progression of 138 days.Citation34
In Hodgkin’s lymphoma, everolimus downregulated the truncated isoform of the transcription factor CCAAT enhancer binding protein beta, which inhibits NF-kB activity.Citation35 Rapamycin has been shown to inhibit mTORC1 also in diffuse large B-cell lymphoma cell linesCitation36 and to overcome the P-glycoprotein-mediated multidrug resistance in B-lymphoma cell lines.Citation37 In primary effusion lymphoma, rapamycin reduced the accumulation of ascites and extended mouse survival, with significant reduction in levels of circulating VEGF.Citation38
Moreover, rapamycin showed a strong antiproliferative effect on B-cell lines derived from organ transplant recipients with Epstein–Barr virus-associated post-transplant lymphoproliferative disorders.Citation39
mTOR inhibitors were effective in follicular lymphoma, where neoplastic cells display phosphorylation of p70S6K and 4E-BP1.Citation40,Citation41
In chronic lymphocytic leukemia (CLL) cells, where PI3K is constitutively active,Citation42 cycle arrest induced by rapamycin was accompanied by reduced expression of cyclins D3, A, and E.Citation43 A phase II trial with oral everolimus was conducted in 7 patients with CLL relapsed after at least 2 lines of therapy. Disease stabilization was observed in 3 patients and partial response in 1 patient; however, the trial was precociously stopped because of infectious toxicity.Citation44
MCL and mTOR inhibitors
Overexpression of the cyclin D1, product of the oncogene Bcl-1, is considered the primary genetic event in MCL and hence mTOR inhibitors are used in the treatment of MCL. Cyclin D1 plays a critical role in cell transition from the G to S phase in response to mitogens.Citation45 The overexpression of cyclin D1 is due to the translocation t(11;14)(q13;q32) juxtaposing the Bcl-1 (CCND1) gene on chromosome 11 to the immunoglobulin heavy chain locus (IgVH) on chromosome 14.Citation46 t(11;14) (q13;q32) is identified in 50%–70% of MCL cases based on the type of the method used.
Cyclin D1, in association with cyclin-dependent kinase-4 and -6, induces the cell to enter the S phase by phosphorylating the retinoblastoma tumor-suppressing protein, which binds to transcription factors, including E2F.Citation47
In addition to the overexpression of cyclin D1, other genes that overexpress in MCL, such as VEGF and Raf-1, represent further possible targets for mTOR inhibitors.
Indeed, a constitutive activation of Akt and mTOR pathways either in MCL cell lines (Granta 519, Jeko-1, and SP-53) or in primary cultures from 30% of MCL patients has been reported.Citation48,Citation49 Moreover, mTOR inhibitors in MCL could synergize with other “canonical” agents, such as vincristine, doxorubicin, bortezomib, and rituximab, with resulting inhibition of Raf-1, MAPK, and mTOR.Citation50,Citation51
Nevertheless, the data on the in vitro activity of different mTOR inhibitors in MCL cell lines are conflicting;Citation52 all compounds induced cell cycle arrest in G0/G1 phase, temsirolimus reduced p21 expression, and rapamycin increased p27 expression; however, the data on cyclin D1 levels are still not clear ().
Table 1 In vitro activity of mTOR inhibitors on MCL cell lines: relevant data from literature
In several MCL cell lines, pharmacological inhibition of the PI3K/Akt pathway by rapamycin was associated with downregulation of cyclin D1 and the antiapoptotic proteins cFLIP, Bcl-XL, and Mcl-1.Citation53 Treatment with rapamycin inhibited the proliferation of Granta and NCEB cells, with accumulation of cells in G1 phase, without modification of the apoptotic process. The expression of cyclins D3, E, and A was strongly reduced in both cell lines, while cyclin D1 expression was not changed.Citation54,Citation55
In another in vitro study, rapamycin inhibited cell proliferation and induced cell cycle arrest in G0/G1 phase mediated by cyclin D3 and p27 deregulation. In the SP-53 cell line only, rapamycin downregulated cyclin D1 levels; this effect on cyclin D1 was observed only in cell lines where GSK3β was activated.Citation48
In MCL, GSK3β is inactivated in about half the cases as a consequence of Wnt stimulation. After that, β-catenin is released and translocated into the nucleus, where it upregulates the transcription of several genes, including cyclin D1.Citation56
In MCL cell lines, cyclin D1 was unmodified by temsirolimus,Citation57 which downregulated p21, thus inducing a cell cycle block in the G1 phase and exerting a cytostatic rather than a cytotoxic action.
Interestingly, temsirolimus showed a synergistic antineoplastic activity with vorinostat, probably adding to the proapoptotic effect exerted by the histone acetylase inhibitors, the induction of autophagy. Autophagy is a reversible, bidirectional process; it not only can enhance and promote survival under stressful conditions but also can lead to cell death. In an in vitro study on MCL cell lines, temsirolimus inhibited mTOR, downregulated p21, and induced autophagy without any effect on pERK, Bcl-2, Bax, Bad, and beclin-1.Citation52
Another factor that supports the use of mTOR inhibitors in MCL is the inhibition of angiogenesis. Indeed, TORC1 activation results in upregulation of HIF1α that leads to increased expression of angiogenic factors, such as VEGF and platelet-derived growth factor-βCitation58 In well-oxygenated cells, HIF1α is continuously produced and degraded by proteosomes. In hypoxic cells, HIF1α translocates to the nucleus, initiating the transcription of genes involved in glycolysis, angiogenesis, cell survival, and metastasis. As VEGF is one of the regulators of the PI3K/Akt activity, increased levels of VEGF induce a further activation of mTOR. Inhibition of mTOR activity affects angiogenesis by reducing the expression of HIF1α̣ and by inhibiting the ability of cells to respond to the mitogenic effect of VEGF.
High levels of VEGF have been associated with poor outcomes in acute lymphoblastic leukemiaCitation59 and non-Hodgkin lymphomas.Citation60,Citation61 In MCL, VEGF expression has been reported in 41% of cases, with an evident negative prognostic significance.Citation62
Recently, our group showed that 2 VEGF polymorphisms associated with higher plasmatic protein levels, G+405C and C+936T, were more frequently detected in MCL cases than in healthy controls, thus supporting the hypothesis that some VEGF genotypes would increase the risk of development of this lymphoma.Citation63
Another upstream regulator of mTOR, particularly interesting in MCL, is the Ras/Raf/ERK/MAPK pathway.Citation64 v-Raf has been reported to act synergistically with c-Myc to induce B-cell tumors in a murine model.Citation65 In a series of patients with MCL and receiving R-hyper-CVAD, our group previously reported that c-Myc overexpression was associated with shorter overall and progression-free survival.Citation66 Like c-Myc, Mcl-1 is overexpressed in MCL;Citation67 this gene, a member of the bcl-2 family, is translationally regulated by mTORC1 and is involved in the antiapoptotic action of mTOR.Citation68
Syk, a tyrosine kinase involved in B-cell receptor signalling, has been reported to be amplified at the DNA level and overexpressed at both RNA and protein levels in MCL cell lines and in a small subset of clinical samples. As inhibition of Syk resulted in potent inhibition of mTOR activity in follicular cells, mantle cells, Burkitt, and diffuse large B-cell lymphoma cell lines, this tyrosine kinase would represent a further good target for mTOR inhibitors.Citation69
Temsirolimus for relapsed MCL
Temsirolimus (also known as CCI-779), a dihydroester of rapamycin suitable for intravenous use, is currently under trial for use in solid tumors, such as renal cancer,Citation70 breast cancer,Citation71 sarcomas,Citation72 and prostate cancer.Citation73 In hematology, it has been tested in MCL, multiple myeloma, and acute myeloid leukemia.Citation74
The prototype mTOR inhibitor, oral rapamycin, is poorly soluble and undergoes extensive first-pass metabolism, leading to low and potentially variable absorption and exposure. For some tumors, maximizing the bioavailability and dose intensity via intravenous administration may provide optimal clinical benefit. Temsirolimus is an ester analog of rapamycin that retains its potent intrinsic mTOR inhibitory activity while exhibiting better solubility for intravenous formulation. In the treatment of advanced renal cell carcinoma, temsirolimus is administered as a 30- to 60-minute infusion once weekly at a flat dose of 25 mg. This dosage results in high peak temsirolimus concentrations and limited immunosuppressive activity.Citation75
From April 2002 to October 2003, 35 MCL patients (median age of 70 years, 91% in stage IV) who failed therapies with alkylating agents, cyclophosphamide, anthracyclines, purine analogs, and rituximab received 250 mg of temsirolimus weekly for 6–12 cyclesCitation76 (). The overall response rate was 38%, with 3% of complete remissions and 35% of partial responses achieved by 3 months. The median time to progression was 6.5 months, median overall survival was 12 months, and the median duration of response was 6.9 months. Nevertheless, dose reduction was necessary in 31 cases: 71% of patients experienced grade 3 and 9% experienced grade 4 hematological toxicity. Thrombocytopenia, anemia, neutropenia, increased triglycerides, diarrhea, hyperglycemia, sensory neuropathy, and rash were the most frequent adverse events.
Table 2 Temsirolimus in MCL patients: results from clinical trials
The most frequent toxicities reported for mTOR inhibitors are mucositis, stomatitis, pneumonitis, rash, nail dystrophy, hyperlipidemia, hyperglycemia, and bone marrow suppression. In phase II trials in renal and breast cancer, the overall favorable safety profile of temsirolimus was confirmed; grade 3–4 mucositis was observed in <5%, skin rash in 4%, pneumonitis in 5%, hyperlipidemia in 6%, hyperglycemia in 17%, thrombocytopenia in <5%, and anemia in 9% of treated patients.Citation77 Thrombocytopenia grade 3–4 occurred in 65%, anemia in 25%, and neutropenia in 28% of MCL cases; this difference was probably due to the frequent involvement of bone marrow (91% of patients were in stage IV) and treatments previously received. Nevertheless, only 1 patient required platelet transfusion and 4 required red cells support. The lower dose levels were evaluated in a phase II trial by the North Central Cancer Treatment Group.Citation78
The objective of this study was to test a low dose of temsirolimus (25 mg weekly) in patients with relapsed MCL. Patients who had a tumor response after 6 cycles were eligible to continue the drug for a total of 12 cycles or 2 cycles after complete remission. The median age of the 29 enrolled patients was 69 years, with 86% of patients in stage IV. The overall response rate was 41%, with 37% of partial responses. The median overall survival from the study entry was 14 months, and the time to progression and median duration of response were 6 months. Hematological toxicities were the most common toxicities, with 50% grade 3 and 4% grade 4 adverse events. Thrombocytopenia was the most frequent cause of dose reduction. Three patients experienced infection without concomitant neutropenia. Thus, this trial reported responses similar to those described for higher dose, but with less toxicity.
From June 2005 to July 2007, 162 patients were randomly assigned to receive temsirolimus at 2 doses (175 mg/wk for 3 weeks and then 75 mg or 25 mg/week) or a treatment chosen by the single investigator among the most frequently adopted agents for the treatment of relapsed MCL (gemcitabine, fludarabine, chlorambucil, cladribine, etoposide, thalidomide, vinblastine, alemtuzumab, lenalidomide).Citation79 Median progression-free survival was 4.8, 3.4, and 1.9 months for temsirolimus 175/75 mg, temsirolimus 175/25 mg, and investigator’s choice groups, respectively. Patients treated with temsirolimus 175/75 mg had significantly longer progression-free survival than those treated with investigator’s choice therapy; those treated with temsirolimus 175/25 mg showed a trend toward longer progression-free survival. The objective response rate was significantly higher in the 175/75 mg group (22%) than in the investigator’s choice group (2%). The median overall survival for the temsirolimus 175/75 mg group and the investigator’s choice group was 12.8 and 9.7 months, respectively. The advantage offered by temsirolimus was independent of age, sex, performance status, stage of disease at diagnosis, number of extranodal sites, and blastoid histology. The most frequent grade 3 or 4 adverse events documented in 89% of patients in the temsirolimus 175/75 mg group and in 80% of patients in the temsirolimus 175/25 group were thrombocytopenia, anemia, neutropenia, and asthenia. Grade 3/4 thrombocytopenia was higher in the temsirolimus 175/75 mg group (59% vs 36% in the investigator’s choice arm), anemia was comparable in the 2 arms (20% vs 17%), and neutropenia was lower in temsirolimus group (15% vs 26%). In the group of patients treated with temsirolimus, the most frequent side effects were asthenia (13% vs 8%), infection (9% vs 4%), diarrhea (7% vs 0%), rash (7% vs 0%), dyspnea (7% vs 9%), fever (6% vs 0%), and pruritus (4% vs 0%). Nevertheless, a lower number of patients discontinued treatment with temsirolimus compared with those receiving standard therapies (43% vs 52%), maintaining also a good quality of life.
At the 2009 European Hematology Association meeting, results from this trial were updated. The median progression-free survival and overall survival were confirmed to be significantly longer for the patients treated with 175/75 mg temsirolimus than for those treated with investigator’s choice therapy (5.2 vs 1.9 months and 5.2 vs 2 months, respectively).Citation80
Moreover, considering the ability of rituximab to inhibit Akt and Raf-1 signalling pathways, 71 relapsed/resistant MCL patients received 25 mg of intravenous temsirolimus every week and 4 weekly doses of rituximab in the first cycle, and then 1 dose of rituximab every other cycle, between May 2005 and March 2009.Citation81 Patients with a tumor response after 6 cycles were eligible to continue treatment for a total of 12 cycles or 2 cycles after complete remission, and were then observed without maintenance. With median age of 67 years, 28% of patients were rituximab refractory. The overall response rate was 48%, with 20% of complete and 28% of partial responses. The median duration of response was 9.5 months for rituximab-sensitive patients and 7.15 months for rituximab-refractory patients. While the combination was generally well tolerated, 12 patients experienced grade 4 toxicity. Hematological toxicities were most common, with 5 patients having grade 4 thrombocytopenia and 3 having grade 4 neutropenia.
Responses (30%) to temsirolimus by patients with MCL are higher than those reported by patients with renal cell carcinoma, breast cancer, lung cancer, and glioblastoma (about 10%). Why patients affected by lymphoma would be more sensitive than those affected by solid tumors is still unexplained; some authors suggest that the different ways of inactivation of PTEN (phosphorylation in lymphoma and mutation/deletion in solid tumors) could be one possible cause. It is also possible that prolonged exposure to temsirolimus could inactivate both the mTORC1 and mTORC2 complexes in sensitive tumors, therefore inhibiting the negative feedback of phosphorylation of Akt.Citation53
Considering these promising results, the future perspective would be to test other mTOR inhibitors, such as everolimus, or drug combinations in MCL, but as first-line therapies. As reported in the 2009 American Society of Hematology meeting, 37 patients with relapsed diffuse large cell lymphoma and MCL received 5 mg/day of everolimus. The overall response rate was 32%, with 29% in the MCL group. The median time to progression for all patients was 3.1 months. The median duration of response for the 12 responders was 5.5 months. Everolimus was well tolerated, with the incidence of grade 3 anemia, neutropenia, and thrombocytopenia occurring in 11%, 16%, and 30% of cases.Citation82
Thus, the perspective of using mTOR inhibitors as first-line treatment for MCL patients would be a challenge for the next future; the association of rituximab, cladribine, and temsirolimus is scheduled for the newly diagnosed MCL (registered at ClinicalTrials.gov as NCT00787969, April 2009). This phase I/II trial is planned to evaluate the efficacy and safety of temsirolimus when given together with cladribine and rituximab; the treatment is repeated every 28 days for up to 6 courses in the absence of disease progression or unacceptable toxicity. As secondary endpoints, the trial includes the assessment of metabolic markers (hyperglycemia and hyperlipidemia) as markers of mTOR inhibition and correlation of response with serum-free light chains, single-nucleotide polymorphisms in host immune genes, vitamin D metabolites, and PI3K pathway member expression.
It is probable that patients not heavily pretreated could represent the best scenario for using mTOR inhibitors to reduce toxicities and increase their efficacies.
In conclusion, the demonstration that temsirolimus at 175 mg/week as induction, followed by 75 mg/week, significantly improved clinical benefit (response rate and progression-free survival) in comparison to “canonical” drugs is the most convincing element for considering the use of this mTOR inhibitor in relapsed MCL patients. Moreover, the fact that temsirolimus is well tolerated in general and that severe clinical side effects >grade 3 are rare events represents another supporting element. Obviously, the optimal dose of temsirolimus, as well as the exploration of new combinations (in particular with anti-CD20 antibodies, histone deacetylase inhibitors and inhibitors of Raf or angiogenesis), is still under discussion, and further studies enrolling larger series of patients are warranted to confirm the above reported promising clinical results.
Disclosure
The authors report no conflicts of interest in this work.
References
- ZuccaERoggeroEPinottiGPatterns of survival in mantle cell lymphomaAnn Oncol1995632572627612491
- RomagueraJEFayadLRodriguezMAHigh rate of durable remissions after treatment of newly diagnosed aggressive mantle-cell lymphoma with rituximab plus hyper-CVAD alternating with rituximab plus high-dose methotrexate and cytarabineJ Clin Oncol200523287013702316145068
- LenzGDreylingMHosterEImmunochemotherapy with rituximab and cyclophosphamide, doxorubicin, vincristine, and prednisone significantly improves response and time to treatment failure, but not long-term outcome in patients with previously untreated mantle cell lymphoma: results of a prospective randomized trial of the German Low Grade Lymphoma Study Group (GLSG)J Clin Oncol20052391984199215668467
- ForstpointnerRDreylingMReppRThe addition of rituximab to a combination of fludarabine, cyclophosphamide, mitoxantrone (FCM) significantly increases the response rate and prolongs survival as compared with FCM alone in patients with relapsed and refractory follicular and mantle cell lymphomas: results of a prospective randomized study of the German Low-Grade Lymphoma Study GroupBlood2004104103064307115284112
- WangMOkiYProBPhase II study of yttrium-90-ibritumomab tiuxetan in patients with relapsed or refractory mantle cell lymphomaJ Clin Oncol200927315213521819770379
- O’ConnorOAMoskowitzCPortlockCPatients with chemotherapy-refractory mantle cell lymphoma experience high response rates and identical progression-free survivals compared with patients with relapsed disease following treatment with single agent bortezomib: results of a multicentre Phase 2 clinical trialBr J Haematol20091451343919220284
- HabermannTMLossosISJusticeGLenalidomide oral monotherapy produces a high response rate in patients with relapsed or refractory mantle cell lymphomaBr J Haematol2009145334434919245430
- GeislerCMantle cell lymphoma: are current therapies changing the course of disease?Curr Oncol Rep200911537137719679012
- SehgalSNBakerHVézinaCRapamycin (AY-22,989), a new antifungal antibiotic. II. Fermentation, isolation and characterizationJ Antibiot (Tokyo)197528107277321102509
- DrakosERassidakisGZMedeirosLJMammalian target of rapamycin (mTOR) pathway signalling in lymphomasExpert Rev Mol Med200810e418241520
- GaumannASchlittHJGeisslerEKImmunosuppression and tumor development in organ transplant recipients: the emerging dualistic role of rapamycinTranspl Int200821320721718069922
- BjornstiMAHoughtonPJThe TOR pathway: a target for cancer therapyNat Rev Cancer20044533534815122205
- GibbonsJJAbrahamRTYuKMammalian target of rapamycin: discovery of rapamycin reveals a signaling pathway important for normal and cancer cell growthSemin Oncol200936Suppl 3S3S1719963098
- CafferkeyRMcLaughlinMMYoungPRJohnsonRKLiviGPYeast TOR (DRR) proteins: amino-acid sequence alignment and identification of structural motifsGene199414111331368163165
- HayNSonenbergNUpstream and downstream of mTORGenes Dev200418161926194515314020
- JozwiakJJozwiakSGrzelaTLazarczykMPositive and negative regulation of TSC2 activity and its effects on downstream effectors of the mTOR pathwayNeuromolecular Med20057428729616391386
- PotterCJPedrazaLGXuTAkt regulates growth by directly phosphorylating Tsc2Nat Cell Biol20024965866512172554
- WullschlegerSLoewithRHallMNTOR signaling in growth and metabolismCell2006124347148416469695
- VignotSFaivreSAguirreDRaymondEmTOR-targeted therapy of cancer with rapamycin derivativesAnn Oncol200516452553715728109
- WullschlegerSLoewithROppligerWHallMNMolecular organization of target of rapamycin complex 2J Biol Chem200528035306973070416002396
- JulienLACarriereAMoreauJRouxPPmTORC1-activated S6K1 phosphorylates Rictor on threonine 1135 and regulates mTORC2 signalingMol Cell Biol201030490892119995915
- GingrasACGygiSPRaughtBRegulation of 4E-BP1 phosphorylation: a novel two-step mechanismGenes Dev199913111422143710364159
- MirshahiPToprakSKFaussatAMMalignant hematopoietic cells induce an increased expression of VEGFR-1 and VEGFR-3 on bone marrow endothelial cells via AKT and mTOR signalling pathwaysBiochem Biophys Res Commun200634931003101016959214
- BaldoPCeccoSGiacominELazzariniRRosBMarastoniSmTOR pathway and mTOR inhibitors as agents for cancer therapyCurr Cancer Drug Targets20088864766519075588
- BrownVISeifAEReidGSTeacheyDTGruppSANovel molecular and cellular therapeutic targets in acute lymphoblastic leukemia and lymphoproliferative diseaseImmunol Res2008421–38410518716718
- AvellinoRRomanoSParasoleRRapamycin stimulates apoptosis of childhood acute lymphoblastic leukemia cellsBlood200510641400140615878982
- CrazzolaraRCisterneAThienMPotentiating effects of RAD001 (Everolimus) on vincristine therapy in childhood acute lymphoblastic leukemiaBlood2009113143297330619196656
- GuLGaoJLiQRapamycin reverses NPM-ALK-induced glucocorticoid resistance in lymphoid tumor cells by inhibiting mTOR signaling pathway, enhancing G1 cell cycle arrest and apoptosisLeukemia200822112091209618685609
- KharasMGDeaneJAWongSPhosphoinositide 3-kinase signaling is essential for ABL oncogene-mediated transformation of B-lineage cellsBlood2004103114268427514976048
- XuQSimpsonSESciallaTJBaggACarrollMSurvival of acute myeloid leukemia cells requires PI3 kinase activationBlood2003102397298012702506
- FolloMYMongiorgiSBosiCThe Akt/mammalian target of rapamycin signal transduction pathway is activated in high-risk myelodysplastic syndromes and influences cell survival and proliferationCancer Res20076794287429417483341
- HoangBBenavidesAShiYFrostPLichtensteinAEffect of autophagy on multiple myeloma cell viabilityMol Cancer Ther2009871974198419509276
- FrostPShiYHoangBLichtensteinAAKT activity regulates the ability of mTOR inhibitors to prevent angiogenesis and VEGF expression in multiple myeloma cellsOncogene200726162255226217016437
- FaragSSZhangSJansakBSPhase II trial of temsirolimus in patients with relapsed or refractory multiple myelomaLeuk Res200933111475148019261329
- DuttonAReynoldsGMDawsonCWYoungLSMurrayPGConstitutive activation of phosphatidyl-inositide 3 kinase contributes to the survival of Hodgkin’s lymphoma cells through a mechanism involving Akt kinase and mTORJ Pathol2005205449850615714459
- GuptaMAnsellSMNovakAJKumarSKaufmannSHWitzigTEInhibition of histone deacetylase overcomes rapamycin-mediated resistance in diffuse large B-cell lymphoma by inhibiting Akt signaling through mTORC2Blood2009114142926293519641186
- PopIVPopLMGhetieMAVitettaESTargeting mammalian target of rapamycin to both downregulate and disable the P-glycoprotein pump in multidrug-resistant B-cell lymphoma cell linesLeuk Lymphoma20095071155116219557637
- GasperiniPTosatoGTargeting the mammalian target of Rapamycin to inhibit VEGF and cytokines for the treatment of primary effusion lymphomaLeukemia200923101867187419554030
- NepomucenoRRBalatoniCENatkunamYSnowALKramsSMMartinezOMRapamycin inhibits the interleukin 10 signal transduction pathway and the growth of Epstein Barr virus B-cell lymphomasCancer Res200363154472448012907620
- LeseuxLHamdiSMAl SaatiTSyk-dependent mTOR activation in follicular lymphoma cellsBlood2006108134156416216912221
- GuptaMDillonSRZiesmerSCA proliferation-inducing ligand mediates follicular lymphoma B-cell proliferation and cyclin D1 expression through phosphatidylinositol 3-kinase-regulated mammalian target of rapamycin activationBlood2009113215206521619321861
- RingshausenIPeschelCDeckerTMammalian target of rapamycin (mTOR) inhibition in chronic lymphocytic B-cell leukemia: a new therapeutic optionLeuk Lymphoma2005461111915621776
- DeckerTHippSRingshausenIRapamycin-induced G1 arrest in cycling B-CLL cells is associated with reduced expression of cyclin D3, cyclin E, cyclin A, and survivinBlood2003101127828512393642
- DeckerTSandherrMGoetzeKOelsnerMRingshausenIPeschelCA pilot trial of the mTOR (mammalian target of rapamycin) inhibitor RAD001 in patients with advanced B-CLLAnn Hematol200988322122718704419
- JaresPColomerDCampoEGenetic and molecular pathogenesis of mantle cell lymphoma: perspectives for new targeted therapeuticsNat Rev Cancer200771075076217891190
- DecaudinDMantle cell lymphoma: a biological and therapeutic paradigmLeuk Lymphoma200243477378112153164
- SherrCJD-type cyclinsTrends Biochem Sci19952051871907610482
- Dal ColJZancaiPTerrinLDistinct functional significance of Akt and mTOR constitutive activation in mantle cell lymphomaBlood2008111105142515118339899
- RudeliusMPittalugaSNishizukaSConstitutive activation of Akt contributes to the pathogenesis and survival of mantle cell lymphomaBlood200610851668167616645163
- HarituniansTMoriAO’KellyJLuongQTGilesFJKoefflerHPAntiproliferative activity of RAD001 (everolimus) as a single agent and combined with other agents in mantle cell lymphomaLeukemia200721233333917136116
- LeseuxLLaurentGLaurentCPKC zeta mTOR pathway: a new target for rituximab therapy in follicular lymphomaBlood2008111128529117855629
- YounesATherapeutic activity of mTOR inhibitors in mantle cell lymphomaAutophagy20084570770918469512
- PeponiEActivation of mammalian target of rapamycin signaling promotes cell cycle progression and protects cells from apoptosis in mantle cell lymphomaAm J Pathol200616962171218017148679
- HippSRingshausenIOelsnerMBognerCPeschelCDeckerTInhibition of the mammalian target of rapamycin and the induction of cell cycle arrest in mantle cell lymphoma cellsHaematologica200590101433143416219581
- WolowiecDBergerFFfrenchPBryonPAFfrenchMCDK1 and cyclin A expression is linked to cell proliferation and associated with prognosis in non-Hodgkin’s lymphomasLeuk Lymphoma1999351–214715710512172
- GelebartPAnandMArmaniousHConstitutive activation of the Wnt canonical pathway in mantle cell lymphomaBlood2008112135171517918787224
- YazbeckVYBuglioDGeorgakisGVTemsirolimus downregulates p21 without altering cyclin D1 expression and induces autophagy and synergizes with vorinostat in mantle cell lymphomaExp Hematol200836444345018343280
- GiatromanolakiAKoukourakisMIPezzellaFPhosphorylated VEGFR2/KDR receptors are widely expressed in B-cell non-Hodgkin’s lymphomas and correlate with hypoxia inducible factor activationHematol Oncol200826421922418461646
- KoomagiRZintlFSauerbreyAVolmMVascular endothelial growth factor in newly diagnosed and recurrent childhood acute lymphoblastic leukemia as measured by real-time quantitative polymerase chain reactionClin Cancer Res20017113381338411705851
- HazarBPaydasSZorludemirSSahinBTuncerIPrognostic significance of microvessel density and vascular endothelial growth factor (VEGF) expression in non-Hodgkin’s lymphomaLeuk Lymphoma200344122089209314959852
- KuramotoKSakaiAShigemasaKHigh expression of MCL1 gene related to vascular endothelial growth factor is associated with poor outcome in non-Hodgkin’s lymphomaBr J Haematol2002116115816111841410
- PottiAGantiAKKargasSKochMImmunohistochemical detection of C-kit (CD117) and vascular endothelial growth factor (VEGF) overexpression in mantle cell lymphomaAnticancer Res20022252899290112530014
- GalimbertiSNagyBPalumboGAVascular endothelial growth factor polymorphisms in mantle cell lymphomaActa Haematol20101232919520029173
- RouxPPShahbazianDVuHRAS/ERK signaling promotes site-specific ribosomal protein S6 phosphorylation via RSK and stimulates cap-dependent translationJ Biol Chem200728219140561406417360704
- KurieJMMorseHCIIIPrincipatoMAv-myc and v-raf act synergistically to induce B-cell tumors in pristane-primed adult BALBC miceOncogene1990545775822183159
- NagyBGalimbertiSBenedettiERAF-1 over-expression does condition survival of patients affected by aggressive mantle cell lymphomaLeuk Res200731111595159717572489
- NagyBLundánTLarramendyMLAbnormal expression of apoptosis-related genes in hematological malignancies: overexpression of MYC is poor prognostic sign in mantle cell lymphomaBr J Haematol2003120344344441
- MillsJRHippoYRobertFmTORC1 promotes survival through translational control of Mcl-1Proc Natl Acad Sci U S A200810531108531085818664580
- RinaldiAKweeITaborelliMGenomic and expression profiling identifies the B-cell associated tyrosine kinase Syk as a possible therapeutic target in mantle cell lymphomaBr J Haematol2006132330331616409295
- HudesGRBerkenblitAFeingoldJAtkinsMBRiniBIDutcherJClinical trial experience with temsirolimus in patients with advanced renal cell carcinomaSemin Oncol200936Suppl 3S26S3619963097
- MitaMMMitaARowinskyEKMammalian target of rapamycin: a new molecular target for breast cancerClin Breast Cancer20034212613712864941
- MitaMMTolcherAWThe role of mTOR inhibitors for treatment of sarcomasCurr Oncol Rep20079431632217588357
- TolcherAWNovel therapeutic molecular targets for prostate cancer: the mTOR signaling pathway and epidermal growth factor receptorJ Urol2004171S4143 discussion S44.14713752
- CoiffierBRibragVExploring mammalian target of rapamycin (mTOR) inhibition for treatment of mantle cell lymphoma and other hematologic malignanciesLeuk Lymphoma200950121916193019757306
- BoniJPHugBLeisterCSonnichsenDIntravenous temsirolimus in cancer patients: clinical pharmacology and dosing considerationsSemin Oncol200936Suppl 3S18S2519963096
- WitzigTEGeyerSMGhobrialIPhase II trial of single-agent temsirolimus (CCI-779) for relapsed mantle cell lymphomaJ Clin Oncol200523235347535615983389
- SankhalaKMitaAKellyKMahalingamDGilesFMitaMThe emerging safety profile of mTOR inhibitors, a novel class of anticancer agentsTarget Oncol20094213514219381454
- AnsellSMInwardsDJRowlandKMJrLow-dose, single-agent temsirolimus for relapsed mantle cell lymphoma: a phase 2 trial in the North Central Cancer Treatment GroupCancer2008113350851418543327
- HessGHerbrechtRRomagueraJPhase III study to evaluate temsirolimus compared with investigator’s choice therapy for the treatment of relapsed or refractory mantle cell lymphomaJ Clin Oncol200927233822382919581539
- HessGRomagueraJHerbrechtRTemsirolimus for the treatment of patients with relapsed or refractory mantle cell lymphoma. Supportive efficacy analyses from the phase 3 studyHaematologica200994Suppl 2S391 Abstract 0973.
- AnsellSMTangHKurtinPA phase II study of temsirolimus (CCI-779) in combination with rituximab in patients with relapsed or refractory mantle cell lymphoma [ASH Annual Meeting Abstracts]Blood20091141665
- ReederCBGornetMKHabermannTMA phase II trial of the oral mTOR inhibitor everolimus (RAD001) in relapsed aggressive non-Hodgkin lymphoma (NHL) [ASH Annual Meeting Abstracts]Blood2007110121